Abstract
Background:
South Asian people who originate from the Indian subcontinent have greater percent body fat (%BF) for the same body mass index (BMI) compared with white Caucasians. This has been implicated in their increased risk of type 2 diabetes and cardiovascular disease. There is limited information comparing different measures of body fat in this ethnic group.
Objectives:
The objectives of this study were: (1) to investigate the correlation of %BF measured by a foot-to-foot bioelectrical impedance analysis (FF-BIA) against the BOD POD, a method of air-displacement plethysmography, and (2) to determine the correlations of simple anthropometric measures, (that is, BMI, body adiposity index (BAI), waist circumference (WC), hip circumference (HC) and waist-to-hip ratio (WHR)) against the BOD POD measure of body fat.
Methods:
Eighty apparently healthy South Asian men and women were recruited from the community, and measurements of height, weight, WC, HC and body composition using Tanita FF-BIA and BOD POD were taken.
Results:
The mean±s.d. age of participants was 27.78±10.49 years, 42.5% were women, and the mean BMI was 22.68±3.51 kg m−2. The mean body fat (%BF) calculated by FF-BIA and BOD POD was 21.94±7.88% and 26.20±8.47%, respectively. The %BF calculated by FF-BIA was highly correlated with the BOD POD (Pearson’s r=0.83, P<0.001), however, FF-BIA underestimated %BF by 4.3%. When anthropometric measures were compared with % BF by BOD POD, the BAI showed the strongest correlation (r=0.74) and the WHR showed the weakest (r=0.33). BAI generally underestimated %BF by 2.6% in comparison with %BF by BOD POD. The correlations of BOD POD with other measures of %BF were much stronger in subjects with a BMI >21 kg m−2 than those with a BMI ⩽21 kg m−2.
Conclusion:
The FF-BIA and BAI estimates of %BF are highly correlated with that of BOD POD among people of South Asian origin, although both methods somewhat underestimate % BF. Furthermore, their correlations with % BF from BOD POD are significantly weakened among men and women with a BMI ⩽21 kg m−2.
Similar content being viewed by others
Introduction
People of South Asian origin living in Canada have a higher risk of developing type 2 diabetes and cardiovascular disease when compared with other ethnicities.1 There are several factors contributing to this higher risk, including that South Asians have greater adiposity for a given level of body mass index (BMI), and more visceral and ectopic adipose tissue accumulation, including fatty liver.2, 3
The most commonly used measure to categorize individuals as being overweight or obese is the BMI. However, BMI does not distinguish between fat and fat-free mass, and several studies have shown that a low BMI is not associated with a low percent body fat (%BF) in the South Asian population.3 Furthermore, South Asians have greater abdominal obesity, total abdominal fat and intra-abdominal adipose tissue for a similar value of BMI compared with white Caucasian populations.2 Razak et al.2 observed that a BMI >21 kg m−2 is associated with dysglycemia and dyslipidemia in South Asians, whereas comparable changes do not occur among white Caucasians until their BMI is >30 kg m−2. Given the propensity of South Asians to develop adiposity-related disorders, it is important to have methods to accurately analyze body composition and %BF in this high-risk population.
Several techniques to measure body composition under controlled conditions have been developed. A commonly used reference method in body composition studies is dual X-ray absorptiometry (DXA). However, DXA equipment is expensive, difficult to use in large population-based studies and exposes individuals to some radiation.4, 5 Other methods of body composition analysis have been developed, including the foot-to-foot bioelectrical impedance analysis (FF-BIA), and the BOD POD. Several studies have validated the FF-BIA against DXA.6 Furthermore, FF-BIA is cheap, portable, time-efficient and requires minimal training. However, FF-BIA has been reported to be influenced by biological factors such as pulsatile blood flow and total amount of body water, which may limit its use in healthy and non-healthy populations.7 In addition, the FF-BIA technique may not be a good representation of %BF in abdominally obese individuals.8 BOD POD is the first commercially available air-displacement plethysmograph and is considered to be among the most valid and reliable measures of body fat.9 The advantages of BOD POD include its quick, comfortable, automated, noninvasive and safe measurement process, and its accommodation of diverse range of subjects including children, obese, elderly and disabled.9 However, BOD POD equipment requires trained operators, and is not portable, making it difficult to use in large population-based studies.
