Key Points
-
Struvite stones form a subset of kidney stones that are exclusively associated with urease-producing bacteria
-
Stone culture at the time of treatment or urine culture from the renal pelvis provides useful clinical information for directing antibiotic therapy
-
Percutaneous nephrolithotomy (PCNL) is the gold-standard approach for treatment of staghorn infection calculi but other interventions might have an adjunctive role in therapy
-
Residual stone fragments can be removed using urease inhibitors, acidification therapy, dissolution therapy, extracorporeal shockwave lithotripsy, ureteroscopy, PCNL, or anatrophic nephrolithotomy
-
Repeat imaging and urine cultures should be performed within 3 months of the procedure to confirm a stone-free status or identify recurrence
Abstract
Infection stones—which account for 10–15% of all urinary calculi—are thought to form in the presence of urease-producing bacteria. These calculi can cause significant morbidity and mortality if left untreated or treated inadequately; optimal treatment involves complete stone eradication in conjunction with antibiotic therapy. The three key principles of treating struvite stones are: removal of all stone fragments, the use of antibiotics to treat the infection, and prevention of recurrence. Several methods to remove stone fragments have been described in the literature, including the use of urease inhibitors, acidification therapy, dissolution therapy, extracorporeal shockwave lithotripsy, ureteroscopy, percutaneous nephrolithotomy (PCNL), and anatrophic nephrolithotomy. PCNL is considered to be the gold-standard approach to treating struvite calculi, but adjuncts might be used when deemed necessary. When selecting antibiotics to treat infection, it is necessary to acquire a stone culture or, at the very least, urine culture from the renal pelvis at time of surgery, as midstream urine cultures do not always reflect the causative organism.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Change history
27 May 2014
In the version of this article initially published online Wai Ho Choy's name was spelled incorrectly. The error has been corrected for the print, HTML and PDF versions of the article.
References
Hesse, A. & Bach, D. Harnsteine, Pathobiochemie and Klinisch-chemische Diagnostik (eds Breuer, H., Buttner, H. & Stamm, D.) (Thieme Verlag, 1982).
Resnick, M. I. Evaluation and management of infection stones. Urol. Clin. North Am. 8, 265–276 (1981).
Lee, M. C. & Bariol, S. V. Changes in upper urinary tract stone composition in Australia over the past 30 years. BJU Int. 112 (Suppl. 2), 65–68 (2013).
Shafi, H. et al. Bacteriological study and structural composition of staghorn stones removed by the anatrophic nephrolithotomic procedure. Saudi J. Kidney Dis. Transpl. 24, 418–423 (2013).
Koga, S., Arakaki, Y., Matsuoka, M. & Ohyama, C. Staghorn calculi–long-term results of management. Br. J. Urol. 68, 122–124 (1991).
Schwartz, B. F. & Stoller, M. L. Nonsurgical management of infection-related renal calculi. Urol. Clin. North Am. 26, 765–778 (1999).
Evans, K. & Costabile, R. A. Time to development of symptomatic urinary calculi in a high risk environment. J. Urol. 173, 858–861 (2005).
Bichler, K. H. et al. Urinary infection stones. Int. J. Antimicrob. Agents 19, 488–498 (2002).
Bhadra, B., Roy, P. & Chakraborty, R. Serratia ureilytica sp. nov., a novel urea-utilizing species. Int. J. Syst. Evol. Microbiol. 55, 2155–2158 (2005).
Mariappan, P., Smith, G., Moussa, S. A. & Tolley, D. A. One week of ciprofloxacin before percutaneous nephrolithotomy significantly reduces upper tract infection and urosepsis: a prospective controlled study. BJU Int. 98, 1075–1079 (2006).
Gault, M. H. et al. Bacteriology of urinary tract stones. J. Urol. 153, 1164–1170 (1995).
Akagashi, K. et al. Characteristics of patients with staghorn calculi in our experience. Int. J. Urol. 11, 276–281 (2004).
Tavichakorntrakool, R. et al. Extensive characterizations of bacteria isolated from catheterized urine and stone matrices in patients with nephrolithiasis. Nephrol. Dial. Transplant. 27, 4125–4130 (2012).
