Abstract
Introduction:
Although body fat and body fat distribution are known to be related to cardiovascular diseases (CVDs), it is unknown whether specific 30-year developmental patterns of body fat are associated with CVDs. This study examines the existence of distinct developmental patterns of total fat measured by the sum of four skinfolds (S4SFs) and body fat distribution measured by the skinfold thickness ratio (SFratio), and relates these patterns to micro- and macrovascular functions.
Methods:
In 2006, 259 apparently healthy subjects were examined on micro- and macrovascular functions, using video microscopy and carotid ultrasound sonography. Body fat, using both S4SFs and SFratio, was measured for 10 times over 30 years, from 13 years onwards. Latent class growth analyses (LCGA) were used to obtain distinct developmental patterns of S4SFs and SFratio. This is a data-drive hypothesis-generating approach and could possibly give a new perspective on body fatness over time. In addition, a mixed-method approach is used to obtain individual growth parameters. Linear regression analyses were used to examine the relationship of these patterns and individual growth parameters with micro- and macrovascular functions.
Results:
LCGA identified normal and unfavourable developmental patterns in S4SFs and SFratio. Both men and women with an unfavourable developmental pattern of S4SFs showed impaired carotid compliance (β=−0.216, P=0.004 and β=−0.109, P=0.039, respectively), carotid distensibility (β=−5.078, P=0.001 and β=−5.118, P<0.001, respectively) and Young’s elastic modulus (β=0.066, P=0.065 and β=0.107, P<0.001, respectively). In contrast, no relationship for microvascular function with developmental patterns of S4SFs was found. Developmental patterns of the SFratio were associated with neither measures of micro- nor macrovascular functions. No associations were using the individual growth parameters.
Conclusions:
For macrovascular function, there is a relationship of 30-year developmental patterns of S4SFs, whereas no such relationship was found for the 30-year developmental patterns of S4SFs or SFratio with microvascular function.
Similar content being viewed by others
Introduction
The epidemic proportions of obesity or high body fat are widely recognized.1 One of the main negative effects of high body fat is the development of cardiovascular disease (CVD). Even in apparently healthy adults, high body fat and a central pattern of body fat is cross-sectionally associated with microvascular and macrovascular functions.2,3 Fat-induced changes in microvascular function are hypothesized to affect insulin sensitivity and peripheral resistance, which may cause diabetes and hypertension.3, 4 On a macrovascular level, fat-induced changes are hypothesized to affect local and regional vessel wall stiffness parameters, which may adversely have an impact on atherosclerosis development and cardiac afterload. Both changes in micro- and macrovascular functions are regarded as early markers of vascular dysfunction, which can appear in relatively healthy subjects.3, 4 Despite several studies,5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 the association, if any, between particular developmental patterns of body fat and vascular dysfunction is unknown.
A relatively new explorative method for identifying developmental patterns of, for example, body fat is latent class growth analyses (LCGAs).14 To the best of our knowledge, it is unknown whether distinct developmental patterns of body fat are associated with micro and macrovascular perturbations. Therefore, in the current study, the presence of distinct 30-year developmental patterns (from 13 to 42 years of age) of body fat is examined. The main aim of the study is to examine the potential association of such distinct developmental patterns in relation to both micro- and macrovascular functions.
Subjects and methods
Study population
The observational Amsterdam Growth and Health Longitudinal Study started in 1977 and initially consisted of ∼600 boys and girls of the age of 13 years.15 Over the last 30 years, 10 follow-up visits have taken place in 1977, 1978, 1979, 1980, 1985, 1991, 1993, 1996, 2000 and 2006. These have resulted in the current database including anthropometric (body height, body weight and skinfold thickness) and biological parameters (serum sample parameters and blood pressure). The study is described elsewhere in detail.15 In the most recent round of measurement, when subjects reached the age of 42 years, microvascular function and large artery properties were assessed in 344 subjects in addition to the regular measurements. The study was approved by the medical ethics committee of the VU University Medical Center, and all subjects gave their written informed consent. Only participants who completed at least three measurement rounds were included, and participants using cardiovascular-related medication (N=7) were excluded from further analyses.
