Abstract
Weight reduction may be necessary in patients with end-stage liver disease (ESLD) before liver transplantation. Although very low calorie diets (VLCDs) are a highly effective weight loss strategy, they risk inducing protein-calorie malnutrition, sarcopenia and hepatic encephalopathy in ESLD patients. We report for the first time on the use of VCLDs in ESLD. Two severely obese individuals with ESLD underwent a modified VLCD to become eligible for liver transplantation. Patients consumed four protein supplements and one lean meal daily, equivalent to 800 kilocalories (kcal) and were closely monitored during the diet period. Subject 1, a 46-year-old male with alcoholic cirrhosis, lost 44.1 kg after 28 weeks on a modified VLCD. Liver function and MELD (model for end-stage liver disease) scores improved and he currently does not require listing for transplantation. Subject 2, a 64-year-old female with non-alcoholic steatohepatitis, lost 39.7 kg after a 30-week modified VLCD. She is awaiting liver transplantation listing with a stable MELD score. VLCDs were well tolerated by both patients without adverse effects. In conclusion, under close medical supervision VLCDs in patients with ESLD can be safe and effective in reducing weight, facilitating liver transplantation listing, and possibly improving liver damage.
Similar content being viewed by others
Case series
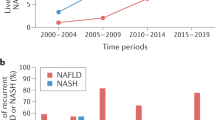
Obesity is a major risk factor for liver failure. Nonalcoholic fatty liver disease (NAFLD), the hepatic manifestation of insulin resistance, is increasing in prevalence in parallel with obesity and metabolic syndrome. Nonalcoholic steatohepatitis (NASH) is a subset of NAFLD characterized by inflammation and hepatic cell injury and is currently the third most common indication for liver transplantation in the United States.1 Obesity is also independently associated with the progression of fibrosis in patients with biopsy-confirmed NASH.1
Weight reduction is the established treatment for NAFLD. Some liver transplant programs consider severe obesity to be a relative contraindication to liver transplant because of the risk of complications.2 Consequently patients are sometimes required to lose weight before being placed on the transplant list. However, the optimal weight loss strategy for patients with ESLD is unknown. Surgical weight loss is effective but expensive and relatively high risk.1 Intensive medical weight loss strategies raise the risk of protein-calorie malnutrition, vitamin deficiencies and sarcopenia, especially in chronically ill-undernourished patients. Complicating matters is the lack of information about the ideal balance of macronutrients in ESLD. Low-protein diets are frequently used, although they may increase the risk of sarcopenia and worsen overall nutritional status.1 In contrast, high protein intake may trigger hepatic encephalopathy.
Very low calorie ketogenic diets (VLCDs) involve an intensive, nutritionally complete, carbohydrate-restricted regimen that is proportionally high in protein, typically provides between 700 and 800 kcal daily and causes large, rapid weight loss. Whether VLCDs are effective and tolerated in patients with ESLD has not been studied, perhaps because of their intensity and/or concerns about the amount of protein and calories provided. Here we report on two obese patients with ESLD who underwent a modified VLCD (800 kcal daily; 25% carbohydrates, 45% protein, 30% fat), using Robard Corporation products (Mt. Laurel, NJ, USA) and self-prepared food to become eligible for liver transplantation.
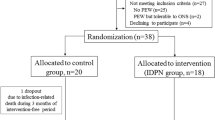
Two severely obese subjects independently scheduled a consultation for weight loss in order to become eligible for liver transplant listing, with a body mass index (BMI) end point <37 kg m−2. The treatment was performed in the author’s weight loss clinic as part of a standard clinical intervention, and therefore IRB approval was not obtained. However, both patients signed informed consent before starting VLCD therapy and also provided written permission for inclusion in a Case Study Report. ESLD in subject 1 was secondary to alcohol-related cirrhosis and in subject 2 was caused by nonalcoholic steatohepatitis. A comprehensive screening questionnaire and baseline testing were completed before their initial visit. Subjects agreed to comply with the nutritional intervention, regular physician follow-up visits and monitoring protocols.
Weight loss was achieved using a modified VLCD with partial meal replacements and a self-selected meal. Nutrimed medical VLCD products were used. The diet comprises ∼800 kcal per day (25% carbohydrates, 45% protein, 30% fat), with at least 75 grams of protein and all essential vitamins and nutrients. Subjects were advised to consume one Nutrimed supplement (15 gm protein bars, shakes/smoothies/soups) every 2–3 h for a total of four daily, and one lean meal consisting of two nonstarchy vegetables servings (∼4 ounces each) and one protein serving (∼4 ounces). Subjects consumed at least 2 l of water or noncaloric beverages and a multivitamin daily. Carbohydrate content was restricted to ⩽50 gm per day in order to limit calories and suppress appetite by inducing and maintaining a mild nutritional ketosis. Study subjects were provided with information describing what proteins and vegetables could be consumed for the lean meal.
The lifestyle intervention also involved activity recommendations and behavior modification. Exercise was recommended after the second week on the diet using both aerobic (cardio) and resistance (weights, bands) with a goal to work up to burning at least 2000 calories a week. Behavioral modification handouts were included as part of the VLCD program and were provided at every visit. Compliance was reinforced through self-monitoring records (weekly food and activity diaries), which were reviewed during the office visits.
Patient 1
Mr B is a 46-year-old male with a history of alcohol-related cirrhosis with portal hypertension, fatty liver, chronic kidney disease and severe obesity (see baseline characteristics in the Table 1). Mr B was placed on a modified VLCD and lost 44.1 kg (97 lb) after 28 weeks, without adverse side effects. He was then transitioned to a balanced diet. Liver function and MELD scores improved (see Table 1). He currently does not require listing for transplantation and is being followed medically. Six months post VLCD, Mr B has maintained his weight loss and is doing well.