In addition to FF-BIA and BOD POD, there are simple anthropometric measures that enable brief screening of individuals in an office setting and in population-based studies. These include BMI, waist circumference (WC), hip circumference (HC) and waist-to-hip ratio (WHR). More recently, a new index for estimating %BF in adults, known as the body adiposity index (BAI) has been proposed.10
The purpose of this study is to examine the utility of different body composition measurement methods to determine %BF in a South Asian population living in Canada. The primary objectives were: (1) to investigate the correlation of a FF-BIA against the BOD POD, a method of air-displacement plethysmography, and (2) to determine the correlations of simple anthropometric measures, (that is, BMI, BAI, WC, HC and WHR) against the BOD POD measure of body fat.
Materials and methods
Study sample
The study received approval from the Hamilton Health Sciences Research Ethics Board on 8 December 2011, and all participants provided informed consent. The eligible participants for this study were healthy South Asian males and females between 18 and 60 years of age. Participants were recruited through advertisements at McMaster University, Hindu Temple in Hamilton, Ontario, and through electronic advertising in the city of Hamilton. South Asian ethnicity was verified at the time of the clinic visit. Participants were excluded if they had history of heart disease or were pregnant.
Study design
All participants were asked to observe a 2-h fast before their scheduled appointment, which was confirmed upon arrival. Each participant’s height was measured using a wall-mounted standiometer device to the nearest 0.5 cm. A measuring tape was used to measure each participant’s HC and WC. The plane of the tape was kept perpendicular to the long axis of the body and parallel to the floor. HC was measured at the level of maximum extension of buttocks, and the WC was measured at the level of the umbilicus. Subsequently, each participant had his or her body fat measured using the Tanita BIA scale (BC- 585F; Tanita Corporation, Tokyo, Japan) and BOD POD (Life Measurement Instruments, Concord, CA, USA). All assessments were conducted at the Population Health Research Institute Research Clinics, Hamilton General Hospital.
BIA methodology
The FF-BIA resembles a bathroom scale. The age, sex and height of each participant were entered in the scale, and the participant was asked to step on the platform barefooted, ensuring that his/her clothing was not in contact with the scale. The electrodes connected to the foot pads send a low and safe electrical signal through the body, and the measured %BF value was displayed.
The FF-BIA measures impedance against a small electrical current sent through the body, which is related to the conduction properties of the tissue. The fat-free mass in the body contains electrolyte-rich water and has relatively low impedance, whereas the fat mass is devoid of fluids and has higher impedance. In a FF-BIA, the current circulates in the legs and lower part of the trunk. The fat-free mass (FFM) is measured from an extrapolation to the whole body by using an equation of resistance, weight, height, age and sex. The prediction equations differ between males and females in the healthy adult general population, and these are validated against DXA measures. The manufacturers have kept these equations confidential and they have not been reported in literature.
BOD POD
BOD POD measures body volume using the amount of air displaced in an enclosed chamber. The subject sits in the 450-l front chamber, and the instrumentation is housed in the 300-l rear chamber. Between the two chambers, a volume perturbing element in the form of a movable diaphragm oscillates back and forth causing sinusoidal volume perturbations that are equal in magnitude but opposite in sign with a magnitude of 350 ml.11 The changes in volume cause small pressure fluctuations of approximately 1 cm3 H2O that are analyzed by the software to yield chamber air volume (V1).11 This process is then repeated with the subject introduced into the test chamber (V2). The difference V1−V2 is the body volume (Vb(raw)). In the BOD POD, the air is maintained under adiabatic conditions, and Poisson’s law is used to describe the relationship between pressure and volume: P1/P2=(V2/V1)γ, where γ is 1.4 for air.11
Although air is mostly maintained under adiabatic conditions, measurement error can be caused by isothermal air in the lungs, near skin or hair and in clothing.9, 11 To reduce this potential error, participants wear a tight-fitting swimsuit and a swimcap during the test. Likewise, the BOD POD software calculates a surface area artifact to correct for the apparent negative volume effects caused by the isothermal air at skin surface. The surface area artifact is calculated as a product of body surface area (derived from weight and height) and a constant. Finally, the last step of BOD POD measures the subject’s lung air volume (Vtg) to account for the isothermal air in lungs.11
The body volume (Vb) is calculated by the following formula:11

