Key Points
-
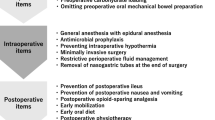
Enhanced recovery programmes (ERPs) are multimodal and have preoperative, intraoperative and postoperative components
-
The surgery itself is only one of many important steps; others include preoperative patient education, postoperative multimodal analgesia and early commencement of enteral nutrition
-
Reappraisal of existing ERPs, assessment of patient experience and identification of areas of improvement are key to ensuring a consistently high level of care
-
Discharge criteria are the tolerance of a normal diet, adequate pain control with oral analgesia, competence with either stoma care (conduit) or catheter care (neobladder) and the patient feeling adequately supported
-
Follow-up support includes follow-up telephone calls, a scheduled date for clinical review and an emergency contact
Abstract
Radical cystectomy is associated with high rates of surgical morbidity. The magnitude of the surgical insult is associated with the degree of stress response, particularly in ageing patients with multiple comorbidities. Attempts to limit this response and identify areas of improvement with respect to patient selection and optimization, anaesthesia, surgical technique and postoperative care underpin the multimodal approach to enhanced recovery pathways. No single intervention significantly reduces morbidity, but the combination of many interventions at all levels of the pathway is likely to accelerate the patient journey from diagnosis to return to normal function.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Kehlet, H. Multimodal approach to control postoperative pathophysiology and rehabilitiation. Br. J. Anaesth. 78, 606–617 (1997).
NHS Institute for Innovation and Improvement. Enhanced Recovery Programme [online], (2008).
Cerantola, Y. et al. Guidelines for perioperative care after radical cystectomy for bladder cancer: Enhanced Recovery After Surgery (ERAS®) society recommendations. Clin. Nutr. 32, 879–887 (2013).
Ronco, M., Iona, L., Fabbro, C., Bulfone, G. & Palese, A. Patient education outcomes in surgery: a systematic review from 2004 to 2010. Int. J. Evid. Based Healthc. 10, 309–323 (2012).
Broadbent, E. et al. A brief relaxation intervention reduces stress and improves surgical wound healing response: a randomised trial. Brain Behav. Immun. 26, 212–217 (2012).
Kiecolt-Glaser, J. K., Page, G. G., Marucha, P. T., MacCallum, R. C. & Glaser, R. Psychological influences on surgical recovery. Perspectives from psychoneuroimmunology. Am. Psychol. 53, 1209–1218 (1998).
Kahokehr, A., Broadbent, E., Wheeler, B. R., Sammour, T. & Hill, A. G. The effect of perioperative psychological intervention on fatigue after laparoscopic cholecystectomy: a randomized controlled trial. Surg. Endosc. 26, 1730–1736 (2012).
Tonnesen, H., Nielsen, P. R., Lauritzen, J. B. & Moller, A. M. Smoking and alcohol intervention before surgery: evidence for best practice. Br. J. Anaesth. 102, 297–306 (2009).
Tonnesen, H. et al. Effect of preoperative abstinence on poor postoperative outcome in alcohol misusers: randomised controlled trial. BMJ 318, 1311–1316 (1999).
Mastracci, T. M. et al. Effect of preoperative smoking cessation interventions on postoperative complications. J. Am. Coll. Surg. 212, 1094–1096 (2011).
Tonnesen, H., Kaiser, A. H., Nielsen, B. B. & Pedersen, A. E. Reversibility of alcohol-induced immune depression. Br. J. Addict. 87, 1025–1028 (1992).
Chaudhri, S., Brown, L., Hassan, I. & Horgan, A. F. Preoperative intensive, community-based vs. traditional stoma education: a randomized, controlled trial. Dis. Colon Rectum 48, 504–509 (2005).
Colwell, J. C. & Gray, M. Does preoperative teaching and stoma site marking affect surgical outcomes in patients undergoing ostomy surgery? J. Wound Ostomy Continence Nurs. 34, 492–496 (2007).