Patient 2
Ms J is a 64-year-old female with decompensated cirrhosis from nonalcoholic steatohepatitis complicated by ascites and encephalopathy, severe obesity with remote gastric stapling, impaired fasting glucose and borderline chronic kidney disease. Characteristics before and after a 30-week modified VLCD are shown in the Table 1. Ms J lost 39.7 kg (87.4 lb) after 30 weeks on a modified VLCD and was then transitioned to a balanced nutritional plan. She tolerated the VLCD very well, had no adverse side effects and is awaiting liver transplantation listing. Her MELD score is stable. Little change in her body composition percentages was seen, which may have been related to the presence of ascites, which interferes with bioelectrical analysis (BIA) of body composition.
The VLCD is a promising weight loss strategy to treat patients with advanced liver disease, particularly fatty liver, a process initiated by intrahepatic triglyceride accumulation.3 Carbohydrate-restricted ketogenic diets such as the VLCD promote weight loss, reduce intrahepatic triglyceride levels and improve serum glucose, triglycerides and insulin sensitivity.3, 4 Hepatic ketogenesis also maintains hepatic redox balance and prevents the accumulation of fatty acid intermediates.3 Studies in patients before bariatric surgery demonstrate significant decreases in mean liver volume and hepatic fat with a VLCD intervention.5 Because excess calories, saturated and trans-fats, and fructose are also steatogenic,6 VLCDs offer additional advantages beyond simple carbohydrate restriction, including reducing total calories and fat and emphasizing high-quality protein to optimize nutritional status during intensive weight loss. In addition, meal replacements (high protein bars or shakes) promote significantly greater and sustainable weight loss, compared with self-selected calorie-controlled diets.7, 8 Moreover, higher protein intake increases satiety and produces a favorable thermogenic effect,9, 10 further enhancing weight loss.
Weight loss may be especially important in obese patients with cirrhosis to improve eligibility for transplantation. As obesity is associated with serious operative risks, many severely obese patients are considered ineligible for transplantation.11 Bariatric surgery in severely obese patients with decompensated liver disease is controversial and extremely high risk, limiting its use. VLCD intervention requires experience and frequent patient monitoring, but when part of a comprehensive lifestyle program it induces significant and sustainable weight loss and clinical resolution of co-morbidities without the downsides of surgery. A notable aspect of our report is that the VLCD was very well tolerated (and adhered to) by individuals with ESLD. Neither subject had any associated adverse effects during weight loss. No major changes in biochemical markers occurred during the study period that is not reflected in the Table 1. However, this is a very small case series, and further study in larger cohorts is warranted.
In conclusion, if undertaken with close medical supervision a VLCD may offer important weight loss and other significant health benefits to obese patients with ESLD.
References
Watt KD . Reducing the load: The evolution and management of obesity and nonalcoholic steatohepatitis before liver transplantation. Liver Transpl 2012; 18: S552–S558.
Dick AAS, Spitzer AL, Seifert CF, Deckert A, Carithers RL, Reyes JD et al. Liver transplantation at the extremes of body mass index. Liver Transpl 2009; 15: 968–977.
Schuger RC, Crawford PA . Low-carbohydrate ketogenic diets, glucose homeostasis, and nonalcoholic fatty liver disease. Curr Opin Nutr Metab Care 2012; 15: 374–380.
Sumithran P, Proietto J . Ketogenic diets for weight loss: A review of their principles, safety and efficacy. Obes Res Clin Pract 2008; 2: 1–13.
Lewis MC, Phillips ML, Slavotinek JP, Kow L, Thompson CH, Toouli J . Change in liver size and fat content after treatment with Optifast® Very Low Calorie Diet. Obes Surg 2006; 16: 697–701.
Sullivan S . Implications of diet on nonalcoholic fatty liver disease. Curr Opin Gastroenterol 2010; 26: 160–164.
Li Z, Bowerman S, Heber D . Meal replacement: a valuable tool for weight management. Obes Manag 2006; 2: 23–28.
Casazza K, Fontaine KR, Astrup A, Birch LL, Brown AW, Bohan Brown MM et al. Myths, presumptions, and facts about obesity. N Engl J Med 2013; 368: 446–454.
Bray GA, Smith SR, de Jonge L, Xie H, Rood J, Martin CK et al. Effect of dietary protein content on weight gain, energy expenditure, and body composition during overeating: a randomized controlled trial. JAMA 2012; 307: 47–55.
Li Z, Heber D . Overeating and overweight: Extra calories increase fat mass while extra protein increases lean mass. JAMA 2012; 307: 86–87.
Rafiq N, Younossi ZM . Effects of weight loss on nonalcoholic fatty liver disease. Semin Liver Dis 2008; 28: 427–433.
Acknowledgements
We thank both study subjects, who provided written permission for publication of this case report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Temmerman, J., Friedman, A. Very low calorie ketogenic weight reduction diet in patients with cirrhosis: a case series. Nutr & Diabetes 3, e95 (2013). https://doi.org/10.1038/nutd.2013.36
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nutd.2013.36
Keywords
This article is cited by
-
Very-low-calorie ketogenic diet (VLCKD) in the management of metabolic diseases: systematic review and consensus statement from the Italian Society of Endocrinology (SIE)
Journal of Endocrinological Investigation (2019)
-
Diete chetogeniche: ruolo nel trattamento di sovrappeso e obesità
L'Endocrinologo (2017)