Abstract
Embryonal cancer can arise from postnatally persistent embryonal remnant or rest cells, which are uniquely characterized by the absence of p53 mutations. Perinatal overexpression of the MycN oncoprotein in embryonal cancer precursor cells causes postnatal rests, and later tumor formation through unknown mechanisms. However, overexpression of Myc in adult tissues normally activates apoptosis and/or senescence signals as an organismal defense mechanism against cancer. Here, we show that perinatal neuroblastoma precursor cells exhibited a transiently diminished p53 response to MycN oncoprotein stress and resistance to trophic factor withdrawal, compared with their adult counterpart cells from the TH-MYCN+/+ transgenic mouse model of neuroblastoma. The adult stem cell maintenance factor and Polycomb group protein, Bmi1 (B-cell-specific Moloney murine leukemia virus integration site), had a critical role at neuroblastoma initiation in the model, by repressing p53 responses in precursor cells. We further show in neuroblastoma tumor cells that Bmi1 could directly bind p53 in a complex with other Polycomb complex proteins, Ring1A or Ring1B, leading to increased p53 ubiquitination and degradation. Repressed p53 signal responses were also seen in precursor cells for other embryonal cancer types, medulloblastoma and acute lymphoblastic leukemia. Collectively, these date indicate a general mechanism for p53 inactivation in some embryonal cell types and consequent susceptibility to MycN oncogenesis at the point of embryonal tumor initiation.
Similar content being viewed by others
Introduction
Neuroblastoma and medulloblastoma are embryonal childhood tumors of the peripheral and central nervous systems, respectively.1, 2 The early onset of the disease and the potential of some neuroblastoma cell lines to differentiate into several distinct cell types in vitro, point to neuroblastoma as a disease of neural crest-derived stem cells.3, 4 Medulloblastoma arises from granule neurone precursors (GNPs) of the developing cerebellum.5 The mechanism of embryonal cancer initiation is unknown.
During normal embryonal neurodevelopment there is high proliferation and migration of neural crest cells, however, only 15–40% of post-migratory cells survive to form mature neural tissues.6 Postnatally persistent embryonal cells with tumorigenic capacity must possess both the capacity to resist cell death imposed by trophic factor withdrawal during the final stages of neurodevelopment and undergo secondary changes that characterize later tumor promotion and progression.
We have previously shown that perinatal MycN oncoprotein expression in neuroblastoma and medulloblastoma precursor cells can cause postnatal neuroblast and GNP hyperplasia, respectively, which are initiating events in these diseases.7, 8 MycN belongs to the Myc family of transcription factors and, although commonly overexpressed by many human cancers, its regulated expression is essential for the development of the nervous system.9 A peculiarity of Myc proteins is their capacity to both enhance cell proliferation and survival through influences on the cell cycle, and conversely, sensitize cells for apoptosis through mechanisms such as p53 upregulation and/or activation.10, 11 Indeed, p53 has recently been identified as a MycN target gene, and the ability of MycN to sensitize cells for p53-mediated apoptosis acts is a safeguard against cancer.12 These data suggest that MycN upregulation cannot be solely responsible for embryonal tumor initiation, and that additional factors are required to block p53-mediated apoptosis.
Several mechanisms have already been suggested to explain p53 downregulation in neuroblastoma, including upregulation of MDM2 (murine double minute) and Bmi1 (B-cell-specific Moloney murine leukemia virus integration site).13, 14 Although MDM2 is a major regulator of p53, MDM2 amplification has been seen in only 2% of neuroblastoma15 and p53/MDM2 pathway repression is most evident at relapse,16 suggesting that MDM2-independent mechanisms are likely to be involved in the inhibition of cell death in neuroblastoma at the initiation stage. Bmi1 was first described as an oncogene cooperating with c-Myc during the initiation of lymphomas17, 18 and its upregulation has frequently been observed in many human cancers,19 including neuroblastoma.13, 20 Bmi1 expression has an important role in both the development and maintenance of cancer stem cells by conferring on them stem-like properties, such as resistance to death signaling.21 Some molecular mechanisms underlying the regulation of apoptosis and differentiation by Bmi1 have been proposed, such as repression of the tumor suppressors p16INK4a and p19ARF (p14ARF in humans),19 but other mechanisms are likely to be involved.
Here, we identified a novel mechanism for Bmi1-mediated inactivation of apoptotic barriers. Bmi1 reduced p53 protein levels by directly inducing its polyubiquitination and proteasomal degradation. Bmi1 repressed p53 responses in neuroblastoma precursor cells, suggesting some specialised perinatal cells exposed to an oncogenic MycN signal can resist cell death and persist postnatally due to an inherent regulatory effect of Bmi1 on p53 stress responses. These results suggest that drugs targeting Bmi1 activity may restore p53 activation, causing subsequent tumor cell death in vivo, and hence may have an important impact in the design of future therapeutic strategies for child cancer prevention.
Results
MycN protects neuroblastoma precursor cells from death stimuli
In the TH-MYCN+/+ transgenic mouse model of neuroblastoma, MycN oncoprotein expression is targeted to the neural crest, thereby inducing neuroblastoma development with a phenotypic, biochemical and cytogenetic profile very similar to the human disease.22 Importantly, this model fully recapitulates the p53 wild-type (WT) status, chemosensitivity and p53-dependent apoptotic responses of human neuroblastoma.23, 24 We first used neuroblastoma precursor cells (that is, perinatal primary sympathetic ganglia from the TH-MYCN+/+ mice) to investigate the effects of MycN expression on the response to death stimuli and the replicative potential of these precancer cells.
We found that cultured paravertebral ganglia cells from 2-week-old homozygote TH-MYCN+/+ transgenic mice were resistant to cell death caused by the withdrawal of nerve growth factor, the trophic factor for sympathetic nervous tissue, when compared with normal WT controls (Figure 1a). Perinatal ganglia cells from normal mice or rats infected with a MycN-expressing adenoviral vector in vitro also demonstrated resistance to nerve growth factor withdrawal, indicating that death resistance in TH-MYCN+/+ ganglia cells was caused by MycN expression and not factors specific to the transgene (Figure 1b). Terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) immunofluorescence indicated that MycN expression blocked the apoptotic response of neuroblastoma precursor cells (Figure 1c). Furthermore, we analyzed two key molecules in terminal stages of apoptosis: the activation of caspase-activated deoxyribonuclease (CAD), which is responsible for inter-nucleosomal DNA cleavage; and, the release of the apoptosis-inducing factor (AIF), which stimulates chromatin condensation. When MycN-expressing cells were exposed to apoptotic stimuli, we observed inhibition of CAD activation and thus inability to translocate from the cytoplasm to the nucleus (Figure 1d). We also observed little mitochondrial release and translocation of AIF to the nucleus in MycN-expressing cells (Figure 1e). The protective effect of MycN was also seen when ganglia were exposed to other noxious stimuli, such as serum withdrawal or hypoxia in vitro (Supplementary Figure S1). TH-MYCN+/+ mice were then injected with 5-bromo-2'-deoxyuridine at 2 weeks of age and neuroblast replication in vivo was assessed by immunohistochemistry in paravertebral ganglia. As expected, MycN expression caused a marked increase in neuroblast replication compared with WT controls (Figure 1f).
