Abstract
Although warfarin is the most widely used anticoagulant worldwide, the mechanism by which warfarin inhibits its target, human vitamin K epoxide reductase (hVKOR), remains unclear. Here we show that warfarin blocks a dynamic electron-transfer process in hVKOR. A major fraction of cellular hVKOR is in an intermediate redox state containing a Cys51-Cys132 disulfide, a characteristic accommodated by a four-transmembrane-helix structure of hVKOR. Warfarin selectively inhibits this major cellular form of hVKOR, whereas disruption of the Cys51-Cys132 disulfide impairs warfarin binding and causes warfarin resistance. Relying on binding interactions identified by cysteine alkylation footprinting and mass spectrometry coupled with mutagenesis analysis, we conducted structure simulations, which revealed a closed warfarin-binding pocket stabilized by the Cys51-Cys132 linkage. Understanding the selective warfarin inhibition of a specific redox state of hVKOR should enable the rational design of drugs that exploit the redox chemistry and associated conformational changes in hVKOR.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Pirmohamed, M. Warfarin: almost 60 years old and still causing problems. Br. J. Clin. Pharmacol. 62, 509–511 (2006).
Rost, S. et al. Mutations in VKORC1 cause warfarin resistance and multiple coagulation factor deficiency type 2. Nature 427, 537–541 (2004).
Li, T. et al. Identification of the gene for vitamin K epoxide reductase. Nature 427, 541–544 (2004).
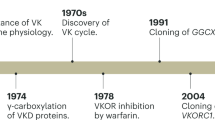
Tie, J.-K. & Stafford, D.W. Structure and function of vitamin K epoxide reductase. Vitam. Horm. 78, 103–130 (2008).
Chu, P.-H., Huang, T.-Y., Williams, J. & Stafford, D.W. Purified vitamin K epoxide reductase alone is sufficient for conversion of vitamin K epoxide to vitamin K and vitamin K to vitamin KH2. Proc. Natl. Acad. Sci. USA 103, 19308–19313 (2006).
Hildebrandt, E.F., Preusch, P.C., Patterson, J.L. & Suttie, J.W. Solubilization and characterization of vitamin K epoxide reductase from normal and warfarin-resistant rat liver microsomes. Arch. Biochem. Biophys. 228, 480–492 (1984).
Bügel, S. Vitamin K and bone health in adult humans. Vitam. Horm. 78, 393–416 (2008).
Karsenty, G. & Ferron, M. The contribution of bone to whole-organism physiology. Nature 481, 314–320 (2012).
Berkner, K.L. Vitamin K-dependent carboxylation. Vitam. Horm. 78, 131–156 (2008).
Oldenburg, J., Marinova, M., Müller-Reible, C. & Watzka, M. The vitamin K cycle. Vitam. Horm. 78, 35–62 (2008).
Tie, J.K., Jin, D.Y., Tie, K. & Stafford, D.W. Evaluation of warfarin resistance using transcription activator-like effector nucleases-mediated vitamin K epoxide reductase knockout HEK293 cells. J. Thromb. Haemost. 11, 1556–1564 (2013).
Li, W. et al. Structure of a bacterial homologue of vitamin K epoxide reductase. Nature 463, 507–512 (2010).
Rishavy, M.A., Usubalieva, A., Hallgren, K.W. & Berkner, K.L. Novel insight into the mechanism of the vitamin K oxidoreductase (VKOR): electron relay through Cys43 and Cys51 reduces VKOR to allow vitamin K reduction and facilitation of vitamin K-dependent protein carboxylation. J. Biol. Chem. 286, 7267–7278 (2011).
Tie, J.K., Nicchitta, C., von Heijne, G. & Stafford, D.W. Membrane topology mapping of vitamin K epoxide reductase by in vitro translation/cotranslocation. J. Biol. Chem. 280, 16410–16416 (2005).
Carlisle, T.L. & Suttie, J.W. Vitamin K dependent carboxylase: subcellular location of the carboxylase and enzymes involved in vitamin K metabolism in rat liver. Biochemistry 19, 1161–1167 (1980).
Tie, J.-K., Jin, D.-Y. & Stafford, D.W. Human vitamin K epoxide reductase and its bacterial homologue have different membrane topologies and reaction mechanisms. J. Biol. Chem. 287, 33945–33955 (2012).
Chen, D., Cousins, E., Sandford, G. & Nicholas, J. Human herpesvirus 8 viral interleukin-6 interacts with splice variant 2 of vitamin K epoxide reductase complex subunit 1. J. Virol. 86, 1577–1588 (2012).
