Abstract
Objective:
Standard approaches have found that rapid growth during the first 2 years of life is a risk factor for overweight in later childhood. Our objective was to test whether growth velocity, independent of concurrent size, was associated with overweight using a nonlinear random-effects model that allows for enhanced specifications and estimations.
Methods:
Longitudinal data from a birth cohort in Mexico (n=586) were used to estimate growth trajectories over 0–24 months for body mass index (BMI), length and weight using the SuperImposition by Translation and Rotation (SITAR) models. The SITAR models use a nonlinear random-effects model to estimate an average growth curve for BMI, length and weight and each participant’s deviation from this curve on three dimensions—size, velocity and timing of peak velocity. We used logistic regression to estimate the association between overweight status at 7–9 years and size, velocity and timing of BMI, length and weight trajectories during 0–24 months. We tested whether any association between velocity and overweight varied by relative size during 0–24 months or birth weight.
Results:
SITAR models explained the majority of the variance in BMI (73%), height (86%) and weight (85%) between 0–24 months. When analyzed individually, relative BMI/length/weight (size) and BMI/length/weight velocity during 0–24 months were each associated with increased odds of overweight in late childhood. Associations for timing of peak velocity varied by anthropometric measure. However, in the mutually adjusted models, only relative BMI/length/weight (size) remained statistically significant. We found no evidence that any association between velocity and overweight varied by size during 0–24 months or birth weight.
Conclusions:
After mutual adjustment, size during 0–24 months of life (as opposed to birth size), but not velocity or timing of peak velocity, was most consistently associated with overweight in later childhood.
Similar content being viewed by others
Introduction
Body size and growth during infancy and childhood may have lasting effects on adult health.1 Larger birth size and faster growth velocity during infancy and childhood have been associated with increased risk for childhood obesity,2, 3, 4, 5 while small size at birth has been associated with higher risk for cardiovascular disease in adulthood.6, 7 Small size at birth in combination with faster growth velocity may be particularly detrimental and has been associated with obesity and cardiometabolic disease in childhood, adolescence and adulthood.8, 9, 10, 11, 12, 13
Several biological mechanisms have been posited for how size and growth during infancy may affect risk for obesity later in life. Programming or a predictive adaptive response, where cues from the environment cause permanent changes to physiological functioning during certain periods of developmental plasticity is one set of mechanisms through which either small size, small size combined with rapid growth velocity or rapid growth velocity itself is hypothesized to affect health later in life.7, 14, 15, 16 Small size at birth may be indicative of suboptimal intrauterine environments that may create a physiology that is predisposed to energy conservation.15, 16 This fetal or neonatal predictive adaptation is thought to work at the epigenetic level, and animal studies suggest multiple common alterations as a consequence of mismatched fetal and postnatal nutrition environments that result in a physiology that favors an insulin-resistant state and an increased propensity for accumulation of fat mass.13 These alterations include changes to appetite control, taste preference, the hypothalamus, pancreas function and endothelial functioning.13 The programming will be maladaptive if the environment later in life differs substantially from intrauterine environment and this mismatch in environments is the mechanism by which faster growth velocity in combination with smaller size at birth is hypothesized to be particularly detrimental.17
Faster growth velocity, independent of size at birth, is also hypothesized to induce programming as a result of the hyperinsulinemic state caused by overfeeding.18, 19 The mechanisms of faster growth independent of birth size as a trigger for programming or a predictive adaptive response are not as well-studied as those for small size in combination with faster growth, but the idea that programming due to overnutrition or growth may create a predisposition for fat accumulation is commonly held.13, 19 If higher growth velocity programs future obesity, we would expect that children who grew faster than average during infancy, independent of attained size during infancy, would exhibit a greater risk of obesity later in life compared with those who did not grow fast. By contrast, it is also conceivable that rather than a programming mechanism, perhaps just attaining a large size early in life is a marker for increased risk of being obese later not due to programming but rather due to either continued exposure to adequate/surplus nutrition that led to large attained size early in life.
