Abstract
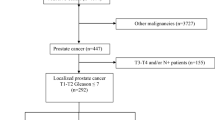
We assessed the impact of bother with urinary and bowel dysfunction on social activities among men in Japan and the United States following primary therapy for localized prostate cancer. In paired longitudinal outcomes studies, we measured general and disease-specific health-related quality of life in 400 Japanese and 427 American men who underwent radical prostatectomy or brachytherapy for localized prostate cancer. Outcomes included the social function domain of the Medical Outcomes Study Short Form-36 and the University of California, Los Angeles Prostate Cancer Index, all of which are scored 0–100. Participants completed the questionnaires before and 1, 12 and 24 months after treatment. Among men who reported any urinary bother, Japanese men had slightly better urinary function than American men (84 vs 77, P<0.01). Before brachytherapy, urinary bother was weakly correlated with social function in both the countries; after brachytherapy, urinary bother was strongly correlated with social function in American but not Japanese men. After brachytherapy, bowel dysfunction had a stronger correlation with social function in American than Japanese men (P<0.05). The bother associated with urinary and bowel dysfunction after surgery or brachytherapy for prostate cancer has a greater impact on social function in American men than in Japanese men.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Litwin MS, Hays RD, Fink A, Ganz PA, Leak B, Leach GE et al. Quality-of-life outcomes in men treated for localized prostate cancer. JAMA 1995; 273: 129.
Smedley BD . Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academies Press: Washington, DC, 2003.
Johnson TK, Gilliland FD, Hoffman RM, Deapen D, Penson DF, Stanford JL et al. Racial/Ethnic differences in functional outcomes in the 5 years after diagnosis of localized prostate cancer. J Clin Oncol 2004; 22: 4193.
Namiki S, Kwan L, Kagawa-Singer M, Tochigi T, Ioritani N, Terai A et al. Cultural comparison of sexual function following radical prostatectomy between Japanese and American men: a prospective longitudinal study. Prostate Cancer Prostatic Dis; e-pub ahead of print October 2007.
Namiki S, Kwan L, Kagawa-Singer M, Saito S, Terai A, Satoh T et al. Sexual function reported by Japanese and American men. J Urol 2008; 179: 245.
Litwin MS, Lubeck DP, Spitalny GM, Henning JM, Carroll PR . Mental health in men treated for early stage prostate carcinoma: a posttreatment, longitudinal quality of life analysis from the cancer of the prostate strategic urologic research endeavor. Cancer 2002; 95: 54.
Walsh PC . Anatomical radical retropubic prostatectomy.In: Walsh PC, Retik AB, Vaughan Jr ED et al. (eds). Campbell's Urology,7th edn, WB Saunders: Philadelphia, 1998, pp 2565.
Sylvester J, Blasko JC, Grimm P, Ragde H . Interstitial implantation techniques in prostate cancer. J Surg Oncol 1997; 66: 65–75.
Hays RD, Sherbourne CD, Mazel RM . The RAND 36-Item Health Survey 1.0. Health Econ 1993; 2: 217.
McHorney CA, Ware Jr JE, Rogers W, Raczek AE, Lu JF . The validity and relative precision of MOS short- and long-form health status scales and Dartmouth COOP charts. Results from the Medical Outcomes Study. Med Care 1992; 5: 253.
Litwin MS, Hays RD, Fink A, Ganz PG, Leake B, Brook RH . The UCLA Prostate Cancer Index: development, reliability, and validity of a health-related quality of life measure. Med Care 1998; 36: 1002.
Fukuhara S, Ware J, Koshinski M . Psychometric and clinical tests of validity of the Japanese SF-36 health survey. J Clin Epidemiol 1998; 51: 1045.
Kakehi Y, Kamoto T, Osamu O, Arai Y, Litwin MS, Fukuhara S . Development Japanese version of the UCLA Prostate Cancer Index: a pilot validation study. Int J Clin Oncol 2002; 7: 306.
Namiki S, Kuwahara M, Ioritani N, Akito T, Arai Y . An evaluation of urinary function after radical prostatectomy in Japanese men: concordance with definitions of urinary continence. BJU Int 2005; 95: 530.
Krupski TL, Saigal CS, Litwin MS . Variation in continence and potency by definition. J Urol 2003; 170: 1291.
Cella D, Lai JS, Chang CH, Peterman A, Slavin M . Fatigue in cancer patients compared with fatigue in the general United States population. Cancer 2002; 94: 528.
Litwin MS, Pasta DJ, Yu J, Stoddard ML, Flanders SC . Urinary function and bother after radical prostatectomy or radiation for prostate cancer: a longitudinal, multivariate quality of life analysis from the cancer of the prostate strategic urologic research endeavor. J Urol 2000; l64: 1973.
Hoffman RH, Hunt WC, Stephenson RA . Patient satisfaction with treatment decisions for clinically localized prostate carcinoma. Results from the Prostate Cancer Outcomes Study. Cancer 2003; 97: 1653.
Lilleby W, Fosså SD, Waehre HR, Olsen DR . Long-term morbidity and quality of life in patients with localized prostate cancer undergoing definitive radiotherapy or radical prostatectomy. Int J Radiat Oncol Biol Phys 1999; 43: 735.
Litwin MS, Flanders SC, Pasta DJ, Stoddard ML, Lubeck DP, Henning JM . Sexual function and bother after radical prostatectomy or radiation for prostate cancer: multivariate quality-of-life analysis from CaPSURE. Cancer of the Prostate Strategic Urologic Research Endeavor. Urology 1999; 54: 503.
Matsumura S, Bito S, Liu H, Kahn K, Fukuhara S, Kagawa-Singer M et al. Acculturation of attitudes toward end-of-life care: a cross-cultural survey of Japanese Americans and Japanese. J Gen Intern Med 2002; 17: 531.
Northouse LL, Mood DW, Montie JE, Sandler HM, Forman JD, Hussain M et al. Living with prostate cancer: patients’ and spouses’ psychosocial status and quality of life. J Clin Oncol 2007; 25: 4171.
Kagawa-Singer M . Redefining health: living with cancer. Soc Sci Med 1993; 37: 295.
Acknowledgements
Dr Tatsuo Tochigi and Dr Sadafumi Kawamura, Miyagi Cancer Center; Dr Naomasa Ioritani and Dr Masataka Aizawa, Sendai Shakaihoken Hospital; Emiko Izutu, Tohoku University Hospital and Griselda Lopez, University of California, Los Angeles, assisted with data collection and management.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Namiki, S., Kwan, L., Kagawa-Singer, M. et al. Distress and social dysfunction following prostate cancer treatment: a longitudinal cross-cultural comparison of Japanese and American men. Prostate Cancer Prostatic Dis 12, 67–71 (2009). https://doi.org/10.1038/pcan.2008.20
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2008.20
Keywords
This article is cited by
-
The effect of ethnicity and sexual preference on prostate-cancer-related quality of life
Nature Reviews Urology (2012)