Englert, K. M., McAteer, J. A., Lingeman, J. E. & Williams, J. C. Jr. High carbonate level of apatite in kidney stones implies infection, but is it predictive? Urolithiasis 41, 389–394 (2013).
Bazin, D., Daudon, M., Combes, C. & Rey, C. Characterization and some physicochemical aspects of pathological microcalcifications. Chem. Rev. 112, 5092–5120 (2012).
Bazin, D. et al. Absence of bacterial imprints on struvite-containing kidney stones: a structural investigation at the mesoscopic and atomic scale. Urology 79, 786–790 (2012).
Margel, D. et al. Clinical implication of routine stone culture in percutaneous nephrolithotomy—a prospective study. Urology 67, 26–29 (2006).
Balk, N., Strohmaier, W., Schmid, M. & Bichler, K. in 2nd European Symposium on Stone Disease (Urological Research, 1990).
Rahman, N. U., Meng, M. V. & Stoller, M. L. Infections and urinary stone disease. Curr. Pharm. Des. 9, 975–981 (2003).
Griffith, D. & Klein, A. in Stones: Clinical management of urolithiasis (eds Roth, R. & Finlayson, B.) 210–227 (Williams & Wilkins, 1983).
Rose, G. in Urinary Stones: Clinical and Laboratory Aspects 257–266 (University Park Press, 1982).
Nickel, J. C., Emtage, J. & Costerton, J. W. Ultrastructural microbial ecology of infection-induced urinary stones. J. Urol. 133, 622–627 (1985).
Nickel, J. C., Olson, M., McLean, R. J., Grant, S. K. & Costerton, J. W. An ecological study of infected urinary stone genesis in an animal model. Br. J. Urol. 59, 21–30 (1987).
Nickel, J. C., Costerton, J. W., McLean, R. J. & Olson, M. Bacterial biofilms: influence on the pathogenesis, diagnosis and treatment of urinary tract infections. J. Antimicrob. Chemother. 33 (Suppl. A), 31–41 (1994).
Kajander, E. O. & Ciftcioglu, N. Nanobacteria: an alternative mechanism for pathogenic intra- and extracellular calcification and stone formation. Proc. Natl Acad. Sci. USA 95, 8274–8279 (1998).
Raoult, D. et al. Nanobacteria are mineralo fetuin complexes. PLoS Pathog. 4, e41 (2008).
Blandy, J. P. & Singh, M. The case for a more aggressive approach to staghorn stones. J. Urol. 115, 505–506 (1976).
Teichman, J. M., Long, R. D. & Hulbert, J. C. Long-term renal fate and prognosis after staghorn calculus management. J. Urol. 153, 1403–1407 (1995).
Wong, H., Riedl, C. & Griffith, D. in Kidney Stones: Medical and Surgical Management (eds Co, F., Favus, M., Pak, C., Parks, J. & Preminger, G.) 941–950 (Raven Press, 1996).
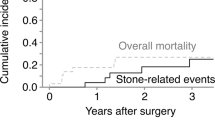
Iqbal, M. W. et al. Contemporary management of struvite stones using combined endourologic and medical treatment: predictors of unfavorable clinical outcome. J. Endourol. http://dx.doi.org/10.1089/end.2013-0257.ECC13.
Marchini, G. S. et al. Absolute Hounsfield unit measurement on noncontrast computed tomography cannot accurately predict struvite stone composition. J. Endourol. 27, 162–167 (2013).
Mostafavi, M. R., Ernst, R. D. & Saltzman, B. Accurate determination of chemical composition of urinary calculi by spiral computerized tomography. J. Urol. 159, 673–675 (1998).
Wisenbaugh, E. S., Paden, R. G., Silva, A. C. & Humphreys, M. R. Dual-energy vs conventional computed tomography in determining stone composition. Urology http://dx.doi.org/10.1016/j.urology.2013.12.023.
Streem, S. B., Yost, A. & Dolmatch, B. Combination “sandwich” therapy for extensive renal calculi in 100 consecutive patients: immediate, long-term and stratified results from a 10-year experience. J. Urol. 158, 342–345 (1997).
