Abstract
Objective:
Type 2 diabetes mellitus (T2DM) affects approximately 10% of Americans, while 79 million Americans are estimated to have glucose intolerance or prediabetes (pre-DM). The present study was designed to determine whether obese patients with pre-DM or T2DM would lose weight as effectively as obese normoglycemic patients, in a medically supervised high-protein, low-calorie-weight management program.
Method:
Patients enrolled in a self-paid, university-based, outpatient weight loss program using prescribed very-low-calorie diet (VLCD) (500–800 cal per day) or LCD diet (800–1200 cal per day), recommended exercise and group behavioral counseling were studied retrospectively. Patients entering the program for the first time and attending weekly clinic visits for more than 4 weeks were included in the analysis.
Results:
A total of 2093 obese patients, of whom 583 patients with pre-DM (fasting glucose ⩾100 and <126 mg dl−1), 367 patients with T2DM and 1143 normoglycemic patients entered the program from 1991 to 2010, who met all the inclusion criteria were included in the analysis. The body weight at baseline was 104.0±20.0 kg for DM, 101.4±18.4 for pre-DM and 99.0±18.8 kg for non-DM. Weight loss and percent of weight loss within 12 months were analyzed using a linear mixed-effects model. There was no significant difference in weight loss between DM vs non-DM (P=0.4597) and pre-DM vs non-DM (P=0.6006) in 12 months. The length of enrollment in the program was positively correlated to weight loss rates in all patients (P<0.001).
Conclusion:
This study demonstrates that obese, pre-DM and DM patients all lost weight as effectively with VLCD or LCD over 12 months. Given the impact of weight loss on the progression of comorbid conditions, these data support the hypothesis that medically supervised diets, including VLCD and LCD, should be more widely used in the prevention and treatment of obese patients with pre-DM or T2DM.
Similar content being viewed by others
Introduction
The most significant comorbid disease associated with the global epidemic of obesity is type 2 diabetes mellitus (T2DM). This epidemic is driven by abdominal visceral and hepatic excess fat and affects both overweight and obese patients. While obesity with a body mass index (BMI) >30 kg m−2 was recently declared a disease by the American Medical Association,1 many individuals around the world develop diabetes at a lower body mass index.2 In the United States, women at a BMI of 27 kg m−2 have an increased risk of T2DM, and the overall risk at a BMI of 30 kg m−2 is 3000% or 30-fold. Although heart disease, hypercholesterolemia, gallstones and other comorbid conditions have a four- to sixfold increased risk, T2DM is linked to obesity in an intimate way that is has been termed ‘Diabesity’.
It is now established that for 2–10 years, obese patients with pre-diabetes (pre-DM) put an extra burden on pancreatic beta-cells to secrete insulin, and to maintain or attempt to maintain euglycemia in the face of insulin resistance.3, 4 Two diabetes prevention studies in patients with hyperglycemia demonstrated that even a modest but labor-intensive lifestyle intervention resulting in a 5% weight loss prevented over half of new cases of diabetes in a 5-year period in comparison with a control group.5, 6 There have been publications supporting the concept that diet and lifestyle management should be the cornerstone of the prevention and treatment of T2DM7, 8 and reduce mortality in patients with T2DM and obesity.9 The NIH Look AHEAD trial examining the impact of weight loss on cardiovascular mortality in patients with T2DM demonstrated significant weight loss in 1 year using a combination of dietary counseling, modest exercise recommendations and meal replacements. There were three predictors of successful weight loss: (1) use of meal replacements; (2) physical activity and (3) recording dietary intake.10 Studies including a meta-analysis of weight loss interventions in adults with T2DM showed that multidisciplinary interventions including VLCD held promise for achieving weight loss.11, 12, 13, 14, 15 We have previously shown that meal replacements are safe and effective in patients with T2DM.16
Therapeutic weight loss in T2DM patients has been very difficult to achieve.17, 18 In practice, both primary care physicians and diabetes specialists focus on the control of hyperglycemia, while giving inadequate or no attention to weight management through changes in diet and lifestyle because of their belief that this is an exercise in futility.19 As a result, obese diabetic patients are increasingly referred for bariatric surgery, an expensive option with significant side effects and the necessity of long-term medical management.20 Recent meta-analysis reporting marked improvements in glycemic control in patients with T2DM after bariatric surgery at 1 year21 reinforce these views.
This retrospective analysis of data from 2093 patients was designed to examine the efficacy of diet, exercise and lifestyle intervention programs in producing weight loss in obese patients with pre-DM or diabetes in comparison with normoglycemic obese patients enrolled in the same outpatient program.
