Key Points
-
A growing proportion of men with prostate cancer of a low volume, stage and grade are being managed with AS
-
No established recommendations exist for delaying, or preventing, the progression of low-risk prostate cancer and, thus, avoiding the need for active treatment
-
Preliminary evidence suggests that lifestyle and/or exercise interventions might have therapeutic potential for men with prostate cancer who are on AS
-
Exercise as medicine for men on AS has the potential to delay both disease progression and the transition to requiring active therapy
-
Trials examining exercise as medicine during AS, as well as other components of lifestyle interventions, are required to build upon previous findings
-
If proven effective, exercise could easily be implemented as a component of clinical best practice during AS, with an array of beneficial effects including enhanced quality of life
Abstract
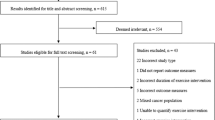
Active surveillance (AS) is a strategy for the management of patients with low-risk, localized prostate cancer, in which men undergo regular monitoring of serum PSA levels and tumour characteristics, using multiparametric MRI and repeat biopsy sampling, to identify signs of disease progression. This strategy reduces overtreatment of clinically insignificant disease while also preserving opportunities for curative therapy in patients whose disease progresses. Preliminary studies of lifestyle interventions involving basic exercise advice have indicated that exercise reduces the numbers of patients undergoing active treatment, as well as modulating the biological processes involved in tumour progression. Therefore, preliminary evidence suggests that lifestyle and/or exercise interventions might have therapeutic potential in this growing population of men with prostate cancer. However, several important issues remain unclear: the exact value of different types of lifestyle and exercise medicine interventions during AS; the biological mechanisms of exercise in delaying disease progression; and the influence of the anxieties and distress created by having a diagnosis of cancer without then receiving active treatment. Future studies are required to confirm and expand these findings and determine the relative contributions of each lifestyle component to specific end points and patient outcomes during AS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Draisma, G. et al. Lead time and overdiagnosis in prostate-specific antigen screening: importance of methods and context. J. Natl Cancer Inst. 101, 374–383 (2009).
Slomski, A. Expert panel advocates surveillance for men with low-risk prostate cancer. JAMA 307, 133 (2012).
Ischia, J. J. et al. Active surveillance for prostate cancer: an Australian experience. BJU Int. 109, S40–S43 (2012).
Tosoian, J. J. et al. Active surveillance program for prostate cancer: an update of the Johns Hopkins experience. J. Clin. Oncol. 29, 2185–2190 (2011).
Cooperberg, M. R., Carroll, P. R. & Klotz, L. Active surveillance for prostate cancer: progress and promise. J. Clin. Oncol. 29, 3669–3776 (2011).
Bul, M. et al. Active surveillance for low-risk prostate cancer worldwide: the PRIAS study. Eur. Urol. 63, 597–603 (2013).
Klotz, L. et al. Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J. Clin. Oncol. 33, 272–277 (2015).
Tosoian, J. J. et al. Intermediate and longer-term outcomes from a prospective active-surveillance program for favorable-risk prostate cancer. J. Clin. Oncol. 33, 3379–3385 (2015).
Bhindi, B. et al. Obesity is associated with risk of progression for low-risk prostate cancers managed expectantly. Eur. Urol. 66, 841–848 (2014).
Pedersen, B. K. & Febbraio, M. A. Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat. Rev. Endocrinol. 8, 457–465 (2012).
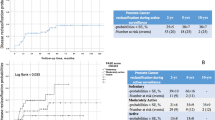
Ornish, D. et al. Intensive lifestyle changes may affect the progression of prostate cancer. J. Urol. 174, 1065–1069 (2005).
Frattaroli, J. et al. Clinical events in prostate cancer lifestyle trial: results from two years of follow-up. Urology 72, 1319–1323 (2008).
Ornish, D. et al. Changes in prostate gene expression in men undergoing an intensive nutrition and lifestyle intervention. Proc. Natl Acad. Sci. USA 105, 8369–8374 (2008).