The effects of starting size, growth velocity and attained size can never be completely separated—attained size is the result of starting size and growth velocity, but if children with the same size during infancy experience similar risks for overweight later in life despite different growth velocities during infancy, then programming due to rapid growth during infancy may be a less likely explanation. Additionally, if rapid growth for small children does not result in an increased risk for overweight unless it results in larger than average size during infancy, this is important knowledge for low- and middle-income country (LMIC) contexts in which ‘catch-up growth’ among small children is routinely encouraged for its short-term morbidity and mortality benefits.20, 21
New methods for growth curve analysis combined with repeated measurements of anthropometrics during early childhood can begin to examine how specific aspects of growth trajectories may relate to future disease risk. For example, the recently developed SuperImposition by Translation and Rotation (SITAR), model is capable of estimating growth trajectories and producing child-specific estimates for size, velocity and timing of peak velocity that can be examined jointly to determine their associations with future health outcomes.22
We utilized the SITAR method, in conjunction with a unique data set that contains measurements of infant size approximately every 3–6 months during the first 24 months of life in order to parameterize early childhood growth trajectories. Our primary goal was to assess whether size, velocity and timing of peak velocity of body mass index (BMI) trajectories during 0–24 months were independently associated with future probability of overweight. We also analyzed size, velocity and timing of peak velocity for length and weight trajectories—we included length as growth in length is a recognized public health priority in lower-income countries, and we included weight for comparability to previous literature. We tested whether any association between velocity and overweight varied by overall size or by size at birth. Our hypotheses were that larger than average size and faster than average growth velocity would both be independently associated with increased odds of overweight at age 8 years and that the association between growth velocity and overweight would vary by size. We had no hypotheses about how timing of peak velocity might be associated with overweight.
Methods
Study population
The data came from a birth cohort in a small urban community in Morelos, Mexico. Household surveillance identified all pregnant women during 1998–2000. The intent of the original survey was to identify women early in pregnancy for inclusion in a randomized controlled trial to test the efficacy of a multiple-micronutrient supplement compared with iron supplementation for improving birth outcomes. No differences by treatment were found for the size of the children at birth or 1 month.23 In a follow-up study, at 3 months of age, children were randomly assigned to receive either a multiple-micronutrient supplement or a supplement of iron with vitamin A. Singleton, term children had anthropometric measurements at approximately 1, 3, 6, 9, 12, 18 and 24 months of age. There were no differences in anthropometric outcomes when analyzed by intent-to-treat, but statistically significant differences in length at 24 months were noted among the high compliers.24 A subsample of the children (n=256) were surveyed when they were 4–6 years old and results were previously reported;25 however, these measurements are not used in the current analysis as they are available only for a portion of the children (n=234) who were eventually followed up in 2008. In 2008, an additional follow-up survey targeting the entire sample of children and their mothers was conducted. The current analyses utilized all of the available length and weight measurements from infancy for each child who had weight and length measured in the 2008 survey. In the present study, supplementation group was not associated with our exposure (growth trajectory) or outcome (overweight). A total of 917 children were enrolled at birth; of these, 654 (71%) participated in the 2008 survey. Our analysis included 586 of the 654 children. Missing data came from BMI measurement at age 8 years (n=65) and infant growth parameters (n=3).
The protocols were approved by the National Institute of Public Health in Mexico and by the Center for the Protection of Human Subjects at the University of California, Berkeley, CA, USA. Women signed informed consent for themselves and their children.
Dependent variables
Our primary outcome of interest was overweight status at age 8 years, which was assessed based on a BMI (kg m−2)-for-age z-score >1 s.d. above the age- and sex-specific reference mean according to the WHO Growth Reference 2007.26 Length, height and weight were directly measured in duplicate using portable equipment by staff trained in standard techniques. Children’s weight was measured in light clothing without shoes to the nearest 100 g on a digital Tanita mother–baby scale (model 1582, Tanita Corp., Arlington Heights, IL, USA). Length and height measurements were measured in a standard position with a portable convertible infantometer/stadiometer (Schorr Industries, Glen Burney, MD, USA) and recorded to the nearest millimeter.
Independent variables
We aimed to determine how growth trajectories during infancy, and particularly the aspects of size and velocity, were associated with overweight in later childhood. We used SITAR models to derive estimates of the relative size, velocity and timing of peak velocity for BMI, length and weight trajectories (separately) between birth and 24 months. We focused on this time period because it is a period of very rapid growth and we had closely spaced, serial anthropometric measurements from this period to inform the growth curves.
Our primary anthropometric measurement of interest during 0–24 months was BMI as BMI is an estimate of weight independent of length, has a moderately high correlation with adiposity (that is, r∼0.70),27 performs better than other power indices (that is, kg m−3 or k m−1 and so on) and other anthropometric measurements28 and higher BMI in childhood is associated with increased risk for cardiometabolic disease in adulthood.27 Among children, BMI is correlated with length.29 However, length is also correlated with adiposity in children. We also examined length and weight trajectories during infancy for their associations with overweight later in childhood.