Patients and methods
Subjects
This was a retrospective chart review of 2093 patients who participated in the weight loss program at the UCLA Risk Factor Obesity Clinic between 1991 and 2010. The study was approved by the Institutional Review Board of University of California, Los Angeles. Patients who met the following inclusion and exclusion criteria were included in the analysis. Inclusion criteria were an age of at least 18 years but <65 years, and BMI of at least 25 kg m−2 but <45 kg m−2,2 enrolled in the program the first time and attended the weekly clinic visits at least for 4 weeks. Exclusion criteria were diagnosis of anorexia, binge eating disorder, bariatric surgery, adrenal insufficiency, myasthenia gravis, any chronic steroid use, any forms of cancer other than skin cancer and any kind of organ transplant.
The medically supervised meal replacement program
All study patients were enrolled in a medically supervised meal replacement weight management program (UCLA Risk Factor Obesity Program). The program has remained essentially the same since 1991. Participants were encouraged to attend seminars held during clinic hours including a series of weekly lectures and interactive meetings on diet, exercise and behavior modification. Dietitians and psychologists were available for consultation at each visit. Weight and vital signs were measured weekly and complete blood count and electrolytes were also recorded at baseline and at 2-week intervals. Every participant was seen on a bi-weekly basis by a physician to assess his/her success with the diet program, review laboratory tests, discuss any issues and adjust medications for any associated medical conditions and an exercise regimen, and also to participate in classes on behavior modification. Electrocardiograms were obtained at baseline and every 8 weeks and the QT interval was followed carefully. Bioelectrical impedance was measured every 8 weeks at the same time that an electrocardiogram was obtained. Target weights were estimated by bioelectrical impedance using preferred percent body fats based on age and gender, and discussed with patients.
Target calories were driven by desired rates of weight loss based on resting metabolic rate estimated using the Cunningham equation and fat-free mass (13.8 cal per day per pound fat-free mass). For the VLCD and LCD diet plans, specially prepared meal replacement products (R-Kane Inc., Pennsauken Township, NJ, USA) were used to provide between 500 and 1000 cal per day. Typical protein-rich powder formulas provided 100 cal with 15 g protein (60% protein, 40% carbohydrate), protein snack bars provided 150 cal and 10 g of protein, and soups provided 70 cal and 15 g of protein. All products were made with water or in some cases patients used sugar-free soft drinks. The protein was of high biological value including soy, casein and whey proteins. Patients were placed on combinations of five to eight servings per day of these products to reach their protein and calorie goals. In addition, after a period of time, many patients transitioned to a partial meal replacement program where four or five servings of meal replacements per day were combined with a defined meal of about 300 cal of lean protein and non-starchy vegetables. After the first 2 weeks in the program, patients were encouraged to exercise for 30 min per day and to add resistance exercise in those patients who were able to do so. Exercise was personalized based on the subject’s ability, inclinations and comorbid orthopedic conditions. Exercise was delayed for the first 2 weeks in the program when diuresis owing to calorie restriction routinely occurred increasing the risk of electrolyte imbalances. Serum potassium was followed bi-weekly and complete metabolic panels including tests of liver and renal function were obtained at 4-week intervals.
Statistical analysis
Summary statistics (mean, standard deviation and frequency distribution) were generated for demographic information and baseline clinical presentation to characterize the study population. Two-sample t-test, Wilcoxon’s test or analysis of variance was used to compare continuous variables, and χ2-test or Fisher’s exact test was used to compare categorical variables among T2DM and pre-DM and non-DM patients. Wilcoxon’s signed-rank test was used to evaluate the change of metabolic parameters from baseline to 6 and 12 months. To evaluate the association between weight loss and T2DM, or pre-DM, a repeated measurement mixed-effects model was used with the linear time trend to infer the average weight loss rate in the VLCD program. The fixed effects included time, T2DM, age, initial weight, sex, hypertension, hypothyroidism, obstructive sleep apnea, depression, low back pain, total number of comorbid conditions and interactions with time. For the random effect, autoregressive correlation was used to account for correlations of outcome within the same subject.