Body fat and body fat distribution
In the Amsterdam Growth and Health Longitudinal Study, body fat and body fat distribution are operationalized in different ways. Body mass index was calculated with weight and height, using standard equipment. The thickness of the sum of four skinfolds (S4SFs) was calculated by summing the thickness of the biceps, triceps, subscapular and suprailiac skinfolds. The skinfold thickness ratio (SFratio) is used as an indicator of body fat distribution and is defined as the subscapular plus the suprailiac skinfold thicknesses divided by the biceps plus the triceps skinfold thicknesses. Central body fat solely is defined as the subscapular and the suprailiac skinfolds taken together. A Holtain calliper was used (Holtain, London, UK).16
Microvascular function
A nailfold capillary videomicroscopy (Capiscope, KK Technologies, Devon, UK) was used to measure microvascular function. Capillaries were visualized in the nailfold of the dorsal skin of the third finger with a system magnification of × 100. With this technique, all capillaries that are erythrocyte perfused (capillary density) are visualized. For all subjects, two separate fields of 1 mm2 were recorded on videotapes. Per field, both baseline perfusion and peak reactive hyperaemia were measured. At first, baseline capillary density was visualized by counting capillaries that were constantly perfused during 15 s in resting state. With counting of the maximal number of perfused capillaries after 4 min of arterial occlusion (300 mm Hg), peak reactive hyperaemia was measured. Microvascular recruitment was calculated as the peak reactive hyperaemia minus the baseline perfusion. All measurements were separated with a 5-min rest period and the capillary density was reported as the number of perfused capillaries per mm2.
Restricting conditions to measure microvascular parameters in participants were a minimum hand temperature of 28 °C, fasting state and at least 30 min rest before the measurement was taken, as this could possibly affect microvascular perfusion.
Reproducibility of the microvascular parameters were tested using intraclass correlation coefficients. In our hands, the intraobserver intraclass correlation coefficients of capillary density counts during baseline and after 4 min of arterial occlusion were 0.97 and 0.96, and the interobserver intraclass correlation coefficients were 0.86 and 0.90, respectively.
Macrovascular function
Macrovascular function was obtained with ultrasound sonography. The ultrasound scanner (Wall track system 2; Pie Medical, Maastricht, The Netherlands) was used to measure carotid and femoral artery capacities. The standardized procedures to obtain artery capacities for the estimation of macrovascular function are described elsewhere in detail.17 Carotid diameter (D), distension (ΔD), Intima Media Thickness (IMT) and carotid and femoral pulse wave transit (TT) were measured. Moreover, scores were calculated for distensibility (DC; (2ΔD × D+2ΔD2)), compliance (CC; (π × (2D × ΔD+ΔD2)) and the Young's elastic modulus (D/(IMT × DC) as well. DC reflects elastic properties and CC reflects a buffering capacity given at a local pulse pressure. Both of these are local parameters, which accounts for the fact that the higher the value, the more stiff the arteries are. Young’s elastic modulus represents local arterial elasticity. Note that the higher the Young’s elastic modulus, the less elastic the arteries are. Furthermore, using both carotid and femoral capacities, pulse-wave velocity as a regional estimate of arterial stiffness is calculated as the carotid–femoral distance or the carotid to femoral pulse-wave transit.
Reproducibility of macrovascular parameters was tested in 200617. In our hands, the interobserver coefficients of variation were 2.7% for the carotid and 4.9% for the femoral diameter properties. For distension properties, the coefficients of variation were 9.5% for carotid and 28.3% for femoral properties. For carotid IMT, a coefficient of variation of 6.2% was found.
Covariates
Systolic blood pressure (SBP) was measured at 5 min intervals, during 60 min, in a supine position with an automated device (Dinamap Procare 100, GE Healthcare, Solingen, Germany). Several fasting blood parameters, such as glucose, insulin, high-density lipoprotein–cholesterol and triglyceride levels were measured by enzymatic or hexokinase techniques (Roche Diagnostics, Mannheim, Germany). Homeostatic model assessment-insulin resistance (HOMA-IR) as a measure of insulin sensitivity was calculated as glucose (mmol l−1) × insulin (mU l−1)/22.5.
Retrospective information on known family history of diabetes and cardiovascular events, medication use and smoking were obtained with validated questionnaires.
