Abstract
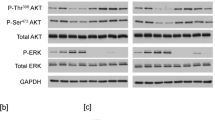
Receptor tyrosine kinase-mediated signaling is tightly regulated by a number of cytoplasmic signaling molecules. In this report, we show that Bcr–Abl transformed chronic myelogenous leukemia (CML) cell lines, K562 and Meg-01, express the receptor for nerve growth factor (NGF), TrkA, on the cell surface; however, the NGF-mediated signal is not particularly strong. Treatment with imatinib, a potent inhibitor of Bcr–Abl tyrosine kinase, downmodulates phosphorylation of downstream molecules. Upon stimulation with NGF, Erk and Akt are phosphorylated to a much greater degree in imatinib-treated cells than in untreated cells. Knockdown of expression of Bcr–Abl using small interfering RNA technique also enhanced NGF-mediated Akt phosphorylation, indicating that Bcr–Abl kinase modifies NGF signaling directly. Imatinib treatment also enhanced NGF signaling in rat adrenal pheochromocytoma cell line PC12 that expresses TrkA and c-Abl, suggesting that it is not only restoration of responsiveness to NGF after blocking oncoprotein activity, but also c-Abl tyrosine kinase per se may be a negative regulator of growth factor signaling. Furthermore, inhibition of Abl tyrosine kinase enhanced clearance of surface TrkA after NGF treatment and simultaneously enhanced NGF-mediated signaling, suggesting that as in neuronal cells ‘signaling endosomes’ are formed in hematopoietic cells. To examine the role of TrkA in CML cells, we studied cell growth or colony formation in the presence or absence of imatinib with or without NGF. We found that NGF treatment induces cell survival in imatinib-treated CML cell lines, as well as colony formation of primary CD34+ CML cells, strongly suggesting that NGF/TrkA signaling contributes to aberrant signaling in CML.
This is a preview of subscription content, access via your institution
Access options








Similar content being viewed by others
References
Blero D, De Smedt F, Pesesse X, Paternotte N, Moreau C, Payrastre B et al. (2001). The SH2 domain containing inositol 5-phosphatase SHIP2 controls phosphatidylinositol 3,4,5-trisphosphate levels in CHO-IR cells stimulated by insulin. Biochem Biophys Res Com 282: 839–843.
Bonati A, Carlo-Stella C, Lunghi P, Albertini R, Pinelli S, Migliaccio E et al. (2000). Selective expression and constitutive phosphorylation of SHC proteins in the CD34+ fraction of chronic myelogenous leukemias. Cancer Res 60: 728–732.
Bracci-Laudiero L, Celestino D, Starace G, Antonelli A, Lambiase A, Procoli A et al. (2003). CD34-positive cells in human umbilical cord blood express nerve growth factor and its specific receptor TrkA. J Neuroimmunol 136: 130–139.
Buchdunger E, Cioffi CL, Law N, Stover D, Ohno-Jones S, Druker BJ et al. (2000). Abl protein-tyrosine kinase inhibitor STI571 inhibits in vitro signal transduction mediated by c-kit and platelet-derived growth factor receptors. J Pharmacol Exp Ther 295: 139–145.
Buchdunger E, Zimmermann J, Mett H, Meyer T, Müller M, Druker BJ et al. (1996). Inhibition of the Abl protein-tyrosine kinase in vitro and in vivo by a 2-phenylaminopyrimidine derivative. Cancer Res 56: 100–104.
Burton EA, Plattner R, Pendergast AM . (2003). Abl tyrosine kinases are required for infection by Shigella flexneri. EMBO J 22: 5471–5479.
Butterfield JH, Weiler D, Dewald G, Gleich GJ . (1988). Establishment of an immature mast cell line from a patient with mast cell leukemia. Leuk Res 12: 345–355.
Chen Z-Y, Ieraci A, Tanowitz M, Lee FS . (2005). A novel endocytic recycling signal distinguishes biological responses of Trk neurotrophin recptors. Mol Biol Cell 16: 5761–5772.
Chevalier S, Praloran V, Smith C, MacGrogan D, Ip NY, Yancopoulos GD et al. (1994). Expression and functionality of the trkA proto-oncogene product/NGF receptor in undifferentiated hematopoietic cells. Blood 83: 1479–1485.
Deininger M, Buchdunger E, Druker BJ . (2005). The development of imatinib as a therapeutic agent for chronic myeloid leukemia. Blood 105: 2640–2653.
Druker BJ, Guilhot F, O’Brien SG, Gathmann I, Kantarjian H, Gattermann N et al. (2007). Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. New Eng J Med 355: 2408–2417.
Druker BJ, Sawyers CL, Kantarjian H, Resta DJ, Reese SF, Ford JM et al. (2001). Activity of a specific inhibitor of the Bcr–Abltyrosine kinase in the blast crisis of chronic myeloid leukemia and acute lymphoblastic leukemia with Philadelphia chromosome. N Engl J Med 344: 1038–1042.
