Abstract
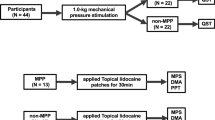
The aim of this Review is to give a short presentation of the manifestations, assessment methods, and mechanisms underlying localized and widespread musculoskeletal pain, deep somatic tissue hyperalgesia and chronification. Hyperalgesia can be explained by increased pain sensitivity of nociceptors located in deep tissue (peripheral sensitization) or by increased responses from dorsal horn neurons (central sensitization). The spreading of pain and sensitization is related to increased synaptic activity in central neurons and to changes in descending control from supraspinal centers. Manifestations related to the different aspects of sensitization can be assessed quantitatively using sensory tests, such as pressure algometry (quantitative palpation) and cuff-algometry. Repeated pressure stimulation can evaluate the degree of temporal summation, which is a proxy for the level of central sensitization, as is expanded referred muscle pain area. The transition of acute localized musculoskeletal pain into chronic widespread pain is related to the progression of peripheral and central sensitization. This sensitization for the chronification of pain should be assessed by adequate pain biomarkers. Furthermore, pain prevention should target early intervention strategies and new anti-hyperalgesic compounds should be developed.
Key Points
-
The different manifestations of localized, regional and widespread musculoskeletal pain involve different peripheral and central mechanisms
-
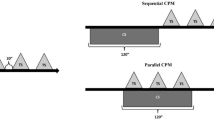
Methodologies are available for quantitative assessment of musculoskeletal pain targeting specific mechanisms such as hyperalgesia, spreading sensitization, temporal summation and pain referral
-
Peripheral and central sensitization are key neurophysiologic mechanisms in musculoskeletal pain
-
Central sensitization is a likely reason for the chronification of widespread pain conditions
-
The transition of acute localized musculoskeletal pain into chronic widespread pain is probably related to the progression of peripheral and central sensitization
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Smart, K. M., Blake, C., Staines, A. & Doody, C. Clinical indicators of 'nociceptive', 'peripheral neuropathic' and 'central' mechanisms of musculoskeletal pain. A Delphi survey of expert clinicians. Man. Ther. 15, 80–87 (2010).
Nijs, J., Van Houdenhove, B. & Oostendorp, R. A. Recognition of central sensitization in patients with musculoskeletal pain: application of pain neurophysiology in manual therapy practice. Man. Ther. 15, 135–141 (2010).
Mense, S., Simons, D. G. & Russell, I. J. Muscle Pain: Understanding Its Nature, Diagnosis, and Treatment (Lippincott Williams & Wilkins, Philadelphia, 2001).
Graven-Nielsen, T. Fundamentals of muscle pain, referred pain, and deep tissue hyperalgesia. Scand. J. Rheumatol. 35 (Suppl. 122), 1–43 (2006).
Kellgren, J. H. Observations on referred pain arising from muscle. Clin. Sci. 3, 175–190 (1938).
Simons, D. G., Travell, J. G. & Simons, L. S. Myofascial Pain and Dysfunction: the Trigger Point Manual (Lippincott Williams & Wilkins, Philadelphia, 1999).
Wolfe, F. et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Report of the multicenter criteria committee. Arthritis Rheum. 33, 160–172 (1990).
Carli, G., Suman, A. L., Biasi, G. & Marcolongo, R. Reactivity to superficial and deep stimuli in patients with chronic musculoskeletal pain. Pain 100, 259–269 (2002).
Felson, D. T. The sources of pain in knee osteoarthritis. Curr. Opin. Rheumatol. 17, 624–628 (2005).
Neugebauer, V., Lücke, T. & Schaible, H. G. N-methyl-D-aspartate (NMDA) and non-NMDA receptor antagonists block the hyperexcitability of dorsal horn neurons during development of acute arthritis in rat's knee joint. J. Neurophysiol. 70, 1365–1377 (1993).
Schaible, H. G. Spinal mechanisms contributing to joint pain. Novartis Found. Symp. 260, 4–22 (2004).
Martindale, J. C., Wilson, A. W., Reeve, A. J., Chessell, I. P. & Headley, P. M. Chronic secondary hypersensitivity of dorsal horn neurones following inflammation of the knee joint. Pain 133, 79–86 (2007).
Imamura, M. et al. Impact of nervous system hyperalgesia on pain, disability, and quality of life in patients with knee osteoarthritis: a controlled analysis. Arthritis Rheum. 59, 1424–1431 (2008).
