Key Points
-
Nocturia remains underreported and undertreated, despite its prevalence and association with significant morbidity and mortality
-
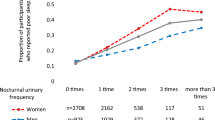
Nocturia has multiple aetiologies, including overproduction of urine (global polyuria and nocturnal polyuria), reduced bladder storage capacity, sleep disorders and a combination of these conditions
-
The frequency volume chart, Nocturia Quality of Life questionnaire and the duration of the first uninterrupted sleep period should be used in the assessment and follow-up monitoring of each patient
-
Management strategies should be targeted to each patient's specific aetiology of nocturia; some patients might require multicomponent therapies
Abstract
Nocturia is an extremely common condition that has major sequelae for affected patients. Through disruption of sleep, nocturia impairs quality of life and worsens health outcomes, and is associated with a variety of morbidities including diabetes, coronary artery disease, obstructive sleep apnoea, obesity, metabolic syndrome, and depression. Unsurprisingly, several studies have also linked nocturia with reduced survival. Nocturia is not simply a consequence of lower urinary tract disease; rather, it is a multifactorial disorder that is often a manifestation of an underlying renal or systemic disease. Through the use of the frequency volume chart, clinicians can accurately quantify nocturia and determine its aetiology. Evaluation of quality of life and sleep using simple measures is essential in order to assess the impact of nocturia on a patient. Numerous treatment options for nocturia exist, but most are associated with minor benefit or lack sufficient evidence supporting their use. By systematically analysing an individual's causes of nocturia, clinicians can design appropriate treatment strategies to most effectively treat this condition.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
van Kerrebroeck, P. et al. The standardisation of terminology in nocturia: report from the Standardisation Sub-committee of the International Continence Society. Neurourol. Urodyn. 21, 179–183 (2002).
Tikkinen, K. A. et al. Nocturia frequency, bother, and quality of life: how often is too often? A population-based study in Finland. Eur. Urol. 57, 488–496 (2010).
Kupelian, V. et al. Association of nocturia and mortality: results from the Third National Health and Nutrition Examination Survey. J. Urol. 185, 571–577 (2011).
Bosch, J. L. & Weiss, J. P. The prevalence and causes of nocturia. J. Urol. 189, S86–S92 (2013).
Chen, F. Y. et al. Perception of nocturia and medical consulting behavior among community-dwelling women. Int. Urogynecol. J. Pelvic Floor Dysfunct. 18, 431–436 (2007).
Welliver, C. et al. Analyzing why men seek treatment for lower urinary tract symptoms and factors associated with non-improvement. Urology 86, 862–867 (2015).
Fitzgerald, M. P., Litman, H. J., Link, C. L., McKinlay, J. B. & BACH Survey Investigators. The association of nocturia with cardiac disease, diabetes, body mass index, age and diuretic use: results from the BACH survey. J. Urol. 177, 1385–1389 (2007).
Agarwal, A. et al. What is the most bothersome lower urinary tract symptom? Individual- and population-level perspectives for both men and women. Eur. Urol. 65, 1211–1217 (2014).
Zhang, L. et al. A population-based survey of the prevalence, potential risk factors, and symptom-specific bother of lower urinary tract symptoms in adult Chinese women. Eur. Urol. 68, 97–112 (2015).
Miranda Ede, P. et al. Nocturia is the lower urinary tract symptom with greatest impact on quality of life of men from a community setting. Int. Neurourol. J. 18, 86–90 (2014).
Aikawa, K. et al. Elucidation of the pattern of the onset of male lower urinary tract symptoms using cluster analysis: efficacy of tamsulosin in each symptom group. Urology 86, 349–353 (2015).
Chartier-Kastler, E. & Chapple, C. R. LUTS/BPH in clinical practice: the importance of nocturia and quality of sleep. BJU Int. 98, 3–8 (2006).
