Abstract
Hydrocele is defined as an abnormal collection of serous fluid in the potential space between the parietal and visceral layers of the tunica vaginalis. In the majority of affected adolescents, hydrocele is acquired and is idiopathic in origin. The pathogenesis of idiopathic hydrocele is thought to be an imbalance in the normal process of fluid production and reabsorption. The diagnosis is usually clinical. Taking a thorough history is essential to rule out any fluctuation in size, which is an indication of a patent processus vaginalis. Scrotal ultrasonography is mandatory in nonpalpable testicles to rule out a subtending testicular solid mass requiring inguinal exploration. Otherwise, open hydrocelectomy via a scrotal incision is the standard treatment of idiopathic hydroceles. The second most common cause of hydrocele in adolescents is varicocelectomy. The risk of hydrocele formation is higher with non-artery-sparing procedures or those performed without microsurgical aid, and in surgery requiring cord dissection. If hydrocele occurs after varicocelectomy, initial management should include observation with or without hydrocele aspiration. Large persistent hydroceles are best served by open hydrocelectomy.
Key Points
-
Hydrocele in adolescents is most often idiopathic and seldom owing to a persistently patent processus vaginalis
-
Varicocelectomy is the second most common cause of hydrocele in adolescents in developed countries; prevalence varies according to surgical technique
-
The diagnosis of hydrocele is generally clinical, but idiopathic cases with a nonpalpable testicle should undergo scrotal ultrasonography to rule out a subtending solid testicular mass
-
Open hydrocelectomy via scrotal incision is the standard approach for idiopathic hydrocele in adolescents
-
Observation should be the initial approach in postvaricocelectomy hydrocele, unless the hydrocele is very large and tense
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Wallace, A. F. Aetiology of the idiopathic hydrocele. Br. J. Urol. 32, 79–96 (1969).
Rubenstein, R. A., Dogra, V. S., Seftel, A. D. & Resnick, M. I. Benign intrascrotal lesions. J. Urol. 171, 1765–1772 (2004).
Oyen, R. H. Scrotal ultrasound. Eur. Radiol. 12, 19–34 (2002).
Leung, M. L., Gooding, G. A. & Williams, R. D. High-resolution sonography of scrotal contents in asymptomatic subjects. AJR Am. J. Roentgenol. 143, 161–164 (1984).
Turgut, A. T. et al. A novel parameter by EFOV US for the quantification and the distinction of physiological amount of scrotal fluid and hydrocele: ratio of testis volume/scrotum volume. Eur. J. Radiol. 63, 414–419 (2007).
Christensen, T., Cartwright, P. C., Devries, C. & Snow, B. W. New onset of hydroceles in boys over 1 year of age. Int. J. Urol. 13, 1425–1427 (2006).
Wilson, J. M., Aaronson, D. S., Schrader, R. & Baskin, L. S. Hydrocele in the pediatric patient: inguinal or scrotal approach? J. Urol. 180, 1724–1727 (2008).
Ozdilek, S. The pathogenesis of idiopathic hydrocele and a simple operative technique. J. Urol. 77, 282–284 (1957).
Rinker, J. R. & Allen, L. A lymphatic defect in hydrocele. Am. Surg. 17, 681–686 (1951).
Pierik, F. H., Dohle, G. R., van Muiswinkel, J. M., Vreeburg, J. T. & Weber, R. F. Is routine scrotal ultrasound advantageous in infertile men? J. Urol. 162, 1618–1620 (1999).
Misseri, R., Gershbein, A. B., Horowitz, M. & Glassberg, K. I. The adolescent varicocele. II: the incidence of hydrocele and delayed recurrent varicocele after varicocelectomy in a long-term follow-up. BJU Int. 87, 494–498 (2001).
Esposito, C. et al. Incidence and management of hydrocele following varicocele surgery in children. J. Urol. 171, 1271–1273 (2004).
Hassan, J. M., Adams, M. C., Pope, J. C. 4th, Demarco, R. T. & Brock, J. W. 3rd. Hydrocele formation following laparoscopic varicocelectomy. J. Urol. 175, 1076–1079 (2006).
Ein, S. H., Nasr, A., Wales, P. & Gerstle, T. The very large recurrent postoperative scrotal hydrocele after pediatric inguinal hernia repair: a rare problem. Pediatr. Surg. Int. 25, 239–241 (2009).
Lemack, G. E., Uzzo, R. G., Schlegel, P. N. & Goldstein, M. Microsurgical repair of the adolescent varicocele. J. Urol. 160, 179–181 (1998).
Minevich, E., Wacksman, J., Lewis, A. G. & Sheldon, C. A. Inguinal microsurgical varicocelectomy in the adolescent: technique and preliminary results. J. Urol. 159, 1022–1024 (1998).
Cayan, S., Acar, D., Ulger, S. & Akbay, E. Adolescent varicocele repair: long-term results and comparison of surgical techniques according to optical magnification use in 100 cases at a single university hospital. J. Urol. 174, 2003–2006 (2005).
Yaman, O., Soygur, T., Zumrutbas, A. E. & Resorlu, B. Results of microsurgical subinguinal varicocelectomy in children and adolescents. Urology 68, 410–412 (2006).
