Abstract
Background:
From a public health perspective it is important to know which of the currently used methods to estimate changes in maternal body fat during pregnancy and the year thereafter is the most adequate.
Objectives:
To evaluate the concurrent validity between leptin and surrogates of fat measures: body mass index (BMI) and the sum of four skin folds.
Design:
Data from the New Life(style) intervention study were analysed as a cohort study.
Setting:
Midwife practices in The Netherlands.
Population:
Healthy pregnant nulliparous women.
Methods:
Anthropometric measurements were done and blood was collected at 15, 25 and 35 weeks of pregnancy and at 6, 26 and 52 weeks after delivery. Data were used if at least 4 out of the 6 measurements were available, leaving 87 women in the analyses. Spearman’s correlation coefficients between leptin and BMI and between leptin and the sum of skin folds were calculated for each time point and for the changes between the time points.
Results:
Correlations between leptin and BMI varied from 0.69 to 0.81. Correlations between leptin and the sum of skin folds were comparable, varying between 0.65 and 0.81.
Correlations between changes in leptin and changes in BMI and the sum of skin folds, respectively, were much lower compared with cross-sectional correlations.
Conclusion:
Because of the high correlation among the three methods and because of the overlapping intervals, all methods seem to be equally adequate to estimate changes in maternal body fat during pregnancy and the year thereafter.
Similar content being viewed by others
Introduction
The prevalence of overweight among the adult Dutch population has increased strongly in the past years (www.cbs.nl/nl/-NL/menu/themas/gezondheid-welzijn/publicaties/artikelen/archief/2011/2011–3514-wm.htm). Overweight is associated with a number of health problems such as hypertension, cardiovascular diseases, diabetes and hypercholesterolemia.1, 2
For women, childbearing is a significant risk factor for developing overweight and obesity.3, 4
During pregnancy, body weight increases and fat storage takes place. Mean fat deposition by 34–36 weeks of gestational age is 4.5 kg.5
For pregnant women, the Institute of Medicine in the United States developed guidelines on the amount of body weight gain during pregnancy considered ‘healthy’, defined as having the best chances for a good pregnancy outcome.6, 7 The advised weight gain differs per prepregnancy body mass index (BMI) category, and overweight and obese women are advised to gain less compared with normal-weight women. In general, ∼40% of women gain weight, as advised. The guidelines only focus on absolute body weight gain and not on relative changes because of, for example, fat storage.8, 9, 10
However, as during pregnancy there is a change in body composition and an accretion of water, body weight gain might not be the best measure reflecting these changes in fat storage.11Furthermore, even when gaining the same body weight, the amount and location of body fat stored might differ between women.12, 13, 14
This is very relevant, as in general, visceral fat poses higher health risks than subcutaneous fat.15
Several methods have been developed for estimating body composition such as weight and BMI,16 waist circumference,17 arm, thigh and calf circumference18, 19 and the four-compartment model20, 21 based on measurement of total body water, total body potassium, body density and bone mineral content (by deuterium dilution, whole-body potassium counting, hydrodensitometry and dual-energy X-ray absorptiometry). However, because of unknown or possibly harmful effects on the fetus, some methods (for example, dual-energy X-ray absorptiometry) cannot be used in pregnancy.
Other measures are not feasible on a large scale because of logistical or financial reasons (for example, computed tomography scan).
Weight gain, a surrogate of fat measure, is the easiest method to carry out. Measuring four skin folds has been validated to assess the amount of fat.13, 22, 23, 24
Biomarkers such as leptin are of more recent date. Leptin inhibits food intake and stimulates energy expenditure in experimental animals and is considered to be a proxy for body fat storage.25 It is proxy for visceral fat and a useful biomarker of fat accumulation-related insulin resistance, inflammation and metabolic risks.26, 27, 28 In pregnancy, apart from the maternal production, it is also produced by the placenta. It starts to increase from the first weeks of pregnancy.29, 30, 31, 32, 33, 34, 35, 36, 37, 38 Maternal leptin levels during pregnancy correlate closely with BMI.32 Fattah et al.39 concluded in 2011 that ‘Visceral fat is the main determinant of circulating maternal leptin in the first trimester of pregnancy’, making it a relevant marker for health risks.