Statistical analyses
Statistical analyses were divided into two steps. In the first step, an LCGA analysis was performed for the four indicators of body fat: S4SF, SFratio and body mass index. The aim of the LCGA analysis is to model heterogeneity by identifying an unspecified number of groups on the basis of a similar developmental pattern.14, 18, 19 A piecewise model is computed by using a linear intercept and slope over time, and allowing for different phases in development (that is, additive unique intercept and slope over the three phases) in adolescence (1977–1980), 20s (1985–1993) and 30s (1996–2006). Time differences between the rounds of measurement are taken into account. The model is considered optimal when individuals are most alike within one subgroup and most different between subgroups. To determine the optimal number of groups, a ‘forward’ approach was taken, starting with a model with one group, implying that all individuals in the study had the same developmental pattern. Subsequently, one group at a time was added and the model fit was assessed by the Bayesian Information Criterion.20 After each step of adding a new group, the model fit was considered better if the Bayesian Information Criterion decreased. The final number of groups was derived not only on the basis of model fit but also on clinically relevant differences between the groups. Thus, if addition of a new group led to a clinically indistinguishable developmental pattern in a model, the model was considered not to be improved.20 The LCGA analyses were conducted with Mplus 5.21.21 In the second step, linear regression analyses were performed, in which the relationship between class membership and vascular function was examined. After a crude model, which depicts the mean difference between the groups and indicates significance of this difference, multivariate analyses allows for the examination of potential mediators such as SBP, high-density lipoprotein, triglyceride and HOMA-IR. Further adjustment was made for the potential confounders smoking, and also for retrospective information on known family history of diabetes and cardiovascular events.
In addition, the relationship between the individual growth parameters and the micro- and macrovascular outcomes were analysed with a cross-sectional linear regression analysis. To obtain these individual growth parameters, a mixed model analysis was performed, in which a linear function with time was used to analyse the development of body fat indicators over time and in which both a random intercept and random slope were added to the model. From this linear development, two individual growth parameters were obtained, that is, the mean value (or intercept) and the linear slope over time. The mixed-models analyses were performed in MLwiN 2.27 (Centre for Multilevel Modelling, Bristol, UK).
Linear regression analyses were performed in PASW statistics 18.0. All analyses were performed separately for men and women.
Results
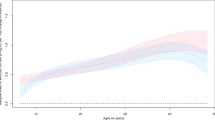
Table 1 shows descriptive information of the variables used in the present study and Figure 1 shows the distinct developmental patterns of S4SFs and SFratio. Central body fat solely is highly correlated (r=0.96 for men and r=0.94 for women) with total body fatness and, therefore, is not analysed separately. On the basis of the model fit (Table 2) indicators and clinical relevance, the final model for both S4SFs and SFratio were two-class solutions, for both men and women. For these models, the developmental pattern that was most similar to ‘normal’ growth, as observed in previous studies,5, 6, 7, 8, 9, 10, 11, 12, 13 was considered to be favourable (solid lines) and the distinct developmental pattern was considered to be unfavourable (dashed lines). For body mass index, a one-class solution was found to be the best. A two-class model for body mass index lead to overlapping developmental patterns, whereas a three-class model lead to very small and partly overlapping developmental patterns with only six men and eight women in the added class.
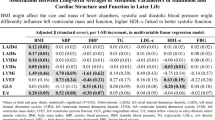
Table 3 (men) and Table 4 (women) show the results of the linear regression analyses to examine the relationship between class membership (independent) and vascular function (dependent). In crude analysis for both men and women, carotid compliance and carotid distensibility were significantly different between the two S4SF patterns. Only in women, the Young’s elastic modulus differed significantly between the two developmental patterns of S4SFs, while IMT differed significantly between the two developmental patterns of SFratio. For all relationships as found in the current study, subjects in the clinically less-favourable pattern showed unfavourable macrovascular function. However, examining potential mediators attenuated the relationships in such a way that they were not significant anymore. SBP was the most important mediator explaining on average 49% and 45% of the relationships between class membership and macrovascular function in men and women, respectively. HOMA-IR was the next important mediator explaining on average 14% and 25% of these relationships for men and women, respectively. For example, the difference between the univariate analysis examining carotid distensibility and class membership in women shows β=−5.118, whereas the multivariate model for this relationship shows β=−2.647, which is a difference of almost 50%. Therefore, biological risk factors and most pronounced SBP and HOMA-IR can partly explain the relationship, as presented in Tables 3 and 4, between class membership and macrovascular function. Further adjustment for smoking and retrospective information on known family history of CVD and diabetes did not alter these relationships (data not shown).
