Abstract
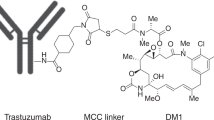
Anthracyclines and taxanes have remarkable anticancer efficacy, but have poor selectivity and high toxicity. Targeted delivery of chemotherapeutics has emerged as a strategy to achieve higher drug levels at the tumor site, to spare noncancerous tissue and potentially to use lower systemic drug doses, thus preventing side effects. In this study, we targeted the HER2 receptor using the monoclonal antibody (mAb) Herceptin (Trastuzumab) chemically conjugated to Doxorubicin or Taxol. In vitro, drug–Herceptin conjugates exhibited cytotoxicity comparable to equimolar concentrations of free drugs, with the benefit that the cytotoxicity of the conjugates was selective for cells expressing the HER2 target. In vivo, treatment of tumor-bearing mice with Taxol–Herceptin conjugates had a reduction of primary tumors comparable to equivalent doses of free drugs. However, Taxol–Herceptin conjugates significantly reduced metastasis compared with equivalent doses of free drugs. Thus, the data support the concept that conjugates might target metastasis better than primary tumors. This would offer a potential therapeutic approach for management of metastatic breast cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Monneret C . Recent developments in the field of antitumour anthracyclines. Eur J Med Chem 2001; 36: 483–493.
Menzin AW, King SA, Aikins JK, Mikuta JJ, Rubin SC . Taxol (paclitaxel) was approved by FDA for the treatment of patients with recurrent ovarian cancer. Gynecol Oncol 1994; 54: 103.
Tewey KM, Chen GL, Nelson EM, Liu LF . Intercalative antitumor drugs interfere with the breakage-reunion reaction of mammalian DNA topoisomerase II. J Biol Chem 1984; 259: 9182–9187.
Schiff PB, Fant J, Horwitz SB . Promotion of microtubule assembly in vitro by taxol. Nature 1979; 277: 665–667.
Schiff PB, Horwitz SB . Taxol stabilizes microtubules in mouse fibroblast cells. Proc Natl Acad Sci USA 1980; 77: 1561–1565.
Lyass O, Uziely B, Ben-Yosef R, Tzemach D, Heshing NI, Lotem M et al. Correlation of toxicity with pharmacokinetics of pegylated liposomal doxorubicin (Doxil) in metastatic breast carcinoma. Cancer 2000; 89: 1037–1047.
da Rocha AB, Lopes RM, Schwartsmann G . Natural products in anticancer therapy. Curr Opin Pharmacol 2001; 1: 364–369.
Danesi R, Fogli S, Gennari A, Conte P, Del Tacca M . Pharmacokinetic-pharmacodynamic relationships of the anthracycline anticancer drugs. Clin Pharmacokinet 2002; 41: 431–444.
Windebank AJ . Chemotherapeutic neuropathy. Curr Opin Neurol 1999; 12: 565–571.
Adams GP, Weiner LM . Monoclonal antibody therapy of cancer. Nat Biotechnol 2005; 23: 1147–1157.
Harris M . Monoclonal antibodies as therapeutic agents for cancer. Lancet Oncol 2004; 5: 292–302.
Reichert JM . Monoclonal antibodies as innovative therapeutics. Curr Pharm Biotechnol 2008; 9: 423–430.
Barros FF, Powe DG, Ellis IO, Green AR . Understanding the HER family in breast cancer: interaction with ligands, dimerization and treatments. Histopathology 2010; 56: 560–572.
Tai W, Mahato R, Cheng K . The role of HER2 in cancer therapy and targeted drug delivery. J Control Release 2010; 146: 264–275.
Dean-Colomb W, Esteva FJ . Her2-positive breast cancer: herceptin and beyond. Eur J Cancer 2008; 44: 2806–2812.
Freudenberg JA, Wang Q, Katsumata M, Drebin J, Nagatomo I, Greene MI . The role of HER2 in early breast cancer metastasis and the origins of resistance to HER2-targeted therapies. Exp Mol Pathol 2009; 87: 1–11.
