Key Points
-
An inconspicuous penis can result in considerable concern for both parents and children
-
9% of patients presenting for initial circumcision have evidence of an inconspicuous penis
-
Micropenis is defined as stretched penile length that is at least 2.5 SD below the mean for the patient's age, without any other abnormalities, such as hypospadias
-
'True micropenis', caused by deficient secretion and action of testosterone, should be distinguished from 'concealed micropenis'
-
Medical and surgical treatments for inconspicuous penis disorders aim to restore normal penis size, standing micturition and enable future sexual activity
-
Surgical correction of concealed penis is currently the gold-standard treatment
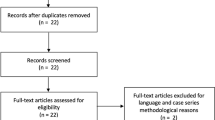
Abstract
The term 'inconspicuous penis' refers to a group of anatomical abnormalities in which the penis looks smaller than is expected. Micropenis can be defined as 'true micropenis'—which results from a defect in the hypothalamic–pituitary–gonadal axis—and 'micropenis secondary to congenital anatomical anomalies of the surrounding and overlying structures'—also known as 'concealed penis'. The different forms of concealed penis include webbed penis, congenital megaprepuce and partially hidden penis caused by prepubic adiposity. This disorder can also have iatrogenic causes resulting from adhesions that are secondary to circumcision—this type of concealed penis is known as 'trapped penis'. However, in both groups, micropenis is defined as a stretched penile length that is at least 2.5 SD below the mean for the patient's age, but without any other penile defects. Patients with true micropenis can be managed with testosterone, which has demonstrated good penile elongation results in the long term. Surgery also has a pivotal role in reconstruction for elongating the penis and for correction of anatomical abnormalities in concealed penis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Bergeson, P. S., Hopkin, R. J., Bailey, R. B., McGill, L. C. & Piattt, J. P. The inconspicuous penis. Pediatrics 92, 794–799 (1993).
Maizels, M., Zaontz, M., Donovan, J., Bushnik, P. N. & Firlit, C. F. Surgical correction of the buried penis: description of a classification system and a technique to correct the disorder. J. Urol. 136, 268–271 (1986).
Williams, C. P., Richardson, B. G. & Bukowski, T. P. Importance of identifying the inconspicuous penis: prevention of circumcision complications. Urology 56, 140–143 (2000).
Cytryn, L., Cytryn, E. & Rieger, R. E. Psychological implications of cryptorchidism. J. Am. Acad. Child. Psychiatry 6, 131–165 (1967).
Wiygul, J. & Palmer, L. S. Micropenis. Scientific World Journal 11, 1462–1469 (2011).
Johnson, P. & Maxwell, D. Fetal penile length. Ultrasound Obstet. Gynecol. 15, 308–310 (2000).
Zalel, Y., Pinhas-Hamiel, O., Lipitz, S., Mashiach, S. & Achiron, R. The development of the fetal penis—an in utero sonographic evaluation. Ultrasound Obstet. Gynecol. 17, 129–131 (2001).
Aaronson, I. A. Micropenis: medical and surgical implications. J. Urol. 152, 4–14 (1994).
Tuladhar, R., Davis, P. G. & Batch, J. Establishment of a normal range of penile length in preterm infants. J. Paediatr. Child Health 34, 471–473 (1998).
Schonfeld, W. A. & Beebe, G. W. Normal growth and variation in the male genitalia from birth to maturity. J. Urol. 48, 759–777 (1942).
Tuladhar, R., Davis, P. G. & Batch, J. Establishment of a normal range of penile length in preterm infants. J. Paediatr. Child Health 34, 471–473 (1998).
Feldman, K.W. & Smith. D. W. Fetal phallic growth and penile standards for newborn male infants. J. Pediatr. 86, 395–398 (1975).
Camurdan, A. D. et al. Current stretched penile length cross-sectional study of 1040 healthy Turkish children aged 0 to 5 years. Urology 70, 572–575 (2007).
Kulkarni, M. L. & Rajendran, N. K. Normal values for penile standards in newborns. Indian Pediatr. 39, 183–186 (1989).