In this study, construct validity of different (surrogate) fat measures in pregnancy and a year postpartum was assessed. Correlations between leptin, body weight and the sum of four skin folds were assessed as a construct validation of these methods.
In addition, changes in leptin levels were correlated to changes in the other measures, as a measure of responsiveness. Data from an intervention study on the effects of counselling on physical activity and diet were used, in which body weight and four skin folds were measured and blood samples taken at 15, 25 and 35 weeks of gestation, and at 6, 26 and 52 weeks postpartum.
Materials and methods
Study population and design
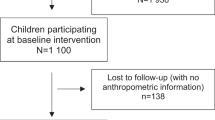
In the New Life(style) study, a randomised controlled trial (ISRCTN 85313483), healthy women expecting their first child and receiving antenatal care from midwives participated.40 At several time points, individual weight gain was discussed in relation to weight gain guidelines for pregnant women of the American Institute of Medicine. A questionnaire was used that retrieved information on demographics, age, marital status, menstrual history, parity, socioeconomic status, medical history, smoking/drinking habits, physical activity, body weight and severe weight changes before pregnancy. Anthropometric measurements, including body weight, body height, triceps, biceps, subscapular and suprailiac skin folds, were carried out and blood was collected by trained staff in the midwifery practices at 15 (T1), 25 (T2), and 35 (T3) weeks of pregnancy and at 6 (T4), 26 (T5) and 52 (T6) weeks after delivery. To assess the concurrent validity between the different methods, the data were used on body weight, skin folds and leptin of those women who gave birth to a live singleton infant after a minimal gestation of 36 weeks and for whom data were available from at least 4 out of the 6 measurements.
Measurements techniques
Body height was measured in bare feet using a wall-mounted height scale (SECA 206, HaB International Ltd., Southam, UK), with an accuracy of 0.1 cm. Calibrated electronic scales (SECA 888) were used to determine body weight of the participants in underwear and pants, with an accuracy of 0.1 kg. Both body weight and body height were measured twice, and the mean value of the two measurements was computed and used to calculate individual BMI (kg m−2).
Skin folds
Harpenden callipers (HaB International Ltd.) were used to assess skin fold thickness of the biceps, triceps, subscapular and suprailiac area, according to the method described by Weiner et al.41 All skin folds were assessed twice and the mean of the two was computed. In case the two measurements of a skin fold differed by >1.0 mm, the skin fold was measured a third time and the mean of the three values was calculated.
Maternal blood sampling and laboratory measurements
Most (89%) samples were taken between 0800 and 1200 h to minimise diurnal variation (leptin shows its maximum expression during the night).42, 43, 44 The last samples were taken at 1645 h. Blood samples were taken from a subgroup of participants during each measurement. All samples were obtained from the antecubital fossa, put on ice and transported by the blood collector. On arrival, blood was processed and stored at −20 °C at the laboratory of the VU University Medical Centre until analysis.
Leptin was determined by radioimmunoassay (Linco Research Inc., St Charles, MO, USA). Inter- and intraassay variations were both <7% in the range measured. The lower limit of quantitation was 0.5 μg l−1.
Statistical analysis
Statistical analyses were carried out using the statistical package SPSS (release 15, SPSS, Inc., Chicago, IL, USA). Descriptive statistics are given as median values and ranges.
As data were not normally distributed, Spearman’s correlations were calculated between the three methods. Confidence intervals were calculated using Bootstrapping (5000 replications).
To assess the responsiveness, changes between time points both during and after pregnancy were evaluated. Spearman’s correlation coefficients were calculated for the correlation between changes in the different estimates of body fat.
