Abstract
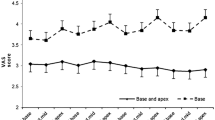
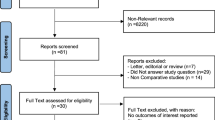
Performance of 16 (16 g) (n=103) and 18 gauge (18 g) (n=101) biopsy needles in transrectal ultrasound (TRUS)-guided 10-core prostate biopsies were compared in terms of cancer detection and pre-defined specimen quality criteria in this prospective randomized study. Cancer detection rates of the two groups were similar, although the mean core volume of 16 g needles was almost twice that of 18 g needles. On the other hand, using 16 g needles significantly improved specimen quality by acquiring less empty cores, small cores and fragmented cores. There were no significant differences among the complication rates and VAS pain scores of the two groups. Sixteen gauge needles can safely be used in TRUS-guided prostate biopsies, as they improve specimen quality without increasing morbidity and patient discomfort.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Paul R, Korzinek C, Necknig U, Niesel T, Alschibaja M, Leyh H et al. Influence of transrectal ultrasound probe on prostate cancer detection in transrectal ultrasound-guided sextant biopsy of prostate. Urology 2004; 64: 532–536.
Vanderkerken J, de la Rosette J, Laguna P, Debruyne F . How and when to take prostate biopsies. Eur Urol 2002; (Suppl 1): 15–20.
Norberg M, Egevad L, Holmberg L, Sparen P, Norten BJ, Busch C . The sextant protocol for ultrasound-guided core biopsies of the prostate underestimates the presence of cancer. Urology 1997; 50: 562–566.
Naughton CK, Miller DC, Mager DE, Ornstein DK, Catalona WJ . A prospective randomized trial comparing 6 versus 12 prostate biopsy cores: impact on cancer detection. J Urol 2000; 164: 388–392.
Pepe P, Aragona F . Prostate needle biopsy: 12 vs 18 cores—is it necessary? Urol Int 2005; 74: 19–22.
de la Taille A, Antiphon P, Salomon L, Cherfan M, Porcher R, Hozneck A et al. Prospective evaluation of a 21-sample needle biopsy procedure designed to improve the prostate cancer detection rate. Urology 2003; 61: 1181–1186.
Taylor JA, Gangarczyk KJ, Fant GV, Mcleod DG . Increasing number of core samples taken at prostate needle biopsy enhances the detection of clinically significant prostate cancer. Urology 2002; 60: 841–845.
Iczkowski KA, Casella G, Seppala RJ, Jones GL, Mishler BA, Qian J et al. Needle core length in sextant biopsy influences prostate cancer detection rate. Urology 2002; 59: 698–703.
Fink K, Hutarew G, Szlauer R, Goetschl R, Schmeller NT . Evaluation of 16-gauge needles for prostate biopsy. Eur Urol Suppl 2006; 5: 312.
Ficarra V, Martignoni G, Novella G, Cerruto MA, Galfano A, Novara G et al. Needle core length is a quality indicator of systematic transperineal prostate biopsy. Eur Urol 2006; 50: 266–271.
Scattoni V, Zlotta AR, Nava L, Roscigno M, Montorsi F, Rigatti P . Prostatic transrectal ultrasound (TRUS) guided biopsy schemes and TRUS prostatic lesion-guided biopsies. Eur Urol 2002; (Suppl 1): 28–34.
Dogan HS, Eskicorapci SY, Ertoy-Baydar D, Akdogan B, Gunay LM, Ozen H . Can we obtain better specimens with an end-cutting prostatic biopsy device? Eur Urol 2005; 47: 297–301.
Ubhayakar GN, Li WY, Corbishley CM, Patel U . Improving glandular coverage during prostate biopsy using a long-core needle: technical performance of an end-cutting needle. BJU Int 2002; 89: 40–43.
Özden E, Göğüş Ç, Tulunay Ö, Baltaci S . The long core needle with end-cut technique for prostate biopsy: Does it really have advantages when compared with standard needles? Eur Urol 2004; 45: 287–291.
Haggarth L, Ekman P, Egevad L . A new core-biopsy instrument with an end-cut technique provides prostate biopsies with increased tissue yield. BJU Int 2002; 90: 51–55.
Levine MA, Ittman M, Melamed J, Lepor H . Two consecutive sets of transrectal ultrasound guided sextant biopsies of the prostate for detection of prostate cancer. J Urol 1998; 159: 471–475.
Karakiewicz PL, Bazinet M, Aprikian AG, Trudel C, Aronson S, Nachabe M et al. Outcome of sextant biopsy according to gland volume. Urology 1997; 49: 55–59.
Guichard G, Larré S, Gallina A, Lazar A, Faucon H, Chemama S et al. Extended 21-sample needle biopsy protocol for diagnosis of prostate cancer in 1000 consecutive patients. Eur Urol 2007; 52: 430–435.
Eskew LA, Bare RL, McCullough DL . Systematic 5 region prostate biopsy is superior to sextant method for diagnosing carcinoma of the prostate. J Urol 1997; 157: 199–202.
Gore JL, Shariat SF, Miles BJ, Kadmon D, Jiang N, Wheeler TM et al. Optimal combinations of systematic sextant and laterally directed biopsies for the detection of prostate cancer. J Urol 2001; 165: 1554–1559.
Morote J, Lopez M, Encabo G, de Torres I . Value of routine transition zone biopsies in patients undergoing ultrasound-guided sextant biopsies for the first time. Eur Urol 1999; 35: 294–297.
Terris MK, Pham TQ, Issa MM, Kabalin JN . Routine transition zone and seminal vesicle biopsies in all patients undergoing transrectal ultrasound guided prostate biopsies are not indicated. J Urol 1997; 157: 204–206.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Inal, G., Öztekin, V., Uğurlu, Ö. et al. Sixteen gauge needles improve specimen quality but not cancer detection rate in transrectal ultrasound-guided 10-core prostate biopsies. Prostate Cancer Prostatic Dis 11, 270–273 (2008). https://doi.org/10.1038/pcan.2008.34
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2008.34
Keywords
This article is cited by
-
Stochastic Sequential Modeling: Toward Improved Prostate Cancer Diagnosis Through Temporal-Ultrasound
Annals of Biomedical Engineering (2021)