SITAR method to derive trajectory estimates
Described in Cole et al.,22 the SITAR method uses a shape invariant spline curve30 and a nonlinear random-effects model31 to simultaneously estimate an average growth curve for BMI, length and weight (separately) for the entire sample and each individual’s deviation from this average curve on three key aspects, size, velocity and timing of peak velocity. Conceptually, these deviations represent how much bigger or smaller each child is across the entire growth period (size estimate), how much faster or slower the child’s growth velocity is across the entire period (velocity estimate) and how much earlier or later the child experienced peak velocity (timing estimate). Specifically, the model is: yit=ai+ h((t−bi)/(exp(−gi)), where yit is the anthropometric measurement (BMI, length or weight) for subject i at time t, h(t) is a natural cubic spline function of age, and ai, bi, and gi are subject-specific ‘shift’ and ‘scale’ random effects22 that correspond to size, timing of peak velocity and velocity, respectively. The size parameter (ai) shifts the entire curve up or down the y axis (which is size (BMI, length or weight) in these models), similar to a random intercept, the timing parameter (Bi) shifts the curve left or right on the x axis (which is age in these models) to shift the age at peak velocity and the velocity parameter (gi) stretches or compresses the entire curve on the age scale to change the slope of the curve.22 As the estimated random effects (size, velocity and timing) are subject-specific, SITAR derives subject-specific quantitative estimates that characterize the growth trajectory and can then be used as outcomes or exposures in subsequent analyses.
Separate size, velocity and timing of peak velocity variables were created for the BMI, length and weight outcomes (that is, relative BMI (size), BMI velocity, timing of peak BMI velocity; relative length (size), length velocity, timing of peak length velocity; relative weight (size), weight velocity, timing of peak weight velocity). We subtracted the mean and divided by the s.d. for each of the SITAR-derived growth trajectory parameters so that the units were comparable for use in the main statistical models. These variables were approximately normally distributed. In the statistical models, we modeled the SITAR growth trajectory parameters (size, timing and velocity) as continuous variables, after checking for approximately linear associations with the outcome by including a quadratic term for each (which was retained if significant).
Covariates
Confounders were chosen based on a directed acyclic graph of the relationship between infant growth trajectory and overweight status at age 8 years old and included maternal age (calculated from birth date), maternal education level (self-report) and maternal BMI (from measured length and weight during child’s infancy). Vitamin supplementation during the randomized controlled trial in infancy was not included as a confounder as it was not associated with our exposure or outcome. All variables were entered as continuous variables in the regression models. A quadratic term for each was entered in the model to allow for curvilinearity and retained if statistically significant. Multiple imputation32 with 10 data sets was used to impute missing values for each of these covariates in order to avoid excluding children from the analysis who were missing information on covariates (maternal age (imputed n=51), maternal BMI (imputed n=11) and maternal education (imputed n=61)).
Statistical analysis
We estimated means/proportions for anthropometric and demographic variables. All z-scores for anthropometric measurements for infants/children were assessed according to the age- and sex-specific WHO Child Growth Standards.33
As some of the SITAR models were moderately to highly correlated, we investigated whether collinearity was problematic for our proposed logistic regression models by examining variance inflation factors for the final models. The variance inflation factors did not exceed 10 (a commonly used cut-point for diagnosing problematic collinearity34) for any of the variables. We concluded that severe collinearity did not appear to be a problem for the mutually adjusted models. Additionally, as previous research has shown differences according to sex between infant size/growth with later life health, we tested whether the relationship between the SITAR growth trajectory parameters and overweight varied by sex by testing the interactions of the size, velocity and timing parameters with sex. Nonsignificant interaction terms allowed us to estimate sex-pooled models.
We estimated separate models for the association between BMI, length and weight trajectories and overweight using logistic regression. For each anthropometric measure, we regressed overweight on each of the SITAR trajectory parameters (size, velocity, timing) separately, while including confounders. Next, we mutually adjusted for all three SITAR growth parameters and confounders to identify which aspects of the growth trajectory were independently associated with overweight at age eight for each anthropometric measure.
To test the hypothesis that the association between velocity and overweight varied by size, we tested the interaction of size and velocity from the SITAR models. We also tested whether the association between velocity and overweight varied by birth weight z-score (continuous) or low birth weight (birth weight z-score of ⩽2).
Sensitivity analyses
For sensitivity analyses, for purposes of comparison with previous literature, we explored whether our results would be different had we modeled odds of overweight at age 8 years as a function of size at birth (BMI-for-age z-score) and net change in z-score for BMI-for-age. In a separate sensitivity test, we assessed whether the results change substantially if size at birth was included in all of the models. We also tested whether our results were robust to overweight classification using the IOTF (International Obesity Task Force) guidelines.35 To see whether our results were robust to specifying a different time period during infancy, we tested whether our main results would change if we had modeled the growth trajectories from 0–12 months (another commonly used time period in infancy) with SITAR rather than 0–24 months.