Results
Participants
Out of the 780 invited women, 246 women participated in the study and were randomised as follows: 123 in the intervention group and 123 in the standard care group. Leptin was only assessed in those women whose body weight and skin fold measurements were known, leaving 122 at T1, 101 at T2, 85 at T3, 86 at T4, 81 at T5 and 81 at T6. Women who gave birth to a live singleton infant after a minimal gestation of 36 weeks were included in the analyses of this study. Of the 87 women, data on BMI, skin folds and leptin on at least four sessions were available, and these women were included in the analyses. The characteristics of the women in the study sample are summarised in Table 1. Analyses showed that the sample included in the analyses was comparable to the total study population with regard to age, prepregnancy BMI, education and ethnicity.
Body weight, BMI, sum of four skin folds and leptin in pregnancy and postpartum
In Table 2, the data on weight, BMI, sum of four skin folds and leptin at all six measurements are presented. In Figure 1, changes in BMI, sum of four skin folds and leptin during pregnancy and a year postpartum are represented for each BMI category (underweight BMI <18.5 kg m−2; healthy weight BMI 18.5–25 kg m−2; overweight or obese BMI >25 kg m−2).
Correlations between different estimates of fat mass
Correlations between leptin and BMI varied from 0.69 to 0.81, with the weakest correlation at 35 weeks of gestation and the strongest correlation at 52 weeks postpartum (Table 3).
Leptin and the sum of skin folds had comparable correlations varying between 0.65 and 0.81, with the weakest correlation at 6 weeks postpartum and the strongest correlation at 52 weeks postpartum.
Of the individual skin folds, the triceps skin fold had the strongest correlation with leptin, ranging from 0.58 to 0.80, with the weakest correlation at 6 weeks postpartum and the strongest at 52 weeks postpartum.
Responsiveness
The mean changes in leptin, body weight and sum of four skin folds per BMI category are depicted in Figure 1. In order to assess responsiveness of the sum of four skin folds and BMI for measuring changes in body fat mass, correlations between changes in leptin and changes in BMI and skin folds were calculated (Table 4).
Compared with cross-sectional correlations between these parameters, correlations between Δ-values representing changes in body weight and changes in leptin were much lower. From 15 to 25 weeks of pregnancy, the correlation between the respective Δ-values was low (0.13) and nonsignificant (P=0.26). In the other time intervals, Δ-values representing changes in leptin were correlated with Δ-values representing changes in body weight, although correlations were moderate (0.28–0.36).
Discussion
In this study the concurrent validity was assessed between leptin and BMI and the sum of four skin folds as (surrogate) fat measures in pregnancy and the year after. In addition, responsiveness towards change of BMI and the sum of four skin folds was studied.
All measures of body fat mass increased steadily from 15 to 35 weeks of pregnancy, and went down rapidly after delivery. At all time points, maternal BMI and skin folds were strongly correlated with leptin, indicating a high concurrent validity with leptin. Correlations between changes in leptin and changes in BMI or skin folds were generally lower.
A correlation coefficient of 0.81 between maternal leptin serum levels and BMI at 6–8 weeks of pregnancy has been reported previously.45 This coefficient went down to 0.50 at birth and went up to 0.76 six weeks after delivery.
In our study a similar pattern was seen, with a correlation coefficient between BMI and leptin that changed from 0.75 (confidence interval (CI) 0.60–0.85) at 15 weeks of pregnancy to 0.69 (CI 0.54–0.79) at 35 weeks, and had the highest 0.81 (CI 0.71–0.88) at 52 weeks postpartum. The lower correlations in late pregnancy and early postpartum are likely because of a change in fluid collection and placental production of leptin.30, 31
The correlation between leptin and skin folds in our study, varied from 0.65 (CI 0.49–0.78) to 0.81(CI 0.68–0.89), overlapping with the correlations found between leptin and BMI.