Kupelian, V. et al. Nocturia and quality of life: results from the Boston area community health survey. Eur. Urol. 61, 78–84 (2012).
Bliwise, D. L. et al. Nocturia and disturbed sleep in the elderly. Sleep Med. 10, 540–548 (2009).
Obayashi, K., Saeki, K. & Kurumatani, N. Quantitative association between nocturnal voiding frequency and objective sleep quality in the general elderly population: the HEIJO-KYO cohort. Sleep Med. 16, 577–582 (2015).
Parthasarathy, S. et al. Nocturia, sleep-disordered breathing, and cardiovascular morbidity in a community-based cohort. PLoS ONE 7, e30969 (2012).
Keenan, S. A. Normal human sleep. Respir. Care Clin. N. Am. 5, 319–331 (1999).
Tasali, E., Leproult, R., Ehrmann, D. A. & Van Cauter, E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc. Natl Acad. Sci. USA 105, 1044–1049 (2008).
Herzog, N. et al. Selective slow wave sleep but not rapid eye movement sleep suppression impairs morning glucose tolerance in healthy men. Psychoneuroendocrinology 38, 2075–2082 (2013).
Cedernaes, J. et al. A single night of partial sleep loss impairs fasting insulin sensitivity but does not affect cephalic phase insulin release in young men. J. Sleep Res. http://dx.doi.org/10.1111/jsr.12340 (2015).
Chami, H. A., Gottlieb, D. J., Redline, S. & Punjabi, N. M. Association between glucose metabolism and sleep-disordered breathing during REM sleep. Am. J. Respir. Crit. Care Med. 192, 1118–1126 (2015).
Kudlow, P. A., Cha, D. S., Lam, R. W. & McIntyre, R. S. Sleep architecture variation: a mediator of metabolic disturbance in individuals with major depressive disorder. Sleep Med. 14, 943–949 (2013).
Fung, M. M. et al. Decreased slow wave sleep increases risk of developing hypertension in elderly men. Hypertension 58, 596–603 (2011).
van Kerrebroeck, P. et al. Desmopressin in the treatment of nocturia: a double-blind, placebo-controlled study. Eur. Urol. 52, 221–229 (2007).
Torimoto, K. et al. Evaluation of sleep quantity and quality in older adults with nocturia using portable electroencephalogram acquisition. J. Urol. 189, e557–e558 (2013).
Finan, P. H., Quartana, P. J. & Smith, M. T. The effects of sleep continuity disruption on positive mood and sleep architecture in healthy adults. Sleep 38, 1735–1742 (2015).
Bliwise, D. L., Dijk, D. J. & Juul, K. V. Nocturia is associated with loss of deep sleep independently from sleep apnea. Neurourol. Urodyn. 34, 392 (2015).
Bliwise, D. L., Holm-Larsen, T., Goble, S. & Norgaard, J. P. Short time to first void is associated with lower whole-night sleep quality in nocturia patients. J. Clin. Sleep Med. 11, 53–55 (2015).
Bliwise, D. L., Holm-Larsen, T. & Goble, S. Increases in duration of first uninterrupted sleep period are associated with improvements in PSQI-measured sleep quality. Sleep Med. 15, 1276–1278 (2014).
Buysse, D. J., Reynolds, C. F. 3rd, Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213 (1989).
Bliwise, D., Juul, K. V., Larsen, T., Van der Meulen, E. & Norgaard, J. P. Increase in first undisturbed sleep period (FUSP) is associated with a reduction in random blood glucose in nocturia patients. Eur. Urol. Suppl. 14, e550–e550a (2015).
Lightner, D. J. et al. Nocturia is associated with an increased risk of coronary heart disease and death. BJU Int. 110, 848–853 (2012).
Bursztyn, M., Jacob, J. & Stessman, J. Usefulness of nocturia as a mortality risk factor for coronary heart disease among persons born in 1920 or 1921. Am. J. Cardiol. 98, 1311–1315 (2006).