Callen, N. et al. Sexual quality of life after hormonal and surgical treatment, including phalloplasty, in men with micropenis: a review. J. Sex. Med. 10, 2890–2903 (2013).
Kayes, O. et al. Therapeutic strategies for patients with micropenis or penile dysmorphic disorder. Nat. Rev. Urol. 9, 499–507 (2012).
Kousta, E., Papathanasiou, A. & Skordis, N. Sex determination and disorders of sex development according to the revised nomenclature and classification in 46, XX individuals. Hormones (Athens) 9, 218–231 (2010).
Hughes, I. A. in Pediatric Endocrinology. 3rd edn Ch. 16 (ed. Sperling, M. A.) 662–685 (Elsevier, 2008).
Achermann, J. C. & Hughes, I. A. in Williams Textbook of Endocrinology. 12th edn Ch. 23 (eds Melmed, S. et al.) 868–934 (Elsevier 2011).
Grumbach, M. M. A window of opportunity: the diagnosis of gonadotropin deficiency in the male infant. J. Clin. Endocrinol. Metab. 90, 3122–3127 (2005).
Hughes, I. A. et al. Consensus Statement on management of intersex disorders. J. Pediatr. Urol. 2, 148–162 (2006).
Quigley, C. A. Editorial: The postnatal gonadotropin and sex steroid surge—Insights from the androgen insensitivity syndrome. J. Clin. Endocrinol. Metab. 87, 24–28 (2002).
Witchel, S. F. & Lee, P. A. in Pediatric Endocrinology. 3rd edn Ch. 4 (ed. Sperling, M. A.) 127–164 (Elsevier, 2008).
Lee, P. A. et al. Micropenis. I. Criteria, etiologies and classification. Johns Hopkins Med. J. 146, 156–163 (1980).
Ahmed, S. F. et al. The role of a clinical score in the assessment of ambiguous genitalia. BJU Int. 85, 120–124 (2000).
Bertelloni, S. et al. Early diagnosis of 5alpha-reductase deficiency in newborns. Sex. Dev. 1, 147–151 (2007).
Walter, K. N. et al. Difficulties in diagnosis and treatment of 5 α-reductase type 2 deficiency in a newborn with 46, XY DSD. Horm. Res. Paediatr. 74, 67–71 (2010).
Tar, A. et al. Hypertelorism and hypospadias associated with a de novo apparently balanced translocation between 8q22.3–23 and 20p13. Am. J. Med. Genet. 68, 231–235 (1997).
Imperato-McGinley, J. et al. Androgens and the evolution of male-gender identity among male pseudohermaphrodites with 5alpha-reductase deficiency. N. Engl. J. Med. 300, 1233–1237 (1979).
Ludwig, G. Micropenis and apparent micropenis—a diagnostic and therapeutic challenge. Andrologia 31 (Suppl. 1), 27 (1999).
Elder, J. in Campbell-Walsh Urology. 9th edn Ch. 129 (ed. Cambell, M. et al.) 3751–3754 (Elsevier, 2007).
Bin-Abbas, B., Conte, F. A., Grumbach, M. M. & Kaplan, S. L. Congenital hypogonadotropic hypogonadism and micropenis: effect of testosterone treatment on adult penile size. Why sex reversal is not indicated. J. Pediatr. 134, 579–583 (1999).
Burstein, S., Grumbach, M. M. & Kaplan, S. L. Early determination of androgen-responsiveness is important in the management of microphallus. Lancet 2, 983–986 (1979).
Nerli, R. B., Guntaka, A. K., Patne, P. B. & Hiremath, M. B. Penile growth in response to hormone treatment in children with micropenis. Indian J. Urol. 29, 288–291 (2013).
Choi, S. K., Han, S. W., Kim, D. H. & de Lignieres, B. Transdermal dihydrotestosterone therapy and its effects on patients with microphallus. J. Urol. 150, 657–660 (1993).
Ben-Galim, E., Hillman, R. E. & Weldon, V. V. Topically applied testosterone and phallic growth. Its effects in male children with hypopituitarism and microphallus. Am. J. Dis. Child. 134, 296–298 (1980).