Tie, J.K., Jin, D.Y. & Stafford, D.W. Conserved loop cysteines of vitamin K epoxide reductase complex subunit 1-like 1 (VKORC1L1) are involved in its active site regeneration. J. Biol. Chem. 289, 9396–9407 (2014).
Silverman, R.B. Model studies for a molecular mechanism of action of oral anticoagulants. J. Am. Chem. Soc. 103, 3910–3915 (1981).
Fasco, M.J. & Principe, L.M. R- and S-Warfarin inhibition of vitamin K and vitamin K 2,3-epoxide reductase activities in the rat. J. Biol. Chem. 257, 4894–4901 (1982).
Fasco, M.J., Principe, L.M., Walsh, W.A. & Friedman, P.A. Warfarin inhibition of vitamin K 2,3-epoxide reductase in rat liver microsomes. Biochemistry 22, 5655–5660 (1983).
Watzka, M. et al. Thirteen novel VKORC1 mutations associated with oral anticoagulant resistance: insights into improved patient diagnosis and treatment. J. Thromb. Haemost. 9, 109–118 (2011).
Rieder, M.J. et al. Effect of VKORC1 haplotypes on transcriptional regulation and warfarin dose. N. Engl. J. Med. 352, 2285–2293 (2005).
Rost, S. et al. Novel mutations in the VKORC1 gene of wild rats and mice: a response to 50 years of selection pressure by warfarin? BMC Genet. 10, 4 (2009).
Hodroge, A., Longin-Sauvageon, C., Fourel, I., Benoit, E. & Lattard, V. Biochemical characterization of spontaneous mutants of rat VKORC1 involved in the resistance to antivitamin K anticoagulants. Arch. Biochem. Biophys. 515, 14–20 (2011).
Pelz, H.J. et al. The genetic basis of resistance to anticoagulants in rodents. Genetics 170, 1839–1847 (2005).
Czogalla, K.J. et al. Human VKORC1 mutations cause variable degrees of 4-hydroxycoumarin resistance and affect putative warfarin binding interfaces. Blood 122, 2743–2750 (2013).
Liu, S., Cheng, W., Fowle Grider, R., Shen, G. & Li, W. Structures of an intramembrane vitamin K epoxide reductase homolog reveal control mechanisms for electron transfer. Nat. Commun. 5, 3110 (2014).
Schulman, S., Wang, B., Li, W. & Rapoport, T.A. Vitamin K epoxide reductase prefers ER membrane-anchored thioredoxin-like redox partners. Proc. Natl. Acad. Sci. USA 107, 15027–15032 (2010).
Cao, Z. et al. The membrane topology of vitamin K epoxide reductase is conserved between human isoforms and the bacterial enzyme. Biochem. J. 473, 851–858 (2016).
Lee, H. & Kim, H. Membrane topology of transmembrane proteins: determinants and experimental tools. Biochem. Biophys. Res. Commun. 453, 268–276 (2014).
von Heijne, G. Membrane-protein topology. Nat. Rev. Mol. Cell Biol. 7, 909–918 (2006).
Sevier, C.S. & Kaiser, C.A. Formation and transfer of disulphide bonds in living cells. Nat. Rev. Mol. Cell Biol. 3, 836–847 (2002).
Su, D. et al. Interactions of apurinic/apyrimidinic endonuclease with a redox inhibitor: evidence for an alternate conformation of the enzyme. Biochemistry 50, 82–92 (2011).
Goodstadt, L. & Ponting, C.P. Vitamin K epoxide reductase: homology, active site and catalytic mechanism. Trends Biochem. Sci. 29, 289–292 (2004).
Jin, D.Y., Tie, J.K. & Stafford, D.W. The conversion of vitamin K epoxide to vitamin K quinone and vitamin K quinone to vitamin K hydroquinone uses the same active site cysteines. Biochemistry 46, 7279–7283 (2007).
Rost, S. et al. Site-directed mutagenesis of coumarin-type anticoagulant-sensitive VKORC1: evidence that highly conserved amino acids define structural requirements for enzymatic activity and inhibition by warfarin. Thromb. Haemost. 94, 780–786 (2005).
Brach, T. et al. Non-invasive topology analysis of membrane proteins in the secretory pathway. Plant J. 57, 534–541 (2009).
van Geest, M. & Lolkema, J.S. Membrane topology and insertion of membrane proteins: search for topogenic signals. Microbiol. Mol. Biol. Rev. 64, 13–33 (2000).