Fan, Y., Wei, F., Lang, Y. & Qi, W. Meta-analysis of nocturia and risk of all-cause mortality in adult population. Int. J. Cardiol. 195, 120–122 (2015).
Nakagawa, H. et al. Impact of nocturia on bone fracture and mortality in older individuals: a Japanese longitudinal cohort study. J. Urol. 184, 1413–1418 (2010).
van Doorn, B., Kok, E. T., Blanker, M. H., Westers, P. & Bosch, J. L. Mortality in older men with nocturia. A 15-year followup of the Krimpen study. J. Urol. 187, 1727–1731 (2012).
Parsons, J. K. et al. Lower urinary tract symptoms increase the risk of falls in older men. BJU Int. 104, 63–68 (2009).
Temml, C. et al. Nocturia is an age-independent risk factor for hip-fractures in men. Neurourol. Urodyn. 28, 949–952 (2009).
Cappuccio, F. P., D'Elia, L., Strazzullo, P. & Miller, M. A. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 33, 585–592 (2010).
Dew, M. A. et al. Healthy older adults' sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosom. Med. 65, 63–73 (2003).
Ensrud, K. E. et al. Sleep disturbances and risk of frailty and mortality in older men. Sleep Med. 13, 1217–1225 (2012).
Tikkinen, K. A. et al. A systematic evaluation of factors associated with nocturia — the population-based FINNO study. Am. J. Epidemiol. 170, 361–368 (2009).
Kupelian, V. et al. Association of lower urinary tract symptoms and the metabolic syndrome: results from the Boston Area Community Health Survey. J. Urol. 182, 616–624; discussion 624–625 (2009).
Liao, C. H., Chiang, H. S. & Yu, H. J. Serum testosterone levels significantly correlate with nocturia in men aged 40–79 years. Urology 78, 631–635 (2011).
Tikkinen, K. A. et al. Reproductive factors associated with nocturia and urinary urgency in women: a population-based study in Finland. Am. J. Obstet. Gynecol. 199, 153.e1–153.e12 (2008).
Bouwman, I. I. et al. Do lower urinary tract symptoms predict cardiovascular diseases in older men? A systematic review and meta-analysis. World J. Urol. 33, 1911–1920 (2015).
Bockenhauer, D. & Bichet, D. G. Pathophysiology, diagnosis and management of nephrogenic diabetes insipidus. Nat. Rev. Nephrol. 11, 576–588 (2015).
Nielsen, S., Kwon, T. H., Frokiaer, J. & Agre, P. Regulation and dysregulation of aquaporins in water balance disorders. J. Intern. Med. 261, 53–64 (2007).
Verbalis, J. G. Renal physiology of nocturia. Neurourol. Urodyn. 33, S6–S9 (2014).
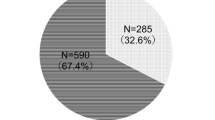
Hofmeester, I. et al. The association between nocturia and nocturnal polyuria in clinical and epidemiological studies: a systematic review and meta-analyses. J. Urol. 191, 1028–1033 (2014).
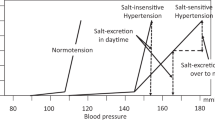
Gulur, D. M., Mevcha, A. M. & Drake, M. J. Nocturia as a manifestation of systemic disease. BJU Int. 107, 702–713 (2011).
Robertson, G. L. Differential diagnosis of polyuria. Annu. Rev. Med. 39, 425–442 (1988).
Jordan, A. S., McSharry, D. G. & Malhotra, A. Adult obstructive sleep apnoea. Lancet 383, 736–747 (2014).
Saito, Y. Roles of atrial natriuretic peptide and its therapeutic use. J. Cardiol. 56, 262–270 (2010).
Witthaus, M. W. et al. Bladder oxidative stress in sleep apnea contributes to detrusor instability and nocturia. J. Urol. 193, 1692–1699 (2015).