Hatipoĝlu, N. & Kurtoĝlu, S. Micropenis: etiology, diagnosis and treatment approaches. J. Clin. Res. Pediatr. Endocrinol. 5, 217–223 (2013).
Main, K. M., Schmidt, I. M., Toppari, J. & Skakkebaek, N. E. Early postnatal treatment of hypogonadotropic hypogonadism with recombinant human FSH and LH. Eur. J. Endocrinol. 146, 75–79 (2002).
Bougnères, P. et al. Effects of an early postnatal treatment of hypogonadotropic hypogonadism with a continuous subcutaneous infusion of recombinant follicle-stimulating hormone and luteinizing hormone. J. Clin. Endocrinol. Metab. 93, 2202–2205 (2008).
Cortes, D., Müller, J. & Skakkebaek, N. E. Proliferation of Sertoli cells during development of the human testis assessed by stereological methods. Int. J. Androl. 10, 589–596 (1987).
Sutherland, R. S. et al. The effect of prepubertal androgen exposure on adult penile length. J. Urol. 156, 783–787 (1996).
Kogan, S. J. & Williams, D. I. The micropenis syndrome: clinical observations and expectations for growth. J. Urol. 118, 311–313 (1977).
Jones, H. W. Jr, Park, I. J. & Rock, J. A. Technique of surgical sex reassignment for micropenis and allied conditions. Am. J. Obstet. Gynecol. 132, 870–877 (1978).
Hinman, F. Jr . Microphallus: characteristics and choice of treatment from a study of 20 cases. J. Urol. 107, 499–505 (1972).
Song, R., Gao, Y., Song, Y., Yu, Y. & Song, Y. The forearm flap. Clin. Plast. Surg. 9, 21–26 (1982).
Kabalin, N., Rosen, J. & Perkash, I. Penile advancement and lengthening in spinal cord injury patients with extracted phallus who have failed penile prosthesis placement alone. J. Urol. 144, 316–318 (1990).
Mokhless, I. A., Abdeldaeim, H. M., Rahman, A., Zahran, M. & Safwat, A. Penile advancement and lengthening for the management of post-circumcision traumatic short penis in adolescents. Urology 76, 1483–1487 (2010).
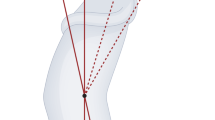
Li, C.-Y. et al. Penile suspensory ligament division for penile augmentation: indications and results. Eur. Urol. 49, 729–733 (2006).
Babaei, A., Safarinejad, M. R., Farrokhi, F. & Iran-Pour, E. Penile reconstruction: evaluation of the most accepted techniques. Urol. J. 7, 71–78 (2010).
Lumen, N., Monstrey, S., Ceulemans, P., van Laecke, E. & Hoebeke, P. Reconstructive surgery for severe penile inadequacy: phalloplasty with a free radial forearm flap or a pedicled anterolateral thigh flap. Adv. Urol. http://dx.doi.org/10.1155/2008/704343.
Monstrey, S. et al. Penile reconstruction: is the radial forearm flap really the standard technique? Plast. Reconstr. Surg. 124, 510–518 (2009).
Leriche, A. et al. Long-term outcome of forearm flee-flap phalloplasty in the treatment of transsexualism. BJU Int. 101, 1297–1300 (2008).
Fang, R. H., Kao, Y. S., Ma, S. & Lin, J. T. Phalloplasty in female-to-male transsexuals using free radial osteocutaneous flap: a series of 22 cases. Br. J. Plast. Surg. 52, 217–222 (1999).
Yang, B., Liu, X. R., Hong, Q. Q., Qiu, R. S. & Ji, C. Y. A comparative study on two kinds of surgical procedures of penile corpora cavernosa augmentation. J. Plast. Reconstr. Aesthet. Surg. 62, 357–364 (2009).
Reilly, J. M. & Woodhouse, C. R. Small penis and the male sexual role. J. Urol. 142, 569–571 (1989).