Silverman, R.B. & Nandi, D.L. Reduced thioredoxin: a possible physiological cofactor for vitamin K epoxide reductase. Further support for an active site disulfide. Biochem. Biophys. Res. Commun. 155, 1248–1254 (1988).
Soute, B.A., Groenen-van Dooren, M.M., Holmgren, A., Lundström, J. & Vermeer, C. Stimulation of the dithiol-dependent reductases in the vitamin K cycle by the thioredoxin system: strong synergistic effects with protein disulphide-isomerase. Biochem. J. 281, 255–259 (1992).
Preusch, P.C. Is thioredoxin the physiological vitamin K epoxide reducing agent? FEBS Lett. 305, 257–259 (1992).
Bevans, C.G. et al. Determination of the warfarin inhibition constant Ki for vitamin K 2,3-epoxide reductase complex subunit-1 (VKORC1) using an in vitro DTT-driven assay. Biochim. Biophys. Acta 1830, 4202–4210 (2013).
Fregin, A. et al. A new cell culture-based assay quantifies vitamin K 2,3-epoxide reductase complex subunit 1 function and reveals warfarin resistance phenotypes not shown by the dithiothreitol-driven VKOR assay. J. Thromb. Haemost. 11, 872–880 (2013).
Fasco, M.J. & Principe, L.M. Vitamin K1 hydroquinone formation catalyzed by a microsomal reductase system. Biochem. Biophys. Res. 97, 1487–1492 (1980).
Wanrooij, S., Goffart, S., Pohjoismäki, J.L.O., Yasukawa, T. & Spelbrink, J.N. Expression of catalytic mutants of the mtDNA helicase Twinkle and polymerase POLG causes distinct replication stalling phenotypes. Nucleic Acids Res. 35, 3238–3251 (2007).
Jessop, C.E., Watkins, R.H., Simmons, J.J., Tasab, M. & Bulleid, N.J. Protein disulphide isomerase family members show distinct substrate specificity: P5 is targeted to BiP client proteins. J. Cell Sci. 122, 4287–4295 (2009).
Wang, Y., Toei, M. & Forgac, M. Analysis of the membrane topology of transmembrane segments in the C-terminal hydrophobic domain of the yeast vacuolar ATPase subunit a (Vph1p) by chemical modification. J. Biol. Chem. 283, 20696–20702 (2008).
Shevchenko, A., Tomas, H., Havlis, J., Olsen, J.V. & Mann, M. In-gel digestion for mass spectrometric characterization of proteins and proteomes. Nat. Protoc. 1, 2856–2860 (2006).
Liu, H. et al. Phycobilisomes supply excitations to both photosystems in a megacomplex in cyanobacteria. Science 342, 1104–1107 (2013).
Walzthoeni, T. et al. False discovery rate estimation for cross-linked peptides identified by mass spectrometry. Nat. Methods 9, 901–903 (2012).
Roy, A., Kucukural, A. & Zhang, Y. I-TASSER: a unified platform for automated protein structure and function prediction. Nat. Protoc. 5, 725–738 (2010).
Grosdidier, A., Zoete, V. & Michielin, O. SwissDock, a protein-small molecule docking web service based on EADock DSS. Nucleic Acids Res. 39, W270–W277 (2011).
Vanommeslaeghe, K. et al. CHARMM general force field: a force field for drug-like molecules compatible with the CHARMM all-atom additive biological force fields. J. Comput. Chem. 31, 671–690 (2010).
Van Der Spoel, D. et al. GROMACS: fast, flexible, and free. J. Comput. Chem. 26, 1701–1718 (2005).
Acknowledgements
We thank D.W. Stafford, J. Tie, and D. Jin (University of North Carolina) for their gift of double-knockout cell lines used in activity assays and for their generous help in the assay protocol; S. Wanrooij (Umeå University) for the gift of the T-REx-293 cell line and the protocol for establishing stable cell lines; J. Tie, D.W. Stafford, S. Liu and T. Ellenberger for critical reading of the manuscript. H.Z. is supported by the DOE (DE-SC0001035 to PARC). W.H. is supported by the China Scholarship Council (201206235027). G.R.B. is supported by a BWF Career Award. J.E.S. is supported by the NIH NHLBI (R01 HL130446 and U54 HL112303). M.L.G. is supported by the NIH NIGMS (P41 GM103422), which financed the MS measurements. W.L. is supported by the NHLBI (R01 HL121718), the AHA (grant-in-aid 14GRNT20310017) and an ASH Scholar Award.