Obayashi, K., Saeki, K. & Kurumatani, N. Association between melatonin secretion and nocturia in elderly individuals: a cross-sectional study of the HEIJO-KYO cohort. J. Urol. 191, 1816–1821 (2014).
Kim, J. W. Effect of shift work on nocturia. Urology 87, 153–160 (2016).
Weiss, J. P. Nocturia: Causes, Consequences and Clinical Approaches (Springer, 2012).
Abrams, P. et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-Committee of the International Continence Society. Neurourol. Urodyn. 21, 167–178 (2002).
Hashim, H. & Abrams, P. Is the bladder a reliable witness for predicting detrusor overactivity? J. Urol. 175, 191–194; discussion 194–195 (2006).
Al-Zahrani, A. A. & Gajewski, J. Urodynamic findings in women with refractory overactive bladder symptoms. Int. J. Urol. 23, 75–79 (2016).
Matharu, G., Donaldson, M. M., McGrother, C. W. & Matthews, R. J. Relationship between urinary symptoms reported in a postal questionnaire and urodynamic diagnosis. Neurourol. Urodyn. 24, 100–105 (2005).
Krystal, A. D., Preud'homme, X. A., Amundsen, C. L. & Webster, G. D. Detrusor overactivity persisting at night and preceding nocturia in patients with overactive bladder syndrome: a nocturnal cystometrogram and polysomnogram study. J. Urol. 184, 623–628 (2010).
Oelke, M. et al. Age and bladder outlet obstruction are independently associated with detrusor overactivity in patients with benign prostatic hyperplasia. Eur. Urol. 54, 419–426 (2008).
Oh, M. M. et al. Is there a correlation between the presence of idiopathic detrusor overactivity and the degree of bladder outlet obstruction? Urology 77, 167–170 (2011).
Araujo, A. B. et al. Sleep related problems and urological symptoms: testing the hypothesis of bidirectionality in a longitudinal, population based study. J. Urol. 191, 100–106 (2014).
Weinberger, J. M., Weiss, J. P., Kashan, M. & Blaivas, J. G. Nocturia: why do people void at night? J. Urol. 189, e800–e801 (2013).
Cornu, J. N. et al. A contemporary assessment of nocturia: definition, epidemiology, pathophysiology, and management — a systematic review and meta-analysis. Eur. Urol. 62, 877–890 (2012).
Weiss, J. P., Blaivas, J. G., Stember, D. S. & Brooks, M. M. Nocturia in adults: etiology and classification. Neurourol. Urodyn. 17, 467–472 (1998).
Marshall, S. D. et al. Nocturia: current levels of evidence and recommendations from the International Consultation on Male Lower Urinary Tract Symptoms. Urology 85, 1291–1299 (2015).
van Haarst, E. P. & Bosch, J. L. The optimal duration of frequency-volume charts related to compliance and reliability. Neurourol. Urodyn. 33, 296–301 (2014).
Burton, C., Weiss, J. P., Parsons, M., Blaivas, J. G. & Coats, A. C. Reference values for the Nocturnal Bladder Capacity Index. Neurourol. Urodyn. 30, 52–57 (2011).
Hofmeester, I. et al. Impact of the International Continence Society (ICS) report on the standardisation of terminology in nocturia on the quality of reports on nocturia and nocturnal polyuria: a systematic review. BJU Int. 115, 520–536 (2015).
Goessaert, A. S., Krott, L., Hoebeke, P., Vande Walle, J. & Everaert, K. Diagnosing the pathophysiologic mechanisms of nocturnal polyuria. Eur. Urol. 67, 283–288 (2015).
van Doorn, B., Blanker, M. H., Kok, E. T., Westers, P. & Bosch, J. L. Prevalence, incidence, and resolution of nocturnal polyuria in a longitudinal community-based study in older men: the Krimpen study. Eur. Urol. 63, 542–547 (2013).
van Haarst, E. P. & Bosch, J. L. A cutoff value based on analysis of a reference population decreases overestimation of the prevalence of nocturnal polyuria. J. Urol. 188, 869–873 (2012).