Zaupa, P., Mayr, J. & Höllwarth, M. E. Antegrade scrotal sclerotherapy for treating primary varicocele in children. BJU Int. 97, 809–812 (2006).
Beutner, S. et al. Treatment of varicocele with reference to age: a retrospective comparison of three minimally invasive procedures. Surg. Endosc. 21, 61–65 (2007).
Diamond, D. A. et al. Varicocele surgery: a decade's experience at a children's hospital. BJU Int. 104, 246–249 (2009).
DeVries, C. R. The role of the urologist in the treatment and elimination of lymphatic filariasis worldwide. BJU Int. 89 (Suppl. 1), 37–43 (2002).
Noroes, J. et al. Pathogenesis of filarial hydrocele: risk associated with intrascrotal nodules caused by death of adult Wuchereria bancrofti. Trans. R. Soc. Trop. Med. Hyg. 97, 561–566 (2003).
Taskinen, S., Fagerholm, R., Aronniemi, J., Rintala, R. & Taskinen, M. Testicular tumors in children and adolescents. J. Pediatr. Urol. 4, 134–137 (2008).
Wolanske, K. & Nino-Murcia, M. Malignant mesothelioma of the tunica vaginalis testis: atypical sonographic appearance. J. Ultrasound Med. 20, 69–72 (2001).
de Lima, G. R. et al. A rare case of malignant hydrocele in a young patient. J. Pediatr. Urol. 5, 243–245 (2009).
Zaslau, S., Perlmutter, A. E., Farivar-Mohseni, H., Chang, W. W. & Kandzari, S. J. Rhabdomyosarcoma of tunica vaginalis masquerading as hydrocele. Urology 65, 1001 (2005).
Tarantino, L., Giorgio, A., de Stefano, G. & Farella, N. Echo color Doppler findings in postpubertal mumps epididymo-orchitis. J. Ultrasound Med. 20, 1189–1195 (2001).
Cozzi, D. A. et al. Infantile abdominoscrotal hydrocele: a not so benign condition. J. Urol. 180, 2611–2615 (2008).
Turgut, A. T. et al. Unilateral idiopathic hydrocele has a substantial effect on the ipsilateral testicular geometry and resistivity indices. J. Ultrasound Med. 25, 837–843 (2006).
Nye, P. J. & Prati, R. C. Jr. Idiopathic hydrocele and absent testicular diastolic flow. J. Clin. Ultrasound 25, 43–46 (1997).
Ahorlu, C. K., Dunyo, S. K., Asamoah, G. & Simonsen, P. E. Consequences of hydrocele and the benefits of hydrocelectomy: a qualitative study in lymphatic filariasis endemic communities on the coast of Ghana. Acta Trop. 80, 215–221 (2001).
Ku, J. H., Kim, M. E., Lee, N. K. & Park, Y. H. The excisional, plication and internal drainage techniques: a comparison of the results for idiopathic hydrocele. BJU Int. 87, 82–84 (2001).
Ali, M. Z. Fournier's gangrene—a rare complication of hydrocele aspiration. J. Coll. Physicians Surg. Pak. 14, 304–305 (2004).
Horstman, W. G. Scrotal imaging. Urol. Clin. North Am. 24, 653–671 (1997).
Norões, J. et al. Ultrasonographic evidence of abnormal lymphatic vessels in young men with adult Wuchereria bancrofti infection in the scrotal area. J. Urol. 156, 409–412 (1996).
Bassel, Y. S., Scherz, H. C. & Kirsch, A. J. Scrotal incision for undescended testes with or without a patent processus vaginalis. J. Urol. 177, 1516–1518 (2007).
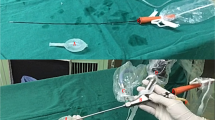
Onol, S. Y. et al. A novel pull-through technique for the surgical management of idiopathic hydrocele. J. Urol. 181, 1201–1205 (2009).
Lord, P. H. A bloodless operation for the radical cure of idiopathic hydrocele. Br. J. Surg. 51, 914–916 (1964).
Singh, D. R., Gupta, S. K. & Gupta, S. Lord's procedure: a curative outpatient operation for primary hydrocele. J. Indian Med. Assoc. 94, 141–142 (1996).
Shah, P. A., Dewoolkar, V. V. & Changlani, T. T. Ambulatory hydrocele surgery: a review of 50 cases. J. R. Coll. Surg. Edinb. 37, 385–386 (1992).
Nigam, V. K. Window operation: new technique for hydrocele. Urology 24, 481–482 (1984).
Arslan, M., Kilinç, M., Yilmaz, K. & Oztürk, A. A new approach in the management of the hydrocele with a silicone catheter. Urology 63, 170–173 (2004).
Rodriguez, W. C., Rodriguez, D. D. & Fortuno, R. F. The operative treatment of hydrocele: a comparison of 4 basic techniques. J. Urol. 125, 804–805 (1981).
Albrecht, W., Höltl, W. & Aharinejad, S. Lord's procedure—the best operation for hydrocele? Br. J. Urol. 68, 187–189 (1991).