Knowing the mass of the subject, the body density (Db) can be calculated by the formula:

Finally, the %BF can be determined using the derived equations, such as the one by Siri12 for the general population:

BOD POD methodology
At the beginning of each testing day, a quality-control procedure was performed. The participants were asked to change into the recommended form-fitting clothing before their test. For each participant, the date of birth, sex, height and ID were entered into the computer. A two-step calibration procedure was then performed, first with the empty test chamber and then with a 50-l calibration cylinder. While the second calibration step was being performed, the subject was weighed on a calibrated electronic scale. Next, the participant was asked to sit inside the BOD POD chamber and instructed to remain still and continue normal breathing while the body volume was being measured. The measurement took 50 s, and this step was repeated after opening and closing the chamber door. The mean of two measurements was used by the BOD POD software as the body volume. If the first two measurements were not within 150 ml of each other, then a third measurement was performed and the software averaged the two measurements that were within 150 ml of each other. The final step involved measurement of thoracic lung volume (Vtg). This began with the subject in the BOD POD chamber breathing normally for equilibration for 4–5 breaths. The participant then inserted a disposable tube into his or her mouth while plugging his or her nose. This tube was connected to a valve in the chamber through an antimicrobial filter, and the participant was asked to breathe through the tube. After a few regular breaths, the system induced airway occlusion for 2 s due to the closure of a shutter valve. At this point, the participant gently made 2–3 gentle quick puffs into the tube. The software assessed the compliance of the subject to this step, and it was repeated if necessary. If the participant felt uncomfortable doing this step or was unable to get a measurement after five tries, then the software calculated a predicted lung volume using prediction equations based on height and weight of subjects.9 The lung volume was successfully measured in 57 participants, whereas the predicted lung volume was used in 23 participants. All these procedures were in accordance with the manufacturer’s recommendations.
Calculation of BAI
The HC and height were used to calculate the BAI using the following equation as suggested by Bergman et al.:10

Statistical considerations
All the statistical analyses were performed using PASW 18 (SPSS Inc., Chicago, IL, USA). Means and ± s.d. are reported for continuous variables. The normal distribution of the dependent variables used in the regression analyses was confirmed using histograms. Linear regression analysis was used to plot the % BF calculated by FF-BIA and BOD POD on the x and y axes, respectively, and to calculate the Pearson’s correlation coefficient (r). Male and female specific linear regression analyses were also performed. Subsequently, linear regression was done between the %BF calculated by BOD POD and each of the anthropometric measures independently, including BMI, BAI, WC, HC and WHR. This analysis was then repeated after dichotomizing the subjects based on their BMI (normal BMI ⩽21 kg m−2 and BMI >21 kg m−2) and also after adjusting for age and sex. This was done because a BMI >21 kg m−2 has been shown to be associated with dysglycemia and dyslipidemia in South Asians.2 The correlation coefficients for %BF calculated by FF-BIA vs BAI measurements were also derived. Finally, the data was analyzed using the Bland–Altman method to assess the agreement in fat content measured by BOD POD vs FF-BIA and BOD POD vs BAI. For all calculations, a two-tailed P-value of <0.05 was considered to be statistically significant.
Results
A total of 80 apparently healthy South Asian adult participants (46 males and 34 females) were recruited into the study. The anthropometric measures of the participants, along with their mean body fat values as determined by BOD POD and BIA are reported in Table 1. The dependent variables were normally distributed. The study population ranged from 18 to 57 years, and the BMI ranged from 17.2 to 31.7 kg m−2. Thirty participants (37.5%) had a BMI ⩽21 kg m−2.
The body fat calculated by FF-BIA ranged from 6.6 to 44.1%, and the BOD POD-calculated %BF ranged from 9.7 to 51.2%. The mean body fat measured by FF-BIA was significantly different from that measured by BOD POD, with the FF-BIA measurement being 4.3% lower in subjects overall (P<0.01).
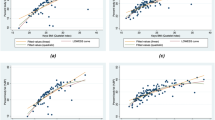
The linear regression analysis showed a significant correlation (r=0.83, P<0.001) between the %BF calculated by BOD POD and FF-BIA. After stratifying by sex, the correlation in males was r=0.75 (P<0.001) and in females was r=0.88 (P<0.001). These plots of %BF measured by BOD POD vs FF-BIA are shown in Figure 1. When stratified according to BMI, the correlations (r) in individuals with a BMI ⩽21 and >21 kg m−2 were 0.59 (P<0.001) and 0.86 (P<0.001), respectively.