Kristensen, S. A., Laustsen, S., Kiesbye, B. & Jensen, B. T. The Urostomy Education Scale: a reliable and valid tool to evaluate urostomy self-care skills among cystectomy patients. J. Wound Ostomy Continence Nurs. 40, 611–617 (2013).
Garth, A. K., Newsome, C. M., Simmance, N. & Crowe, T. C. Nutritional status, nutrition practices and post-operative complications in patients with gastrointestinal cancer. J. Hum. Nutr. Diet. 23, 393–401 (2010).
Cerantola, Y. et al. Are patients at nutritional risk more prone to complications after major urological surgery. J. Urol. 190, 2126–2132 (2013).
Karl, A. et al. Prospective assessment of malnutrition in urological patients. Urology 73, 1072–1076 (2009).
Gregg, J. R. et al. Effect of preoperative nutritional deficiency on mortality after radical cystectomy for bladder cancer. J. Urol. 185, 90–96 (2011).
McClave, S. A. et al. Summary points and consensus recommendations from the North American Surgical Nutrition Summit. JPEN J. Parenter. Enteral Nutr. 37, 99S–105S (2013).
Drover, J. W. et al. Perioperative use of arginine-supplemented diets: a systematic review of the evidence. J. Am. Coll. Surg. 212, 385–399 (2012).
Holte, K., Nielsen, K. G., Madsen, J. L. & Kehlet, H. Physiologic effects of bowel preparation. Dis. Colon Rectum 47, 1397–1402 (2004).
Jung, B. et al. Preoperative mechanical preparation of the colon: the patient's experience. BMC Surg. 7, 5 (2007).
Guenaga, K. F., Matos, D., Castro, A. A., Atallah, A. N. & Wille-Jorgensen, P. Mechanical bowel preparation for elective colorectal surgery. Cochrane Database of Systematic Reviews, Issue 2. Art. No.: CD001544. http://dx.doi.org/10.1002/14651858.CD001544.
Xu, R., Zhao, X., Zhong, Z. & Zhang, L. No advantage is gained by preoperative bowel preparation in radical cystectomy and ileal conduit: a randomized controlled trial of 86 patients. Int. Urol. Nephrol. 42, 947–950 (2010).
Shafii, M., Murphy, D. M., Donovan, M. G. & Hickey, D. P. Is mechanical bowel preparation necessary in patients undergoing cystectomy and urinary diversion? BJU Int. 89, 879–881 (2002).
Brady, M., Kinn, S. & Stuart, P. Preoperative fasting for adults to prevent perioperative complications. Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD004423. http://dx.doi.org/10.1002/14651858.CD004423.
Søreide, E. & Ljungqvist, O. Modern preoperative fasting guidelines: a summary of the present recommendations and remaining questions. Best Pract. Res. Clin. Anaesthesiol. 20, 483–491 (2006).
Smith, I. et al. Perioperative fasting in adults and children: guidelines from the European Society of Anaesthesiology. Eur. J. Anaesthesiol. 28, 556–569 (2011).
Association of Anaesthetists of Great Britain and Ireland (AAGBI). Pre-operative Assessment and Patient Preparation. The Role of the Anaesthetist [online], (2010).
Ljungqvist, O. Jonathan E. Rhoads lecture 2011: insulin resistance and enhanced recovery after surgery. JPEN J. Parenter. Enteral Nutr. 36, 389–398 (2012).
Nygren, J. The metabolic effects of fasting and surgery. Best Pract. Res. Clin. Anaesthesiol. 20, 429–438 (2006).
Crowe, P. J., Dennison, A. & Royle, G. T. The effect of pre-operative glucose loading on postoperative nitrogen metabolism. Br. J. Surg. 71, 635–637 (1984).
Svanfeldt, M. et al. Randomized clinical trial of the effect of preoperative oral carbohydrate treatment on postoperative whole-body protein and glucose kinetics. Br. J. Surg. 94, 1342–1350 (2007).
