Abstract
The wild-type tumor-suppressor gene TP53 encodes several isoforms of the p53 protein. However, while the role of p53 in controlling normal cell cycle progression and tumor suppression is well established, the clinical significance of p53 isoform expression is unknown. A novel bioinformatic analysis of p53 isoform expression in 68 patients with acute myeloid leukemia revealed distinct p53 protein biosignatures correlating with clinical outcome. Furthermore, we show that mutated FLT3, a prognostic marker for short survival in AML, is associated with expression of full-length p53. In contrast, mutated NPM1, a prognostic marker for long-term survival, correlated with p53 isoforms β and γ expression. In conclusion, p53 biosignatures contain useful information for cancer evaluation and prognostication.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Aas T, Borresen AL, Geisler S, Smith-Sorensen B, Johnsen H, Varhaug JE et al. (1996). Specific P53 mutations are associated with de novo resistance to doxorubicin in breast cancer patients. Nat Med 2: 811–814.
Anensen N, Oyan AM, Bourdon JC, Kalland KH, Bruserud O, Gjertsen BT . (2006). A distinct p53 protein isoform signature reflects the onset of induction chemotherapy for acute myeloid leukemia. Clin Cancer Res 12: 3985–3992.
Bourdon JC, Fernandes K, Murray-Zmijewski F, Liu G, Diot A, Xirodimas DP et al. (2005). p53 isoforms can regulate p53 transcriptional activity. Genes Dev 19: 2122–2137.
Bourdon JC, Khoury MP, Diot A, Baker L, Fernandes K, Aoubala M et al. (2011). p53 mutant breast cancer patients expressing p53gamma have as good a prognosis as wild-type p53 breast cancer patients. Breast Cancer Res 13: R7.
Bruserud O, Hovland R, Wergeland L, Huang TS, Gjertsen BT . (2003). Flt3-mediated signaling in human acute myelogenous leukemia (AML) blasts: a functional characterization of Flt3-ligand effects in AML cell populations with and without genetic Flt3 abnormalities. Haematologica 88: 416–428.
Chen J, Ng SM, Chang C, Zhang Z, Bourdon JC, Lane DP et al. (2009). p53 Isoform delta113p53 is a p53 target gene that antagonizes p53 apoptotic activity via BclxL activation in zebrafish. Genes Dev 23: 278–290.
Chrisanthar R, Knappskog S, Lokkevik E, Anker G, Ostenstad B, Lundgren S et al. (2008). CHEK2 mutations affecting kinase activity together with mutations in TP53 indicate a functional pathway associated with resistance to epirubicin in primary breast cancer. PLoS One 3: e3062.
Dohner K, Schlenk RF, Habdank M, Scholl C, Rucker FG, Corbacioglu A et al. (2005). Mutant nucleophosmin (NPM1) predicts favorable prognosis in younger adults with acute myeloid leukemia and normal cytogenetics: interaction with other gene mutations. Blood 106: 3740–3746.
Estey E, Dohner H . (2006). Acute myeloid leukaemia. Lancet 368: 1894–1907.
Falini B, Mecucci C, Tiacci E, Alcalay M, Rosati R, Pasqualucci L et al. (2005). Cytoplasmic nucleophosmin in acute myelogenous leukemia with a normal karyotype. N Engl J Med 352: 254–266.
Fenaux P, Preudhomme C, Quiquandon I, Jonveaux P, Lai JL, Vanrumbeke M et al. (1992). Mutations of the P53 gene in acute myeloid leukaemia. Br J Haematol 80: 178–183.
Fridman JS, Lowe SW . (2003). Control of apoptosis by p53. Oncogene 22: 9030–9040.
Fujita K, Mondal AM, Horikawa I, Nguyen GH, Kumamoto K, Sohn JJ et al. (2009). p53 isoforms delta133p53 and p53beta are endogenous regulators of replicative cellular senescence. Nat Cell Biol 11: 1135–1142.
Gale RE, Hills R, Kottaridis PD, Srirangan S, Wheatley K, Burnett AK et al. (2005a). No evidence that FLT3 status should be considered as an indicator for transplantation in acute myeloid leukemia (AML): an analysis of 1135 patients excluding acute promyelocytic leukemia from the UK MRC AML10 and 12 trials. Blood 106: 3658–3665.
Gale RE, Hills R, Pizzey AR, Kottaridis PD, Swirsky D, Gilkes AF et al. (2005b). Relationship between FLT3 mutation status, biologic characteristics, and response to targeted therapy in acute promyelocytic leukemia. Blood 106: 3768–3776.