Nahta R, Yu D, Hung MC, Hortobagyi GN, Esteva FJ . Mechanisms of disease: understanding resistance to HER2-targeted therapy in human breast cancer. Nat Clin Pract Oncol 2006; 3: 269–280.
Pohlmann PR, Mayer IA, Mernaugh R . Resistance to trastuzumab in breast cancer. Clin Cancer Res 2009; 15: 7479–7491.
Anhorn MG, Wagner S, Kreuter J, Langer K, von Briesen H . Specific targeting of HER2 overexpressing breast cancer cells with doxorubicin-loaded trastuzumab-modified human serum albumin nanoparticles. Bioconjug Chem 2008; 19: 2321–2331.
Guillemard V, Nedev HN, Berezov A, Murali R, Saragovi HU . HER2-mediated internalization of a targeted prodrug cytotoxic conjugate is dependent on the valency of the targeting ligand. DNA Cell Biol 2005; 24: 350–358.
Guillemard V, Saragovi HU . Novel approaches for targeted cancer therapy. Curr Cancer Drug Targets 2004; 4: 313–326.
Paik S, Bryant J, Park C, Fisher B, Tan-Chiu E, Hyams D et al. erbB-2 and response to doxorubicin in patients with axillary lymph node-positive, hormone receptor-negative breast cancer. J Natl Cancer Inst 1998; 90: 1361–1370.
Paik S, Bryant J, Tan-Chiu E, Yothers G, Park C, Wickerham DL et al. HER2 and choice of adjuvant chemotherapy for invasive breast cancer: national surgical adjuvant breast and bowel project protocol B-15. J Natl Cancer Inst 2000; 92: 1991–1998.
Pritchard KI, Shepherd LE, O'Malley FP, Andrulis IL, Tu D, Bramwell VH et al. HER2 and responsiveness of breast cancer to adjuvant chemotherapy. N Engl J Med 2006; 354: 2103–2111.
Ross JS, Slodkowska EA, Symmans WF, Pusztai L, Ravdin PM, Hortobagyi GN . The HER-2 receptor and breast cancer: ten years of targeted anti-HER-2 therapy and personalized medicine. Oncologist 2009; 14: 320–368.
Rayson D, Richel D, Chia S, Jackisch C, van der Vegt S, Suter T . Anthracycline-trastuzumab regimens for HER2/neu-overexpressing breast cancer: current experience and future strategies. Ann Oncol 2008; 19: 1530–1539.
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 2001; 344: 783–792.
Yu D . Mechanisms of ErbB2-mediated paclitaxel resistance and trastuzumab-mediated paclitaxel sensitization in ErbB2-overexpressing breast cancers. Semin Oncol 2001; 28: 12–17.
de Azambuja E, Bedard PL, Suter T, Piccart-Gebhart M . Cardiac toxicity with anti-HER-2 therapies: what have we learned so far? Target Oncol 2009; 4: 77–88.
Guillemard V, Saragovi HU . Taxane-antibody conjugates afford potent cytotoxicity, enhanced solubility, and tumor target selectivity. Cancer Res 2001; 61: 694–699.
Alley SC, Okeley NM, Senter PD . Antibody-drug conjugates: targeted drug delivery for cancer. Curr Opin Chem Biol 2010; 14: 529–537.
Guillemard V, Saragovi HU . Prodrug chemotherapeutics bypass p-glycoprotein resistance and kill tumors in vivo with high efficacy and target-dependent selectivity. Oncogene 2004; 23: 3613–3621.
Lewis Phillips GD, Li G, Dugger DL, Crocker LM, Parsons KL, Mai E et al. Targeting HER2-positive breast cancer with trastuzumab-DM1, an antibody-cytotoxic drug conjugate. Cancer Res 2008; 68: 9280–9290.