MYCN protects precursor cells for neuroblastoma from death stimuli. (a) Survival of cultured ganglia cells from 2-week-old WT littermates or homozygous TH-MYCN+/+ transgenic mice following nerve growth factor (NGF) withdrawal, was determined using neuron-specific βIII tubulin immunofluorescent staining (green). (b) Ganglia cells in culture from 2-week-old mice or rats infected with an adenovirus containing a MYCN-expressing, or a control vector were subjected to NGF withdrawal. Cell viability was quantified by βIII tubulin staining. (c) Apoptosis in cultured ganglion cells from 2-week-old WT or homozygous TH-MYCN+/+ transgenic mice following NGF withdrawal, was measured by TUNEL assay. (d) Ganglia cells were treated with and without NGF for 48 h, then were analyzed for activation of caspase-activated DNase (CAD). The bar graph represents percentage of cells with active CAD translocating into the nucleus to induce rapid fragmentation of nuclear DNA. (e) Quantitation of the percentage of cells with the pro-apoptotic molecule, apoptosis-inducing factor (AIF), translocating from the mitochondria to the nucleus after NGF withdrawal for 48 h. (f) TH-MYCN+/+ mice or WT littermates were given a single intraperitoneal dose of 5-bromo-2'-deoxyuridine (BrdU) (50 mg/kg) at postnatal day 0, 7, 14, or 6 weeks in the case of tumors, and were then euthanized at 6 h post injection. The percentage of BrdU-positive cells in hyperplastic regions of ganglia tissue sections was then analyzed (*P<0.05, **P<0.01, ***P<0.001. All error bars represent means±s.e.m.). (g) Quantitation of percentage of viable cultured ganglia cells from 6-week-old WT mice, or neuroblastoma tumor cell line (NHO2A) derived from a TH-MYCN+/+ mouse tumor, expressing MYCN or control vector, following the serum withdrawal.
We next examined whether the protective effect of a MycN signal could also be conferred upon the mature postnatal cells developing from perinatal neuroblasts. In stark contrast, MycN overexpression in neuroblastoma tumor cell lines (NHO2A cells) derived from TH-MYCN+/+ mouse tumors,23 or primary ganglia cells from 6-week-old WT mice, caused marked cell death in the absence of trophic factor (Figure 1g). These results suggested that the barriers present in normal adult cells exposed to oncoprotein stress were transiently and specifically repressed in perinatal neuroblasts.
Neuroblastoma precursor cells exhibit transient repression of the p53 signal response to MycN oncoprotein stress
An important determinant of Myc-induced apoptosis is the p53 stress response signal.25 Deleting p53 from TH-MYCN+/+ mice has recently been shown to enhance tumorigenicity.24 We evaluated p53 responses to growth factor withdrawal by culturing ganglia from 6-week-old WT, 2-week-old WT or 2-week-old TH-MYCN+/+ mice, subjecting them to growth factor deprivation, and assaying p53 expression by immunofluorescence. Mature ganglia cells from 6-week-old WT mice showed robust p53 responses. In contrast, perinatal 2-week WT ganglia cells exhibited a twofold reduction in p53 responses, while 2-week TH-MYCN+/+ ganglia responses were threefold lower than 6-week-old WT ganglia (Figure 2a and Supplementary Figure S2a). Although exogenous p53 overexpression, restored cell death in the presence or absence of trophic factor in perinatal ganglia cells from both WT and TH-MYCN+/+ mice (Figure 2b), the MDM2 inhibitor, Nutlin-3A, only partially restored death sensitivity in TH-MYCN+/+ ganglia (Figure 2c). In contrast, treatment with quinacrine, known to activate p53 through an MDM2-independent mechanism,26 restored p53 expression (Supplementary Figure S2b) and death sensitivity (Figure 2c) after trophic factor withdrawal in 2-week-old TH-MYCN+/+ ganglia. These results suggested that MycN protects neuroblastoma precursor cells from cell death induced by trophic factor withdrawal through MDM2-independent repression of the p53.
Neuroblastoma precursor cells exhibit transient repression of the p53 signal response to MYCN oncoprotein stress. (a) The bar graph represents quantitation of the mean p53 intensity present in each nucleus using the Imaris software (Bitplane, South Windsor, CT, USA) from TUNEL negative but p53-positive cells (**P<0.01, *P<0.05. All error bars represent means±s.e.m.). (b) Adenoviral p53 expression plasmids or control adenoviruses were used to infect cultured ganglia cells from the indicated mice, followed by nerve growth factor (NGF) withdrawal. Cell viability was quantified by βIII tubulin staining. (c) Ganglion cells in culture from the indicated mice were subjected to NGF withdrawal, with or without Nutlin-3 A (10 μM) or Quinacrine (0.2 μM), and assessed for viability using βIII tubulin positivity (**P<0.01, ***P<0.001. All error bars represent means±s.e.m.).
Bmi1 has a critical role in neuroblastoma tumor initiation
We next investigated the relative roles of Bmi1 and MDM2 as potential negative regulators of the p53 stress signal response in neuroblastoma precursor cells. We showed that Mdm2 mRNA levels were not markedly increased when ganglia cells from 2-week WT, 2-week TH-MYCN+/+ and tumor tissue from TH-MYCN+/+ mice were compared with mature ganglia cells from 6-week WT mice (Figure 3a). This data further support an MDM2-independent mechanism of p53 signal repression. In contrast, we found Bmi1 mRNA expression demonstrated a marked and stepwise increase in 2-week-old ganglia and tumor tissue from TH-MYCN+/+ mice in comparison with their WT counterparts (Figure 3a). The oncogenic function of Bmi1 has been attributed to the transcriptional repression of the Ink4a/ARF (alternate reading frame) locus coding for the p16Ink4a and p19/p14ARF tumor suppressors.19 In agreement, we showed that relative p16Ink4a mRNA levels were inversely proportional to the relative levels of Bmi1 mRNA expression (Figures 3a and b). In contrast, we found a higher p19ARF level in ganglia from 2-week-old TH-MYCN+/+ or WT mice compared with 6-week-old WT mice (Figure 3b), thereby suggesting that the role of Bmi1 upregulation in neuroblastoma precursor cells may not be mediated by p19ARF transcriptional repression.