The highest correlation (0.80, CI 0.69–0.89) was found with the triceps skin fold at 52 weeks postpartum. In another study an increase of the triceps skin fold at 52 weeks post partum was found and it was suggested that the triceps is more sensitive to changes in fluid collection in pregnancy and that the triceps might reflect a new rearrangement of maternal body fat after pregnancy, being a marker of subcutaneous fat.46 In this study we cannot differentiate between the different fat compartments but it might be that fat accumulation during pregnancy is of a mixed (visceral and subcutaneous) pattern.
Why correlations between changes in leptin and changes in body weight or skin fold thickness were considerably lower than between these measures cross-sectionally is not fully clear. In an alternative analysis, we also looked at correlations between relative changes (as a percentage of the levels at 15 weeks of pregnancy) and found the same results. Our observations are therefore not explained by the fact that 5 kg body weight change is different for women who are lean compared with obese women and might have different effects on leptin and/or skin folds. Other explanations might be that changes in leptin are not occurring in concert with changes in body weight and skin folds.
There are some indications that leptin increases first before body fat is stored. This might be because there is a relative leptin resistance during pregnancy.32 But this would only account for lower correlations between changes in leptin and other (surrogate) fat measures in early pregnancy and not in the postpartum period. And on top of this, in nonpregnant obese women, there is already a leptin resistance.47
In our study at least 30% of the variation in leptin remains unexplained. This might have several reasons. The net production of leptin per unit fat increases. In 1997, it was shown that the leptin production per unit fat mass is higher in pregnancy than after delivery.31 Therefore, BMI or other measures of fat mass might correlate less with leptin during pregnancy.
A greater leptin production in visceral fat was observed in pregnant mice, and greater production in subcutaneous fat in nonpregnant mice.48 In pregnancy, visceral fat increases more than subcutaneous fat. Leptin production occurs primarily in visceral fat, and in pregnancy especially fat is stored as visceral fat. BMI or sum of skin folds might not reflect these site-specific changes in fat mass.
Furthermore, the production of leptin by the placenta might make a substantial contribution to the rise in maternal leptin. That explains why in the first and second trimesters, leptin increases before BMI increases.32 In early pregnancy, mRNA content does not increase and cross-sectional comparisons of leptin mRNA concentration in white adipose tissue from pregnant and nonpregnant women are suggesting that adipose tissue leptin makes little contribution to the plasma rise.49 Maternal BMI and skin folds will not reflect the increase in leptin, produced by the placenta.
In the past, different techniques for measuring body composition, including fat mass, were developed but never validated during pregnancy. Total body water and underwater weighing were in the past assessed as a method to assess body fat mass, and found that it was highly reliable and comparable to anthropometric estimation.13
A combination of methods, the four-component model, was advocated to measure body fat in pregnant women.22 In 1997, it was demonstrated that ‘even when pregnancy-specific values were used, individual fat mass estimates (derived from TBW and body density) might differ by >3 kg from the four-component value.21 Fat mass by total body potassium may differ by >10 kg from fat mass by the four-component model during pregnancy, and by 6 kg postpartum. Use of pregnancy-corrected two-compartment models (TBW, total body potassium(TBK) and body density) produced reliable mean fat mass estimates during pregnancy, but individual fat mass estimates varied widely from four-component values’.21
The limitations and strengths of this study need to be discussed. The major strength of our study is the longitudinal measures throughout pregnancy and 1 year thereafter. The obvious limitation of this study is the lack of a gold standard for fat and fat distribution in pregnancy. Further validation of (changes in) fat distribution in pregnancy might be warranted.
In conclusion, our study clearly demonstrated that during pregnancy and 1 year thereafter, maternal body weight and skin folds were highly correlated with leptin at each time point. Because of the overlapping CIs, no preference could be given to any of the three methods studied.