Yuill, K. A., Richardson, R. A., Davidson, H. I., Garden, O. J. & Parks, R. W. The administration of an oral carbohydrate-containing fluid prior to major elective upper-gastrointestinal surgery preserves skeletal muscle mass postoperatively—a randomised clinical trial. Clin. Nutr. 24, 32–37 (2005).
Henriksen, M. G. et al. Effects of preoperative oral carbohydrates and peptides on postoperative endocrine response, mobilization, nutrition and muscle function in abdominal surgery. Acta Anaesthesiol. Scand. 47, 191–199 (2003).
Awad, S., Varadhan, K. K., Ljungqvist, O. & Lobo, D. N. A meta-analysis of randomised controlled trials on preoperative oral carbohydrate treatment in elective surgery. Clin. Nutr. 32, 34–44 (2013).
Prentis, J. M. et al. Impaired cardiopulmonary reserve in an elderly population is related to postoperative morbidity and length of stay after radical cystectomy. BJU Int. 112, E13–E19 (2013).
Wilson, R. J., Davies, S., Yates, D., Redman, J. & Stone, M. Impaired functional capacity is associated with all-cause mortality after major elective intra-abdominal surgery. Br. J. Anaesth. 105, 297–303 (2010).
Valkenet, K. et al. The effects of preoperative exercise therapy on postoperative outcome: a systematic review. Clin. Rehabil. 25, 99–111 (2011).
O'Doherty, A. F., West, M., Jack, S. & Grocott, M. P. Preoperative aerobic exercise training in elective intra-cavity surgery: a systematic review. Br. J. Anaesth. 110, 679–689 (2013).
Walker, K. J. & Smith, A. F. Premedication for anxiety in adult day surgery. Cochrane Database of Systematic Reviews, Issue 7. Art. No.: CD002192. http://dx.doi.org/10.1002/14651858.CD002192.pub2.
Lepouse, C., Lautner, C. A., Liu, L., Gomis, P. & Leon, A. Emergence delirium in adults in the post-anaesthesia care unit. Br. J. Anaesth. 96, 747–753 (2006).
Gustafsson, U. O. et al. Enhanced Recovery After Surgery Society. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Clin. Nutr. 31, 783–800 (2012).
Jorgensen, H., Wetterslev, J., Moiniche, S. & Dahl, J. B. Epidural local anaesthetics versus opiate based analgesic regimes on post operative gastointesinal paralysis, PONV and pain after abdominal surgery. Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD001893. http://dx.doi.org/10.1002/14651858.CD001893.
Lassen, K. et al. Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch. Surg. 144, 961–969 (2009).
Levy, B. F., Scott, M. J., Fawcett, W., Fry, C. & Rockall, T. A. Randomized clinical trial of epidural, spinal or patient-controlled analgesia for patients undergoing laparoscopic colorectal surgery. Br. J. Surg. 98, 1068–1078 (2011).
Wongyingsinn, M. et al. Spinal analgesia for laparoscopic colonic resection using an enhanced recovery after surgery program. Better analgesia, but no benefits on postoperative recovery: a randomised controlled trial. Br. J. Anaesth. 108, 850–856 (2012).
Maffezzini, M., Campodonico, F., Canepa, G., Gerbi, G. & Parodi, D. Current perioperative management of radical cystectomy with intestinal urinary reconstruction for muscle-invasive bladder cancer and reduction of the incidence of postoperative ileus. Surg. Oncol. 17, 41–48 (2008).
Mukhtar, S., Ayres, B. E., Issa, R., Swinn, M. J. & Perry, M. J. A. Challenging boundaries: an enhanced recovery program for radical cystectomy. Ann. R. Coll. Surg. Engl. 95, 200–206 (2013).
Blick, C. et al. The use of a multimodal enhanced recovery program for patients undergoing radical cystectomy. J. Clin. Urol. 234, 234–238 (2013).