Bmi1 has a critical role in neuroblastoma tumor initiation. (a, b) Primary ganglia tissue was isolated from the indicated mice and total mRNA was extracted to analyze the expression of Bmi1, p16, p19 or Mdm2 by quantitative RT–PCR. (c) Cultured ganglia cells from 2-week-old TH-MYCN+/+ mice were infected with an adenoviral construct containing a Bmi1-specific, or a control (Ctl), short hairpin RNA (shRNA), subjected to serum withdrawal, and assessed for viability using βIII tubulin positivity. (d) TH-MYCN+/− mice were crossed with Bmi1+/− mice to create TH-MYCN+/− × Bmi1+/− offspring, which were then assessed for the comparative incidence of tumor-free survival, compared with parent genotypes. (e) Superior cervical and celiac ganglia were collected from mice on postnatal day 12. Sections of ganglia were stained with hematoxylin and eosin and examined with a light microscope for the presence of hyperplastic lesions. Shown are percentages of hyperplasia-containing ganglia from mice of the indicated genotype (means±s.e.m; n=12–15). The proportion of ganglia with neuroblast hyperplasias or rests (>30 cell aggregates) from the offspring were determined by light microscopy from hematoxylin and eosin-stained tissue sections of paravertebral ganglia (***P<0.001, **P<0.01. All error bars represent means±s.e.m.).
Using an adenoviral vector expressing a Bmi1-specific short hairpin RNA, we demonstrated that knocking down Bmi1 in neuroblastoma precursor cells from 2-week-old TH-MYCN+/+ mice restored sensitivity to serum withdrawal (Figure 3c) and a fivefold increase in the proportion of p53-positive cells following serum withdrawal and Bmi1 knockdown, indicating Bmi1 as a critical factor in MycN-mediated death resistance of neuroblastoma precursor cells (Supplementary Figure S3).
We next examined the role of Bmi1 in MycN tumorigenesis in vivo. Importantly, when we crossed hemizygote TH-MYCN+/− mice with hemizygote Bmi+/− knockout mice, we demonstrated a complete loss of tumorigenicity (Figure 3d). All Bmi+/− × TH-MYCN+/+ mice died within the first week of life. We next analyzed and compared perinatal ganglia for histologic evidence of tumor initiation (Figure 3e). We showed a marked 8.5-fold reduction in neuroblast hyperplasia in tumor-prone ganglia from 2-week-old TH-MYCN+/− × Bmi1+/− mice, highlighting Bmi1 as a critical co-factor in embryonal tumor initiation and progression in vivo. In contrast, TH-MYCN+/+ mice crossed with MDM2+/− hemizygote knockout mice demonstrated a smaller 1.9-fold decrease in neuroblast hyperplasia (Figure 3e). Taken together, these results indicated that increased Bmi1 levels in neuroblastoma precursor cells contributed to p53 downregulation and cell death resistance. Bmi1 appeared to be a more potent factor than MDM2 at the point of embryonal tumor initiation.
Bmi1 regulates p53 protein stability independent of MDM2 and ARF
Bmi1 is a component of the Polycomb group multi-protein PRC1 complex, required to maintain the transcriptionally repressive state of several genes, including the Ink4a/ARF locus. It has been shown that when ARF expression is repressed by Bmi1, MDM2 is free to polyubiquitinate p53 and induce its proteasomal degradation.19 We examined the hypothesis that Bmi1 modulated p53 protein stability in human neuroblastoma tumor cell lines. The p53 protein half-life was markedly increased following Bmi1 knockdown with specific small interfering RNA in human NBL-S (Figures 4a and b) and BE(2)C (Supplementary Figure S4) neuroblastoma cells, whereas, exogenous Bmi1 overexpression reduced p53 protein half-life (Figure 4c). Importantly, when the same experiments were conducted in the presence of Nutlin-3A there was no change in the effect of Bmi1 on p53, indicating an MDM2-independent process (Figure 4d). Additionally, the SHEP human neuroblastoma cell line, which is known to carry a homozygous deletion of the p14ARF gene,27 also demonstrated an increased p53 protein stability following Bmi1 knockdown (Figures 4e and f), thereby suggesting that the Bmi1 effect on p53 protein stability is also independent of p14ARF transcriptional regulation. Together these results indicated that Bmi1 regulated p53 protein stability in an MDM2- and ARF-independent manner.
Bmi1 regulates p53 protein stability in an mdm2- and p14arf-independent way. (a, b, e, and f) NBL-S (a, b) or SHEP (e, f) human neuroblastoma cell lines were transfected with either a scrambled or a Bmi1-specific small interfering RNA (siRNA). (c, d) NBL-S cells were transfected with either a Bmi1-flag expressing vector or the corresponding empty vector and treated with Nutlin (10 μM) where indicated. (a, c, and e) Cells were treated with the inhibitor of protein synthesis cycloheximide (25 μg/ml) and lysed at the indicated times. Whole-cell extracts were analyzed by western blotting using anti-p53, -Bmi1 or -actin antibodies.
Bmi1 directly binds p53 and induces p53 polyubiquitination
Bmi1 is known to enhance the E3 ubiquitin-ligase activity of Ring1A and Ring1B, and control the proteasomal degradation of a non-histone protein, topoisomerase 2α,28 indicating that the Bmi1-induced phenotype can be mediated via mechanisms that do not involve transcriptional regulation. Consequently, we examined whether Bmi1 could bind p53 and directly induce its polyubiquitination. We first showed in two human neuroblastoma cell lines (NBL-S and SHEP) that endogenous p53 from whole-cell lysates was co-immunoprecipitated with Flag-tagged Bmi1 (Figure 5a). We next performed glutathione S-transferase (GST) Pull-Down assays using GST fusion Ring1A and Ring1B proteins (produced in bacteria and purified on glutathione-sepharose beads, Supplementary Figure S5a) and whole-cell extracts from SHEP cells either non-transfected or transfected with a p53-Flag expressing vector. These experiments demonstrated that the two Ring proteins also directly bound to endogenous or overexpressed p53 (Figure 5b). In addition, in the presence of overexpressed Bmi1, p53 binding to both GST-Ring1A and GST-Ring1B increased slightly (Supplementary Figure S5b), thereby suggesting that Bmi1 might facilitate this binding, possibly as a scaffold protein.