Correlations between changes were considerably lower and no clear explanation could be given.
References
Doak CM, Wijnhoven TMA, Schokker DF, Visscher TLS, Seidell JC . Age standardization in mapping adult overweight and obesity trends in the WHO European Region. Obes Rev 2012; 13: 174–191.
Popkin BM, Doak CM . The obesity epidemic is a worldwide phenomenon. Nutr Rev 1998; 56: 106–114.
Davis EM, Zyzanski SJ, Olson CM, Stange KC, Horwitz RI . Racial, ethnic, and socioeconomic differences in the incidence of obesity related to childbirth. Am J Public Health 2009; 99: 294–299.
Gore SA, Brown DM, West DS . The role of postpartum weight retention in obesity among women: a review of the evidence. Ann Behav Med 2003; 26: 149–159.
Kopp-Hoolihan LE, van Loan MD, Wong WW, King JC . Fat mass deposition during pregnancy using a four-component model. J Appl Physiol 1999; 87: 196–202.
Rasmussen KM, Catalano PM, Yaktine AL . New guidelines for weight gain during pregnancy: what obstetrician/gynecologists should know. Curr Opin Obstet Gynecol 2009; 21: 521–526.
Rasmussen KM, Abrams B, Bodnar LM, Butte NF, Catalano PM, Siega-Riz MA . Recommendations for weight gain during pregnancy in the context of the obesity epidemic. Obstet Gynecol 2010; 116: 1191–1195.
Althuizen E, van Poppel MNM, Seidell JC, van Mechelen W . Correlates of absolute and excessive weight gain during pregnancy. J Womens Health 2009; 18: 1559–1566.
Forsum E, Sadurskis A, Wager J . Estimation of body fat in healthy Swedish women during pregnancy and lactation. Am J Clin Nutr 1989; 50: 465–473.
Larciprete G, Valensise H, Vasapollo B, Altomare F, Sorge R, Casalino B et al. Body composition during normal pregnancy: reference ranges. Acta Diabetol 2003; 40 (Suupl 1): S225–S232.
Davison JM . Edema in pregnancy. Kidney Int 1997; 59: S90–S96.
Ehrenberg HM, Huston-Presley L, Catalano PM . The influence of obesity and gestational diabetes mellitus on accretion and the distribution of adipose tissue in pregnancy. Am J Obstet Gynecol 2003; 189: 944–948.
Huston-Presley L, Wong WW, Roman NM, Amini SB, Catalano PM . Anthropometric estimation of maternal body composition in late gestation. Obstet Gynecol 2000; 96: 33–37.
Kinoshita T, Itoh M . Longitudinal variance of fat mass deposition during pregnancy evaluated by ultrasonography: the ratio of visceral fat to subcutaneous fat in the abdomen. Gynecol Obstet Invest 2006; 61: 115–118.
Matsushita Y, Nakagawa T, Yamamoto S, Takahashi Y, Yokoyama T, Mizoue T et al. Effect of longitudinal changes in visceral fat area and other anthropometric indices to the changes in metabolic risk factors in Japanese men: the Hitachi Health Study. Diabetes Care 2012; 35: 1139–1143.
Lindsay CA, Huston L, Amini SB, Catalano PM . Longitudinal changes in the relationship between body mass index and percent body fat in pregnancy. Obstet Gynecol 1997; 89: 377–382.
Mahaba HM, Ismail NA, El Teheiwy MM, El-Goewily MM, Ramadan MS . Development of weight gain charts for healthy Egyptian pregnant women. J Egypt Public Health Assoc 2001; 76: 369–391.
Khadivzadeh T . Mid upper arm and calf circumferences as indicators of nutritional status in women of reproductive age. East Mediterr Health J 2002; 8: 612–618.
Perez A, Murillo C, Hernandez R, Herrera HA . Circumferences to evaluate changes in body mass and amount of total fat of women in second and third trimester of pregnancy. Nutr Hosp 2010; 25: 662–668.