Gjertsen BT, Cressey LI, Ruchaud S, Houge G, Lanotte M, Doskeland SO . (1994). Multiple apoptotic death types triggered through activation of separate pathways by cAMP and inhibitors of protein phosphatases in one (IPC leukemia) cell line. J Cell Sci 107: 3363–3377.
Gjertsen BT, Oyan AM, Marzolf B, Hovland R, Gausdal G, Doskeland SO et al. (2002). Analysis of acute myelogenous leukemia: preparation of samples for genomic and proteomic analyses. J Hematother Stem Cell Res 11: 469–481.
Graupner V, Schulze-Osthoff K, Essmann F, Janicke RU . (2009). Functional characterization of p53beta and p53gamma, two isoforms of the tumor suppressor p53. Cell Cycle 8: 1238–1248.
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G et al. (1998). The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children′s Leukaemia Working Parties. Blood 92: 2322–2333.
Grisendi S, Mecucci C, Falini B, Pandolfi PP . (2006). Nucleophosmin and cancer. Nat Rev Cancer 6: 493–505.
Haferlach C, Dicker F, Herholz H, Schnittger S, Kern W, Haferlach T . (2008). Mutations of the TP53 gene in acute myeloid leukemia are strongly associated with a complex aberrant karyotype. Leukemia 22: 1539–1541.
Hainaut P . (1995). The tumor suppressor protein p53: a receptor to genotoxic stress that controls cell growth and survival. Curr Opin Oncol 7: 76–82.
Hall PA, McCluggage WG . (2006). Assessing p53 in clinical contexts: unlearned lessons and new perspectives. J Pathol 208: 1–6.
Irish JM, Hovland R, Krutzik PO, Perez OD, Bruserud O, Gjertsen BT et al. (2004). Single cell profiling of potentiated phospho-protein networks in cancer cells. Cell 118: 217–228.
Irish JM, Anensen N, Hovland R, Skavland J, Borresen-Dale AL, Bruserud O et al. (2007). Flt3 Y591 duplication and Bcl-2 overexpression are detected in acute myeloid leukemia cells with high levels of phosphorylated wild-type p53. Blood 109: 2589–2596.
Kojima K, Vickers SM, Adsay NV, Jhala NC, Kim HG, Schoeb TR et al. (2007). Inactivation of Smad4 accelerates Kras(G12D)-mediated pancreatic neoplasia. Cancer Res 67: 8121–8130.
Komeno Y, Kurokawa M, Imai Y, Takeshita M, Matsumura T, Kubo K et al. (2005). Identification of Ki23819, a highly potent inhibitor of kinase activity of mutant FLT3 receptor tyrosine kinase. Leukemia 19: 930–935.
Kottaridis PD, Gale RE, Frew ME, Harrison G, Langabeer SE, Belton AA et al. (2001). The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood 98: 1752–1759.
Levine AJ . (1997). p53, the cellular gatekeeper for growth and division. Cell 88: 323–331.
Levine AJ, Oren M . (2009). The first 30 years of p53: growing ever more complex. Nat Rev Cancer 9: 749–758.
Lonning PE . (2003). Study of suboptimum treatment response: lessons from breast cancer. Lancet Oncol 4: 177–185.
Löwenberg B, Downing JR, Burnett A . (1999). Acute myeloid leukemia. N Engl J Med 341: 1051–1062.
Löwenberg B, van Putten W, Theobald M, Gmur J, Verdonck L, Sonneveld P et al. (2003). Effect of priming with granulocyte colony-stimulating factor on the outcome of chemotherapy for acute myeloid leukemia. N Engl J Med 349: 743–752.
Löwenberg B . (2008). Acute myeloid leukemia: the challenge of capturing disease variety. Hematology Am Soc Hematol Educ Program 1–11.
Mayer RJ, Davis RB, Schiffer CA, Berg DT, Powell BL, Schulman P et al. (1994). Intensive postremission chemotherapy in adults with acute myeloid leukemia. Cancer and Leukemia Group B. N Engl J Med 331: 896–903.
Pardee TS, Zuber J, Lowe SW . (2011). Flt3-ITD alters chemotherapy response in vitro and in vivo in a p53-dependent manner. Exp Hematol 39: 473–485 e474.
Parsons DW, Jones S, Zhang X, Lin JC, Leary RJ, Angenendt P et al. (2008). An integrated genomic analysis of human glioblastoma multiforme. Science 321: 1807–1812.
Petitjean A, Achatz MI, Borresen-Dale AL, Hainaut P, Olivier M . (2007). TP53 mutations in human cancers: functional selection and impact on cancer prognosis and outcomes. Oncogene 26: 2157–2165.