Tiselius, H. et al. Guidelines on urolithiasis. EUA Guidelines [online], (2013).
Zanetti, G. et al. Infections and urolithiasis: current clinical evidence in prophylaxis and antibiotic therapy. Arch. Ital. Urol. Androl. 80, 5–12 (2008).
Charton, M., Vallancien, G., Veillon, B. & Brisset, J. M. Urinary tract infection in percutaneous surgery for renal calculi. J. Urol. 135, 15–17 (1986).
Cadeddu, J. A. et al. Clinical significance of fever after percutaneous nephrolithotomy. Urology 52, 48–50 (1998).
Dogan, H. S. et al. Antibiotic prophylaxis in percutaneous nephrolithotomy: prospective study in 81 patients. J. Endourol. 16, 649–653 (2002).
Gonen, M., Turan, H., Ozturk, B. & Ozkardes, H. Factors affecting fever following percutaneous nephrolithotomy: a prospective clinical study. J. Endourol. 22, 2135–2138 (2008).
Chen, L. et al. Systemic inflammatory response syndrome after percutaneous nephrolithotomy: an assessment of risk factors. Int. J. Urol. 15, 1025–1028 (2008).
Cheung, M. C., Lee, F., Yip, S. K. & Tam, P. C. Outpatient holmium laser lithotripsy using semirigid ureteroscope. Is the treatment outcome affected by stone load? Eur. Urol. 39, 702–708 (2001).
Fernandez, A., Foell, K., Nott, L., Denstedt, J. D. & Razvi, H. Percutaneous nephrolithotripsy in patients with urinary diversions: a case-control comparison of perioperative outcomes. J. Endourol. 25, 1615–1618 (2011).
Gutierrez, J. et al. Urinary tract infections and post-operative fever in percutaneous nephrolithotomy. World J. Urol. 31, 1135–1140 (2013).
Sharifi Aghdas, F., Akhavizadegan, H., Aryanpoor, A., Inanloo, H. & Karbakhsh, M. Fever after percutaneous nephrolithotomy: contributing factors. Surg. Infect. (Larchmt) 7, 367–371 (2006).
Draga, R. O., Kok, E. T., Sorel, M. R., Bosch, R. J. & Lock, T. M. Percutaneous nephrolithotomy: factors associated with fever after the first postoperative day and systemic inflammatory response syndrome. J. Endourol. 23, 921–927 (2009).
Knopf, H. J., Graff, H. J. & Schulze, H. Perioperative antibiotic prophylaxis in ureteroscopic stone removal. Eur. Urol. 44, 115–118 (2003).
Tenke, P., Kovacs, B., Benko, R., Ashaber, D. & Nagy, E. Continuous versus intermittent levofloxacin treatment in complicated urinary tract infections caused by urinary obstruction temporarily relieved by foreign body insertion. Int. J. Antimicrob. Agents 28 (Suppl. 1), 82–85 (2006).
Costantino, G. et al. The antibacterial chemoprophylaxis in ureteroscopy: the employment of the levofloxacin used as switch-therapy versus oral treatment with a single 500 mg once a day. Gazz. Med. Ital. Arch. Sci. Med. 164, 43–46 (2005).
Dincel, C., Ozdiler, E., Ozenci, H., Tazici, N. & Kosar, A. Incidence of urinary tract infections in patients without bacteriuria undergoing SWL: comparison of stone types. J. Endourol. 12, 1–3 (1998).
Pettersson, B. & Tiselius, H. G. Are prophylactic antibiotics necessary during extracorporeal shockwave lithotripsy?. Br. J. Urol. 63, 449–452 (1989).
Bierkens, A. et al. The value of antibiotic prophylaxis during extracorporeal shockwave lithotripsy in the prevention of urinary tract infections in patients with urine proven sterile prior to treatment. Eur. Urol. 31, 30–35 (1997).
Turk, C. et al. Guidelines on urolithiasis. EUA Guidelines [online], (2013).
Preminger, G. M. et al. Chapter 1: AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J. Urol. 173, 1991–2000 (2005).