Alpha was set to 0.05 for main effects and 0.10 for interactions. SITAR growth curve analyses were performed in R36 using the nlme (nonlinear mixed effect) library.37 All other statistical analyses were performed in Stata 11 (Stata Corporation, College Station, TX, USA).38
Results
Compared with the WHO Child Growth Standards, children were lighter, shorter and thinner than the reference mean at birth (Table 1). At 8 years old, 14% of the sample was stunted (length-for-age <2 s.d. below the reference median) and 33% were overweight or obese (Table 1).
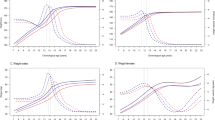
The SITAR models explained a very large portion of the variance in BMI, height and weight between 0–24 months (73, 86 and 85%, respectively). For comparison, a model that includes only birth BMI and change in BMI from 0–24 months explained only 44% of the variance in BMI. The estimated average growth trajectories from the SITAR models for BMI, length and weight are displayed in Figure 1. The s.ds. of the random-effect SITAR parameters (that is, size, velocity, timing) describe the degree of variation around the sample average curve and are shown in dashed lines in Figure 1 (+/−1 s.d.). Of note, the timing of peak velocity (panels 1a, 2b, 3c), which shifts the entire curve left or right, would have different consequences for BMI compared with length and weight due to different curve shapes. For BMI, earlier timing of peak velocity (lower values for timing) would result in an earlier decrease in BMI-for-age. For length and weight, earlier timing of peak velocity would result in an earlier increase in length/weight-for-age.
Average growth curve (solid line) of each SITAR parameter: (1) size, (2) velocity, (3) timing of peak velocity; (a) BMI trajectory, (b) height trajectory, (c) weight trajectory. The s.ds. are displayed as dashed lines. Values for s.ds. in the BMI models were: 1.21 kg m−2 for size, 0.25 fractional units for velocity, 0.56 months for timing; in height models: 2.49 cm, 0.12 fractional units, 1.0 months; in weight models: 1 kg, 0.14 fractional units, 1.14 months.
Early life BMI trajectories and overweight in late childhood
In covariate-adjusted models, the SITAR-derived estimates for relative BMI (size), BMI velocity and timing of peak BMI velocity were each significantly, positively associated with overweight when analyzed individually (Table 2, Models 1–3). In the mutually adjusted model, only the relative BMI was significantly associated with greater odds of overweight at age 8 years (Table 2, Model 4). We found no evidence that the association between BMI velocity and overweight varied by relative BMI (size) during 0–24 months or by birth weight (results not shown).
Early life length trajectories and overweight in late childhood
The SITAR-derived estimates for relative length (size), length velocity and timing of peak length velocity were each significantly associated with greater odds of overweight when analyzed individually. Similar to the results for BMI, in the mutually adjusted models, only relative length was associated with greater odds of overweight (Table 2). There was no evidence that any association between length velocity and overweight varied by relative length during 0–24 months or by birth weight.
Early life weight trajectories and overweight in late childhood
The SITAR-derived estimates for relative weight (size) and relative weight velocity during 0–24 months were both significantly positively associated with overweight at 8 years of age when analyzed individually in adjusted models, whereas relative timing of peak velocity was not significantly associated with overweight (Table 2). In the mutually adjusted models, relative weight was significantly associated with greater odds for overweight. Weight velocity was not significantly associated with odds of overweight. The quadratic term for timing of peak weight velocity was included in the mutually adjusted models due to statistical significance. Post hoc testing indicated that the predicted probability of overweight was lower when the timing of peak velocity was lower or higher than the mean; however, these results were only statistically significant for values higher (but not lower) than the mean, indicating that experiencing peak weight velocity at a later age during early childhood was associated with a decreased probability of overweight later in childhood. Again, we found no evidence that any association between velocity and overweight varied by size for the models of weight trajectories.
Sensitivity analyses
To mirror the typical approach used in this literature (c.f. review Baird et al.5), we modeled odds of overweight as a function of size at birth and net change in z-score between birth and 24 months for BMI and weight (separately). In these models, we found that larger birth size and faster growth were both positively, statistically significantly associated with odds of overweight. We could not additionally include attained size at 24 months in these models as the three measures are collinear. For robustness checks, we (1) used IOTF cut-points for overweight, (2) added size at birth to the models, and (3) examined growth trajectories during 0–12 months only, none of which substantively changed the main findings.