Kiddoo, D. A., Wollin, T. A. & Mador, D. R. A population based assessment of complications following outpatient hydrocelectomy and spermatocelectomy. J. Urol. 171, 746–748 (2004).
Hopps, C. V. & Goldstein, M. Microsurgical reconstruction of iatrogenic injuries to the epididymis from hydrocelectomy. J. Urol. 176, 2077–2079 (2006).
Beiko, D. T., Kim, D. & Morales, A. Aspiration and sclerotherapy versus hydrocelectomy for treatment of hydroceles. Urology 61, 708–712 (2003).
Shan, C. J., Lucon, A. M. & Arap, S. Comparative study of sclerotherapy with phenol and surgical treatment for hydrocele. J. Urol. 169, 1056–1059 (2003).
Fracchia, J. A., Armenakas, N. A. & Kohan, A. D. Cost-effective hydrocele ablation. J. Urol. 159, 864–867 (1998).
Musa, M. T., Fahal, A. H. & el Arabi, Y. E. Aspiration sclerotherapy for hydroceles in the tropics. Br. J. Urol. 76, 488–490 (1995).
Bullock, N. & Thurston, A. V. Tetracycline sclerotherapy for hydroceles and epididymal cysts. Br. J. Urol. 59, 340–342 (1987).
Stattin, P., Karlberg, L. & Damber, J. E. Long-term outcome of patients treated for hydrocele with the sclerosant agent sodium tetradecyl sulphate. Scand. J. Urol. Nephrol. 30, 109–113 (1996).
Badenoch, D. F., Fowler, C. G., Jenkins, B. J., Roberts, J. V. & Tiptaft, R. C. Aspiration and instillation of tetracyline in the treatment of testicular hydrocele. Br. J. Urol. 59, 172–173 (1987).
Khaniya, S., Agrawal, C. S., Koirala, R., Regmi, R. & Adhikary, S. Comparison of aspiration-sclerotherapy with hydrocelectomy in the management of hydrocele: a prospective randomized study. Int. J. Surg. 7, 392–395 (2009).
Van der Brink, B. A., Palmer, L. S., Gitlin, J., Levitt, S. B. & Franco, I. Lymphatic-sparing laparoscopic varicocelectomy versus microscopic varicocelectomy: is there a difference? Urology 70, 1207–1210 (2007).
Glassberg, K. I., Poon, S. A., Gjertson, C. K., DeCastro, G. J. & Misseri, R. Laparoscopic lymphatic sparing varicocelectomy in adolescents. J. Urol. 180, 326–330 (2008).
Oswald, J., Körner, I. & Riccabona, M. The use of isosulphan blue to identify lymphatic vessels in high retroperitoneal ligation of adolescent varicocele—avoiding postoperative hydrocele. BJU Int. 87, 502–504 (2001).
Schwentner, C. et al. Laparoscopic varicocele ligation in children and adolescents using isosulphan blue: a prospective randomized trial. BJU Int. 98, 861–865 (2006).
Makari, J. H. et al. Safety and efficacy of intratesticular injection of vital dyes for lymphatic preservation during varicocelectomy. J. Urol. 178, 1026–1030 (2007).
Barroso, U. Jr, Andrade, D. M., Novaes, H., Netto, J. M. & Andrade, J. Surgical treatment of varicocele in children with open and laparoscopic Palomo technique: a systematic review of the literature. J. Urol. 181, 2724–2728 (2009).
Castagnetti, M., Cimador, M., DiPace, M. R., Catalano, P. & De Grazia, E. 'Preemptive hydrocelectomy' in subinguinal varicocelectomy. Urol. Int. 81, 14–16 (2008).
Tsikopoulos, G. K., Roussis, X. S., Georgakis, J., Papouis, G. & Tryfonas, G. J. Does incision of the tunica vaginalis during the Palomo procedure prevent post-operative hydrocele? Br. J. Urol. 81, 612–613 (1998).
Castagnetti, M. et al. Evolving management of adolescent varicocele. J. Pediatr. Urol. 4, 107–112 (2008).
Zampieri, N., El-Dalati, G., Ottolenghi, A. & Camoglio, F. S. Percutaneous aspiration for hydroceles after varicocelectomy. Urology 74, 1122–1124 (2009).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Cimador, M., Castagnetti, M. & De Grazia, E. Management of hydrocele in adolescent patients. Nat Rev Urol 7, 379–385 (2010). https://doi.org/10.1038/nrurol.2010.80
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2010.80
This article is cited by
-
A pictorial review of scrotal and penile pathology on computed tomography
Emergency Radiology (2024)
-
Watchful waiting for communicating hydrocoele in infants
Egyptian Pediatric Association Gazette (2022)
-
Updated classification system for primary hydrocele
Abdominal Radiology (2022)
-
A comparison of a novel endoscopic “Su-Wang technique” with the open “Jaboulay’s procedure” for the surgical treatment of adult primary vaginal hydrocele
Scientific Reports (2019)
-
Multiparametric ultrasonography of the testicles
Nature Reviews Urology (2013)