Paterson, R., Fernandez, A., Razvi, H. & Sutton, R. Evaluation and medical management of the kidney stone patient. CUA Guidelines. http://www.cua.org/userfiles/files/guidelines/ksm_2011_en.pdf (2013).
Healy, K. A. & Ogan, K. Pathophysiology and management of infectious staghorn calculi. Urol. Clin. North Am. 34, 363–374 (2007).
Orsola, A. et al. Staghorn calculi in children: treatment with monotherapy extracorporeal shock wave lithotripsy. J. Urol. 162, 1229–1233 (1999).
Meretyk, S. et al. Complete staghorn calculi: random prospective comparison between extracorporeal shock wave lithotripsy monotherapy and combined with percutaneous nephrostolithotomy. J. Urol. 157, 780–786 (1997).
Delaney, C. P., Creagh, T. A., Smith, J. M. & Fitzpatrick, J. M. Do not treat staghorn calculi by extracorporeal shockwave lithotripsy alone! Eur. Urol. 24, 355–357 (1993).
Gleeson, M. J. & Griffith, D. P. Extracorporeal shockwave lithotripsy monotherapy for large renal calculi. Br. J. Urol. 64, 329–332 (1989).
Lam, H. S. et al. Staghorn calculi: analysis of treatment results between initial percutaneous nephrostolithotomy and extracorporeal shock wave lithotripsy monotherapy with reference to surface area. J. Urol. 147, 1219–1225 (1992).
Esen, A. A., Kirkali, Z. & Guler, C. Open stone surgery: is it still a preferable procedure in the management of staghorn calculi? Int. Urol. Nephrol. 26, 247–253 (1994).
Koko, A. K., Onuora, V. C., Al Turki, M. A., Mesbed, A. H. & Al Jawini, N. A. Extracorporeal shockwave lithotripsy monotherapy is not adequate for management of staghorn renal calculi. Saudi J. Kidney Dis. Transpl. 14, 487–491 (2003).
El-Assmy, A. et al. Extracorporeal shock-wave lithotripsy monotherapy of partial staghorn calculi. Prognostic factors and long-term results. Scand. J. Urol. Nephrol. 40, 320–325 (2006).
Marguet, C. G. et al. Simultaneous combined use of flexible ureteroscopy and percutaneous nephrolithotomy to reduce the number of access tracts in the management of complex renal calculi. BJU Int. 96, 1097–1100 (2005).
Landman, J. et al. Combined percutaneous and retrograde approach to staghorn calculi with application of the ureteral access sheath to facilitate percutaneous nephrolithotomy. J. Urol. 169, 64–67 (2003).
Hamamoto, S. et al. Endoscopic combined intrarenal surgery for large calculi: simultaneous use of flexible ureteroscopy and mini-percutaneous nephrolithotomy overcomes the disadvantageous of percutaneous nephrolithotomy monotherapy. J. Endourol. 28, 28–33 (2014).
Assimos, D. G. Anatrophic nephrolithotomy. Urology 57, 161–165 (2001).
Assimos, D. G. et al. A comparison of anatrophic nephrolithotomy and percutaneous nephrolithotomy with and without extracorporeal shock wave lithotripsy for management of patients with staghorn calculi. J. Urol. 145, 710–714 (1991).
Paik, M. L., Wainstein, M. A., Spirnak, J. P., Hampel, N. & Resnick, M. I. Current indications for open stone surgery in the treatment of renal and ureteral calculi. J. Urol. 159, 374–378 (1998).
Al-Kohlany, K. M. et al. Treatment of complete staghorn stones: a prospective randomized comparison of open surgery versus percutaneous nephrolithotomy. J. Urol. 173, 469–473 (2005).
Wong, C. & Leveillee, R. J. Single upper-pole percutaneous access for treatment of > or = 5-cm complex branched staghorn calculi: is shockwave lithotripsy necessary? J. Endourol. 16, 477–481 (2002).
Aron, M. et al. Multi-tract percutaneous nephrolithotomy for large complete staghorn calculi. Urol. Int. 75, 327–332 (2005).