Goran MI, Toth MJ, Poehlman ET . Cross-validation of anthropometric and bioelectrical resistance prediction equations for body composition in older people using the 4-compartment model as a criterion method. J Am Geriatr Soc 1997; 45: 837–843.
Hopkinson JM, Butte NF, Ellis KJ, Wong WW, Puyau MR, Smith EO . Body fat estimation in late pregnancy and early postpartum: comparison of two-, three-, and four-component models. Am J Clin Nutr 1997; 65: 432–438.
Durnin JV, Rahaman MM . The assessment of the amount of fat in the human body from measurements of skinfold thickness. Br J Nutr 2003; 89: 147–155.
Licitra L, Pregazzi R, Troiano L, Guaschino S . Anthropometric skin-fold and impedance measurement assessment of the maternal nutritional status at the end of pregnancy. Comments deduced from a study of 54 cases. Minerva Ginecol 1998; 50: 379–382.
Lederman SA, Pierson RN Jr, Wang J, Paxton A, Thornton J, Wendel J et al. Body composition measurements during pregnancy. Basic Life Sci 1993; 60: 193–195.
Harwood HJ Jr . The adipocyte as an endocrine organ in the regulation of metabolic homeostasis. Neuropharmacology 2012; 63: 57–75.
Singh P, Peterson TE, Sert-Kuniyoshi FH, Glenn JA, Davison DE, Romero-Corral A et al. Leptin signaling in adipose tissue: role in lipid accumulation and weight gain. Circ Res 2012; 111: 599–603.
Nakatani H, Hirose H, Yamamoto Y, Saito I, Itoh H . Significance of leptin and high-molecular weight adiponectin in the general population of Japanese male adolescents. Metabolism 2008; 57: 157–162.
Caprio M, Fabbrini E, Isidori AM, Aversa A, Fabbri A . Leptin in reproduction. Trends Endocrinol Metabol 2001; 12: 65–72.
Hauguel-de Mouzon S, Lepercq J, Catalano P . The known and unknown of leptin in pregnancy. Am J Obstet Gynecol 2006; 194: 1537–1545.
Lepercq J, Challier JC, Guerre-Millo M, Cauzac M, Vidal H, Hauguel-de Mouzon S . Prenatal leptin production: evidence that fetal adipose tissue produces leptin. J Clin Endocrinol Metab 2001; 86: 2409–2413.
Butte NF, Hopkinson JM, Nicolson MA . Leptin in human reproduction: serum leptin levels in pregnant and lactating women. J Clin Endocrinol Metab 1997; 82: 585–589.
Highman TJ, Friedman JE, Huston LP, Wong WW, Catalano PM . Longitudinal changes in maternal serum leptin concentrations, body composition, and resting metabolic rate in pregnancy. Am J Obstet Gynecol 1998; 178: 1010–1015.
Magni P, Martini L, Motta M . Leptin actions on the reproductive axis. J Clin Endocrinol Metab 2001; 86: 946–947.
Pickavance L, Tadayyon M, Williams G, Vernon RG . Lactation suppresses diurnal rhythm of serum leptin. Biochem Biophys Res Commun 1998; 248: 196–199.
Sattar N, Greer IA, Pirwani I, Gibson J, Wallace AM . Leptin levels in pregnancy: marker for fat accumulation and mobilization? Acta Obstet Gynecol Scand 1998; 77: 278–283.
Stein TP, Scholl TO, Schluter MD, Schroeder CM . Plasma leptin influences gestational weight gain and postpartum weight retention. Am J Clin Nutr 1998; 68: 1236–1240.
Tamas P, Sulyok E, Szabo I, Vizer M, Ertl T, Rascher W et al. Changes of maternal serum leptin levels during pregnancy. Gynecol Obstet Invest 1998; 46: 169–171.