Table 2 shows the Pearson’s correlation coefficients (r) and the corresponding P-values between %BF calculated by BOD POD and anthropometric measures, including FF-BIA, BMI, BAI, WC, HC and WHR for all subjects (both unadjusted and adjusted for age and sex). The r values after the subjects were dichotomized based on BMI are also shown in this table. Among simple anthropometric measures, BAI was found to have the strongest correlation with %BF measured by BOD POD (r=0.74), especially in individuals with a BMI >21 kg m−2 (r=0.76). When the variables were adjusted for age and sex, the correlation coefficients of the anthropometric measures with BOD POD %BF ranged from 0.48 (with WHR) to 0.59 (with BIA) for individuals with BMI ⩽21 kg m−2, and from 0.73 (with WHR) to 0.88 (with BIA and WC) for individuals with a BMI >21 kg m−2.
The Pearson’s correlation between the %BF calculated by FF-BIA and BAI measurements was found to be 0.86 (P<0.001). After stratifying by sex, the correlation in males was r=0.85 (P<0.001) and in females was r=0.82 (P<0.001). The correlation in individuals with a BMI ⩽21 and >21 kg m−2 were 0.77 (P<0.001) and 0.85 (P<0.001), respectively.
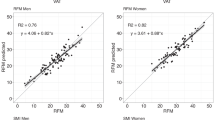
The Bland–Altman analysis plots of agreement between %BF measured by BOD POD and that measured by FF-BIA and BAI are shown in Figure 2. The average difference between the %BF measured by FF-BIA and BOD POD was −4.3% (95% CI −13.9 to 5.4%). Five of the 80 points were outside of these limits of agreement. In comparison with BOD POD, FF-BIA underestimated %BF in 81% (n=65) of the participants. There was a nonsignificant relationship (r=0.13) between the difference between the %BF measured by FF-BIA and BOD POD vs the average of BOD POD and FF-BIA measurements. The average difference between BAI and %BF measured by BOD POD was found to be −2.6% (95% CI −14.8 to 9.6%). Five out of the 80 data points were outside of these limits of agreement. Compared with BOD POD, BAI underestimated %BF in 62% (n=51) of the subjects. There was a significant negative slope (r=0.76) between the difference vs the average of BAI and BOD POD measurements.
Discussion
We observed strong correlations between BOD POD estimates of %BF and those from both FF-BIA and BAI (r=0.83 and 0.74, respectively). Both methods underestimate %BF compared with BOD POD, and both the FF-BIA and BAI correlations with BOD POD are substantially weaker among subjects with a BMI ⩽21 kg m−2. A strong correlation was also observed between %BF measured by FF-BIA and BAI measurements. Collectively, this implies that either BIA or BAI can be used to classify South Asians into relative %BF categories at a population level, although some caution must be used in populations with low mean BMI, that is, <21. In addition, comparisons of %BF among individuals across studies where different assessment methods of % BF are used should be interpreted with caution.
BOD POD uses densitometry to measure body composition, and assumes a two-component model, dividing the body into fat mass and fat-free mass. FF-BIA also uses a two-component model to estimate body composition by measuring the electrical resistance against a mild current sent through the lower limbs. There have been no previous studies comparing these two modalities. However, some studies have reported a strong correlation of hand-to-foot BIA to the BOD POD measurement of %BF in White Caucasian adults.13, 14 Levenhagen et al.13 reported in 20 subjects a correlation coefficient (r) of 0.94 (r=0.93 for females and 0.80 for males), and Biaggi et al.14 reported in 47 subjects a high overall correlation of 0.86 and a nonsignificant overestimation of 1.12% BF by BIA. In contrast, we observed using the FF-BIA machine that BIA systematically underestimates %BF when compared with BOD POD.