Abraham, L. et al. Development and validation of a quality-of-life measure for men with nocturia. Urology 63, 481–486 (2004).
Weiss, J. P., Zinner, N. R., Klein, B. M. & Norgaard, J. P. Desmopressin orally disintegrating tablet effectively reduces nocturia: results of a randomized, double-blind, placebo-controlled trial. Neurourol. Urodyn. 31, 441–447 (2012).
Cho, S. Y. et al. Short-term effects of systematized behavioral modification program for nocturia: a prospective study. Neurourol. Urodyn. 31, 64–68 (2012).
Miyazaki, T. et al. Nocturia in patients with sleep-disordered breathing and cardiovascular disease. Circ. J. 79, 2632–2640 (2015).
Wang, T., Huang, W., Zong, H. & Zhang, Y. The efficacy of continuous positive airway pressure therapy on nocturia in patients with obstructive sleep apnea: a systematic review and meta-analysis. Int. Neurourol. J. 19, 178–184 (2015).
Miyazato, M. et al. Effect of continuous positive airway pressure on nocturnal urine production in patients with obstructive sleep apnea syndrome. Neurourol. Urodyn. 85, 333–336 (2015).
Reynard, J. M., Cannon, A., Yang, Q. & Abrams, P. A novel therapy for nocturnal polyuria: a double-blind randomized trial of frusemide against placebo. Br. J. Urol. 81, 215–218 (1998).
Maggi, C. A. Prostanoids as local modulators of reflex micturition. Pharmacol. Res. 25, 13–20 (1992).
Addla, S. K., Adeyoju, A. B., Neilson, D. & O'Reilly, P. Diclofenac for treatment of nocturia caused by nocturnal polyuria: a prospective, randomised, double-blind, placebo-controlled crossover study. Eur. Urol. 49, 720–725 (2006).
Caldwell, P. H., Deshpande, A. V. & Von Gontard, A. Management of nocturnal enuresis. BMJ 347, f6259 (2013).
Hammer, M. & Vilhardt, H. Peroral treatment of diabetes insipidus with a polypeptide hormone analog, desmopressin. J. Pharmacol. Exp. Ther. 234, 754–760 (1985).
Andersson, K. C. et al. Pharmacologic treatment of urinary incontinence (eds Abrams, P. C. et al.) (EAU-ICUD, 2013).
Oelke, M. et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur. Urol. 64, 118–140 (2013).
Ebell, M. H., Radke, T. & Gardner, J. A systematic review of the efficacy and safety of desmopressin for nocturia in adults. J. Urol. 192, 829–835 (2014).
Juul, K. V., Klein, B. M. & Norgaard, J. P. Long-term durability of the response to desmopressin in female and male nocturia patients. Neurourol. Urodyn. 32, 363–370 (2013).
Weiss, J. P., Herschorn, S., Albei, C. D. & van der Meulen, E. A. Efficacy and safety of low dose desmopressin orally disintegrating tablet in men with nocturia: results of a multicenter, randomized, double-blind, placebo controlled, parallel group study. J. Urol. 190, 965–972 (2013).
Sand, P. K., Dmochowski, R. R., Reddy, J. & van der Meulen, E. A. Efficacy and safety of low dose desmopressin orally disintegrating tablet in women with nocturia: results of a multicenter, randomized, double-blind, placebo controlled, parallel group study. J. Urol. 190, 958–964 (2013).
Juul, K. V., Klein, B. M., Sandstrom, R., Erichsen, L. & Norgaard, J. P. Gender difference in antidiuretic response to desmopressin. Am. J. Physiol. Renal Physiol. 300, F1116–F1122 (2011).
Yamaguchi, O., Nishizawa, O., Juul, K. V. & Norgaard, J. P. Gender difference in efficacy and dose response in Japanese patients with nocturia treated with four different doses of desmopressin orally disintegrating tablet in a randomized, placebo-controlled trial. BJU Int. 111, 474–484 (2013).