Segal, R. J. et al. Resistance exercise in men receiving androgen deprivation therapy for prostate cancer. J. Clin. Oncol. 21, 1653–1659 (2003).
Segal, R. J. et al. Randomized controlled trial of resistance or aerobic exercise in men receiving radiation therapy for prostate cancer. J. Clin. Oncol. 27, 344–351 (2009).
Galvao, D. A., Taaffe, D. R., Spry, N., Joseph, D. & Newton, R. U. Combined resistance and aerobic exercise program reverses muscle loss in men undergoing androgen suppression therapy for prostate cancer without bone metastases: a randomized controlled trial. J. Clin. Oncol. 28, 340–347 (2010).
Buffart, L. M. et al. Mediators of the resistance and aerobic exercise intervention effect on physical and general health in men undergoing androgen deprivation therapy for prostate cancer. Cancer 120, 294–301 (2014).
Galvao, D. A. et al. A multicentre year-long randomised controlled trial of exercise training targeting physical functioning in men with prostate cancer previously treated with androgen suppression and radiation from TROG 03.04 RADAR. Eur. Urol. 65, 856–864 (2014).
Cormie, P. et al. Can supervised exercise prevent treatment toxicity in patients with prostate cancer initiating androgen-deprivation therapy: a randomised controlled trial. BJU Int. 115, 256–266 (2015).
Buffart, L. M. et al. The effect, moderators, and mediators of resistance and aerobic exercise on health-related quality of life in older long-term survivors of prostate cancer. Cancer 121, 2821–2830 (2015).
Newton, R. U. & Galvao, D. A. Exercise in prevention and management of cancer. Curr. Treat. Options Oncol. 9, 135–146 (2008).
Mann, S., Beedie, C. & Jimenez, A. Differential effects of aerobic exercise, resistance training and combined exercise modalities on cholesterol and the lipid profile: review, synthesis and recommendations. Sports Med. 44, 211–221 (2014).
Galvao, D. A. et al. Resistance training and reduction of treatment side effects in prostate cancer patients. Med. Sci. Sports Exerc. 38, 2045–2052 (2006).
Galvao, D. A., Taaffe, D. R., Spry, N., Joseph, D. & Newton, R. U. Acute versus chronic exposure to androgen suppression for prostate cancer: impact on the exercise response. J. Urol. 186, 1291–1297 (2011).
Cormie, P. et al. Exercise maintains sexual activity in men undergoing androgen suppression for prostate cancer: a randomized controlled trial. Prostate Cancer Prostatic Dis. 16, 170–175 (2013).
Bourke, L. et al. Lifestyle changes for improving disease-specific quality of life in sedentary men on long-term androgen-deprivation therapy for advanced prostate cancer: a randomised controlled trial. Eur. Urol. 65, 865–872 (2014).
O'Connor, G. T. et al. Physical exercise and reduced risk of nonfatal myocardial infarction. Am. J. Epidemiol. 142, 1147–1156 (1995).
Helmrich, S. P., Ragland, D. R., Leung, R. W. & Paffenbarger, R. S. Jr. Physical activity and reduced occurrence of non-insulin-dependent diabetes mellitus. N. Engl. J. Med. 325, 147–152 (1991).
Jakicic, J. M. & Otto, A. D. Physical activity considerations for the treatment and prevention of obesity. Am. J. Clin. Nutr. 82 (Suppl.), S226–S229 (2005).
Singh, N. A. et al. A randomized controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. J. Gerontol. A. Biol. Sci. Med. Sci. 60, 768–776 (2005).
Ettinger, W. H. Jr et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST). JAMA 277, 25–31 (1997).
Lautenschlager, N. T. et al. Effect of physical activity on cognitive function in older adults at risk for Alzheimer disease: a randomized trial. JAMA 300, 1027–1037 (2008).
Larson, E. B. et al. Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older. Ann. Intern. Med. 144, 73–81 (2006).
Paffenbarger, R. S. Jr et al. The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. N. Engl. J. Med. 328, 538–545 (1993).