Smith, J. et al. The evolution of the Southampton Enhanced Recovery Program for radical cystectomy and the aggregation of marginal gains. BJU Int. http://dx.doi.org/10.1111/bju.12644.
Dutton, T. J., McGrath, J. S. & Daugherty, M. O. Use of rectus sheath catheters for pain relief in patients undergoing major pelvic urological surgery. BJU Int. 113, 246–253 (2014).
Pruthi, R. D. S., Chun, J. & Richman, M. Reducing time to oral diet and hospital discharge in patients undergoing radical cystectomy using a perioperative care plan. Urology 62, 661–665 (2003).
Bundgaard-Nielsen, M., Secher, N. H. & Kehlet, H. Liberal vs restrictive perioperative fluid therapy—a critical assessment of the evidence. Acta Anaesthesiol. Scand. 53, 843–851 (2009).
Pillai, P. et al. A double-blind randomized controlled clinical trial to access the effect of Doppler optimized intraoperative fluid management on outcome following radical cystectomy. J. Urol. 186, 2201–2206 (2011).
Knott, A. et al. Consensus views on implementation and measurement of enhanced recovery after surgery in England: Delphi study. BMJ Open 2, e001878 (2012).
Powell-Tuck, J. et al. British Consensus Guidelines on Intravenous Fluid Therapy for Adult Surgical Patients [online], (2008).
Harper, C. M., McNicholas, T. & Gowrie-Mohan, S. Maintaining perioperative normothermia. BMJ 326, 721–722 (2003).
Moola, S. & Lockwood, C. Effectiveness of strategies for the management and/or prevention of hypothermia within the adult perioperative environment. Int. Evid. Based Healthc. 9, 337–345 (2011).
Camus, Y., Dleva, E., Cohen, S. & Lienhart, A. The effects of warming intravenous fluids on intraoperative hypothermia and postoperative shivering during prolonged abdominal surgery. Acta Anaesthesiol. Scand. 40, 779–782 (1996).
European Association of Urology. Guidelines on Urological Infections [online], (2011).
American Urological Association. Best Practice Policy Statement on Urologic Surgery Antimicrobial Prophylaxis [online], (2008).
Maiwald, M. & Chan, E. S. The forgotten role of alcohol: a systematic review and meta-analysis of the clinical efficacy and perceived role of chlorhexidine in skin antisepsis. PLoS ONE 7, e44277 (2012).
Dyer, J., Wyke, S. & Lynch, C. Hospital Episode Statistics data analysis of postoperative venous thromboembolus in patients undergoing urological surgery: a review of 126,891 cases. Ann. R. Coll. Surg. Engl. 95, 65–69 (2013).
Clément, C. et al. Incidence, risk profile and morphological pattern of lower extremity venous thromboembolism after urological cancer surgery. J. Urol. 186, 2293–2297 (2011).
Vandlac, A. A. et al. Timing, incidence, and risk factors of venous thromboembolism in patients undergoing radical cystectomy for malignancy: A case for extended duration pharmacologic prophylaxis. J. Urol. 191, 943–947 (2014).
Rasmussen, M. S., Jørgensen, L. N. & Wille-Jørgensen, P. Prolonged thromboprophylaxis with low molecular weight heparin for abdominal or pelvic surgery. Cochrane Database of Systematic Reviews, Issue 1. Art. No.: CD004318. http://dx.doi.org/10.1002/14651858.CD004318.
American Urological Association. Best Practice Policy Statement for the Prevention of Deep Vein Thrombosis in Patients Undergoing Urologic Surgery [online], (2008).
National Institute for Health and Clinical Excellence. Venous thromboembolism: reducing the risk [online], (2010).
The British Association of Urological Surgeons. Analysis of cystectomy dataset January–December 2011 [online], (2012).
Kluth, L. A. et al. Impact of perioperative blood transfusion on the outcome of patients undergoing radical cystectomy for urothelial carcinoma of the bladder. BJU Int. 113, 393–398 (2014).