Rembratt, A., Riis, A. & Norgaard, J. P. Desmopressin treatment in nocturia; an analysis of risk factors for hyponatremia. Neurourol. Urodyn. 25, 105–109 (2006).
Johnson, T. M. et al. The effect of doxazosin, finasteride and combination therapy on nocturia in men with benign prostatic hyperplasia. J. Urol. 178, 2045–2050; discussion 2050–2051 (2007).
Eisenhardt, A., Schneider, T., Cruz, F. & Oelke, M. Consistent and significant improvement of nighttime voiding frequency (nocturia) with silodosin in men with LUTS suggestive of BPH: pooled analysis of three randomized, placebo-controlled, double-blind phase III studies. World J. Urol. 32, 1119–1125 (2014).
Johnson, T. M. et al. Changes in nocturia from medical treatment of benign prostatic hyperplasia: secondary analysis of the Department of Veterans Affairs Cooperative Study Trial. J. Urol. 170, 145–148 (2003).
Roehrborn, C. G., Van Kerrebroeck, P. & Nordling, J. Safety and efficacy of alfuzosin 10 mg once-daily in the treatment of lower urinary tract symptoms and clinical benign prostatic hyperplasia: a pooled analysis of three double-blind, placebo-controlled studies. BJU Int. 92, 257–261 (2003).
Tanaka, T. et al. Efficacy of naftopidil for nocturia in male patients with lower urinary tract symptoms: comparison of morning and evening dosing. Int. J. Urol. 22, 317–321 (2015).
Oelke, M. et al. Effects of tadalafil on nighttime voiding (nocturia) in men with lower urinary tract symptoms suggestive of benign prostatic hyperplasia: a post hoc analysis of pooled data from four randomized, placebo-controlled clinical studies. World J. Urol. 32, 1127–1132 (2014).
Oelke, M. et al. Impact of dutasteride on nocturia in men with lower urinary tract symptoms suggestive of benign prostatic hyperplasia (LUTS/BPH): a pooled analysis of three phase III studies. World J. Urol. 32, 1141–1147 (2014).
Oelke, M. et al. Nocturia improvement in the combination of Avodart(®) and tamsulosin (CombAT) study. World J. Urol. 32, 1133–1140 (2014).
Falahatkar, S., Mokhtari, G., Pourreza, F., Asgari, S. A. & Kamran, A. N. Celecoxib for treatment of nocturia caused by benign prostatic hyperplasia: a prospective, randomized, double-blind, placebo-controlled study. Urology 72, 813–816 (2008).
Simaioforidis, V. et al. Tamsulosin versus transurethral resection of the prostate: effect on nocturia as a result of benign prostatic hyperplasia. Int. J. Urol. 18, 243–248 (2011).
Choi, W. S., Ku, J. H., Oh, S. J., Kim, S. W. & Paick, J. S. Change of nocturnal polyuria after holmium laser enucleation of the prostate in patients with benign prostatic hyperplasia. Urology 84, 650–656 (2014).
Machino, R. et al. Detrusor instability with equivocal obstruction: a predictor of unfavorable symptomatic outcomes after transurethral prostatectomy. Neurourol. Urodyn. 21, 444–449 (2002).
de Nunzio, C. et al. The evolution of detrusor overactivity after watchful waiting, medical therapy and surgery in patients with bladder outlet obstruction. J. Urol. 169, 535–539 (2003).
Weiss, J. P. et al. Efficacy and safety of flexible dose fesoterodine in men and women with overactive bladder symptoms including nocturnal urinary urgency. J. Urol. 189, 1396–1401 (2013).
Buser, N., Ivic, S., Kessler, T. M., Kessels, A. G. & Bachmann, L. M. Efficacy and adverse events of antimuscarinics for treating overactive bladder: network meta-analyses. Eur. Urol. 62, 1040–1060 (2012).