Kojic LD, Wiseman SM, Ghaidi F, Joshi B, Nedev H, Saragovi HU et al. Raft-dependent endocytosis of autocrine motility factor/phosphoglucose isomerase: a potential drug delivery route for tumor cells. PloS One 2008; 3: e3597.
Benlimame N, He Q, Jie S, Xiao D, Xu YJ, Loignon M et al. FAK signaling is critical for ErbB-2/ErbB-3 receptor cooperation for oncogenic transformation and invasion. J Cell Biol 2005; 171: 505–516.
Stockmeyer B, Beyer T, Neuhuber W, Repp R, Kalden JR, Valerius T et al. Polymorphonuclear granulocytes induce antibody-dependent apoptosis in human breast cancer cells. J Immunol 2003; 171: 5124–5129.
Cooley S, Burns LJ, Repka T, Miller JS . Natural killer cell cytotoxicity of breast cancer targets is enhanced by two distinct mechanisms of antibody-dependent cellular cytotoxicity against LFA-3 and HER2/neu. Exp Hematol 1999; 27: 1533–1541.
ElBayoumi TA, Torchilin VP . Tumor-targeted nanomedicines: enhanced antitumor efficacy in vivo of doxorubicin-loaded, long-circulating liposomes modified with cancer-specific monoclonal antibody. Clin Cancer Res 2009; 15: 1973–1980.
Nabholtz JM, Gligorov J . The role of taxanes in the treatment of breast cancer. Expert Opin Pharmacother 2005; 6: 1073–1094.
Tubiana-Hulin M . How to maximize the efficacy of taxanes in breast cancer. Cancer Treat Rev 2005; 31: S3–S9.
Krop IE, Beeram M, Modi S, Jones SF, Holden SN, Yu W et al. Phase I study of trastuzumab-DM1, an HER2 antibody-drug conjugate, given every 3 weeks to patients with HER2-positive metastatic breast cancer. J Clin Oncol 2010; 28: 2698–2704.
Kato H, Faria TN, Stannard B, Roberts CT, LeRoith D . Role of tyrosine kinase activity in signal transduction by the insulin-like growth factor-I (IGF-I) receptor. Characterization of kinase-deficient IGF-I receptors and the action of an IGF-I-mimetic antibody (alpha IR-3). J Biol Chem 1993; 268: 2655–2661.
Yen L, Benlimame N, Nie ZR, Xiao D, Wang T, Al Moustafa AE et al. Differential regulation of tumor angiogenesis by distinct ErbB homo- and heterodimers. Mol Biol Cell 2002; 13: 4029–4044.
Xu Y, Benlimame N, Su J, He Q, Alaoui-Jamali MA . Regulation of focal adhesion turnover by ErbB signalling in invasive breast cancer cells. Br J Cancer 2009; 100: 633–643.
Omelyanenko V, Kopeckova P, Gentry C, Shiah JG, Kopecek J . HPMA copolymer-anticancer drug-OV-TL16 antibody conjugates. 1. influence of the method of synthesis on the binding affinity to OVCAR-3 ovarian carcinoma cells in vitro. J Drug Target 1996; 3: 357–373.
Stan AC, Radu DL, Casares S, Bona CA, Brumeanu TD . Antineoplastic efficacy of doxorubicin enzymatically assembled on galactose residues of a monoclonal antibody specific for the carcinoembryonic antigen. Cancer Res 1999; 59: 115–121.
Acknowledgements
We are thankful to Amrit Kirpalani for help with in vivo assays. This work was funded by the McGill Center for Experimental Therapeutics in Cancer Fund to Cure Breast Cancer, and by the Canadian Institutes of Health Research (CIHR), and in part by the Quebec Breast Cancer Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Oncogene website
Supplementary information
Rights and permissions
About this article
Cite this article
Garcia, A., Nedev, H., Bijian, K. et al. Reduced in vivo lung metastasis of a breast cancer cell line after treatment with Herceptin mAb conjugated to chemotherapeutic drugs. Oncogene 32, 2527–2533 (2013). https://doi.org/10.1038/onc.2012.283
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/onc.2012.283