Bmi1 Binds p53 and, together with Ring1A or Ring1B, directly induces p53 polyubiquitination. (a) SHEP and NBL-S cells were transfected with either a Bmi1-flag expressing vector or the corresponding empty vector. Whole-cell extracts were incubated with anti-flag antibodies to immunoprecipitate Bmi1. The immunoprecipitated samples, as well as the inputs, were analyzed by western blotting using anti-p53 or anti-flag antibodies. (b) Whole-cell extracts from SHEP cells overexpressing, or not, p53-flag were incubated with recombinant GST, GST-Ring1A or GST-Ring1B proteins produced in bacteria and purified on glutathione-sepharose beads. After incubation, these samples, as well the inputs (IN), were analyzed by western blotting using anti-p53 antibodies. (c, e) NBL-S (c) or SHEP (e) cells were transfected with either a Bmi1-flag expressing vector or a control vector, together with either an Ubiquitin-HA expressing vector or a control vector. Forty-eight hours after transfection, cells were treated with Nutlin (10 μM, 8 h) and MG132 (15 μM, 5 h), and lysed. Whole-cell extracts were incubated with anti-p53 antibodies. The immunoprecipitated samples, as well as the inputs, were analyzed by western blotting using anti-flag, -HA or -p53 antibodies. (d, f) NBL-S (d) or SHEP (f) cells were transfected with either a scrambled or a Bmi1-specific small interfering RNA (siRNA). After 24 h, the same cells were transfected with either an HA-ubiquitin expressing vector or a control vector. Twenty-four hours later, cells were treated with MG132 (15 μM, 5 h) and whole-cell extracts were incubated with anti-p53 antibodies. The immunoprecipitated samples, as well as the inputs were analyzed by western blotting using anti-HA or -p53 antibodies. (g) The p53 substrate purified from SHEP cells was incubated in ubiquitination reactions containing the indicated components, and products were analyzed by western blotting using anti-p53 antibodies.
In order to assess whether Bmi1 can directly induce p53 polyubiquitination, we performed ex-vivo and in vitro ubiquitination assays. For ex-vivo assays, neuroblastoma cells were transfected with a HA-tagged ubiquitin-expressing vector or a control vector, together with a Flag-tagged Bmi1-expressing vector or a control vector. Proteasome-mediated degradation and MDM2-mediated p53 polyubiquitination were inhibited by treating the cells with MG132 and Nutlin-3A. The p53 protein was then immunoprecipitated from whole-cell lysates and analyzed by western blot using either HA-, p53- or Flag-specific antibodies. We observed increased p53 polyubiquitination in both NBL-S and p14ARF-deleted SHEP neuroblastoma cells overexpressing Bmi1 (Figures 5c and e, right panels). Conversely, Bmi1 knockdown markedly reduced p53 ubiquitination (Figures 5d and f). We verified that these results were not due to a difference in p53 expression levels (Supplementary Figure S5c–f). In addition, Bmi1 itself appeared to be mono-ubiquitinated (Figures 5c and e, left panels), as previously described.29
In vitro ubiquitination reactions were performed using purified and eluted GST-tagged Bmi1, together with either GST-Ring1A or GST-Ring1B as E3 ligase complexes. The p53 substrate was purified from whole SHEP protein extracts and incubated with ubiquitin reaction components including Ubiquitin, E1 (activating enzyme), E2 (conjugating enzyme) and E3 as indicated on Figure 5g. p53 ubiquitination was analyzed by western blot using anti-p53 antibodies. We showed that both Ring1A and Ring1B induced p53 mono- and di-ubiquitination, and that Bmi1 markedly increased the efficacy of the reaction (Figure 5g). We also identified UbcH5a and UbcH5c as E2 enzymes involved in the reaction (Figure 5g), whereas UbcH6 could not efficiently mediate Bmi1/Ring-dependent p53 ubiquitination (Supplementary Figure S5g). Collectively, these results demonstrated that the Bmi1/Ring1A and Bmi1/Ring1B complexes acted as E3 ubiquitin ligases for p53 by directly binding p53 and inducing its multiubiquitination in vitro and polyubiquitination ex vivo.
MYCN protects precursor cells for medulloblastoma and leukemia from death due to trophic factor withdrawal
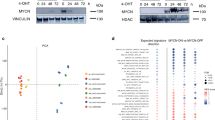
We next examined the hypothesis that aberrant MycN expression in precursor cells for other embryonal cancer types might also result in resistance to trophic factor withdrawal. Hyperplasia of medulloblastoma precursor cells or GNPs precedes medulloblastoma tumorigenesis in Ptch1+/− mice in a similar manner to neuroblastoma precursor cells in TH-MYCN+/+ mice.8 GNPs from 1-week-old Ptch1+/− mice exhibited increased survival when their trophic factor, sonic hedgehog (Shh), was withdrawn from the culture medium. We transfected Ptch1+/− GNPs with a MycN-specific small interfering RNA (Supplementary Figure S6a), and observed a significant increase in the level of apoptosis following Shh withdrawal, compared with control (Figure 6a). In agreement with previous studies suggesting a direct role for Bmi1 in medulloblastoma tumorigenesis,30 we found increased Bmi1 expression in perinatal Ptch1+/− GNPs and tumor, compared with perinatal WT GNPs (Figure 6b). Importantly, GNPs also failed to induce p53 following serum withdrawal (Figure 6c). These data implicate inactivation of the p53 stress response in GNPs at the time of medulloblastoma tumor initiation.
MYCN protects precursor cells for other embryonal malignancies from trophic factor withdrawal-induced death. (a) GNP from 1-week-old hemizygous Ptch1+/− knockout mice, or WT littermates, were cultured with and without their trophic factor, Shh, and evaluated for apoptosis using TUNEL immunofluorescent staining. Additionally, the same experiment was carried out after GNPs were transfected with a vector expressing an short hairpin RNA (shRNA), which blocked MYCN expression, or empty vector control. (b) GNPs from 1-week-old Ptch1+/− mice or WT littermates were isolated, along with medulloblastoma tumor tissue from Ptch1+/− mice, and total mRNA was extracted to analyze Bmi1 mRNA expression by quantitative RT–PCR. (c) An immunoblot stained with an antibody, which identified p53 or actin in GNP protein extracts, cultured with and without Shh, from 1-week-old Ptch1+/− or WT mice. Protein from the murine neuroblastoma NHO2A cells withdrawn from serum, was used as a positive control for p53 expression. (d) Primary murine Pre-B lymphocytes were purified from the bone marrow of 2-week-old normal mice, grown continuously in IL-7, and then infected with a retrovirus expressing MYCN or empty vector. Pre-B cells, with or without MYCN, were compared for colony counts after 3 weeks in semi-solid culture conditions, following withdrawal of their trophic factor, IL-7. (e) TUNEL-positive pre-B cells measured by immunofluorescence in liquid culture 48 h after IL-7 withdrawal. (f) An immunoblot stained with an antibody that identified p53 or actin in protein extracts from Pre-B lymphocytes infected with a retrovirus expressing MYCN or empty vector following IL-7 withdrawal (***P<0.001, *P<0.05. All error bars represent means±s.e.m.).