Arendt-Nielsen, L. et al. Sensitization in patients with painful knee osteoarthritis. Pain doi: 10.1016/j.pain.2010.04.003.
Mense, S. Nociception from skeletal muscle in relation to clinical muscle pain. Pain 54, 241–289 (1993).
Sessle, B. J., Hu, J. W. & Yu, X. M. In New Trends in Referred Pain and Hyperalgesia Ch. 6 (eds Vecchiet, L., Albe-Fessard, D., Lindblom, U. & Giamberardino, M. A.) 59–71 (Elsevier Science Publishers B. V., Amsterdam, 1993).
Marchettini, P., Simone, D. A., Caputi, G. & Ochoa, J. L. Pain from excitation of identified muscle nociceptors in humans. Brain Res. 7 40, 109–116 (1996).
Chapman, C. R. et al. Pain measurement: an overview. Pain 22, 1–31 (1985).
Gracely, R. H. In Wall and Melzack's Textbook of Pain Ch. 17 (eds McMahon, S. B. & Koltzenburg, M.) 267–289 (Elsevier, Churchill Livingstone, 2006).
Turk, D. C. & Melzack, R. Handbook of Pain Assessment (Guilford, New York, 1992).
Svensson, P. & Arendt-Nielsen, L. Induction and assessment of experimental muscle pain. J. Electromyogr. Kinesiol. 5, 131–140 (1995).
Jensen, K., Andersen, H. O., Olesen, J. & Lindblom, U. Pressure-pain threshold in human temporal region. Evaluation of a new pressure algometer. Pain 2 5, 313–323 (1986).
Chesterton, L. S., Sim, J., Wright, C. C. & Foster, N. E. Interrater reliability of algometry in measuring pressure pain thresholds in healthy humans, using multiple raters. Clin. J. Pain 23, 760–766 (2007).
Graven-Nielsen, T., Mense, S. & Arendt-Nielsen, L. Painful and non-painful pressure sensations from human skeletal muscle. Exp. Brain Res. 159, 273–283 (2004).
Polianskis, R., Graven-Nielsen, T. & Arendt-Nielsen, L. Spatial and temporal aspects of deep tissue pain assessed by cuff algometry. Pain 100, 19–26 (2002).
Jespersen, A. et al. Computerized cuff pressure algometry: a new method to assess deep-tissue hypersensitivity in fibromyalgia. Pain 131, 57–62 (2007).
Svendsen, O., Edwards, C. N., Lauritzen, B. & Rasmussen, A. D. Intramuscular injection of hypertonic saline: in vitro and in vivo muscle tissue toxicity and spinal neurone c-fos expression. Basic Clin. Pharmacol. Toxicol. 97, 52–57 (2005).
Mense, S. & Hoheisel, U. In Fundamentals of Musculoskeletal Pain Ch. 1 (eds Graven-Nielsen, T., Arendt-Nielsen, L. & Mense, S.) 3–17 (International Association for the Study of Pain, Seattle, 2008).
Vanderweeën, L., Oostendorp, R. A., Vaes, P. & Duquet, W. Pressure algometry in manual therapy. Man. Ther. 1, 258–265 (1996).
Andersen, H., Ge, H. Y., Arendt-Nielsen, L., Danneskiold-Samsøe, B. & Graven-Nielsen, T. Increased trapezius pain sensitivity is not associated with increased tissue hardness. J. Pain doi: 10.1016/j.jpain.2009.09.017.
Ge, H. Y. et al. Contribution of the local and referred pain from active myofascial trigger points in fibromyalgia syndrome. Pain 147, 233–240 (2009).
Ge, H. Y., Wang, Y., Danneskiold-Samsøe, B., Graven-Nielsen, T. & Arendt-Nielsen, L. The predetermined sites of examination for tender points in fibromyalgia syndrome are frequently associated with myofascial trigger points. J. Pain doi: 10.1016/j.jpain.2009.10.006.
Arendt-Nielsen, L. & Graven-Nielsen, T. Translational Aspects of Musculoskeletal Pain: From Animals to Patients in Fundamentals of Musculoskeletal Pain (eds Graven-Nielsen, T., Arendt-Nielsen, L. & Mense, S.) 347–366 (International Association for the Study of Pain, Seattle, 2008).