Yokoyama, O., Hiro, S., Hotta, S., Mogami, S. & Yamagami, H. Efficacy of fesoterodine on nocturia and quality of sleep in Asian patients with overactive bladder. Urology 83, 750–755 (2014).
Rackley, R. et al. Nighttime dosing with tolterodine reduces overactive bladder-related nocturnal micturitions in patients with overactive bladder and nocturia. Urology 67, 731–736; discussion 736 (2006).
Kaplan, S. A. et al. Tolterodine and tamsulosin for treatment of men with lower urinary tract symptoms and overactive bladder: a randomized controlled trial. JAMA 296, 2319–2328 (2006).
Kim, T. H. et al. Comparison of the efficacy and safety of 2 mg and 4 mg tolterodine combined with an alpha-blocker in men with lower urinary tract symptoms and overactive bladder: A randomised controlled trial. BJU Int. 117, 307–315 (2016).
Yokoyama, O. et al. Add-on anticholinergic therapy for residual nocturia in patients with lower urinary tract symptoms receiving α1-blocker treatment: a multi-centre, prospective, randomised study. World J. Urol. 33, 659–667 (2015).
Johnson, T. M. 2nd, Burgio, K. L., Redden, D. T., Wright, K. C. & Goode, P. S. Effects of behavioral and drug therapy on nocturia in older incontinent women. J. Am. Geriatr. Soc. 53, 846–850 (2005).
Johnson, T. M. et al. Efficacy of adding behavioural treatment or antimuscarinic drug therapy to α-blocker therapy in men with nocturia. BJU Int. 112, 100–108 (2013).
Chapple, C. R. et al. A proof-of-concept study: mirabegron, a new therapy for overactive bladder. Neurourol. Urodyn. 32, 1116–1122 (2013).
Yamaguchi, O. et al. Safety and efficacy of mirabegron as 'add-on' therapy in patients with overactive bladder treated with solifenacin: a post-marketing, open-label study in Japan (MILAI study). BJU Int. 116, 612–622 (2015).
Kuo, H. C. et al. Results of a randomized, double-blind, parallel-group, placebo- and active-controlled, multicenter study of mirabegron, a β3-adrenoceptor agonist, in patients with overactive bladder in Asia. Neurourol. Urodyn. 34, 685–692 (2015).
Nitti, V. W. et al. Results of a randomized phase III trial of mirabegron in patients with overactive bladder. J. Urol. 189, 1388–1395 (2013).
Peters, K. M. et al. Randomized trial of percutaneous tibial nerve stimulation versus extended-release tolterodine: results from the overactive bladder innovative therapy trial. J. Urol. 182, 1055–1061 (2009).
Canbaz Kabay, S. et al. Long term sustained therapeutic effects of percutaneous posterior tibial nerve stimulation treatment of neurogenic overactive bladder in multiple sclerosis patients: 12-months results. Neurourol. Urodyn. http://dx.doi.org/10.1002/nau.22868 (2015).
Kabay, S. et al. The clinical and urodynamic results of percutaneous posterior tibial nerve stimulation on neurogenic detrusor overactivity in patients with Parkinson's disease. Urology 87, 76–81 (2016).
Sun, Y., Luo, D., Tang, C., Yang, L. & Shen, H. The safety and efficiency of onabotulinumtoxinA for the treatment of overactive bladder: a systematic review and meta-analysis. Int. Urol. Nephrol. 47, 1779–1788 (2015).
Hamidi Madani, A. et al. Transurethral intraprostatic Botulinum toxin-A injection: a novel treatment for BPH refractory to current medical therapy in poor surgical candidates. World J. Urol. 31, 235–239 (2013).
Wilt, T., Ishani, A., Mac Donald, R., Rutks, I. & Stark, G. Pygeum africanum for benign prostatic hyperplasia. Cochrane Database Syst. Rev. 1, CD001044 (2002).