Linder, B. J. et al. The impact of perioperative blood transfusion on cancer recurrence and survival following radical cystectomy. Eur. Urol. 63, 839–845 (2013).
Aning, J. et al. Towards bloodless cystectomy: a 10-year experience of intra-operative cell salvage during radical cystectomy. BJU Int. 110, E608–E613 (2012).
Waters, J. H., Yazer, M., Chen, Y. F. & Kloke, J. Blood salvage and cancer surgery: a meta-analysis of available studies. Transfusion 52, 2167–2173 (2012).
Dutton, T. J., Daugherty, M. O., Mason, R. G. & McGrath, J. S. Implementation of the Exeter enhanced recovery programme for patients undergoing radical cystectomy. BJU Int. 113, 719–725 (2014).
Warde, N. Bladder cancer: Reperitonealization after extended PLND and cystectomy improves postoperative pain and recovery of bowel function. Nat. Rev. Urol. 8, 8 (2011).
Roth, B. et al. Readaptation of the peritoneum following extended pelvic lymphadenectomy and cystectomy has a significant beneficial impact on early postoperative recovery and complications: results of a prospective randomized trial. Eur. Urol. 59, 204–210 (2011).
Collins, J. & Wiklund, N. Totally intracorporeal robot assisted radical cystectomy: optimizing total outcomes. BJU Int. http://dx.doi.org/10.1111/bju.12558.
Pruthi, R. S. et al. Robotic radical cystectomy for bladder cancer: surgical and pathological outcomes in 100 consecutive cases. J. Urol. 183, 510–514 (2010).
Ahmed, K. et al. Analysis of intracorporeal compared with extracorporeal urinary diversion after robot-assisted radical cystectomy: results from the International Robotic Cystectomy Consortium. Eur. Urol. 65, 340–347 (2014).
Li, K. et al. Systematic review and meta-analysis of comparative studies reporting early outcomes after robot-assisted radical cystectomy versus open radical cystectomy. Cancer Treat. Rev. 39, 551–560 (2013).
Nix, J. et al. Prospective randomized controlled trial of robotic versus open radical cystectomy for bladder cancer: perioperative and pathologic results. Eur. Urol. 57, 196–201 (2010).
Karliczek, A. et al. Drainage or nondrainage in elective colorectal anastomosis: a systematic review and meta-analysis. Colorectal Dis. 8, 259–265 (2006).
Nelson, R., Edwards, S. & Tse, B. Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database of Systematic Reviews, Issue 3. Art. No.: CD004929. http://dx.doi.org/10.1002/14651858.CD004929.
Schroeder, D., Gillanders, L., Mahr, K. & Hill, G. L. Effects of immediate postoperative enteral nutrition on body composition, muscle function, and wound healing. J. Parenter. Enter. Nutr. 15, 376–383 (1991).
Osland, E., Yunus, R. M., Khan, S. & Memon, M. A. Early versus traditional postoperative feeding in patients undergoing resectional gastrointestinal surgery: a meta-analysis. J. Parenter. Enter. Nutr. 35, 473–487 (2011).
Holte, K. et al. Epidural anesthesia, hypotension, and changes in intravascular volume. Anesthesiology 100, 281–286 (2004).
Soni, N. British consensus guidelines on intravenous fluid therapy for adult surgical patients (GIFTASUP): Cassandra's view. Anaesthesia 64, 235–238 (2009).
Choi, H. et al. Chewing gum has a stimulatory effect on bowel motility in patients after open or robotic radical cystectomy for bladder cancer: a prospective randomized comparative study. Urology 77, 884–890 (2011).
Kouba, E. J., Wallen, E. M. & Pruthi, R. S. Gum chewing stimulates bowel motility in patients undergoing radical cystectomy with urinary diversion. Urology 70, 1053–1056 (2007).