Druker BJ, Tamura S, Buchdunger E, Ohno S, Segal GM, Fanning S et al. (1996). Effects of a selective inhibitor of the Abl tyrosine kinase on the growth of Bcr–Ablpositive cells. Nat Med 2: 561–566.
Feller SM . (2001). Crk family adaptors-signalling complex formation and biological roles. Oncogene 20: 6348–6371.
Giuriato S, Blero D, Robaye B, Bruyns C, Payrastre B, Erneux C . (2002). SHIP2 overexpression strongly reduces the proliferation rate of K562 erythroleukemia cell line. Biochem Biophys Res Commun 296: 106–110.
Heinrich MC, Griffith DJ, Druker BJ, Wait CL, Ott KA, Zigler AJ . (2000). Inhibition of c-kit receptor tyrosine kinase activity by STI 571, a selective tyrosine kinase inhibitor. Blood 96: 925–932.
Howe CL, Valletta JS, Rusnak AS, Mobley WC . (2001). NGF signaling from clathrin-coated vesicles: evidence that signaling endosomes serve as a platform for the Ras-MAPK pathway. Neuron 32: 801–814.
Huang EJ, Reichardt LF . (2003). Trk receptors: roles in neuronal signal transduction. Annu Rev Biochem 72: 609–642.
Kaebisch A, Brokt S, Seay U, Lohmeyer J, Jaeger U, Pralle H . (1996). Expression of the nerve growth factor receptor c-TRK in human myeloid leukaemia cells. Br J Haematol 95: 102–109.
Koch A, Mancini A, El Bounkari O, Tamura T . (2005). The SH2-domian-containing inositol 5-phosphatase (SHIP)-2 binds to c-Met directly via tyrosine residue 1356 and involves hepatocyte growth factor (HGF)-induced lamellipodium formation, cell scattering and cell spreading. Oncogene 24: 3436–3447.
Koch A, Mancini A, Stefan M, Niedenthal R, Niemann H, Tamura T . (2000). Direct interaction of nerve growth factor receptor, TrkA, with non-receptor tyrosine kinase, c-Abl, through the activation loop. FEBS letter 469: 72–76.
Mancini A, Koch A, Wilms R, Tamura T . (2002). c-Cbl associates directly with the C-terminal tail of the receptor for the macrophage colony-stimulating factor, c-Fms, and down-modulates this receptor but not the viral oncogene v-Fms. J Biol Chem 277: 14635–14640.
Matsuda H, Coughlin MD, Bienenstock J, Denburg JA . (1988). Nerve growth factor promotes human hemopoietic colony growth and differentiation. Proc Natl Acad Sci USA 85: 6508–6512.
Mulloy JC, Jankovic V, Wunderlich M, Delwel R, Cammenga J, Krejci O et al. (2005). AML1-ETO fusion protein up-regulates TRKA mRNA expression in human CD34+ cells, allowing nerve growth factor-induced expansion. Proc Natl Acad Sci USA 102: 4016–4021.
Muraille E, Pessese X, Kuntz C, Erneux C . (1999). Distribution of the src-homology-2-domain-containing inositol 5-phosphatase SHIP-2 in both non-haemopoietic and haemopoietic cells and possible involvement of SHIP-2 in negative signalling of B-cells. Biochem J 342: 697–705.
Obermeier A, Lammers R, Wiesmüller KH, Jung G, Schlessinger J, Ullrich A . (1993). Identification of Trk binding site for SHC and phosphatidylinositol 3′-kinase and formation of a multimeric signaling complex. J Biol Chem 268: 22963–22966.
O’Brien SG, Guilhot F, Larson RA, Gathmann I, Baccarani M, Cervantes F et al.. (2003). Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. New Eng J Med 348: 994–1004.
Rajagopal R, Chen ZY, Lee FS, Chao MV . (2004). Transactivation of Trk neurotrophin receptors by G-protein-coupled receptor ligands occurs on intracellular membranes. J Neurosci 24: 6650–6658.
Riccio A, Pierchala BA, Ciarallo CL, Ginty DD . (1997). An NGF-TrkA-mediated retrograde signal to transcription factor CREB in sympathetic neurons. Science 277: 1097–1100.
Sattler M, Mohi MG, Pride YB, Quinnan LR, Malouf NA, Podar K et al. (2002). Critical role for Gab2 in transformation by BCR/ABL. Cancer Cell 1: 479–492.
Saxena S, Howe CL, Cosgaya JM, Steiner P, Hirling H, Chan JR et al. (2005). Differential endocytic sorting of p75NTR and TrkA in response to NGF: a role for late endosomes in TrkA trafficking. Mol Cell Neurosci 28: 571–587.
Scheijen B, Griffin JD . (2002). Tyrosine kinase oncogenes in normal hematopoiesis and hematological disease. Oncogene 21: 3314–3333.