Lee, P. A. & Houk, C. P. Outcome studies among men with micropenis. J. Pediatr. Endocrinol. Metab. 17, 1043–1053 (2004).
Wisniewski, A. B. & Migeon, C. J. Long-term perspectives for 46, XY patients affected by complete androgen insensitivity syndrome or congenital micropenis. Semin. Reprod. Med. 20, 297–304 (2002).
Radhakrishnan, J., Razzaq, A. & Manickam, K. Concealed penis. Pediatr. Surg. Int. 18, 668–672 (2002).
Chu, C. C., Chen, Y. H., Diau, G. Y., Loh, I. W. & Chen, K. C. Preputial flaps to correct buried penis. Pediatr. Surg. Int. 23, 1119–1121 (2007).
Crawford, B. S. Buried penis. Br. J. Plast. Surg. 30, 96–99 (1977).
Redman, J. F. Buried penis: a congenital syndrome of a short penile shaft and a paucity of penile shaft skin. J. Urol. 173, 1714–1717 (2005).
Wollin, M., Duffy, P. G., Malone, P. S. & Ransley, P. G. Buried penis. A novel approach. Br. J. Urol. 65, 97–100 (1990).
Joseph, V. T. A new approach to the surgical correction of buried penis. J. Pediatr. Surg. 30, 727–729 (1995).
Cromie, W. J., Ritchey, M. L., Smith, R. C. & Zagaja, G. P. Anatomical alignment for the correction of buried penis. J. Urol. 160, 1482–1484 (1998).
Casale, A. J., Beck, S. D., Cain, M. P., Adams, M. C. & Rink, R. C. Concealed penis in childhood: a spectrum of etiology and treatment. J. Urol. 162, 1165–1168 (1999).
Alter, G. J. & Ehrlich, R. M. A new technique for correction of the hidden penis in children and adults. J. Urol. 161, 455–459 (1999).
Donahoe, P. K. & Keating, M. A. Preputial unfurling to correct the buried penis. J. Pediatr. Surg. 21, 1055–1057 (1986).
Boemers, T. M. L. & De Jong, T. P. V. M. The surgical correction of buried penis: a new technique. J. Urol. 154, 550–552 (1995).
Shapiro, S. R. Surgical treatment of the “buried” penis. Urology 30, 554–559 (1987).
Shenoy, M. U., Srinivasan, J., Sully, L. & Rance, C. H. Buried penis: surgical correction using liposuction and realignment of skin. BJU Int. 86, 527–530 (2000).
Liu, X., He, D. W., Hua, Y., Zhang, D. Y. & Wei, G. H. Congenital completely buried penis in boys: anatomical basis and surgical technique. BJU Int. 112, 271–275 (2013).
Perger, L., Hanley, R. S. & Feins, N. R. Penoplasty for buried penis in infants and children: report of 100 cases. Pediatr. Surg. Int. 25, 175–180 (2009).
O'Brien, A., Shapiro, A. M. & Frank, J. D. Phimosis or congenital megaprepuce. BJU Int. 73, 719–720 (1994).
Alter, G. J., Horton, C. E. & Horton, C. E. Jr . Buried penis as a contraindication for circumcision. J. Am. Coll. Surg. 178, 487–490 (1994).
Rod, J., Desmonts, A., Petit, T. & Ravasse, P. Congenital megaprepuce: a 12-year experience (52 cases) of this specific form of buried penis. J. Pediatr. Urol. 9, 784–788 (2013).
Brisson, P., Patel, H., Chan, M. & Feins, N. Penoplasty for buried penis in children: report of 50 cases. J. Pediatr. Surg. 36, 421–425 (2001).
Philip, I. & Nicholas, J. L. Congenital giant preputial sac: case reports. J. Pediatr. Surg. 34, 507–508 (1999).
Shenoy, M. U. & Rance, C. H. Surgical correction of congenital megaprepuce. Pediatr. Surg. Int. 15, 593–594 (1999).
Bisotti, P. Su un caso di “virga palmata”. Rass. Int. Clin. Terap. 33, 452–453 (1953).