For microvascular function, no significant relationship was found with developmental patterns of either S4SFs or SFratio.
Table 5 shows the results of the analyses using individual growth parameters of S4SFs and SFratio. These analyses show no significant relationship with either micro- or macrovascular function.
Discussion
In the present study, we found that an unfavourable 30-year developmental pattern of total body fat was associated with macrovascular function, but not with microvascular function. The specific 30-year developmental patterns of body fat distribution, on the other hand, were not associated with either macro- or microvascular function. We further found that the relationship between the development of body fatness and macrovascular function was highly mediated by SBP.
In the present study, a relatively new statistical technique was used to classify subjects into different development patterns for both total body fat and body fat distribution. This is a hypothesis-generating technique that identifies distinct developmental patterns over time, without a priori characteristics of this difference. It was shown that the two patterns found for total body fat started to differ from each other around the age of 20 years, whereas the two patterns found for body fat distribution started to differ from each other around the age of 30 years. Furthermore, it was shown that although two different patterns were found for body fat distribution, the two patterns did not differ much from each other. This is also probably the reason why we did not find any relationship between body fat distribution with either micro- or macrovascular function, except for IMT in women, although in the literature body fat distribution seems to be more important in relation to CVD risk compared with total body fat.17, 22, 23
A comparison of the currently used LCGA analyses (Tables 3 and 4) with the more conventional approach using individual growth parameters shows some differences. Where no associations were observed with individual growth parameters, two distinct developmental patterns differed in macrovascular function. The LCGA analysis is a data-driven approach that helps in generating a hypothesis. One of the advantages of using developmental trajectories is that these trajectories combine the slope and the average value into one pattern, whereas these are separated in the approach using individual growth parameters.
The association of total body fat with macrovascular function is attenuated after examining the potential mediation for biological risk factors, by adding variables such as SBP and HOMA-IR, which on average account for about 14% and 45%, respectively, of the explained variance in men and 25% and 49%, respectively, in women. When both are added to the regression model, >50% of the relationships were explained. This was more or less expected, because both SBP and HOMA-IR are known to be associated with macrovascular dysfunction.2, 3, 4
In previous studies, body fat was found to be associated with both microvascular2, 4, 23, 24 and macrovascular functions.3, 13, 25 The current study could only confirm the association with macrovascular function. In the present study, three possible explanations as to why macrovascular function was associated with body fat and microvascular function was not may lie in the mechanism behind detrimental effects of body fat. First, the exchange of gases, nutrients and metabolites between the blood and tissues occurs almost exclusively at the level of the capillaries, and an adequate function of the capillaries, therefore, is essential for tissue and organ function. Given this important function of capillaries, it could be hypothesized that it may be important to protect capillary function. A protection mechanism of the capillaries that is alike is described in normal physiological responses such as the venoarteriolar reflex, protecting the lower extremities from increased pressure after standing up from a sitting position, or the myogenic response, as a response to increased resistance in arterioles, both of which serve to protect the capillaries from severe increases in pressure and, which, in turn, could increase proximal blood pressure.26, 27 In concordance with such a hypothesis, normal physiological responses, such as the prolonged hypertension, may be maintained. Thus, the luminal narrowing induced by the myogenic response may be maintained by a form of remodelling in which the vessel-wall components are rearranged without growth, known as eutrophic inward remodelling.27, 28 Initially, this remodelling was considered to protect the capillaries from increased pressures, but later on it may be instrumental in causing microvascular rarefaction, owing