Discussion
We applied the newly developed SITAR method for analyzing and characterizing growth curves to determine how infant/early childhood growth trajectories were associated with odds of childhood overweight. In contrast to standard approaches, our approach allowed for the mutual adjustment of size, velocity and timing of peak velocity of the early life growth trajectory, in order to examine which aspects of growth trajectories were independently associated with overweight later in childhood. For BMI, length and weight trajectories, being relatively larger during 0–24 months of age was associated with greater odds of overweight. In each of the models, after controlling for relative size, BMI velocity, length velocity or weight velocity were not associated with increased odds of overweight in later childhood. We found no evidence that any association between BMI/length/weight velocity and overweight might vary by relative size (BMI/length/weight) in early childhood or by birth weight.
Our finding that size (as indicated by BMI/length/weight) during infancy was most consistently associated with odds of overweight in later childhood is consistent with several studies demonstrating the degree to which children and adolescents tend to track along a particular growth percentile over many years. In a study of approximately 500 000 US children, Binkin et al.39 documented the tendency for children born larger to remain larger and children born smaller to remain smaller from birth to 5 years old. More recently, the strong tendency to track in weight categories (that is, normal weight, overweight, obese) between adolescence and adulthood was demonstrated among a large, nationally representative sample of US teenagers.40, 41 For length in particular, previous repeated cross-sectional findings from high-income countries have shown that taller children are more likely to be overweight/obese42, 43 and birth length has previously been positively associated with BMI in the Philippines.44
In contrast to the hypothesis that being born small and growing fast may be particularly detrimental for adult health,13 we found no evidence that this was the case in our sample. In LMIC undergoing rapid nutrition transitions, a substantial portion of the population may experience growth restriction in utero or infancy followed by exposure to an abundant food environment later in life. Only two other studies have tested whether the association between velocity and overweight varies by size at birth in LMIC. Contrary to our null findings, previous work in a subset of our sample in Mexico found that the association between growth velocity and overweight at age 4–6 years varied by birth size.25 The authors reported that having higher growth velocity during the first year of life (compared with lower growth velocity) was associated with increased odds of obesity only among infants born small or normal size. For infants born larger, high velocity did not significantly increase risk for overweight. There are a number of possible reasons for the difference in findings within a subset of children in the same study. These explanations include (1) different parameterization of size and growth (that is, use of starting size and subsequent net change in anthropometric z-score vs SITAR method), (2) different sample (only 161 children had complete covariates for the analyses of overweight at age 4–6 years), (3) difference in reference growth charts and time period analyzed during early childhood, and (4) difference in the timing of the outcome measure (that is, at age 4–6 years vs age 7–9 years). As we have access to the data from the previous analysis, we have explored likely explanations, post hoc. First, we tested whether this difference is purely a change in this relationship over time, (that is, explanation listed in (4)—that the relationship that was seen with overweight at age 4–6 years was no longer apparent at age 7–9 years, even among the same children using the same method). We restricted the sample to only children who had been included in the previous analysis and also had BMI measurements at age 7–9 years (n=148) and used the conventional model and confounders used in the previous paper. We found that the previously reported significant interaction between growth velocity and birth size in their association with overweight at age 4–6 years was apparent as expected (P for interaction=0.01); however, this same interaction with the same sample was no longer significant when examining overweight at age 7–9 years (P for interaction=0.78). Among this sample, the relationships between growth velocity and starting size and subsequent overweight/obesity are different depending on how much later in life overweight/obesity is measured. The one other study, to our knowledge, in a LMIC to examine whether the effects of growth velocity on overweight or obesity varied by birth size found that the interaction between rapid growth and birth size was not statistically significant,45 which is similar to our findings with older ages using the conventional model.
In contrast to many studies that emphasize the importance of growth during early childhood as a risk factor for future overweight and obesity, our results emphasize size as a risk factor. However, at least some of this difference is simply due to statistical modeling choices and interpretation, rather than biological mechanism. In sensitivity analyses, we use the more traditional approach of modeling birth weight and the net change in weight/bmi z-score from birth until 24 months. Using this approach, we also find that velocity is positively associated with overweight risk. In conventional models, the researcher must choose to either include starting size and growth or starting size and subsequent size, as starting size plus growth equals subsequent size, and these three aspects cannot be modeled concurrently in traditional models. Even when stating size and subsequent size is modeled, often the interpretation has focused on growth velocity as the mechanism, rather than size. Using the SITAR method, although individual-specific estimates for relative size, velocity and time are derived and, in theory, their independent association with overweight risk can be obtained, the fact remains that we are relying on a statistical separation of two entwined processes. Additionally, the SITAR method uses mean size over the period 0–24 months, so some of the velocity effect is captured in the size effect. This parameterization de-emphasizes the role of velocity. Both approaches are valid, and their differing results emphasize that the choice of statistical model can influence conclusions.