Author information
Authors and Affiliations
Contributions
G.S., H.Z., W.C., J.E.S., M.L.G. and W.L. conceived the studies. G.S. designed and performed experiments with contributions from W.C., W.H., H.Z., Q.L., Y.Y., S.L., J.E.S. and W.L. W.C., G.S., H.Z. and W.L. analyzed the data. F.Z. performed MD simulation with assistance from G.R.B. W.L., G.S., M.L.G. and J.E.S. wrote the manuscript with input from the team.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
Supplementary Figure 1 Cys51-Cys132 is an intramolecular disulfide bond.
(a) The wild-type hVKOR protein shows a monomeric band on a non-reducing SDS-PAGE gel. To prevent disulfide shuffling, the cells were treated with NEM to block reactive free cysteines. Uncropped blot/gel images are shown in Supplementary Data Set 2. (b-c) Cys51-Cys132 linked peptides of various lengths (in addition to Fig. 2c,d) have been identified by mass measurements before and after reduction of the disulfide bond (left), and by MS/MS (right). (d) Cys51-Cys132 is preserved in a C43A C135A double mutant, which eliminates alternative ways of forming disulfide bonds between the four conserved cysteines, so that Cys51-Cys132 becomes the only possible form (see inset). Both Cys51 and Cys132 are oxidized in this double mutant, and both can be reduced by DTT (as wild-type hVKOR in Fig. 2b). Error bars, same analysis as in Fig. 2b. MS and MS/MS spectra can be found in Supplementary Data Set 1. (e) A Cys51-Cys132 linked peptide is identified in this double mutant.
Supplementary Figure 2 The electron-transfer pathway and associated conformational changes.
(a) Scheme of an electron transfer pathway proposed to regenerate hVKOR activity. The observed oxidation level of each conserved cysteine (Figs. 2b, 3, and 4) reflects a combination of different redox states in this pathway. State I: a pair of free cysteines (green) from a redox partner reduces (blue arrow) the Cys43-Cys51 disulfide (red) in fully oxidized hVKOR. State II to III: electron transfer (blue arrows) generates alternative disulfide bonds (red bars) and Cys51-Cys132 is formed as an intermediate state (III). State IV to V: all cysteines are reduced and hVKOR is catalytically active to reduce KO. State V to I: Reduction of KO (KO to K and K to hydroquinone KH2) generates the Cys132-Cys135 disulfide, and the Cys43-Cys51 disulfide (as in Fig. 4b-e), thereby regenerating State I. (b) Electron transfer is associated with conformational changes in the crystal structures of a bacterial VKOR homolog. Left, A C56A mutant (corresponding to C51A in hVKOR; in parentheses) generates a structure (PDB code: 3KP9) with the Cys130-Cys133 disulfide (Cys132-Cys135 in hVKOR). Right, A C50A mutant (C43A in hVKOR) generates a structure (PDB code: 4NV2 and 4NV5) with the Cys56-Cys130 disulfide (Cys51-Cys132 in hVKOR). Comparison of these two structures shows that the formation of different disulfide bonds (during electron transfer as in a) is associated with conformational changes in HL1-2 (red). In particular, the N-terminal part of the short helix alternates between extended (left) and helical (right) conformations, which directly change the VKOR active site.
Supplementary Figure 3 Cysteine mutations result in a predictable pattern of redox changes in hVKOR.
(a) Redox changes after cysteine mutations (for comparison, Fig. 3c shows only the four conserved cysteines). Error bars, same analysis as in Fig. 2b. MS and MS/MS spectra can be found in Supplementary Data Set 1. (b) Predictions (left) based on a redistribution mechanism (Supplementary Note) fit well with the observed redox changes (right) after cysteine mutations. The P values from two-tailed Student t test (right) are calculated by comparing the changes between mutants and wild-type (observed in a); the values are shown in green for cysteines that become more reduced, in red for those that become more oxidized, and in black for insignificant changes.
Supplementary Figure 4 Cysteine mutations block substrate-induced oxidation through electron transfer.
The KO treatment is 5 h and these mutants are analyzed in the same way as for the wild-type hVKOR in Fig. 4. The red arrows indicate the direction of oxidation and the cross signs indicate mutations. All subsequent oxidation in the pathway are blocked by the mutation of conserved cysteines (right). In contrast, mutation of non-conserved cysteines (left) has no effect. Error bars, same analysis as in Fig. 2b. MS and MS/MS spectra can be found in Supplementary Data Set 1.
Supplementary Figure 5 MS analysis of cysteine protection induced by warfarin binding.