Woodside B, Abizaid A, Walker C . Changes in leptin levels during lactation: implications for lactational hyperphagia and anovulation. Horm Behav 2000; 37: 353–365.
Fattah C, Barry S, O'Connor N, Farah N, Stuart B, Turner MJ . Maternal leptin and body composition in the first trimester of pregnancy. Gynecol Endocrinol 2011; 27: 263–266.
Althuizen E, van Poppel MNM, Seidell JC, van der Wijden C, van Mechelen W . Design of the New Life(style) study: a randomised controlled trial to optimise maternal weight development during pregnancy. BMC Public Health 2006; 6: 168.
Weiner JS, Lourie JA . Practical Human Biology, Academic Press. New York, 1981; 0127419608.
Cizza G, Ronsaville DS, Kleitz H, Eskandari F, Mistry S, Torvik S et al. Clinical subtypes of depression are associated with specific metabolic parameters and circadian endocrine profiles in women: the power study. PLoS One 2012; 7: e28912.
Paracchini V, Pedotti P, Taioli E . Genetics of leptin and obesity: a HuGE review. Am J Epidemiol 2005; 162: 101–114.
George F, Donald P, Jon L Academic Press: Elsevier, 2012. p. 280 ISBN 978–0–12–3750976, figure 12.5.
Schubring C, Prohaska F, Prohaska A, Englaro P, Blum W, Siebler T et al. Leptin concentrations in maternal serum and amniotic fluid during the second trimenon: differential relation to fetal gender and maternal morphometry. Eur J Obstet Gynecol Reprod Biol 1999; 86: 151–157.
Forsum E, Sadurskis A, Wager J . Resting metabolic rate and body composition of healthy Swedish women during pregnancy. Am J Clin Nutr 1988; 47: 942–947.
Kennedy A, Gettys TW, Watson P, Wallace P, Ganaway E, Pan Q et al. The metabolic significance of leptin in humans: gender-based differences in relationship to adiposity, insulin sensitivity, and energy expenditure. J Clin Endocrinol Metab 1997; 82: 1293–1300.
Schlitt JM, Schulz LC . The source of leptin, but not leptin depletion in response to food restriction, changes during early pregnancy in mice. Endocrine 2012; 41: 227–235.
Catalano PM, Nizielski SE, Shao JH, Preston L, Qiao LP, Friedman JE . Downregulated IRS-1 and PPAR gamma in obese women with gestational diabetes: relationship to FFA during pregnancy. Am J Physiol Endocrinol Metabol 2002; 282: E522–E533.
Acknowledgements
We thank Dr Aart Jan van der Lelij, Professor of Clinical Endocrinology at the Erasmus MC Department of Internal Medicine, for his critical remarks. We also thank the counsellors, midwives and participants who participated in this trial. This study was financially supported by a grant from The Netherlands Organization for Health Research and Development (ZonMw,grant4010.0017). Financial support of this publication is provided by The Netherlands Organisation for Scientific Research (NWO).
Ethics Approval
The Medical Ethics Committee of VU University Medical Centre has approved the study design (registration number 2004/184), protocols and informed consent procedure on 11 November 2004 (ISRCTN Trial Registration: http://www.controlled-trials.com/ISRCTN85313483).
Author Contributions
CL van der Wijden had a role in designing and planning of the study, performed the analyses partially and drafted the article. HA Delemarre-van der Waal had a role in design and planning of the study, and critically revised the study results and article. W van Mechelen had a role in the design and conception of the study, performed the analyses partially and partially drafted the article. MNM van Poppel had role in the conception of the study, and revised the article critically. All authors approved this version for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
van der Wijden, C., Delemarre-van der Waal, H., van Mechelen, W. et al. The concurrent validity between leptin, BMI and skin folds during pregnancy and the year after. Nutr & Diabetes 3, e86 (2013). https://doi.org/10.1038/nutd.2013.27
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nutd.2013.27