Using a statistical model that attempts to parse three key aspects of growth, our findings are less consistent with the idea that rapid growth during 0–24 months programs future obesity.46, 47, 48 A recent study also using nontraditional methods, also suggests that almost all of the association between growth and hypertension is mediated through body size.49 We should note that our outcome of overweight is one of size, so it is certainly possible that size during early life is particularly relevant for large size later in childhood and that this may not be the case for other outcomes, such as glucose intolerance or hypertension.
Our statistical technique, which involved multiple measurements and a smoothed subject-specific trajectory of growth, enabled us to begin to investigate the independent contribution of size, growth velocity and timing of peak velocity on future risk of overweight. The SITAR method offers advantages over alternative longitudinal growth modeling methods. First, it enables use of all available data without excluding subjects who may be missing one or more anthropometric measurements. This differs from using conditional weights with regression models, which also offer the advantage of including multiple repeated measurements, but are limited to subjects who have been measured at all time periods. Latent class growth modeling is an alternative approach that considers the entire growth trajectory; however, this method results in a qualitative description of the growth pattern and membership in a trajectory class, but it does not quantify any key aspects of growth for each individual. The SITAR method is similar to a random intercept, random coefficient growth curve with a piecewise cubic spline to model size-for-age; however, by utilizing a shape invariant model and estimating each child’s deviation from that mean curve with three random effects that correspond to size, velocity and timing, we find the SITAR model to be more parsimonious and interpretable.
There are limitations to our study. First, BMI is not a direct measure of adiposity; however, among children, BMI is correlated with adiposity and future cardiometabolic disease biomarkers.27, 50 Second, we cannot control for pubertal stage, which could theoretically be a confounder or a mediator. However, the majority of our sample was likely prepubescent at follow-up as average age was 8 (s.d. 0.83) years old, and the recent estimates from a sample of Mexican Americans suggest mean age of entry into puberty is 10.4 years for girls.51 Third, some loss to follow-up occurred. We tested for differences in observed means in mean birth weight, birth BMI, birth length, mother’s age, education and maternal BMI, and there were no statistical differences between children enrolled at birth and those who were included in the follow-up. Six of the nine SITAR parameters were also not significantly different. We have no reason to believe that the relationship of interest would be different among those lost to follow-up. Fifth, our infant growth trajectories cover the period from 0–24 months. It is possible that a different time period during very early infancy (for example, 0–3 months19) may be most relevant for velocity in influencing overweight risk.19 Additional studies using SITAR with closely spaced measurements during very early infancy could address this question.
Conclusions
This study utilized data from a 10-year longitudinal study in Mexico that included up to eight measurements of anthropometrics between 0–24 months. We combined this unique data with the SITAR method to determine which aspects of the 0–24-month growth trajectory were independently associated with overweight in late childhood. Our main finding that size, rather than velocity or timing of peak velocity, was most consistently associated with higher odds of overweight. Attained size is likely particularly important for outcomes that are also classified by size, such as overweight, and it will be important to conduct similar analyses with additional measures of adiposity and with cardiometabolic outcomes as well.
References
Singhal A, Lucas A . Early origins of cardiovascular disease: is there a unifying hypothesis? Lancet 2004; 363: 1642–1645.
Taveras EM, Rifas-Shiman SL, Belfort MB, Kleinman KP, Oken E, Gillman MW . Weight status in the first 6 months of life and obesity at 3 years of age. Pediatrics 2009; 123: 1177–1183.
Oken E, Gillman MW . Fetal origins of obesity. Obes Res 2003; 11: 496–506.
Gillman MW, Rifas-Shiman SL, Belfort MB, Kleinman K, Oken E, Taveras EM . Size at birth, infant growth, and obesity at age 3 years. Early Hum Dev 2007; 83: S160–S160.
Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C . Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ 2005; 331: 929–931.
Roseboom TJ, van der Meulen JHP, Osmond C, Barker DJP, Ravelli ACJ, Schroeder-Tanka JM et al. Coronary heart disease after prenatal exposure to the Dutch famine, 1944-45. Heart 2000; 84: 595–598.
Barker DJP . Fetal origins of coronary heart-disease. BMJ 1995; 311: 171–174.
Jones-Smith JC, Fernald LCH, Neufeld LM . Birth size and accelerated growth during infancy are associated with increased odds of childhood overweight in Mexican children. J Am Diet Assoc 2007; 107: 2061–2069.