Wilt, T., Mac Donald, R., Ishani, A., Rutks, I. & Stark, G. Cernilton for benign prostatic hyperplasia. Cochrane Database Syst. Rev. 2, CD001042 (2000).
MacDonald, R., Tacklind, J. W., Rutks, I. & Wilt, T. J. Serenoa repens monotherapy for benign prostatic hyperplasia (BPH): an updated Cochrane systematic review. BJU Int. 109, 1756–1761 (2012).
Chiu, A. F., Huang, M. H., Wang, C. C. & Kuo, H. C. Higher glycosylated hemoglobin levels increase the risk of overactive bladder syndrome in patients with type 2 diabetes mellitus. Int. J. Urol. 19, 995–1001 (2012).
Tyagi, S. et al. Behavioral treatment of insomnia: also effective for nocturia. J. Am. Geriatr. Soc. 62, 54–60 (2014).
Sugaya, K., Nishijima, S., Miyazato, M., Kadekawa, K. & Ogawa, Y. Effects of melatonin and rilmazafone on nocturia in the elderly. J. Int. Med. Res. 35, 685–691 (2007).
Drake, M. J., Mills, I. W. & Noble, J. G. Melatonin pharmacotherapy for nocturia in men with benign prostatic enlargement. J. Urol. 171, 1199–1202 (2004).
Vaughan, C. P., Endeshaw, Y., Nagamia, Z., Ouslander, J. G. & Johnson, T. M. A multicomponent behavioural and drug intervention for nocturia in elderly men: rationale and pilot results. BJU Int. 104, 69–74 (2009).
Kawahara, T. et al. Ramelteon combined with an α1-blocker decreases nocturia in men with benign prostatic hyperplasia. BMC Urol. 13, 30 (2013).
Doo, S. W., Kim, J. H., Yang, W. J. & Song, Y. S. Is there any objective improvement of nocturia by combination treatment of zolpidem and alpha-blocker therapy for unresponsive to alpha-blocker monotherapy in men with lower urinary tract symptoms? Low. Urin. Tract. Symptoms 5, 134–139 (2013).
Miwa, K. et al. Efficacy of combination therapy with tamsulosin and zolpidem on nocturia in patients with benign prostatic hyperplasia. Cent. European J. Urol. 64, 232–235 (2011).
Bae, W. J. et al. Desmopressin add-on therapy for refractory nocturia in men receiving α-blockers for lower urinary tract symptoms. J. Urol. 190, 180–186 (2013).
Cho, S. Y. et al. Effect of combined systematized behavioral modification education program with desmopressin in patients with nocturia: a prospective, multicenter, randomized, and parallel study. Int. Neurourol. J. 18, 213–220 (2014).
Author information
Authors and Affiliations
Contributions
J.P.W. and H.D. discussed the content for this article and wrote it, H.D. researched data for this article and all authors were involved in the review and editing of the article before submission.
Corresponding author
Ethics declarations
Competing interests
J.P.W. declares that he serves as consultant for Allergan, Astellas, Elsevier, Ferring, Pfizer, Symptelligence and Vantia. H.D. and A.E. declare no competing interests.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Dani, H., Esdaille, A. & Weiss, J. Nocturia: aetiology and treatment in adults. Nat Rev Urol 13, 573–583 (2016). https://doi.org/10.1038/nrurol.2016.134
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2016.134
This article is cited by
-
Nykturie – Epidemiologie, Pathophysiologie und Therapie
Journal für Urologie und Urogynäkologie/Österreich (2022)
-
Nocturia: its characteristics, diagnostic algorithm and treatment
International Urology and Nephrology (2022)
-
Nykturie – Epidemiologie, Pathophysiologie und Therapie
Urologie in der Praxis (2021)
-
The mediating role of sleep quality in the association between nocturia and health-related quality of life
Health and Quality of Life Outcomes (2019)
-
Frequent nocturnal urination in older men is associated with arterial stiffness: The Nagahama study
Hypertension Research (2019)