Sörensen, J., Graven-Nielsen, T., Henriksson, K. G., Bengtsson, M. & Arendt-Nielsen, L. Hyperexcitability in fibromyalgia. J. Rheumatol. 25, 152–155 (1998).
Wright, A., Graven-Nielsen, T., Davies, I. I. & Arendt-Nielsen, L. Temporal summation of pain from skin, muscle and joint following nociceptive ultrasonic stimulation in humans. Exp. Brain Res. 144, 475–482 (2002).
Graven-Nielsen, T., Arendt-Nielsen, L., Svensson, P. & Jensen, T. S. Quantification of local and referred muscle pain in humans after sequential i.m. injections of hypertonic saline. Pain 69, 111–117 (1997).
Nie, H., Arendt-Nielsen, L., Andersen, H. & Graven-Nielsen, T. Temporal summation of pain evoked by mechanical stimulation in deep and superficial tissue. J. Pain 6, 348–355 (2005).
Staud, R. et al. Temporal summation of pain from mechanical stimulation of muscle tissue in normal controls and subjects with fibromyalgia syndrome. Pain 102, 87–95 (2003).
Staud, R., Craggs, J. G., Perlstein, W. M., Robinson, M. E. & Price, D. D. Brain activity associated with slow temporal summation of C-fiber evoked pain in fibromyalgia patients and healthy controls. Eur. J. Pain 12, 1078–1089 (2008).
Nie, H., Arendt-Nielsen, L., Madeleine, P. & Graven-Nielsen, T. Enhanced temporal summation of pressure pain in the trapezius muscle after delayed onset muscle soreness. Exp. Brain Res. 170, 182–190 (2006).
Banic, B. et al. Evidence for spinal cord hypersensitivity in chronic pain after whiplash injury and in fibromyalgia. Pain 107, 7–15 (2004).
Laursen, R. J., Graven-Nielsen, T., Jensen, T. S. & Arendt-Nielsen, L. The effect of compression and regional anaesthetic block on referred pain intensity in humans. Pain 80, 257–263 (1999).
Hoheisel, U., Mense, S., Simons, D. G. & Yu, X. M. Appearance of new receptive fields in rat dorsal horn neurons following noxious stimulation of skeletal muscle: a model for referral of muscle pain? Neurosci. Lett. 15 3, 9–12 (1993).
Mense, S. Referral of muscle pain. New aspects. Am. Pain Soc. J. 3, 1–9 (1994).
Andersen, H., Arendt-Nielsen, L., Svensson, P., Danneskiold-Samsøe, B. & Graven-Nielsen, T. Spatial and temporal aspects of muscle hyperalgesia induced by nerve growth factor in humans. Exp. Brain Res. 191, 371–382 (2008).
Gibson, W., Arendt-Nielsen, L. & Graven-Nielsen, T. Referred pain and hyperalgesia in human tendon and muscle belly tissue. Pain 120, 113–123 (2006).
Schulte, H. et al. Pharmacological modulation of experimental phasic and tonic muscle pain by morphine, alfentanil and ketamine in healthy volunteers. Acta Anaesthesiol. Scand. 47, 1020–1030 (2003).
Arendt-Nielsen, L. & Graven-Nielsen, T. Central sensitization in fibromyalgia and other musculoskeletal disorders. Curr. Pain Headache Rep. 7, 355–361 (2003).
Graven-Nielsen, T., Curatolo, M. & Mense, S. In Proceedings of the 11th World Congress on Pain Ch. 21 (eds Flor, H., Kalso, E. & Dostrovsky, J. O.) 217–230 (IASP Press, Seattle, 2006).
Hoheisel, U., Sander, B. & Mense, S. Myositis-induced functional reorganisation of the rat dorsal horn: Effects of spinal superfusion with antagonists to neurokinin and glutamate receptors. Pain 69, 219–230 (1997).
Dimcevski, G. et al. Assessment of experimental pain from skin, muscle, and esophagus in patients with chronic pancreatitis. Pancreas 35, 22–29 (2007).
Drewes, A. M. et al. Central sensitization in patients with non-cardiac chest pain: a clinical experimental study. Scand. J. Gastroenterol. 41, 640–649 (2006).
Graven-Nielsen, T. et al. Ketamine reduces muscle pain, temporal summation, and referred pain in fibromyalgia patients. Pain 85, 483–491 (2000).