Scherr M, Battmer K, Blömer U, Schiedlmeier B, Ganser A, Grez M et al. (2002). Lentiviral gene transfer into peripheral blood-derived CD34+ NOD/SCID-repopulating cells. Blood 99: 709–712.
Scherr M, Battmer K, Schultheis B, Ganser A, Eder M . (2005). Stable RNA interference (RNAi) as an option for anti-bcr–abl therapy. Gene Therapy 12: 12–21.
Scherr M, Battmer K, Winkler T, Heidenreich O, Ganser A, Eder M . (2003). Specific inhibition of bcr–abl gene expression by small interfering RNA. Blood 101: 1566–1569.
Simone MD, De Santis S, Vigneti E, Papa G, Amadori S, Aloe L . (1999). Nerve growth factor: a survey of activity on immune and hematopoietic cells. Hematol Oncol 17: 1–10.
Snider WD . (1994). Functions of the neurotrophins during nervous system development: what the knockouts are teaching us. Cell 77: 627–638.
Stephens RM, Loeb DM, Copeland TD, Pawson T, Greene LA, Kaplan D . (1994). Trk receptors use redundant signal transduction pathways involving SHC and PLC-γ1 to mediate NGF response. Neuron 12: 691–705.
Tam S-Y, Tsai M, Yamaguchi M, Yano K, Butterfield JH, Galli SJ . (1997). Expression of functional TrkA receptor tyrosine kinase in the HMC-1 human mast cell line and in human mast cells. Blood 90: 1807–1820.
Tanos B, Pendergast AM . (2006). Abl tyrosine kinase regulates endocytosis of the epidermal growth factor receptor. J Biol Chem 281: 32714–32723.
Tuveson DA, Willis NA, Jacks T, Griffin JD, Singer S, Fletcher CD et al. (2001). STI571 inactivation of the gastrointestinal stromal tumor c-KIT oncoprotein: biological and clinical implications. Oncogene 20: 5054–5058.
von Bubnoff N, Peschel C, Duyster J . (2003). Resistance of Philadelphia-chromosome positive leukemia towards the kinase inhibitor imatinib (STI571, Glivec): a targeted oncoprotein strikes back. Leukemia 17: 829–838.
Wang WL, Healy ME, Sattler M, Verma S, Lin J, Maulik G et al. (2000). Growth inhibition and modulation of kinase pathways of small cell lung cancer cell lines by the novel tyrosine kinase inhibitor STI 571. Oncogene 19: 3521–3528.
Wisniewski D, Strife A, Swendeman S, Erdjument-Bromage H, Geromanos S, Kavanaugh WM et al. (1999). A novel SH2-containing phosphatidylinositol 3,4,5-trisphosphate 5-phosphatase (SHIP2) is constitutively tyrosine phosphorylated and associated with src homologous and collagen gene (SHC) in chronic myelogenous leukemia progenitor cells. Blood 93: 2707–2720.
Yano H, Cong F, Birge RB, Goff SP, Chao MV . (2000). Association of the Abl tyrosine kinase with the Trk nerve growth factor receptor. J Neurosci Res 59: 356–364.
Zhang Y, Moheban DB, Conway BR, Bhattacharyya A, Segal RA . (2000). Cell surface Trk receptors mediate NGF-induced survival while internalized receptors regulate NGF-induced differentiation. J Neurosci 20: 5671–5678.
Acknowledgements
We thank Regina Wilms and Sabine Klebba-Faerber for technical assistance, and Bruce Boschek for critically reading the paper. The research was supported by Sonderforschungsbereich 566 (B2 and A12), the Deutsche Forschungsgemeinschaft (Ta-111/8/-4, Ko-2249/3-1), MHH-HiLF program to AK, and HW and J Hector Stiftung to MS and ME.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koch, A., Scherr, M., Breyer, B. et al. Inhibition of Abl tyrosine kinase enhances nerve growth factor-mediated signaling in Bcr–Abl transformed cells via the alteration of signaling complex and the receptor turnover. Oncogene 27, 4678–4689 (2008). https://doi.org/10.1038/onc.2008.107
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/onc.2008.107
Keywords
This article is cited by
-
Inhibition of Tropomyosin Receptor Kinase A Signaling Negatively Regulates Megakaryopoiesis and induces Thrombopoiesis
Scientific Reports (2019)
-
Murine precision-cut liver slices (PCLS): a new tool for studying tumor microenvironments and cell signaling ex vivo
Cell Communication and Signaling (2014)
-
THOC5, a member of the mRNA export complex, contributes to processing of a subset of wingless/integrated (Wnt) target mRNAs and integrity of the gut epithelial barrier
BMC Cell Biology (2013)
-
Transcriptional regulation of immediate-early gene response by THOC5, a member of mRNA export complex, contributes to the M-CSF-induced macrophage differentiation
Cell Death & Disease (2013)
-
Imatinib mesilate-induced phosphatidylinositol 3-kinase signalling and improved survival in insulin-producing cells: role of Src homology 2-containing inositol 5′-phosphatase interaction with c-Abl
Diabetologia (2013)