Bhargava SK, Sachdev HS, Fall CHD, Osmond C, Lakshmy R, Barker DJP et al. Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. N Engl J Med 2004; 350: 865–875.
Eriksson JG, Forsen T, Tuomilehto J, Winter PD, Osmond C, Barker DJP . Catch-up growth in childhood and death from coronary heart disease: longitudinal study. BMJ 1999; 318: 427–431.
Adair LS, Cole TJ . Rapid child growth raises blood pressure in adolescent boys who were thin at birth. Hypertension 2003; 41: 451–456.
Gluckman PD, Cutfield W, Hofman P, Hanson MA . The fetal, neonatal, and infant environments - the long-term consequences for disease risk. Early Hum Dev 2005; 81: 51–59.
Gluckman PD, Hanson MA, Beedle AS, Raubenheimer D . Fetal and neonatal pathways to obesity. Obes Metab 2008; 36: 61–72.
Hanson M, Godfrey KM, Lillycrop KA, Burdge GC, Gluckman PD . Developmental plasticity and developmental origins of non-communicable disease: Theoretical considerations and epigenetic mechanisms. Prog Biophys Mol Biol 2011; 106: 272–280.
Hales CN, Barker DJ . Type 2 (non-insulin-dependent) diabetes mellitus: the thrifty phenotype hypothesis. Diabetologia 1992; 35: 595–601.
Hales CN, Barker DJ . The thrifty phenotype hypothesis. Br Med Bull 2001; 60: 5–20.
Gluckman PD, Hanson MA, Beedle AS, Raubenheimer D . Fetal and neonatal pathways to obesity. Front Horm Res. [Review] 2008; 36: 61–72.
Gluckman PD, Hanson MA . Developmental and epigenetic pathways to obesity: an evolutionary-developmental perspective. Int J Obes 2008; 32 (Suppl 7): S62–S71.
Singhal A, Kennedy K, Lanigan J, Fewtrell M, Cole TJ, Stephenson T et al. Nutrition in infancy and long-term risk of obesity: evidence from 2 randomized controlled trials. Am J Clin Nutr 2010; 92: 1133–1144.
Adair LS, Prentice AM . A critical evaluation of the fetal origins hypothesis and its implications for developing countries. J Nutr 2004; 134: 191–193.
Victora CG, Barros FC . Commentary: the catch-up dilemma - relevance of Leitch’s ‘low-high’ pig to child growth in developing countries. Int J Epidemiol 2001; 30: 217–220.
Cole TJ, Donaldson MDC, Ben-Shlomo Y . SITAR—a useful instrument for growth curve analysis. Int J Epidemiol 2010; 39: 1558–1566.
Ramakrishnan U, Gonzalez-Cossio T, Neufeld LM, Rivera J, Martorell R . Multiple micronutrient supplementation during pregnancy does not lead to greater infant birth size than does iron-only supplementation: a randomized controlled trial in a semirural community in Mexico. Am J Clin Nutr 2003; 77: 720–725.
Ramakrishnan U, Neufeld LM, Flores R, Rivera J, Martorell R . Multiple micronutrient supplementation during early childhood increases child size at 2 y of age only among high compliers. Am J Clin Nutr 2009; 89: 1125–1131.
Jones-Smith JC, Fernald LC, Neufeld LM . Birth size and accelerated growth during infancy are associated with increased odds of childhood overweight in Mexican children. J Am Diet Assoc 2007; 107: 2061–2069.
de Onis M, Lobstein T . Defining obesity risk status in the general childhood population: Which cut-offs should we use? Int J Pediatr Obes [Editorial Material] 2010; 5: 458–460.
Freedman DS, Sherry B . The validity of BMI as an indicator of body fatness and risk among children. Pediatrics [Validation Studies] 2009; 124 (Suppl 1): S23–S34.
Cole TJ, Freeman JV, Preece MA . Body mass index reference curves for the UK, 1990. Arch Dis Child 1995; 73: 25–29.
Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS . Inter-relationships among childhood BMI, childhood height, and adult obesity: the Bogalusa Heart Study. Int J Obes Relat Metab Disord 2004; 28: 10–16.
Lindstrom MJ . Self modelling with random shift and scale parameters and a free knot spline shape function. Stat Med 1995; 14: 2009–2021.
Pinheiro JC, Bates DM . Mixed-effects models in S and S-PLUS. Springer Verlag: New York, NY, 2009.
Sterne JAC, White IR, Carlin JB, Spratt M, Royston P, Kenward MG et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 2009; 338: b2393.