to increased systemic resistance, that subsequently reduces the number of capillaries. In fact, the microcirculation, as an important site for pressure dissipation, is part of a vicious cycle that maintains and amplifies high blood pressure if it is not treated adequately.23, 29 The population in the present study has no such levels of blood pressure or increased peripheral resistance and, therefore, may not have entered this vicious circle. Second, microvascular function may be more influenced by the perivascular adipose tissue than by the systemic adipose tissue depots.30 The methods to obtain estimates of body fat in the present study are indicators of the systemic adipose tissue and are therefore less related to microvascular function.30 Third, and in addition to the previous explanation, the methods to measure the central and peripheral body fat have some limitations. The currently used methods are well known in epidemiological research; however, these non-invasive measures cannot fully replace the idea of visceral and ectopic fat, which are identified to be harmful in experimental research.30 Using only non-invasive measures, it is simply impossible to separate the ectopic part from the visceral part. Previous research using high central fat over peripheral fat, however, had shown associations of these measures of body fat with CVD.1, 2, 3, 4, 6, 17
This study has some limitations. At first, the study population is an apparently healthy cohort, which means none of the subjects in this population have clinical levels of micro- and macrovascular functions.4, 31 Besides this, some of the microvascular parameters might not be influenced by the body fat levels within the healthy range, while more morbid levels of body fat could affect these parameters. Furthermore, the measures used in this study are not gold standard, but were invented with the intention to non-invasively measure body fat parameters in population studies.16
In conclusion, in healthy subjects there was no relationship between life-course developmental patterns of total body fat and body fat distribution and microvascular function. In contrast, there was a relationship between life-course developmental patterns of total body fat and macrovascular function, which is largely explained by increased blood pressure and decreased insulin sensitivity. This relationship was not found for the developmental patterns of body fat distribution.
References
Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet 2011; 377: 557–567.
Czernichow S, Greenfield JR, Galan P, Bastard JP, Charnaux N, Samaras K et al. Microvascular dysfunction in healthy insulin-sensitive overweight individuals. J Hypertens 2010; 28: 325–332.
Ferreira I, Van De Laar RJ, Prins MH, Twisk JW, Stehouwer CD . Carotid stiffness in young adults: a life-course analysis of its early determinants: the Amsterdam Growth and Health Longitudinal Study. Hypertension 2012; 59: 54–61.
De Jongh RT, Serné EH, IJzerman RG, Jørstad HT, Stehouwer CDA . Impaired local microvascular vasodilatory effects of insulin and reduced skin microvascular vasomotion in obese women. Microvasc Res 2008; 75: 256–262.
Adair LS . Child and adolescent obesity: epidemiology and developmental perspectives. Physiol Behav 2008; 94: 8–16.
Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C et al. Being big or growing fast: systematic review of size and growth in infancy and later obesity. Br Med J 2005; 331: 929.
Barker SJP, Osmond C, Forsén TJ, Kajantie E, Eriksson JG . Trajectories of growth among children who have coronary events as adults. N Engl J Med 2005; 353: 1802–1809.
Ferraro KF, Thorpe RJ, Wilkinson JA . The life course of severe obesity: does childhood overweight matter? J Gerontol Ser B Psychol Sci Soc Sci 2003; 58: S110–S119.
Huang D, Brecht M-L, Hara M, Hser Y-I . Influences of a covariate on growth mixture modeling. J Drug Issue 2010; 40: 173–194.
Nonnemaker JM, Morgan-Lopez AA, Pais JM, Finkelstein EA . Youth BMI trajectories: evidence from the NLSY97. Obes Silver Spring Md 2009; 17: 1274–1280.
Ostbye T, Malhorta R, Landerman LR . Body mass trajectories through adulthood: results from the National Longitudinal Survey of Youth 1979 Cohort (1981–2006). Int J Epidemiol 2011; 40: 240–250.
Pryor LE, Tremblay RE, Boivin M, Touchette E, Dubois L, Genolini C et al. Developmental trajectories of body mass index in early childhood and their risk factors: an 8-year longitudinal study. Arch Pediatr Adolesc Med 2011; 165: 906–912.
Tirosh A, Shai I, Afek A, Dubnov-Raz G, Ayalon N, Gordon B et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med 2011; 364: 1315–1325.
Nagin DS, Odgers CL . Group-based trajectory modelling in clinical research. Ann Rev Clin Psychol 2010; 6: 109–138.