Ekelund, L. G. et al. Physical fitness as a predictor of cardiovascular mortality in asymptomatic North American men. The Lipid Research Clinics Mortality Follow-up Study. N. Engl. J. Med. 319, 1379–1384 (1988).
Myers, J. et al. Exercise capacity and mortality among men referred for exercise testing. N. Engl. J. Med. 346, 793–801 (2002).
Taaffe, D. R., Daly, R. M., Suominen, H., Galvao, D. A. & Bolam, K. A. in Osteoporosis (eds Marcus, R. et al.) 683–719 (Elsevier Inc., 2013).
Ornish, D. et al. Increased telomerase activity and comprehensive lifestyle changes: a pilot study. Lancet Oncol. 9, 1048–1057 (2008).
Ornish, D. et al. Effect of comprehensive lifestyle changes on telomerase activity and telomere length in men with biopsy-proven low-risk prostate cancer: 5-year follow-up of a descriptive pilot study. Lancet Oncol. 14, 1112–1120 (2013).
Magbanua, M. J. et al. Physical activity and prostate gene expression in men with low-risk prostate cancer. Cancer Causes Control 25, 515–523 (2014).
Cao, Y. & Ma, J. Body mass index, prostate cancer-specific mortality, and biochemical recurrence: a systematic review and meta-analysis. Cancer Prev. Res. (Phila.) 4, 486–501 (2011).
Perez-Hernandez, A. I., Catalan, V., Gomez-Ambrosi, J., Rodriguez, A. & Fruhbeck, G. Mechanisms linking excess adiposity and carcinogenesis promotion. Front. Endocrinol. (Lausanne) 5, 65 (2014).
Atlantis, E. et al. Inverse associations between muscle mass, strength, and the metabolic syndrome. Metabolism 58, 1013–1022 (2009).
Moon, S. S. Low skeletal muscle mass is associated with insulin resistance, diabetes, and metabolic syndrome in the Korean population: the Korea National Health and Nutrition Examination Survey (KNHANES) 2009–2010. Endocr. J. 61, 61–70 (2014).
Buch, A. et al. Muscle function and fat content in relation to sarcopenia, obesity and frailty of old age — an overview. Exp. Gerontol. 76, 25–32 (2016).
Wang, Y. et al. Mitogenic and anti-apoptotic effects of insulin in endometrial cancer are phosphatidylinositol 3-kinase/Akt dependent. Gynecol. Oncol. 125, 734–741 (2012).
Djiogue, S. et al. Insulin resistance and cancer: the role of insulin and IGFs. Endocr. Relat. Cancer 20, R1–R17 (2013).
Nishida, Y. et al. Effect of low-intensity aerobic exercise on insulin-like growth factor-I and insulin-like growth factor-binding proteins in healthy men. Int. J. Endocrinol. 2010, 452820 (2010).
Mina, D. S. et al. Exercise effects on adipokines and the IGF axis in men with prostate cancer treated with androgen deprivation: a randomized study. Can. Urol. Assoc. J. 7, E692–E698 (2013).
van Kruijsdijk, R. C., van der Wall, E. & Visseren, F. L. Obesity and cancer: the role of dysfunctional adipose tissue. Cancer Epidemiol. Biomarkers Prev. 18, 2569–2578 (2009).
Xiang, Y. Z. et al. The association between metabolic syndrome and the risk of prostate cancer, high-grade prostate cancer, advanced prostate cancer, prostate cancer-specific mortality and biochemical recurrence. J. Exp. Clin. Cancer Res. 32, 9 (2013).
Vingren, J. L. et al. Testosterone physiology in resistance exercise and training: the up-stream regulatory elements. Sports Med. 40, 1037–1053 (2010).
Ellem, S. J. & Risbridger, G. P. The dual, opposing roles of estrogen in the prostate. Ann. NY Acad. Sci. 1155, 174–186 (2009).
Ellem, S. J. & Risbridger, G. P. Treating prostate cancer: a rationale for targeting local oestrogens. Nat. Rev. Cancer 7, 621–627 (2007).