Markers of the leukemic clone in pre-B lymphocytes can be detected perinatally in most children who much later develop acute lymphoblastic leukemia.31 Thus, we examined the hypothesis that perinatal murine pre-B cells, dependent on the trophic factor interleukin-7 (IL-7) for survival ex vivo, might also demonstrate a survival benefit when forced to express MycN. Pre-B cells, purified from the bone marrow of 2-week-old normal mice32 and infected with a retrovirus expressing MycN (Supplementary Figure S6b), demonstrated enhanced colony forming ability following withdrawal of IL-7, in liquid and semi-solid culture conditions, compared with vector only controls (Figure 6d). In a comparison with control pre-B cells, we also observed reduced apoptosis after IL-7 withdrawal in MycN-overexpressing cells as measured by TUNEL staining (Figure 6e), which correlated with a decreased p53 induction as shown by western blot (Figure 6f).
Discussion
Following organogenesis, embryonal cells produced in excess of requirements are deleted by mechanisms such as trophic factor insufficiency.6 If this process is incomplete, embryonal cell rests may persist to later become cancerous, a theory suggested more than a century ago33, 34 and more recently confirmed by murine and human studies.7, 35, 36 Our findings have important implications for our understanding of rest cell persistence and embryonal tumorigenesis, and the links between normal embryogenesis and cancer.
Here, we showed that MycN overexpression caused resistance to death from trophic factor withdrawal in normal perinatal precursor cells for three different embryonal cancer types, in agreement with previous studies in neuroblastoma models.37, 38 Importantly, we showed that this effect was transient in the perinatal period and correlated with increased Bmi1 mRNA expression, compared with mature postnatal cells. Moreover, Bmi1 mRNA expression was induced by MycN in a stepwise manner during tumorigenesis, consistent with a recent study showing that MycN induced Bmi1 transcription.20 The presence of high Bmi1 levels in both cancer precursor cells and normal perinatal cells is consistent with its role in the regulation of stem cell maintenance and renewal, as well as in the development and progression of human cancers.19
Normal differentiated cells have an equilibrium between the expression levels of pro-apoptotic and antiapoptotic proteins. In normal neural progenitor cells, medulloblastoma and neuroblastoma cells, this equilibrium appeared to be shifted towards repressed pro-apoptotic p53 stress responses, thereby impairing MycN capacity to sensitize cells for apoptosis. This is presumably because embryonal malignancies arise from progenitor cells, which are already proliferating as part of normal development.39 Importantly, we have shown that Bmi1 knockdown in neuroblastoma precursor cells and normal perinatal cells restored p53 responses and death sensitivity. We hypothesize that transient Bmi1-mediated p53 downregulation in normal perinatal cells could have a protective value, as the embryonal environment can be subjected to frequent stresses, such as hypoxia or nutrient deprivation. The protective function of Bmi1 during embryogenesis may be exploited during embryonal tumor initiation through persistent downregulation of p53 responses (Figure 7).
A model for neuroblastoma initiation. Following migration from the neural crest to their final destination, both progenitor cells (neuroblasts, yellow) and post-mitotic neurons (orange) are produced in excess to final requirements. Only those cells that have differentiated and made appropriate connections are retained, other cells being deleted by apoptosis. The immature neurons die in large numbers as they compete for trophic factors (e.g. nerve growth factor (NGF)). We propose that MycN (red) and Bmi1 (purple) overexpression, as well as apoptosis pathway downregulation, are required for normal neural crest development. However, neuroblasts can persist pathologically postnatally, evading apoptotic mechanisms, due to transient repression of the p53 (green) stress response signal by Bmi1 and continued exposure to MycN. Further postnatal oncogenic events are required to progress from precancer cells to neuroblastoma. Downregulated proteins are represented in gray. Green and red arrows indicate upregulation and downregulation, respectively.
The molecular mechanism so far proposed to explain Bmi1-mediated apoptosis regulation is via the repression of p19ARF (p14ARF in humans) transcription, consequent inhibition of MDM2 and stabilization of p53. However, we did not observe a decrease in p19ARF mRNA levels synchronous with the increased Bmi1 levels in WT and TH-MYCN+/+ perinatal ganglia cells. Moreover, the MDM2 inhibitor, Nutlin-3A, could not completely restore death sensitivity and p53 levels in neuroblastoma precursor cells. These observations suggested that an Ink4a/ARF-independent mechanism was responsible for the Bmi1-mediated regulation of p53 levels that we observed, in agreement with recent studies in neural stem cells and several cancers.40, 41 Here, for the first time, we found that Bmi1 directly bound, together with Ring1A and Ring1B, to the p53 protein and induced its polyubiquitination and subsequent degradation.
Although Bmi1 itself lacks E3 enzymatic activity, it can act as a dose-dependent modulator of Ring1B and Ring1A E3 ubiquitin-ligase activity.29 However, in agreement with various reports showing that Bmi1 is the rate-limiting factor in the ubiquitination reactions mediated by the Ring proteins,28, 29 we demonstrated that Bmi1 overexpression or knockdown was sufficient to, respectively, induce or inhibit p53 polyubiquitination and regulate p53 stability. In vitro, we showed that Bmi1 strongly increased both Ring1A- and Ring1B-mediated p53 mono- and di-ubiquitination, thereby suggesting that an E4 enzyme is necessary in vivo for the elongation of the ubiquitin chain primed by these two E3 ligase complexes, as previously shown for MDM2-mediated p53 polyubiquitination.42, 43 Indeed, although known to directly induce p53 polyubiquitination, MDM2 does not polyubiquitinate p53 in vitro. Instead, it catalyzes the addition of single ubiquitin moieties to p53, thereby priming it for E4 enzyme-mediated ubiquitin chain elongation.42, 43
Importantly, Bmi1 expression was necessary for neuroblastoma initiation in TH-MYCN transgenic mice in vivo. Although we and others14 have previously demonstrated a role for MDM2 in embryonal cancer development, here we showed that the role of MDM2 in embryonal cancer initiation is less significant than the role played by Bmi1. Mdm2 mRNA levels were not significantly increased in normal perinatal cells or neuroblastoma precursor cells when compared with mature cells. TH-MYCN+/+ mice crossed with Mdm2+/− hemizygote knockout mice demonstrated only a small decrease in neuroblast hyperplasia. Nutlin-3A treatment of perinatal ganglia from TH-MYCN+/+ mice did not completely restore sensitivity to cell death after trophic factor withdrawal, whereas Bmi1 knockdown in the same cells had a much stronger effect. These findings are crucial for guiding future development of new drugs for neuroblastoma treatment or prevention.