Interestingly, when simple anthropometric measures of body composition were compared with the BOD POD %BF, the BAI (an index made up of height and HC) showed the strongest correlation (r=0.74, P<0.001). The other simple anthropometric measures (BMI, WC, HC and WHR) were reasonably well correlated with %BF by BOD POD, except among individuals with a low BMI (Table 2). BAI is a relatively new measure proposed recently by Bergman et al.10 and has been validated against DXA scanning and shown to be strongly correlated in people of Mexican-American, African-American, European-American and Spanish-Mediterranean ethnicities.10, 15, 16 One of the major advantages of the BAI is that it is simple to collect and thus is appropriate for use in large population studies, including in rural areas of India, where electronic or mechanical measurement of BF-measuring machines may not be practical. Another benefit of using BAI is that the same equation is valid for both men and women. Bergman et al.10 found a strong correlation of BAI with DXA (r=0.79 in Mexican-American adults and r=0.85 in African-Americans), and concluded that BAI is a valid measure of %BF. In comparison with DXA, BAI has also been shown to be a better measure of adiposity than BMI patients with familial partial lipodystrophy matched with healthy volunteers (r=0.71 with BAI and 0.27 with BMI),17 in 2900 healthy white Caucasians (r=0.74 with BAI and 0.54 with BMI),15 and in 623 healthy white Caucasian adults (ρ(c)=0.75 with BAI and ρ(c)=0.44 with BMI)16 In contrast, a cross-sectional study conducted in a multiethnic sample of 1151 adults of White Caucasian, Black, Hispanic and Asian ethnicities reported a strong correlation between DXA and both BAI (r=0.86) and BMI (r=0.74).18 A recent study by Geliebter et al.19 conducted in 19 clinically severe obese (mean BMI=46.5±9.0 kg m−2) women compared BAI and BMI in relation to %BF measured by BIA, BOD POD and DXA. Overall, BMI was better correlated with all the BF measurements compared with BAI, although this study was small and represented an extreme population. The Bland–Altman analysis in our study showed that BAI generally underestimates %BF, however, the significantly negative slope implies that the BAI overestimates %BF at lower fat levels and underestimates %BF at higher fat levels in comparison with BOD POD. In contrast, Freedman et al.18 found that BAI generally overestimated %BF compared with DXA, although similar to our findings, the overestimation by BAI was greater at lower BF levels. The Bland–Altman plots in the study by Bergman et al.10 also suggest an overestimation of %BF by BAI compared with DXA in individuals with low fat levels; however, this was not discussed in their study.
The significant underestimation of %BF by both FF-BIA and BAI may be explained by the unique BF distribution of South Asians. South Asians have a significantly greater total abdominal fat and intra-abdominal adipose tissue compared with white Caucasians, for a similar value of BMI.3 The FF-BIA estimates %BF based on the fat content in legs and does not account well for the greater amount of abdominal fat, whereas the %BF measured by BOD POD accounts for the whole body. That is, the impedance of the current in FF-BIA might overestimate the content of lean tissue in individuals with proportionally higher intra-abdominal adipose tissue, and thus, estimates of %BF based on current impedance in such individuals would result in an underestimation of the true value. The equation for BAI assumes %BF is proportional to HC and inversely proportional to height. This equation implies an overall density/volume that is fixed for a given height and HC combination. An increase in intra-abdominal adipose tissue without associated increases in either HC or height would result in an underestimation of assumed overall body volume, and thus an underestimation of %BF.
Estimates of %BF based on FF-BIA and BAI seem to be better in larger individuals (BMI >21 kg m−2). It may be that random error in anthropometry measurements required for these methods have a greater impact on smaller individuals. For example, a 1-cm error in HC has a greater impact on an individual with an 80-cm HC than it would on one with a 100-cm HC. Likewise, 1 kg of unaccounted intra-abdominal fat would cause a greater error in the estimated %BF in someone with 20 kg of BF than it would in an individual with 40 kg of BF. The relatively better smaller underestimation seen in BAI compared with FF-BIA might be due to the extra parameter (that is, HC) to account for individual morphology. However, it is noteworthy that neither method completely accounts for morphology differences, and thus, both will be susceptible to error when morphology deviates from that of the average population. Future studies should further elucidate these observations.
The potential limitations of our study include our relatively homogeneous South Asian sample as most of our participants were university students, which may limit the generalization of our results to other South Asians living in Canada and abroad. However, we attempted to recruit a range of individuals across all categories of BMI and %BF, which may partially offset this limitation. In addition, the measurement of WC at the level of umbilicus may be criticized as it is not the location recommended by the World Health Organization. This limitation is likely minor, as previous studies comparing measured and reported WC have concluded that sufficiently accurate WC measurements are obtained from participants, even if no instructions are given on how to take the measurement.20, 21
Conclusion
The FF-BIA and BAI estimates of %BF are highly correlated with that from BOD POD among people of South Asian origin, although both methods somewhat underestimate % BF. Furthermore, their correlations with % BF from BOD POD are significantly weakened among men and women with a BMI ⩽21 kg m−2.
References
Misra A, Khurana L . The metabolic syndrome in South Asians: epidemiology, determinants, and prevention. Metabol Syndr Relat Disord 2009; 7: 497–514.
Razak F, Anand SS, Shannon H, Vuksan V, Davis B, Jacobs R et al. Defining obesity cut points in a multiethnic population. Circulation 2007; 115: 2111–2118.
Misra A, Khurana L . Obesity-related non-communicable diseases: South Asians vs White Caucasians. Int J Obes (Lond) 2011; 35: 167–187.