King, C. D. et al. Deficiency in endogenous modulation of prolonged heat pain in patients with irritable bowel syndrome and temporomandibular disorder. Pain 143, 172–178 (2009).
Kosek, E. & Hansson, P. Modulatory influence on somatosensory perception from vibration and heterotopic noxious conditioning stimulation (HNCS) in fibromyalgia patients and healthy subjects. Pain 70, 41–51 (1997).
Julien, N., Goffaux, P., Arsenault, P. & Marchand, S. Widespread pain in fibromyalgia is related to a deficit of endogenous pain inhibition. Pain 114, 295–302 (2005).
Kosek, E. & Ordeberg, G. Lack of pressure pain modulation by heterotopic noxious conditioning stimulation in patients with painful osteoarthritis before, but not following, surgical pain relief. Pain 88, 69–78 (2000).
Sandrini, G. et al. Abnormal modulatory influence of diffuse noxious inhibitory controls in migraine and chronic tension-type headache patients. Cephalalgia 26, 782–789 (2006).
Arendt-Nielsen, L. & Yarnitsky, D. Experimental and clinical applications of quantitative sensory testing applied to skin, muscles and viscera. J. Pain 10, 556–572 (2009).
Jensen, K. B. et al. Evidence of dysfunctional pain inhibition in fibromyalgia reflected in rACC during provoked pain. Pain 144, 95–100 (2009).
Nie, H., Madeleine, P., Arendt-Nielsen, L. & Graven-Nielsen, T. Temporal summation of pressure pain during muscle hyperalgesia evoked by nerve growth factor and eccentric contractions. Eur. J. Pain 13, 704–710 (2009).
Slater, H., Arendt-Nielsen, L., Wright, A. & Graven-Nielsen, T. Sensory and motor effects of experimental muscle pain in patients with lateral epicondylalgia and controls with delayed onset muscle soreness. Pain 114, 118–130 (2005).
Gracely, R. H., Petzke, F., Wolf, J. M. & Clauw, D. J. Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia. Arthritis Rheum. 46, 1333–1343 (2002).
Giesecke, T. et al. Evidence of augmented central pain processing in idiopathic chronic low back pain. Arthritis Rheum. 50, 613–623 (2004).
Johansen, M. K., Graven-Nielsen, T., Olesen, A. S. & Arendt-Nielsen, L. Generalised muscular hyperalgesia in chronic whiplash syndrome. Pain 83, 229–234 (1999).
Bajaj, P., Bajaj, P., Graven-Nielsen, T. & Arendt-Nielsen, L. Osteoarthritis and its association with muscle hyperalgesia: an experimental controlled study. Pain 93, 107–114 (2001).
O'Neill, S., Manniche, C., Graven-Nielsen, T. & Arendt-Nielsen, L. Generalized deep-tissue hyperalgesia in patients with chronic low-back pain. Eur. J. Pain 11, 415–420 (2007).
Author information
Authors and Affiliations
Contributions
T. Graven-Nielsen & L. Arendt-Nielsen researched the data for the article, provided a substantial contribution to discussions of the content, and contributed equally to writing, reviewing and editing the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Graven-Nielsen, T., Arendt-Nielsen, L. Assessment of mechanisms in localized and widespread musculoskeletal pain. Nat Rev Rheumatol 6, 599–606 (2010). https://doi.org/10.1038/nrrheum.2010.107
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrrheum.2010.107
This article is cited by
-
Conditioned pain modulation (CPM) paradigm type affects its sensitivity as a biomarker of fibromyalgia
Scientific Reports (2024)
-
Effects of interdisciplinary pain rehabilitation programs on neuropathic and non-neuropathic chronic pain conditions – a registry-based cohort study from Swedish Quality Registry for Pain Rehabilitation (SQRP)
BMC Musculoskeletal Disorders (2023)
-
The role of endogenous opioids in mindfulness and sham mindfulness-meditation for the direct alleviation of evoked chronic low back pain: a randomized clinical trial
Neuropsychopharmacology (2023)
-
A novel computational approach to pain perception modelling within a Bayesian framework using quantitative sensory testing
Scientific Reports (2023)
-
Long‐lasting decreased pain threshold negatively affects functional recovery after arthroscopic rotator cuff repair
Knee Surgery, Sports Traumatology, Arthroscopy (2023)