Results
Study population
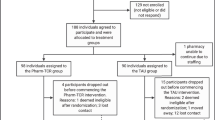
There were 3483 patients enrolled in our VLCD program between 1991 and 2010. A total of 2093 patients met the inclusion and exclusion criteria and were included in the analysis. There were 583 patients with pre-DM, 367 patients with DM and 1143 without DM (Figure 1). The baseline characteristics of the patients are demonstrated in Table 1. The mean age of all patients was 45.85±11.15, with BMI of 35.19±4.99 kg m−2. The pre-DM and DM patients were older, had higher body weight and higher percentage of male than the non-DM patients. More patients with DM had obesity-related chronic medical conditions of depression (P<0.0001), degenerative arthritis (P<0.0001), dyslipidemia (P=0.0132), hypertension (P=0.001), hypothyroidism (P<0.0001) and obstructive sleep apnea (P=0.0006).
The mean enrollment time for all patients in the clinic was 213.10±122.62 days. There were no statistical differences among the three groups (P=0.7440) (Table 2). The longer the patients enrolled in the weight loss program, the higher the average daily weight loss (Table 5). During the 12-month period, 51.08% of total patients attended the program for 6 months and 29.05% attended for 12 months. The retention rate for all the groups at any study time point during 12 months were the same (Table 2).
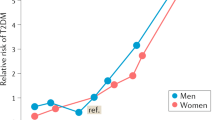
Effect of meal replacement program on body weight
The average mean total weight loss for all patients was 12.0±5.6 kg at 3 months, 15.6±8.4 kg at 6 months, 15.8±10.0 kg at 9 months and 14.4±10.2 kg at 12 months. The mean percent weight loss from baseline is shown in Figure 2. The percent weight loss from baseline for all patients was 9.88±4.33% at month 3, 15.35±8.18% at month 6, 15.08±10.23% at month 9 and 13.77±10.38% at month 12. These percent weight losses were not different in the pre-DM, T2DM or normoglycemic patients. Using mixed-model regression analysis, weight loss rates were not statistically different among the patients with pre-DM, DM and normoglycemia.
Effect of meal replacement program on body composition
Body composition was measured by bioimpedance analysis every 8 weeks at the same time that an electrocardiogram was obtained. The average mean body fat percent at baseline was 40.86±5.51 for pre-DM, 40.29±5.77 for DM and 39.23±5.60 for non-DM patients. The pre-DM and DM patients had statistically higher fat percentage than non-DM patients (P<0.0001 pre-DM vs non-DM, P<0.01 for DM vs non-DM) because of a lower fat-free mass. However, there was no significant difference in the reduction in percent fat among the above three groups of patients at any time point studied over the 12 months of participation in the program (see Table 3).
Age, gender and comorbidities on weight loss
In the analysis including all patients, aged 18–65 years, age was not a significant factor in weight loss rate (P=0.8138). However, female gender did affect rates of weight as being female was associated with 8.99±1.75 g greater average daily weight loss (P<0.0001) (Table 4). Neither pre-DM nor T2DM was associated with differences in rates of weight loss. Patients with hypertension, hypothyroidism and obstructive sleep apnea had significantly less weight loss over time (Table 4). Dyslipidemia and degenerative arthritis were associated with more weight loss (5.14±2.19 g, P=0.0192 for dyslipidemia; 10.07±3.53 g, P=0.0043 for degenerative arthritis), while depression had no impact on average daily weight loss rates (Table 4).
Changes in weight-related comorbidities
The patients with DM had higher systolic blood pressure at baseline (DM patients 125.01±22.56 mmHg vs non-DM patients 120.25±11.35 mmHg, P<0.001, vs pre-DM patients 122.77±15.22 mmHg, P<0.0001). There was significant reduction of systolic blood pressure at month 6 but not at month 12 for patients in all three groups. The diastolic blood pressure was significantly lowered for all patients at months 6 and 12 (Table 5).
The blood glucose level for DM patients at baseline was 118.60±51.82 mg dl−1, with a statistically significant average decrease of 8.39±29.77 mg dl−1 (P<0.0001) at month 6 and 6.29±26.73 mg dl−1 (P<0.05) at month 12. The blood glucose level at baseline for pre-DM patients decreased significantly at month 6 by 3.20±10.68 mg dl−1 (P<0.0001) and at month 12 by 2.21±17.36 mg dl−1 (P<0.05). The blood glucose level for non-DM patients increased at month 6 (1.61±14.21 mg dl−1, P<0.05) and no change at month 12. Compared with patients without DM, the patients with DM and pre-DM had significantly more blood glucose reduction at months 6 and 12 (P<0.000 at month 6, P<0.05 at month 12). In the mixed-effect model analysis the weight change was significantly associated with a change in blood glucose (P<0.0001) and there was no difference for the association between DM and pre-DM patients.