Wijnstok NJ, Hoekstra T, Van Mechelen W, Kemper HCG, Twisk JWR . Cohort profile: the Amsterdam Growth and Health Longitudinal Study. Int J Epidemiol 2013; 42: 422–429.
Weiner J, Lourie J . A Guide to Field Methods, Handbook Number 9. Blackwell Science Inc: Oxford, 1986.
Schouten F, Twisk WR, De Boer MR, Stehouwer CDA, Serné EH, Smulders YMJ et al. Increases in central fat mass and decreases in peripheral fat mass are associated with accelerated arterial stiffening in healthy adults: the Amsterdam Growth and Health Longitudinal Study. Am J Clin Nutr 2011; 94: 40–48.
Jung T, Wickrama KAS . An introduction to latent class growth analysis and growth mixture modeling. Soc Personal Psychol Comp 2008; 2: 302–317.
Muthén BO, Muthén LK . Integrating person-centered and variable centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exper Res 2000; 24: 882–891.
Nylund K, Asparouhov T, Muthén BO . Deciding on the number of classes in latent class analysis and growth mixture modelling: A Monte Carlo Simulation Study. Struct Equati Model 2007; 14: 535–569.
Muthén LK, Muthén BO . Mplus User’s Guide Seventh edition Los Angeles, CA, 2012.
Mitchell G, Vita J, Larson M, Parise H, Keyes M, Warmer E, Vasan R et al. Cross-sectional relations of peripheral microvascular function, cardiovascular disease risk factors, and aortic stiffness. Circulation 2005; 112: 3722–3728.
Levy BI, Ambrosio G, Pries AR, Struijker-Boudier HAJ . Microcirculation in hypertension: a new target for treatment? Circulation 2001; 104: 735–740.
Serné EH, Stehouwer CDA, Ter Maaten JC, Ter Wee PM, Rauwerda JAA, Donker AJMJ et al. Microvascular function relates to insulin sensitivity and blood pressure in normal subjects. Circulation 1999; 23: 896–902.
Strandberg TE, Strandberg AY, Salomaa VV, Pitkälä KH, Tilvis RS, Sirola J et al. Explaining the obesity paradox: cardiovascular risk, weight change, and mortality during long-term follow-up in men. Eur Heart J 2009; 30: 1720–1727.
Hassan AA, Tooke JE . Mechanism of the postural vasoconstrictor response in the human foot. Clin Sci 1988; 75: 379–387.
Feihl F, Liaudet L, Waeber B, Levy BI . Hypertension: a disease of the microcirculation? Hypertension 2006; 48: 1012–1017.
Park JB, Schiffrin EL . Small artery remodeling is the most prevalent (earliest?) form of target organ damage in mild essential hypertension. J Hypertens 2001; 19: 921–930.
Struijker-Boudier HAJ, Heijnen BFJ, Liu Y-P, Staessen JA . Phenotyping the microcirculation. Hypertension 2012; 60: 523–527.
Yudkin JS, Eringa E, Stehouwer CDA . ‘Vasocrine’ signalling from perivascular fat: a mechanism linking insulin resistance to vascular disease. Lancet 2005; 365: 1817–1820.
Dijk JM, Algra A, Van Der Graaf Y, Grobbee DE, Bots ML . Carotid stiffness and the risk of new vascular events in patients with manifest cardiovascular disease. The SMART study. Eur Heart J 2005; 26: 1213–1220.
Acknowledgements
This study was financially supported by The Netherlands Heart Foundation grant number (2007-B178).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Wijnstok, N., Serné, E., Hoekstra, T. et al. The relationship between 30-year developmental patterns of body fat and body fat distribution and its vascular properties: the Amsterdam Growth and Health Longitudinal Study. Nutr & Diabetes 3, e90 (2013). https://doi.org/10.1038/nutd.2013.31
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nutd.2013.31
Keywords
This article is cited by
-
Long-term outcomes and prognostic factors in papillary thyroid microcarcinoma patients with distant metastases
Endocrine (2022)
-
Why item response theory should be used for longitudinal questionnaire data analysis in medical research
BMC Medical Research Methodology (2015)
-
What the Long Term Cohort Studies that Began in Childhood Have Taught Us about the Origins of Coronary Heart Disease
Current Cardiovascular Risk Reports (2014)