Borghi E, de Onis M, Garza C, Van den Broeek J, Frongillo EA, Grummer-Strawn L et al. Construction of the World Health Organization child growth standards: selection of methods for attained growth curves. Stat Med 2006; 25: 247–265.
O’brien RM . A caution regarding rules of thumb for variance inflation factors. Qual Quantity 2007; 41: 673–690.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320: 1240–1243.
Team RDC. R: A language and environment for statistical computing. R Foundation for Statistical Computing. ISBN: Vienna, Austria, 3–900051 2009.
Pinheiro J, Bates D, DebRoy S, Sarkar D, the R Core team 2008 nlme: linear and nonlinear mixed effects models R package version 2008; 3: 1–89.
Stata Corporation. Stata Statistical Software. Release 11.0 ed. Texas Station, 2009.
Binkin NJ, Yip R, Fleshood L, Trowbridge FL . Birth weight and childhood growth. Pediatrics 1988; 82: 828.
Gordon-Larsen P, The NS, Adair LS . Longitudinal trends in obesity in the United States from adolescence to the third decade of life. Obesity (Silver Spring) 2010; 18: 1801–1804.
The NS, Suchindran C, North KE, Popkin BM, Gordon-Larsen P . Association of adolescent obesity with risk of severe obesity in adulthood. JAMA 2010; 304: 2042–2047.
Buchan IE, Bundred PE, Kitchiner DJ, Cole TJ . Body mass index has risen more steeply in tall than in short 3-year olds: serial cross-sectional surveys 1988, Äì2003. Int J Obes 2006; 31: 23–29.
Jason EM . Socioeconomic status, height, and obesity in children. Econ Human Biol 2009; 7: 376–386.
Adair LS . Size at birth and growth trajectories to young adulthood. Am J Hum Biol 2007; 19: 327–337.
Monteiro POA, Victora CG, Barros FC, Monteiro LMA . Birth size, early childhood growth, and adolescent obesity in a Brazilian birth cohort. Int J Obes 2003; 27: 1274–1282.
Godfrey KM, Sheppard A, Gluckman PD, Lillycrop KA, Burdge GC, McLean C et al. Epigenetic gene promoter methylation at birth is associated with child’s later adiposity. Diabetes 2011; 60: 1528–1534.
Muhlhausler BS, Adam CL, Findlay PA, Duffield JA, McMillen IC . Increased maternal nutrition alters development of the appetite-regulating network in the brain. FASEB J 2006; 20: 1257–1259.
McMillen IC, Edwards LJ, Duffield J, Muhlhausler BS . Regulation of leptin synthesis and secretion before birth: implications for the early programming of adult obesity. Reproduction 2006; 131: 415–427.
Tilling K, Davies N, Windmeijer F, Kramer MS, Bogdanovich N, Matush L et al. Is infant weight associated with childhood blood pressure? Analysis of the Promotion of Breastfeeding Intervention Trial (PROBIT) cohort. Int J Epidemiol 2011; 40: 1227–1237.
Dietz WH, Bellizzi MC . Introduction: the use of body mass index to assess obesity in children. Am J Clin Nutr 1999; 70: 123S–125SS.
Sun SS, Schubert CM, Chumlea WC, Roche AF, Kulin HE, Lee PA et al. National estimates of the timing of sexual maturation and racial differences among US children. Pediatrics 2002; 110: 911–919.
Acknowledgements
Funding for this study was provided by Eunice Kennedy Shriver National Institute of Child Health and Human Development R21 HD056581. We are grateful to Tim Cole for providing his assistance with R programs to run SITAR models and helpful guidance on model implementation. Any errors are those of the authors alone.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Jones-Smith, J., Neufeld, L., Laraia, B. et al. Early life growth trajectories and future risk for overweight. Nutr & Diabetes 3, e60 (2013). https://doi.org/10.1038/nutd.2012.32
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nutd.2012.32
Keywords
This article is cited by
-
Ethnoracial disparities in childhood growth trajectories in Brazil: a longitudinal nationwide study of four million children
BMC Pediatrics (2024)
-
Longitudinal association between the timing of adiposity peak and rebound and overweight at seven years of age
BMC Pediatrics (2022)
-
Adherence to index-based dietary patterns in childhood and BMI trajectory during the transition to adolescence: the EPOCH study
International Journal of Obesity (2021)
-
Maternal urinary concentrations of organophosphate ester metabolites: associations with gestational weight gain, early life anthropometry, and infant eating behaviors among mothers-infant pairs in Rhode Island
Environmental Health (2020)
-
Family Spirit Nurture (FSN) – a randomized controlled trial to prevent early childhood obesity in American Indian populations: trial rationale and study protocol
BMC Obesity (2019)