The baseline total cholesterol was comparable in all patients. The triglyceride level for DM patients was significantly decreased at month 6 by 37.55±76.13 mg dl−1 (P<0.001) but not at month 12, while pre-DM and non-DM patients had significant reduction at both months 6 and 12. The high-density lipoprotein-cholesterol level for patients in all three groups was significantly increased in association with weight loss, but without any significant difference among groups. There was a significant decrease of low-density lipoprotein at month 6 only for DM and non-DM patients at months 6 and 12 but no change for pre-DM patients (Table 5).
Discussion
Weight loss is often one of the first recommendations made to patients who have a new diagnosis of T2DM. However, therapeutic weight loss in T2DM patients has been very difficult to achieve and patients with T2DM have less success with maintaining their weight loss.19 Many of the medications traditionally used to control blood glucose in diabetics, including insulin, thiazolidinediones and sulfonylureas,22, 23, 24 can result in increased body fat over time. Among the above interventions, insulin is the one associated with the greatest amount of weight gain when used as monotherapy. Two of the largest studies to demonstrate this include the Diabetes Control and Complications Trial (DCCT) and United Kingdom Prospective Diabetes Study (UKPDS).25, 26 In the former study involving patients with T1DM, the intensive insulin group had an average weight gain of 4.6 kg more than those on conventional therapy.26 The latter study in T2DM also demonstrated a mean weight gain of 4 kg in the intensive group as compared with a diet-controlled treatment of DM. Insulin sensitizers such as thiazolidinediones and insulin secretagogues such as sulfonylureas also produce weight gain as monotherapy, but not to the same extent as that found with insulin.22, 27, 28
The effort to drive hemoglobin A1c down to prevent complications can reduce the effectiveness of weight management interventions. There is most likely no one specific reason why weight gain is an associated side effect of these hypoglycemic medications. Current proposed mechanisms include: (1) reduction of glycosuria resulting in retention of calories; (2) anabolic effects of insulin; (3) increased appetite; (4) decreased leptin production; and (5) fluid retention.19 Of these, increased appetite and reduction of glycosuria appear to have the greatest effect on weight gain. A reduction in basal metabolic rate has also been examined to explain weight gain with glycemic control. However, several studies investigating basal metabolic rate before and after therapy with insulin, thiazolidinediones or sulfonylurea have not been able to confirm a reduced basal metabolic rate as the cause for weight gain.29, 30, 31
Several studies reported significantly less weight loss in T2DM than in non-DM patients.32, 33, 34 Our study has tested the hypothesis that diabetes or pre-DM would lose weight less effectively than non-diabetic obese patients. It should be noted that all three groups have insulin resistance, while only the pre-DM and DM groups have abnormalities of insulin secretion. In a study explicitly designed to compare the weight loss of T2DM and non-DM with age- and weight-matched patients, Guare et al.35 found that obese T2DM patients can lose as much weight as controls during a 16-week behavioral weight loss program, but had difficulty maintaining their lost weight. In a more recent study, Baker et al.36 found near-identical weight change between DM vs non-DM patients in a 24-week VLCD weight loss clinical trial (diabetes: 8.5±1.3 kg vs control: 9.4±1.2 kg, P=0.64). In the current study, we have examined the weight loss of a large number of pre-DM, DM and non-DM patients in a real-world outpatient program and found VLCD to be clinically effective in inducing weight loss in patients with pre-DM and T2DM as in obese patients without diabetes.
Owing to the widely held perception that diets cannot produce and maintain adequate weight loss for pre-DM and DM patients, there has been increased interest in recommending bariatric surgery as the only practical weight loss modality for patients with T2DM. Our data demonstrate that pre-DM and DM patients can lose about 15% of initial body weight at 6 months and patients remaining in the program for 12 months maintained a 14% weight loss. One of the reasons that bariatric surgery has been preferred is that dietary adherence is viewed as uniformly poor. However, over 50% of the patients enrolled for 6 months and 30% of patients enrolled for 12 months were adherent in our medically supervised program. The diet program was well tolerated without metabolic complications or serious adverse events, and is an alternative to bariatric surgery for a significant subset of patients with obesity and hyperglycemia or T2DM.