Risbridger, G. et al. Evidence that epithelial and mesenchymal estrogen receptor-α mediates effects of estrogen on prostatic epithelium. Dev. Biol. 229, 432–442 (2001).
Takizawa, I. et al. Estrogen receptor alpha drives proliferation in PTEN-deficient prostate carcinoma by stimulating survival signaling, MYC expression and altering glucose sensitivity. Oncotarget 6, 604–616 (2015).
McPherson, S. J. et al. Estrogen receptor-β activated apoptosis in benign hyperplasia and cancer of the prostate is androgen independent and TNFα mediated. Proc. Natl Acad. Sci. USA 107, 3123–3128 (2010).
Hussain, S. et al. Estrogen receptor β activation impairs prostatic regeneration by inducing apoptosis in murine and human stem/progenitor enriched cell populations. PLoS ONE 7, e40732 (2012).
Nielsen, S. F., Nordestgaard, B. G. & Bojesen, S. E. Statin use and reduced cancer-related mortality. N. Engl. J. Med. 367, 1792–1802 (2012).
Moon, H., Hill, M. M., Roberts, M. J., Gardiner, R. A. & Brown, A. J. Statins: protectors or pretenders in prostate cancer? Trends Endocrinol. Metab. 25, 188–196 (2014).
Mostaghel, E. A., Solomon, K. R., Pelton, K., Freeman, M. R. & Montgomery, R. B. Impact of circulating cholesterol levels on growth and intratumoral androgen concentration of prostate tumors. PLoS ONE 7, e30062 (2012).
Zhuang, L., Kim, J., Adam, R. M., Solomon, K. R. & Freeman, M. R. Cholesterol targeting alters lipid raft composition and cell survival in prostate cancer cells and xenografts. J. Clin. Invest. 115, 959–968 (2005).
Nassar, Z. D., Hill, M. M., Parton, R. G. & Parat, M. O. Caveola-forming proteins caveolin-1 and PTRF in prostate cancer. Nat. Rev. Urol. 10, 529–536 (2013).
Moon, H. et al. Diet-induced hypercholesterolemia promotes androgen-independent prostate cancer metastasis via IQGAP1 and caveolin-1. Oncotarget 6, 7438–7453 (2015).
Earnest, C. P. et al. Maximal estimated cardiorespiratory fitness, cardiometabolic risk factors, and metabolic syndrome in the aerobics center longitudinal study. Mayo Clin. Proc. 88, 259–270 (2013).
Rundqvist, H. et al. Effect of acute exercise on prostate cancer cell growth. PLoS ONE 8, e67579 (2013).
Barnard, R. J., Ngo, T. H., Leung, P. S., Aronson, W. J. & Golding, L. A. A low-fat diet and/or strenuous exercise alters the IGF axis in vivo and reduces prostate tumor cell growth in vitro. Prostate 56, 201–206 (2003).
Leung, P. S., Aronson, W. J., Ngo, T. H., Golding, L. A. & Barnard, R. J. Exercise alters the IGF axis in vivo and increases p53 protein in prostate tumor cells in vitro. J. Appl. Physiol. (1985) 96, 450–454 (2004).
Fruhbeis, C., Helmig, S., Tug, S., Simon, P. & Kramer-Albers, E. M. Physical exercise induces rapid release of small extracellular vesicles into the circulation. J. Extracell. Vesicles 4, 28239 (2015).
Colombo, M., Raposo, G. & Thery, C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu. Rev. Cell Dev. Biol. 30, 255–289 (2014).
Tickner, J. A., Urquhart, A. J., Stephenson, S. A., Richard, D. J. & O'Byrne, K. J. Functions and therapeutic roles of exosomes in cancer. Front. Oncol. 4, 127 (2014).
Trock, B. J. Circulating biomarkers for discriminating indolent from aggressive disease in prostate cancer active surveillance. Curr. Opin. Urol. 24, 293–302 (2014).
Mucci, L. A. et al. Prospective study of prostate tumor angiogenesis and cancer-specific mortality in the health professionals follow-up study. J. Clin. Oncol. 27, 5627–5633 (2009).