(a) The untreated and warfarin-treated wild-type hVKOR were alkylated with NEM and compared by quantitative MS. Warfarin inhibits the alkylation of four cysteines (**P < 0.001, ***P < 0.0001) in hVKOR. Error bars, same analysis as in Fig. 2b. (b) Cysteine mutations change the pattern of warfarin-induced protection. Wild-type hVKOR (data from a) and each cysteine mutant was monitored for the change in NEM alkylation of individual cysteines induced by warfarin binding. Each bar shows the difference (as in Fig. 6c) between apparent oxidation levels for warfarin-treated samples and untreated samples. Mutations of C51A, C132A, and C135A block warfarin-induced changes (**P < 0.001, ***P < 0.0001; compared with wild type), thereby confirming the gel shift analyses (Fig. 5c) indicating that these mutations interfere with warfarin binding. In contrast, C43A, C16A, C85A, and C96A mutations have insignificant effects. Error bars, same analysis as in Fig. 2b but with error propagation calculated for the subtraction. MS and MS/MS spectra can be found in Supplementary Data Set 1.
Supplementary Figure 6 The Cys51-Cys132 disulfide is important for warfarin binding.
(a) Cysteine mutations were tested for warfarin-induced gel shift as control experiments for Fig. 5c. Uncropped blot/gel images are shown in Supplementary Data Set 2. (b) The activity of cysteine mutants. C132A and C135A are inactive mutants because they delete active site residues. The activity of C43A is also low and does not allow reliable analysis for warfarin resistance in Fig. 5d. Error bars defined in Online Methods. Source data for basal activity are available in Supplementary Data Set 4.
Supplementary Figure 7 Confirming the MD-predicted warfarin-binding pocket by clustering of WRs.
(a) Novel WRs identified by alanine scanning mutagenesis (orange) and naturally occurring WRs (blue) together indicate that the warfarin binding region is located at the luminal portion of the hVKOR protein according to the four-TM model (bars below). These data are shown as a heat map in Fig. 7a. Error bars defined in Online Methods. Source data for resistance and basal activity are available in Supplementary Data Set 3, 4. (b) Strong WR residues are highly conserved in eukaryotic VKOR homolog proteins. The sequences of these proteins were generated from the Psi-Blast search of the human VKOR against eukaryotic proteins in a non-redundant NCBI database. Top 500 sequences from the search were used to plot the sequence logo.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–7 and Supplementary Note (PDF 1637 kb)
Supplementary Data Set 1
MS and product-ion (MS/MS) spectra of all the cysteine-containing peptides. (PDF 4490 kb)
Supplementary Data Set 2
Uncropped western blots. (PDF 13897 kb)
Supplementary Data Set 3
Inhibition and resistance. (XLSX 25 kb)
Supplementary Data Set 4
Basal activity. (XLSX 14 kb)
Supplementary Data Set 5
Coordinates of a representative structure from an ensemble generated via molecular dynamics simulation of hVKOR with warfarin. (TXT 3130 kb)
Supplementary Data Set 6
PDB validation report for the hVKOR model. (PDF 111 kb)
The warfarin-binding pocket.
Warfarin binds to HL1-2 and luminal part of the transmembrane helices. With HL1-2 stabilized by the Cys132-Cys135 disulfide bond, strong WR residues form a close pocket (electrostatic surface) for warfarin to bind. (MOV 18014 kb)
Electron transfer is associated with conformational changes at the VKOR active site.
Four structures (PDB code: 3KP9, 4NV2, 4NV5, and 4NV6) of the bacterial VKOR homolog are combined and a trajectory of conformational changes is modeled. These structures show a short helix (part of HL1-2; red) at the active site change conformations when alternative disulfide bonds are formed during electron transfer. The sequence of this helical region is highly conserved between the bacterial homolog and hVKOR. Therefore, similar conformational changes may occur in hVKOR, and warfarin may selectively bind to a conformational state stabilized by the Cys132-Cys135 disulfide. (MOV 3217 kb)
Rights and permissions
About this article
Cite this article
Shen, G., Cui, W., Zhang, H. et al. Warfarin traps human vitamin K epoxide reductase in an intermediate state during electron transfer. Nat Struct Mol Biol 24, 69–76 (2017). https://doi.org/10.1038/nsmb.3333
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nsmb.3333
This article is cited by
-
ROS regulated reversible protein phase separation synchronizes plant flowering
Nature Chemical Biology (2021)
-
Genetic variation in human drug-related genes
Genome Medicine (2017)
-
Vitamin K epoxide reductase and its paralogous enzyme have different structures and functions
Scientific Reports (2017)
-
New pieces to an old puzzle: identifying the warfarin-binding site that prevents clotting
Nature Structural & Molecular Biology (2017)