The TP53 gene encoding the p53 protein is probably the most commonly mutated gene in human cancers, but it is rarely mutated in embryonal tumors.11 However, inactivation of p53 contributes significantly to the development of these two tumors in specific animal models.24, 44 Our findings demonstrate that p53 responses are markedly and transiently repressed by Bmi1, and to a much lesser extent MDM2, in normal perinatal precursor cells for medulloblastoma and neuroblastoma, providing a possible explanation for the lack of p53 gene deletions or mutations in embryonal cancer types. Moreover, our data indicate that reactivation of the p53 stress response through the inhibition of Bmi1 activity in precancer cells may be an effective prevention strategy for human embryonal cancer.
Materials and methods
Cell culture
SHEP-S1, BE(2)-C, and NBL-S neuroblastoma cells and HEK293 embryonic kidney cells were cultured in Dulbecco's modified Eagle's medium supplemented with 10% fetal calf serum. Mouse and rat primary ganglion cells were maintained in complete Neurobasal-A media (Invitrogen, Mount Waverley, VIC, Australia) on poly-D-lysine and laminin-coated coverslips (HD Scientific, Wetherill Park, NSW, Australia) in 24-well plates in the presence of 3.3 μM Aphidicolin (Sigma Aldrich, Castle Hill, NSW, Australia) and 50 ng/ml nerve growth factor (GroPep, Adelaide, SA, Australia). Mouse NHO2A, perpetuated from a TH-MYCN+/+ mouse tumor, were grown in RPMI 1640 with 20% fetal calf serum-supplemented 2 mM L-glutamine, 1 mM sodium pyruvate, 1 × nonessential amino acids and penicillin/streptomycin (Invitrogen).
Mouse primary GNPs were grown in neurobasal media supplemented with 1% v/v N2, 1 mM sodium pyruvate solution, 1% v/v penicillin-streptomycin (Invitrogen) and 20 ng/ml Shh (R&D systems, Minneapolis, MN, USA). Pre-B cells were grown in RPMI 1640 media (Gibco, Melbourne, Victoria, Australia) containing 10% fetal calf serum, 10 ng/ml recombinant mouse IL-7 (R&D systems) and 50 μM β Mercaptoethanol (Invitrogen).
Mouse models
TH-MYCN+/+ transgenic mice on a mixed C57BL/6J and 129 × 1/SvJ genetic background, where the human MYCN cDNA is expressed in a tissue-specific manner under the influence of the rat tyrosine hydroxylase promoter, were a generous gift from Dr W Weiss at University of California, San Francisco.22 The neuroblastoma tumor incidence for TH-MYCN mice is 30% at 13 weeks of age for hemizygotes and 100% at 6 weeks of age for homozygotes. For the cross between Bmi1 knockout mice and TH-MYCN transgenic mice, TH-MYCN transgenic mice on the 129 × 1/SvJ genetic background were obtained from the Mouse Models of Human Cancers Consortium at National Cancer Institute-Frederick. Bmi1+/− mice45 on the C57BL/6J genetic background was kindly provided by Dr Sean Morrison at the University of Michigan at Ann Arbor, with the permission from Dr Maarten van Lohuizen at the Netherlands Cancer Institute. WT, hemizygous MYCN+/− and MYCN+/−/Bmi1+/− mice were generated by crossing MYCN+/−/Bmi1+/− mice with Bmi1+/− mice and maintained under specific pathogen-free conditions at the animal facility of the University of Toledo Health Science Campus. The MDM2+/− gene knockout mice on a C57BL/6J genetic background were kindly provided by Dr G Lozano, MD Anderson Cancer Center, Houston, TX, USA. Mouse crosses between TH-MYCN+/− transgenic, and Bmi+/− knockout mice at the University of Toledo College of Medicine, Toledo, OH, USA, and MDM2 knockout mice at Texas Children’s Hospital, Houston, TX, USA were carried out after five to seven backcrosses against the genetic background strain, to ensure congenicity. Mice with a conditional allele of Patched1 (Ptcflox/+) were created at the Institute for Molecular Biosciences at the University of Queensland, Brisbane, Australia.46 They were mated with transgenic mice carrying the Cre recombinase gene under the control of the rat nestin promoter and enhancer (NestinCre/Cre), to create hemizygous Ptch1 knockout (+/−) mice. All animal studies were pre-approved by the Institutional Animal Care and Use Committees at the four institutions.
Primary ganglia, GNP and Pre-B cell isolation
Primary paravertebral ganglia tissue was isolated from 2-week or 6-week-old homozygous TH-MYCN+/+ transgenic mice or WT littermates, and tumor tissue from 6-week-old TH-MYCN+/+ mice as previously described.7 GNPs were isolated from the cerebellum of 1-week-old Ptch1+/− mice or WT littermates. Tumor tissue was isolated from 20-week-old Ptc1+/− mice displaying signs of ataxia as previously described.8 Conditions for the derivation and culture of bone marrow derived B cells were adapted from published work.47
Apoptosis assays
Apoptotic cell death of primary ganglia, GNPs and pre-B cells following growth factor withdrawal was measured by the TUNEL assay. In brief, the primary cultures were grown in the presence nerve growth factor, Shh or IL-7. The cells were then deprived of trophic factor for 24 h, fixed and incubated with the TUNEL reaction mixture (Roche, Sydney, NSW, Australia). The treated cells were washed and visualized using fluorescence microscopy. The proportion of TUNEL-positive cells was determined and expressed as a percentage of primary cells maintained in the trophic factor.