Ellis KJ . Human body composition: in vivo methods. Physiological reviews 2000; 80: 649–680.
Maddalozzo GF, Cardinal BJ, Snow CA . Concurrent validity of the BOD POD and dual energy X-ray absorptiometry techniques for assessing body composition in young women. J Am Dietet Assoc 2002; 102: 1677–1679.
Jaffrin MY . Body composition determination by bioimpedance: an update. Curr Opin Clin Nutr Metab Care 2009; 12: 482–486.
Miyatake N, Nonaka K, Fujii M . A new air displacement plethysmograph for the determination of Japanese body composition. Diabetes Obes Metab 1999; 1: 347–351.
Gagnon C, Menard J, Bourbonnais A, Ardilouze JL, Baillargeon JP, Carpentier AC et al. Comparison of foot-to-foot and hand-to-foot bioelectrical impedance methods in a population with a wide range of body mass indices. Metab Syndr Relat Disord 2010; 8: 437–441.
Fields DA, Goran MI, McCrory MA . Body-composition assessment via air-displacement plethysmography in adults and children: a review. Am J Clin Nutr 2002; 75: 453–467.
Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG et al. A better index of body adiposity. Obesity 2011; 19: 1083–1089.
Dempster P, Aitkens S . A new air displacement method for the determination of human body composition. Med Science Sports Exerc 1995; 27: 1692–1697.
Siri WE . Body composition from fluid spaces and density: analysis of methods. 1961. Nutrition 1993; 9: 480–491 discussion 480, 492.
Levenhagen DK, Borel MJ, Welch DC, Piasecki JH, Piasecki DP, Chen KY et al. A comparison of air displacement plethysmography with three other techniques to determine body fat in healthy adults. JPEN 1999; 23: 293–299.
Biaggi RR, Vollman MW, Nies MA, Brener CE, Flakoll PJ, Levenhagen DK et al. Comparison of air-displacement plethysmography with hydrostatic weighing and bioelectrical impedance analysis for the assessment of body composition in healthy adults. Am J Clin Nutr 1999; 69: 898–903.
Lopez AA, Cespedes ML, Vicente T, Tomas M, Bennasar-Veny M, Tauler P et al. Body adiposity index utilization in a Spanish Mediterranean population: comparison with the body mass index. PLoS One 2012; 7: e35281.
Johnson W, Chumlea WC, Czerwinski SA, Demerath EW . Concordance of the recently published body adiposity index with measured body fat percent in European-American adults. Obesity 2012; 20: 900–903.
Godoy-Matos AF, Moreira RO, Valerio CM, Mory PB, Moises RS . A new method for body fat evaluation, body adiposity index, is useful in women with familial partial lipodystrophy. Obesity 2012; 20: 440–443.
Freedman DS, Thornton J, Pi-Sunyer FX, Heymsfield SB, Wang J, Pierson RN Jr et al. The body adiposity index (hip circumference/height(1.5)) is not a more accurate measure of adiposity than is BMI, waist circumference, or hip circumference. Obesity 2012; 20: 2438–2444.
Geliebter A, Atalayer D, Flancbaum L, Gibson CD . Comparison of body adiposity index (BAI) and BMI with estimations of % body fat in clinically severe obese women. Obesity 2012; 21: 493–498.
Spencer EA, Roddam AW, Key TJ . Accuracy of self-reported waist and hip measurements in 4492 EPIC-Oxford participants. Public Health Nutr 2004; 7: 723–727.
Lim LL, Seubsman SA, Sleigh A, Bain C . Validity of self-reported abdominal obesity in Thai adults: a comparison of waist circumference, waist-to-hip ratio and waist-to-stature ratio. Nutr Metab Cardiovas Dis 2012; 22: 42–49.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Kalra, S., Mercuri, M. & Anand, S. Measures of body fat in South Asian adults. Nutr & Diabetes 3, e69 (2013). https://doi.org/10.1038/nutd.2013.10
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nutd.2013.10
Keywords
This article is cited by
-
Ethnic Specific body fat percent prediction equation as surrogate marker of obesity in Ethiopian adults
Journal of Health, Population and Nutrition (2021)
-
Analyze the Differential Rates of Anterior Cruciate Ligament Injuries Between Men and Women by Biomechanical Study of Single-Leg Landing in Badminton
Indian Journal of Orthopaedics (2021)
-
Performance of newly developed body mass index cut-off for diagnosing obesity among Ethiopian adults
Journal of Physiological Anthropology (2019)