Traut, U. et al. Systemic procinetic pharmacologic treatment for postoperative adynamic ileus following abdominal surgery in adults. Cochrane Database Systematic Reviews, Issue 1. Art. No.: CD004930. http://dx.doi.org/10.1002/14651858.CD004930.
Lightfoot, A. J. et al. Treatment of postoperative ileus after bowel surgery with low-dose intravenous erythromycin. Urology 69, 611–615 (2007).
Pruthi, R. S. et al. Fast track program in patients undergoing radical cystectomy: results in 362 consecutive patients. J. Am. Coll. Surg. 210, 93–99 (2010).
Vaughan-Shaw, P. G., Fecher, I. C., Harris, S. & Knight, J. S. A meta-analysis of the effectiveness of the opioid receptor antagonist alvimopan in reducing hospital length of stay and time to GI recovery in patients enrolled in a standardized accelerated recovery program after abdominal surgery. Dis. Colon Rectum 55, 611–620 (2012).
Kauf, T. L. et al. Alvimopan, a peripherally acting mu-opioid receptor antagonist, is associated with reduced costs after radical cystectomy-economic analysis of a phase 4 randomized, controlled trial. J. Urol. 191, 1721–1727 (2014).
Lee, C. et al. Alvimopan accelerates gastrointestinal recovery after radical cystectomy: a multicentre randomized placebo-controlled trial. Eur. Urol. http://dx.doi.org/10.1016/j.eururo.2014.02.036.
Coxib and tradiotional NSAID trialists' (CNT) collaboration. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Lancet 382, 769–779 (2013).
Klein, M., Gogenur, I. & Rosenberg, J. Postoperative use of non-steroidal anti-inflammatory drugs in patients with anastomotic leakage requiring reoperation after colorectal resection: cohort study based on prospective data. BMJ 345, e6166 (2012).
Lassen, K. et al. Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch. Surg. 144, 961–969 (2009).
Henriksen, M. G., Jensen, M. B., Hansen, H. V., Jespersen, T. W. & Hesso, I. Enforced mobilization, early oral feeding, and balanced analgesia improve convalescence after colorectal surgery. Nutrition 18, 147–152 (2002).
Vlug, M. S. et al. Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann. Surg. 254, 868–875 (2011).
Arumainayagam, N., McGrath, J., Jefferson, K. P. & Gillatt, D. Introduction of an enhanced recovery protocol for radical cystectomy. BJU Int. 101, 698–701 (2008).
Karl, A. et al. A new concept for early recovery after surgery in patients undergoing radical cystectomy for bladder cancer: results of a prospective randomized study. J. Urol. 191, 335–340 (2014).
Ohno, T. Eliminate muda, mura, muri completely [online], (2004).
Pruthi, R. S. & Raynor, M. C. Enhanced recovery programmes: an important step towards going lean in healthcare. BJU Int. 113, 685–686 (2014).
Author information
Authors and Affiliations
Contributions
J.S. researched data for the article and wrote the article. All authors made a substantial contribution to discussion of its content and reviewed/edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Smith, J., Pruthi, R. & McGrath, J. Enhanced recovery programmes for patients undergoing radical cystectomy. Nat Rev Urol 11, 437–444 (2014). https://doi.org/10.1038/nrurol.2014.164
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2014.164
This article is cited by
-
Association between use of ERAS protocols and complications after radical cystectomy
World Journal of Urology (2022)
-
Comparison of intracorporeal and extracorporeal urinary diversions after laparoscopic radical cystectomy in females with bladder cancer
World Journal of Surgical Oncology (2019)
-
The Preoperative Assessment and Optimization of Patients Undergoing Major Urological Surgery
Current Urology Reports (2017)
-
Current Status of Robot-Assisted Radical Cystectomy and Intracorporeal Urinary Diversion
Current Urology Reports (2016)
-
Enhanced Recovery Protocols (ERP) in Robotic Cystectomy Surgery. Review of Current Status and Trends
Current Urology Reports (2015)