Although VLCD has previously been shown to result in weight loss in patients with and without T2DM14, 37 and to induce rapid improvements in glycemia and dyslipidemia in patients with type 2 diabetes,15, 34 our study demonstrated beneficial changes in blood pressure, blood glucose and lipids. Most of our patients were taking medications for their T2DM and for comorbid medical conditions, and our practice protocols call for real-time adjustment of all the medications, especially hypoglycemic agents. The change of medications was not captured in the electronic data entry and we may have underestimated the effects of weight loss on glucose control as a result. Similarly, patients on statin drugs for hypercholesterolemia also discontinued their use of drugs when low-density lipoprotein-cholesterol levels declined below the optimal levels suggested by their doctors.
The limitations of the study include: retrospective study design; pre-DM and DM were defined by fasting blood glucose values instead of oral glucose tolerance test and hemoglobin A1c; lack of information on changes of medications over time.
Our results indicating successful weight loss can be achieved in patients with DM, but the approach to weight loss in obese diabetic patients will need to be more aggressive and comprehensive. A successful program requires more than educational sessions with dietitians and a manual of instruction on weight loss.17, 18 A comprehensive program with multidisciplinary team members engaged with patients on a regular basis can help a significant subset of obese T2DM patients to achieve a metabolically meaningful weight loss. Comparative effectiveness research initiatives to assess and identify those obese patients with pre-DM or DM who do not require bariatric surgery are needed.
References
American Medical Association. Obesity is a Disease. American Medical Association Annual Meeting; Chicago, IL, USA; 18 June 2013.
Hu FB . Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care 2011; 34: 1249–1257.
Perreault L, Pan Q, Mather KJ, Watson KE, Hamman RF, Kahn SE . Effect of regression from prediabetes to normal glucose regulation on long-term reduction in diabetes risk: results from the Diabetes Prevention Program Outcomes Study. Lancet 2012; 379: 2243–2251.
Tabak AG, Herder C, Rathmann W, Brunner EJ, Kivimaki M . Prediabetes: a high-risk state for diabetes development. Lancet 2012; 379: 2279–2290.
Gregg EW, Chen H, Wagenknecht LE, Clark JM, Delahanty LM, Bantle J et al. Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA 2012; 308: 2489–2496.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403.
Anderson JW, Kendall CW, Jenkins DJ . Importance of weight management in type 2 diabetes: review with meta-analysis of clinical studies. J Am Coll Nutr 2003; 22: 331–339.
Maggio CA, Pi-Sunyer FX . The prevention and treatment of obesity. Application to type 2 diabetes. Diabetes Care 1997; 20: 1744–1766.
Williamson DF, Thompson TJ, Thun M, Flanders D, Pamuk E, Byers T . Intentional weight loss and mortality among overweight individuals with diabetes. Diabetes Care 2000; 23: 1499–1504.
Wadden TA, West DS, Neiberg RH, Wing RR, Ryan DH, Johnson KC et al. One-year weight losses in the Look AHEAD study: factors associated with success. Obesity (Silver Spring, MD) 2009; 17: 713–722.
Amatruda JM, Richeson JF, Welle SL, Brodows RG, Lockwood DH . The safety and efficacy of a controlled low-energy ('very-low-calorie') diet in the treatment of non-insulin-dependent diabetes and obesity. Arch Intern Med 1988; 148: 873–877.
Henry RR, Gumbiner B . Benefits and limitations of very-low-calorie diet therapy in obese NIDDM. Diabetes Care 1991; 14: 802–823.
Norris SL, Zhang X, Avenell A, Gregg E, Brown TJ, Schmid CH et al. Long-term non-pharmacologic weight loss interventions for adults with type 2 diabetes. Cochrane Database Syst Rev 2005; 18, CD004095.
Capstick F, Brooks BA, Burns CM, Zilkens RR, Steinbeck KS, Yue DK . Very low calorie diet (VLCD): a useful alternative in the treatment of the obese NIDDM patient. Diabetes Res Clin Pract 1997; 36: 105–111.
Wing RR, Marcus MD, Salata R, Epstein LH, Miaskiewicz S, Blair EH . Effects of a very-low-calorie diet on long-term glycemic control in obese type 2 diabetic subjects. Arch Intern Med 1991; 151: 1334–1340.
Li Z, Hong K, Saltsman P, DeShields S, Bellman M, Thames G et al. Long-term efficacy of soy-based meal replacements vs an individualized diet plan in obese type II DM patients: relative effects on weight loss, metabolic parameters, and C-reactive protein. Eur J Clin Nutr 2005; 59: 411–418.
Milne RM, Mann JI, Chisholm AW, Williams SM . Long-term comparison of three dietary prescriptions in the treatment of NIDDM. Diabetes Care 1994; 17: 74–80.