Glanz, S. Adult congenital penile deformity. Plast. Reconstr. Surg. 41, 579–580 (1968).
Srinivasan, A. K., Plamer, L. S. & Plamer, J. S. Inconspicuous penis. ScientificWorldJournal 11, 2559–2564 (2011).
Perlmutter, A. D. & Chamberlain, J. W. Webbed penis without chordee. J. Urol. 107, 320–321 (1972).
Masih, B. K. & Brosman, S. A. Webbed penis. J. Urol. 111, 690–692 (1974).
Shepard, G. H., Wilson, C. S. & Sallade, R. L. Webbed penis. Plast. Reconstr. Surg. 66, 453–454 (1980).
Redman, J. F. Technique for the correction of penoscrotal fusion. J. Urol. 133, 432–433 (1985).
Wilson, C. S. & Sallade. R. L. Webbed penis. Plast. Reconstr. Surg. 66, 453–454 (1980).
Puri, P. Webbed penis without chordee. J. Pediatr. Surg. 11, 125. (1976).
Dilley, A. V. & Currie, B. G. Webbed penis. Pediatr. Surg. Int. 15, 447–448 (1999).
Montasser, E. & El Gohary, M. A. Webbed penis: a new classification. J. Indian Assoc. Pediatr. Surg. 15, 50–52 (2010).
Williams, C. P., Richardson, B. G. & Bukowski, T. P. Importance of identifying the inconspicuous penis: prevention of circumcision complications. Urology 56, 140–142, (2000).
Blalock, H. J., Vemulakonda, V., Ritchey, M. L. & Ribbeck, M. Outpatient management of phimosis following newborn circumcision. J. Urol. 169, 2332–2334 (2003).
Erogĝlu, E., Bastian, O. W., Ozkan, H. C., Yorukalp, O. E. & Goksel, A. K. Buried penis after newborn circumcision. J. Urol. 181, 1841–1843 (2009).
Bekerecioglu, M., Inaloz, H. S., Tercan, M. & Isik, D. Keloid formation on an inconspicuous penis. J. Dermatol. 32, 835–838 (2005).
Lipszyc, E., Pfister, C., Liard, A. & Mitrofanoff, P. Surgical treatment of buried penis. Eur. J. Pediatr. Surg. 7, 292–295 (1997).
Palmer, J. S., Elder, J. S. & Palmer, L. S. The use of betamethasone to manage the trapped penis following neonatal circumcision. J. Urol. 174, 1577–1578 (2005).
Radhakrishnan, J. & Reyes, H. M. Penoplasty for buried penis secondary to “radical” circumcision. J. Pediatr. Surg. 19, 629–631 (1984).
Levitt, S. B., Smith, R. B. & Ship, A. G. Iatrogenic microphallus secondary to circumcision. Urology 8, 472–474 (1976).
Gillet, M. D. et al. Split-thickness skin graft for the management of concealed penis. J. Urol. 173, 579–582 (2005).
Borsellino, A., Spagnoli, A., Vallasciani, S., Martini, L. & Ferro, F. Surgical approach to concealed penis: technical refinements and outcome. Urology 69, 1195–1198 (2007).
Author information
Authors and Affiliations
Contributions
P.C. and R.O. researched data for the article. M.C.and M.G. made a substantial contribution todiscussion of content. All authors contributed to writing the article. M.C. reviewed and edited thearticle before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Cimador, M., Catalano, P., Ortolano, R. et al. The inconspicuous penis in children. Nat Rev Urol 12, 205–215 (2015). https://doi.org/10.1038/nrurol.2015.49
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2015.49
This article is cited by
-
Towards clinical application of tissue engineering for erectile penile regeneration
Nature Reviews Urology (2019)
-
Surgical and Non-surgical Penile Elongation Techniques
Current Sexual Health Reports (2019)
-
Longer length improvement and more covert incision: a single-center, prospective study of two innovative surgical methods “one stitch” and “four stitch” for pediatric buried penis
World Journal of Urology (2018)