Van Blarigan, E. L. et al. Physical activity and prostate tumor vessel morphology: data from the health professionals follow-up study. Cancer Prev. Res. (Phila.) 8, 962–967 (2015).
Hayes, J. H. et al. Active surveillance compared with initial treatment for men with low-risk prostate cancer: a decision analysis. JAMA 304, 2373–2380 (2010).
Kazer, M. W., Psutka, S. P., Latini, D. M. & Bailey, D. E. Jr. Psychosocial aspects of active surveillance. Curr. Opin. Urol. 23, 273–277 (2013).
Latini, D. M. et al. The relationship between anxiety and time to treatment for patients with prostate cancer on surveillance. J. Urol. 178, 826–831; discussion 831–832 (2007).
Bul, M. et al. Radical prostatectomy for low-risk prostate cancer following initial active surveillance: results from a prospective observational study. Eur. Urol. 62, 195–200 (2012).
Watts, S. et al. A quantitative analysis of the prevalence of clinical depression and anxiety in patients with prostate cancer undergoing active surveillance. BMJ Open 5, e006674 (2015).
Anderson, J. et al. Anxiety in the management of localised prostate cancer by active surveillance. BJU Int. 114 (Suppl. 1), 55–61 (2014).
Bellardita, L. et al. How does active surveillance for prostate cancer affect quality of life? A systematic review. Eur. Urol. 67, 637–645 (2015).
Chambers, S. K., Ferguson, M., Gardiner, R. A., Aitken, J. & Occhipinti, S. Intervening to improve psychological outcomes for men with prostate cancer. Psychooncology 22, 1025–1034 (2013).
Pickles, T. et al. Psychosocial barriers to active surveillance for the management of early prostate cancer and a strategy for increased acceptance. BJU Int. 100, 544–551 (2007).
Osterberg, L. & Blaschke, T. Adherence to medication. N. Engl. J. Med. 353, 487–497 (2005).
Resnick, M. J. et al. Prostate cancer survivorship care guideline: American Society of Clinical Oncology Clinical Practice Guideline endorsement. J. Clin. Oncol. 33, 1078–1085 (2015).
Ornish, D. et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA 280, 2001 (1998).
Acknowledgements
Daniel A. Galvão gratefully acknowledges research funding from a Movember New Directions Development Award obtained through the Prostate Cancer Foundation of Australia's Research Program and a Cancer Council Western Australia Research Fellowship. Suzanne Chambers gratefully acknowledges research funding from an Australian Research Council Professorial Future Fellowship. Michelle Hill gratefully acknowledges research funding from an Australian Research Council Future Fellowship.
Author information
Authors and Affiliations
Contributions
D.A.G., D.T., F.G., R.T., M.F., M.H., S.C., E.Z. and R.N. researched data for the manuscript. All authors made a substantial contribution to discussions of content. D.A.G., D.T., M.H., S.C., E.Z. and R.N. wrote the manuscript and all authors reviewed and/or edited the manuscript prior to submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Galvão, D., Taaffe, D., Spry, N. et al. Enhancing active surveillance of prostate cancer: the potential of exercise medicine. Nat Rev Urol 13, 258–265 (2016). https://doi.org/10.1038/nrurol.2016.46
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2016.46
This article is cited by
-
Lifelong exercise training promotes the remodelling of the immune system and prostate signalome in a rat model of prostate carcinogenesis
GeroScience (2023)
-
Exercise-induced myokines and their effect on prostate cancer
Nature Reviews Urology (2021)
-
Exercise modulation of tumour perfusion and hypoxia to improve radiotherapy response in prostate cancer
Prostate Cancer and Prostatic Diseases (2021)
-
Study protocol: a lifestyle intervention for African American and Hispanic prostate cancer survivors on active surveillance and their partners
Pilot and Feasibility Studies (2020)
-
A systematic review of the feasibility, acceptability, and efficacy of online supportive care interventions targeting men with a history of prostate cancer
Journal of Cancer Survivorship (2019)