Redmon JB, Reck KP, Raatz SK, Swanson JE, Kwong CA, Ji H et al. Two-year outcome of a combination of weight loss therapies for type 2 diabetes. Diabetes Care 2005; 28: 1311–1315.
Pi-Sunyer FX . Weight loss in type 2 diabetic patients. Diabetes Care 2005; 28: 1526–1527.
Heber D, Greenway FL, Kaplan LM, Livingston E, Salvador J, Still C . Endocrine and nutritional management of the post-bariatric surgery patient: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2010; 95: 4823–4843.
Maggard-Gibbons M, Maglione M, Livhits M, Ewing B, Maher AR, Hu J et al. Bariatric surgery for weight loss and glycemic control in nonmorbidly obese adults with diabetes: a systematic review. JAMA 2013; 309: 2250–2261.
Del PS, Pulizzi N . The place of sulfonylureas in the therapy for type 2 diabetes mellitus. Metabolism 2006; 55: S20–S27.
Fonseca V . Effect of thiazolidinediones on body weight in patients with diabetes mellitus. Am J Med 2003; 115 (Suppl 8A): 42S–48S.
Heller S . Weight gain during insulin therapy in patients with type 2 diabetes mellitus. Diabetes Res Clin Pract 2004; 65 (Suppl 1): S23–S27.
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998; 352: 837–853.
The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993; 329: 977–986.
Mori Y, Murakawa Y, Okada K, Horikoshi H, Yokoyama J, Tajima N et al. Effect of troglitazone on body fat distribution in type 2 diabetic patients. Diabetes Care 1999; 22: 908–912.
Patel J, Anderson RJ, Rappaport EB . Rosiglitazone monotherapy improves glycaemic control in patients with type 2 diabetes: a twelve-week, randomized, placebo-controlled study. Diabetes Obes Metab 1999; 1: 165–172.
Franssila-Kallunki A, Groop L . Factors associated with basal metabolic rate in patients with type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia 1992; 35: 962–966.
Makimattila S, Nikkila K, Yki-Jarvinen H . Causes of weight gain during insulin therapy with and without metformin in patients with Type II diabetes mellitus. Diabetologia 1999; 42: 406–412.
Welle S, Nair KS, Lockwood D . Effect of a sulfonylurea and insulin on energy expenditure in type II diabetes mellitus. J Clin Endocrinol Metab 1988; 66: 593–597.
Wing RR, Marcus MD, Epstein LH, Salata R . Type II diabetic subjects lose less weight than their overweight nondiabetic spouses. Diabetes Care 1987; 10: 563–566.
Jackson RA, Moloney M, Lowy C, Wright AD, Hartog M, Pilkington TR et al. Differences between metabolic responses to fasting in obese diabetic and obese nondiabetic subjects. Diabetes 1971; 20: 214–227.
Henry RR, Wallace P, Olefsky JM . Effects of weight loss on mechanisms of hyperglycemia in obese non-insulin-dependent diabetes mellitus. Diabetes 1986; 35: 990–998.
Guare JC, Wing RR, Grant A . Comparison of obese NIDDM and nondiabetic women: short- and long-term weight loss. Obes Res 1995; 3: 329–335.
Baker ST, Jerums G, Prendergast LA, Panagiotopoulos S, Strauss BJ, Proietto J . Less fat reduction per unit weight loss in type 2 diabetic compared with nondiabetic obese individuals completing a very-low-calorie diet program. Metabolism 2012; 61: 873–882.
Miura J, Arai K, Tsukahara S, Ohno M, Ikeda Y . The long term effectiveness of combined therapy by behavior modification and very low calorie diet: 2 years follow-up. Int J Obes 1989; 13 (Suppl 2): 73–77.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Li, Z., Tseng, Ch., Li, Q. et al. Clinical efficacy of a medically supervised outpatient high-protein, low-calorie diet program is equivalent in prediabetic, diabetic and normoglycemic obese patients. Nutr & Diabetes 4, e105 (2014). https://doi.org/10.1038/nutd.2014.1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nutd.2014.1
Keywords
This article is cited by
-
A high-protein total diet replacement alters the regulation of food intake and energy homeostasis in healthy, normal-weight adults
European Journal of Nutrition (2022)
-
Comparative effectiveness of a portion-controlled meal replacement program for weight loss in adults with and without diabetes/high blood sugar
Nutrition & Diabetes (2017)
-
Weight losses with low-energy formula diets in obese patients with and without type 2 diabetes: systematic review and meta-analysis
International Journal of Obesity (2017)