The cells were also incubated with for β-III tubulin (1:400) and caspase-activated deoxyribonuclease (1:200) or apoptosis-inducing factor (1:100) antibodies (Chemicon, Temecula, CA, USA) for 1 h at room temperature, followed by Cy3 and Alexa 488 secondary antibodies for 30 min. The cells were then mounted using Vectorshield medium containing 4',6-diamidino-2-phenylindole and examined by fluorescence microscopy.
Ex vivo ubiquitination assays
For ex vivo ubiquitination assays, neuroblastoma cell lines were transfected with an HA-tagged Ubiquitin-expressing vector (or a control vector) either together with a Flag-Bmi1 expressing vector (or a control vector) or 24 h after transfection with a Bmi1-specific (or scrambled) small interfering RNA. Forty-eight hours after the first transfection, cells were pre-treated for 3 h with the MDM2 inhibitor Nutlin-3 A (10 μM) and then treated for five extra hours with the protease inhibitor MG132 (15 μM). Cells were lysed in Ubiquitin Lysis Buffer containing N-ethyl-maleimide, and protease and phosphatase inhibitors. Cell lysates were pre-incubated 1 h at 4 °C with an anti-p53 antibody and then over night at 4 °C with G Sepharose beads (Sigma, St Louis, MO, USA). After extensive washes with Ubiquitin Lysis Buffer, the immunoprecipitated samples, as well as inputs were resolved by sodium dodecyl sulfate–PAGE and analyzed by western blot using the indicated antibodies.
Statistics
Statistical analyses were performed with the Student’s t-test for independent samples (nonparametric), and results are expressed as mean±s.e. unless otherwise specified. P-value ⩽0.05 was considered as statistically significant. Cell-based studies consisted of 4–12 independent experiments. In animal-based studies, n=5–10 animals per group.
References
Brodeur GM . Neuroblastoma: biological insights into a clinical enigma. Nat Rev Cancer 2003; 3: 203–216.
Gilbertson RJ . Medulloblastoma: signalling a change in treatment. Lancet Oncol 2004; 5: 209–218.
Ciccarone V, Spengler BA, Meyers MB, Biedler JL, Ross RA . Phenotypic diversification in human neuroblastoma cells: expression of distinct neural crest lineages. Cancer Res 1989; 49: 219–225.
Ross RA, Spengler BA, Domenech C, Porubcin M, Rettig WJ, Biedler JL . Human neuroblastoma I-type cells are malignant neural crest stem cells. Cell Growth Differ 1995; 6: 449–456.
Yang ZJ, Ellis T, Markant SL, Read TA, Kessler JD, Bourboulas M et al. Medulloblastoma can be initiated by deletion of Patched in lineage-restricted progenitors or stem cells. Cancer Cell 2008; 14: 135–145.
Lossi L, Merighi A . In vivo cellular and molecular mechanisms of neuronal apoptosis in the mammalian CNS. Prog Neurobiol 2003; 69: 287–312.
Hansford LM, Thomas WD, Keating JM, Burkhart CA, Peaston AE, Norris MD et al. Mechanisms of embryonal tumor initiation: distinct roles for MycN expression and MYCN amplification. Proc Natl Acad Sci USA 2004; 101: 12664–12669.
Thomas WD, Chen J, Gao YR, Cheung B, Koach J, Sekyere E et al. Patched1 deletion increases N-Myc protein stability as a mechanism of medulloblastoma initiation and progression. Oncogene 2009; 28: 1605–1615.
Thomas WD, Raif A, Hansford L, Marshall G . N-myc transcription molecule and oncoprotein. Int J Biochem Cell Biol 2004; 36: 771–775.
Hogarty MD . The requirement for evasion of programmed cell death in neuroblastomas with MYCN amplification. Cancer Lett 2003; 197: 173–179.
Johnsen JI, Kogner P, Albihn A, Henriksson MA . Embryonal neural tumours and cell death. Apoptosis 2009; 14: 424–438.
Chen L, Iraci N, Gherardi S, Gamble LD, Wood KM, Perini G et al. p53 is a direct transcriptional target of MYCN in neuroblastoma. Cancer Res 2010; 70: 1377–1388.
Cui H, Hu B, Li T, Ma J, Alam G, Gunning WT et al. Bmi-1 is essential for the tumorigenicity of neuroblastoma cells. Am J Pathol 2007; 170: 1370–1378.
Chen Z, Lin Y, Barbieri E, Burlingame S, Hicks J, Ludwig A et al. Mdm2 deficiency suppresses MYCN-Driven neuroblastoma tumorigenesis in vivo. Neoplasia 2009; 11: 753–762.
Momand J, Jung D, Wilczynski S, Niland J . The MDM2 gene amplification database. Nucleic Acids Res 1998; 26: 3453–3459.
Peirce SK, Findley HW . Targeting the MDM2-p53 interaction as a therapeutic strategy for the treatment of cancer. Cell Health and Cytoskeleton 2010; 2: 49–58.
Haupt Y, Alexander WS, Barri G, Klinken SP, Adams JM . Novel zinc finger gene implicated as myc collaborator by retrovirally accelerated lymphomagenesis in E mu-myc transgenic mice. Cell 1991; 65: 753–763.
van Lohuizen M, Verbeek S, Scheijen B, Wientjens E, van der Gulden H, Berns A . Identification of cooperating oncogenes in E mu-myc transgenic mice by provirus tagging. Cell 1991; 65: 737–752.
Jiang L, Li J, Song L . Bmi-1 stem cells and cancer. Acta Biochim Biophys Sin 2009; 41: 527–534.
Ochiai H, Takenobu H, Nakagawa A, Yamaguchi Y, Kimura M, Ohira M et al. Bmi1 is a MYCN target gene that regulates tumorigenesis through repression of KIF1Bbeta and TSLC1 in neuroblastoma. Oncogene 2010; 29: 2681–2690.
Kang MK . Polycomb group proteins: new targets of anti-cancer therapy. Cell Cycle 2010; 9: 2704.
Weiss WA, Aldape K, Mohapatra G, Feuerstein BG, Bishop JM . Targeted expression of MYCN causes neuroblastoma in transgenic mice. EMBO J 1997; 16: 2985–2995.
Cheng AJ, Cheng NC, Ford J, Smith J, Murray JE, Flemming C et al. Cell lines from MYCN transgenic murine tumours reflect the molecular and biological characteristics of human neuroblastoma. Eur J Cancer 2007; 43: 1467–1475.
Chesler L, Goldenberg DD, Collins R, Grimmer M, Kim GE, Tihan T et al. Chemotherapy-induced apoptosis in a transgenic model of neuroblastoma proceeds through p53 induction. Neoplasia 2008; 10: 1268–1274.