Preudhomme C, Fenaux P . (1997). The clinical significance of mutations of the P53 tumour suppressor gene in haematological malignancies. Br J Haematol 98: 502–511.
Rohaly G, Chemnitz J, Dehde S, Nunez AM, Heukeshoven J, Deppert W et al. (2005). A novel human p53 isoform is an essential element of the ATR-intra-S phase checkpoint. Cell 122: 21–32.
Schnittger S, Schoch C, Kern W, Mecucci C, Tschulik C, Martelli MF et al. (2005). Nucleophosmin gene mutations are predictors of favorable prognosis in acute myelogenous leukemia with a normal karyotype. Blood 106: 3733–3739.
Schottelius A, Brennscheidt U, Ludwig WD, Mertelsmann RH, Herrmann F, Lubbert M . (1994). Mechanisms of p53 alteration in acute leukemias. Leukemia 8: 1673–1681.
Shah SP, Morin RD, Khattra J, Prentice L, Pugh T, Burleigh A et al. (2009). Mutational evolution in a lobular breast tumour profiled at single nucleotide resolution. Nature 461: 809–813.
Srinivasa SP, Doshi PD . (2002). Extracellular signal-regulated kinase and p38 mitogen-activated protein kinase pathways cooperate in mediating cytokine-induced proliferation of a leukemic cell line. Leukemia 16: 244–253.
Tallman MS, Gilliland DG, Rowe JM . (2005). Drug therapy for acute myeloid leukemia. Blood 106: 1154–1163.
Van Belle W, Anensen N, Haaland I, Bruserud O, Hogda KA, Gjertsen BT . (2006). Correlation analysis of two-dimensional gel electrophoretic protein patterns and biological variables. BMC Bioinform 7: 198.
Verhaak RG, Goudswaard CS, van Putten W, Bijl MA, Sanders MA, Hugens W et al. (2005). Mutations in nucleophosmin (NPM1) in acute myeloid leukemia (AML): association with other gene abnormalities and previously established gene expression signatures and their favorable prognostic significance. Blood 106: 3747–3754.
Vousden KH, Lane DP . (2007). p53 in health and disease. Nat Rev Mol Cell Biol 8: 275–283.
Wahlin A, Brinch L, Hornsten P, Evensen SA, Oberg G, Simonsson B et al. (1997). Outcome of a multicenter treatment program including autologous or allogeneic bone marrow transplantation for de novo acute myeloid leukemia. Eur J Haematol 58: 233–240.
Wheatley K, Burnett AK, Goldstone AH, Gray RG, Hann IM, Harrison CJ et al. (1999). A simple, robust, validated and highly predictive index for the determination of risk-directed therapy in acute myeloid leukaemia derived from the MRC AML 10 trial. United Kingdom Medical Research Council′s Adult and Childhood Leukaemia Working Parties. Br J Haematol 107: 69–79.
Yeh PY, Chuang SE, Yeh KH, Song YC, Chang LL, Cheng AL . (2004). Phosphorylation of p53 on Thr55 by ERK2 is necessary for doxorubicin-induced p53 activation and cell death. Oncogene 23: 3580–3588.
Acknowledgements
This study was supported by grants from the Research Council of Norway's National Program for Research in Functional Genomics, the Western Norway Regional Health Authority and the Norwegian Cancer Society.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Oncogene website
Rights and permissions
About this article
Cite this article
Ånensen, N., Hjelle, S., Van Belle, W. et al. Correlation analysis of p53 protein isoforms with NPM1/FLT3 mutations and therapy response in acute myeloid leukemia. Oncogene 31, 1533–1545 (2012). https://doi.org/10.1038/onc.2011.348
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/onc.2011.348
Keywords
This article is cited by
-
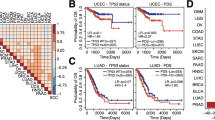
Influence of p53 Isoform Expression on Survival in High-Grade Serous Ovarian Cancers
Scientific Reports (2019)
-
High expression of the p53 isoform γ is associated with reduced progression-free survival in uterine serous carcinoma
BMC Cancer (2018)
-
Anti-proliferative activity of the NPM1 interacting natural product avrainvillamide in acute myeloid leukemia
Cell Death & Disease (2016)
-
Discovery and development of the Polo-like kinase inhibitor volasertib in cancer therapy
Leukemia (2015)
-
Molecular mechanisms of nutlin-3 involve acetylation of p53, histones and heat shock proteins in acute myeloid leukemia
Molecular Cancer (2014)