Wang, Y. et al. Standard-tract combined with mini-tract in percutaneous nephrolithotomy for renal staghorn calculi. Urol. Int. http://dx.doi.org/10.1159/000354427 (2014).
Griffith, D. P. et al. Randomized, double-blind trial of Lithostat (acetohydroxamic acid) in the palliative treatment of infection-induced urinary calculi. Eur. Urol. 20, 243–247 (1991).
Griffith, D. P., Khonsari, F., Skurnick, J. H. & James, K. E. A randomized trial of acetohydroxamic acid for the treatment and prevention of infection-induced urinary stones in spinal cord injury patients. J. Urol. 140, 318–324 (1988).
Williams, J. J., Rodman, J. S. & Peterson, C. M. A randomized double-blind study of acetohydroxamic acid in struvite nephrolithiasis. N. Engl. J. Med. 311, 760–764 (1984).
Chauhan, C. K. & Mihir, J. J. In vitro crystallization, characterization and growth-inhibition study of urinary type struvite crystals. J. Cryst. Growth 362, 330–337 (2013).
Prywer, J. & Torzewska, A. Effect of curcumin against proteus mirabilis during crystallization of struvite from artificial urine. Evid. Based Complement. Alternat. Med. 2012, 862794 (2012).
Daglia, M. Polyphenols as antimicrobial agents. Curr. Opin. Biotechnol. 23, 174–181 (2012).
Torzewska, A. & Rozalski, A. Inhibition of crystallization caused by Proteus mirabilis during the development of infectious urolithiasis by various phenolic substances. Microbiol. Res. http://dx.doi.org/10.1016/j.micres.2013.09.020.
Hellstrom, J. The significance of staphylococci in the development and treatment of renal and ureteral stones. Br. J. Urol. 10, 348–372 (1938).
Shortliffe, L. M. & Spigelman, S. S. Infection stones. Evaluation and management. Urol. Clin. North Am. 13, 717–726 (1986).
Dretler, S. P. & Pfister, R. C. Primary dissolution therapy of struvite calculi. J. Urol. 131, 861–863 (1984).
Fam, B., Rossier, A. B., Yalla, S. & Berg, S. The role of hemiacidrin in the management of renal stones in spinal cord injury patients. J. Urol. 116, 696–698 (1976).
Tiselius, H. G., Hellgren, E., Andersson, A., Borrud-Ohlsson, A. & Eriksson, I. Minimally invasive treatment of infection staghorn stones with shock wave lithotripsy and chemolysis. Scand. J. Urol. Nephrol. 33, 286–290 (1999).
Author information
Authors and Affiliations
Contributions
R.F. and D.L. researched, wrote, edited, reviewed, and discussed the Review with colleagues. W.H.C. helped to research and edit the article. B.C. contributed towards writing and editing.
Corresponding author
Ethics declarations
Competing interests
B.C. declares consulting associations with Boston Scientific, Cook Medical, Olympus ACMI, PercSys and Bard Medical. D.L. declares consulting associations with Boston Scientific, Olympus, Cook Medical, PercSys, and Bard Medical. R.F. and W.H.C. declare no competing interests.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Flannigan, R., Choy, W., Chew, B. et al. Renal struvite stones—pathogenesis, microbiology, and management strategies. Nat Rev Urol 11, 333–341 (2014). https://doi.org/10.1038/nrurol.2014.99
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2014.99
This article is cited by
-
Antibacterial properties and urease suppression ability of Lactobacillus inhibit the development of infectious urinary stones caused by Proteus mirabilis
Scientific Reports (2024)
-
Association between urinary lithiasis, other than struvite by crystallography and non-ureolytic bacteria
Urolithiasis (2024)
-
A retrospective study using machine learning to develop predictive model to identify urinary infection stones in vivo
Urolithiasis (2023)
-
Mineralogy, geochemistry, and micromorphology of human kidney stones (urolithiasis) from Mersin, the southern Turkey
Environmental Geochemistry and Health (2023)
-
The renal pelvis urobiome in the unilateral kidney stone patients revealed by 2bRAD-M
Journal of Translational Medicine (2022)