Sherr CJ . Divorcing ARF and p53: an unsettled case. Nat Rev Cancer 2006; 6: 663–673.
Gurova KV, Hill JE, Guo C, Prokvolit A, Burdelya LG, Samoylova E et al. Small molecules that reactivate p53 in renal cell carcinoma reveal a NF-kappa B-dependent mechanism of p53 suppression in tumors. Proc Natl Acad Sci USA 2005; 102: 17448–17453.
Carr J, Bell E, Pearson AD, Kees UR, Beris H, Lunec J et al. Increased frequency of aberrations in the p53/MDM2/p14(ARF) pathway in neuroblastoma cell lines established at relapse. Cancer Res 2006; 66: 2138–2145.
Alchanati I, Teicher C, Cohen G, Shemesh V, Barr HM, Nakache P et al. The E3 ubiquitin-ligase Bmi1/Ring1A controls the proteasomal degradation of Top2alpha cleavage complex—a potentially new drug target. PLoS One 2009; 4: e8104.
Buchwald G, van der Stoop P, Weichenrieder O, Perrakis A, van Lohuizen M, Sixma TK . Structure and E3-ligase activity of the Ring-Ring complex of polycomb proteins Bmi1 and Ring1b. EMBO J 2006; 25: 2465–2474.
Leung C, Lingbeek M, Shakhova O, Liu J, Tanger E, Saremaslani P et al. Bmi1 is essential for cerebellar development and is overexpressed in human medulloblastomas. Nature 2004; 428: 337–341.
Taub JW, Konrad MA, Ge Y, Naber JM, Scott JS, Matherly LH et al. High frequency of leukemic clones in newborn screening blood samples of children with B-precursor acute lymphoblastic leukemia. Blood 2002; 99: 2992–2996.
Whitlock CA, Witte ON . Long-term culture of murine bone marrow precursors of B lymphocytes. Methods Enzymol 1987; 150: 275–286.
Cohnheim J . Lectures on General Pathology. New Sydenham Society, London, 1889.
Durante F . [Nesso fisio-patologico tra la struttura dei nei materni e la genesi di alcuni tumori maligni]. Arch Memo Observ Chir Prat 1874; 11: 217–226.
Beckwith JB, Perrin EV . In situ neuroblastomas: a contribution to the natural history of neural crest tumors. Am J Pathol 1963; 43: 1089–1104.
Woods WG, Tuchman M, Robison LL, Bernstein M, Leclerc JM, Brisson LC et al. A population-based study of the usefulness of screening for neuroblastoma. Lancet 1996; 348: 1682–1687.
Jasty R, van Golen C, Lin HJ, Solomon G, Heidelberger K, Polverini P et al. Bcl-2 and M-Myc coexpression increases IGF-IR and features of malignant growth in neuroblastoma cell lines. Neoplasia 2001; 3: 304–313.
Wartiovaara K, Barnabe-Heider F, Miller FD, Kaplan DR . N-myc promotes survival and induces S-phase entry of postmitotic sympathetic neurons. J Neurosci 2002; 22: 815–824.
Scotting PJ, Walker DA, Perilongo G . Childhood solid tumours: a developmental disorder. Nat Rev Cancer 2005; 5: 481–488.
Alajez NM, Shi W, Hui AB, Yue S, Ng R, Lo KW et al. Targeted depletion of BMI1 sensitizes tumor cells to P53-mediated apoptosis in response to radiation therapy. Cell Death Differ 2009; 16: 1469–1479.
Fasano CA, Dimos JT, Ivanova NB, Lowry N, Lemischka IR, Temple S . shRNA knockdown of Bmi-1 reveals a critical role for p21-Rb pathway in NSC self-renewal during development. Cell Stem Cell 2007; 1: 87–99.
Grossman SR, Deato ME, Brignone C, Chan HM, Kung AL, Tagami H et al. Polyubiquitination of p53 by a ubiquitin ligase activity of p300. Science 2003; 300: 342–344.
Lai Z, Ferry KV, Diamond MA, Wee KE, Kim YB, Ma J et al. Human mdm2 mediates multiple mono-ubiquitination of p53 by a mechanism requiring enzyme isomerization. J Biol Chem 2001; 276: 31357–31367.
Wetmore C, Eberhart DE, Curran T . Loss of p53 but not ARF accelerates medulloblastoma in mice heterozygous for patched. Cancer Res 2001; 61: 513–516.
van der Lugt NM, Domen J, Linders K, van Roon M, Robanus-Maandag E, te Riele H et al. Posterior transformation, neurological abnormalities, and severe hematopoietic defects in mice with a targeted deletion of the bmi-1 proto-oncogene. Genes Dev 1994; 8: 757–769.
Ellis T, Smyth I, Riley E, Graham S, Elliot K, Narang M et al. Patched 1 conditional null allele in mice. Genesis 2003; 36: 158–161.
Rolink A, Kudo A, Karasuyama H, Kikuchi Y, Melchers F . Long-term proliferating early pre B cell lines and clones with the potential to develop to surface Ig-positive, mitogen reactive B cells in vitro and in vivo. EMBO J 1991; 10: 327–336.
Acknowledgements
We thank W Weiss for the TH-MYCN mice, and D Kaplan for the adenoviral vector MYCN constructs. This work was supported by the National Health & Medical Research Council of Australia, Cancer Institute New South Wales, Cure for Life Foundation and the Cancer Council New South Wales.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Oncogene website
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Calao, M., Sekyere, E., Cui, H. et al. Direct effects of Bmi1 on p53 protein stability inactivates oncoprotein stress responses in embryonal cancer precursor cells at tumor initiation. Oncogene 32, 3616–3626 (2013). https://doi.org/10.1038/onc.2012.368
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/onc.2012.368
Keywords
This article is cited by
-
Cellular senescence in neuroblastoma
British Journal of Cancer (2022)
-
Heterochromatic genome instability and neurodegeneration sharing similarities with Alzheimer’s disease in old Bmi1+/− mice
Scientific Reports (2019)
-
The novel BMI-1 inhibitor PTC596 downregulates MCL-1 and induces p53-independent mitochondrial apoptosis in acute myeloid leukemia progenitor cells
Blood Cancer Journal (2017)
-
Single nucleotide polymorphism rs11669203 in TGFBR3L is associated with the risk of neuroblastoma in a Chinese population
Tumor Biology (2016)
-
miR-200c Inhibits invasion, migration and proliferation of bladder cancer cells through down-regulation of BMI-1 and E2F3
Journal of Translational Medicine (2014)