Key Points
-
Most progressive strength and aerobic endurance training programmes have positive effects that last for 12 weeks
-
Extended progressive strength training improves muscle strength for up to 24 months and aerobic endurance training increases walking capacity at 6–16 months
-
Balance training improves balance, gait and mobility, and reduces falls for up to 12 months after completion of treatment
-
Gait training improves gait performance and walking capacity for up to 6 months after training
-
Tai chi and dance improve balance and tai chi reduces fall frequency up to 6 months after training
-
A training period of at least 6 months is effective for achieving clinically meaningful improvement in UPDRS-III scores
Abstract
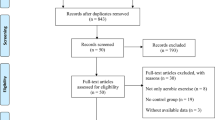
Parkinson disease (PD) is a progressive, neurodegenerative movement disorder with symptoms reflecting various impairments and functional limitations, such as postural instability, gait disturbance, immobility and falls. In addition to pharmacological and surgical management of PD, exercise and physical therapy interventions are also being actively researched. This Review provides an overview of the effects of PD on physical activity — including muscle weakness, reduced aerobic capacity, gait impairment, balance disorders and falls. Previously published reviews have discussed only the short-term benefits of exercises and physical therapy for people with PD. However, owing to the progressive nature of PD, the present Review focuses on the long-term effects of such interventions. We also discuss exercise-induced neuroplasticity, present data on the possible risks and adverse effects of exercise training, make recommendations for clinical practice, and describe new treatment approaches. Evidence suggests that a minimum of 4 weeks of gait training or 8 weeks of balance training can have positive effects that persist for 3–12 months after treatment completion. Sustained strength training, aerobic training, tai chi or dance therapy lasting at least 12 weeks can produce long-term beneficial effects. Further studies are needed to verify disease-modifying effects of these interventions.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
European Parkinson's Disease Association. What is Parkinson's? EPDA http://www.epda.eu.com/en/pd-info/about-parkinsons/ (2015).
Pringsheim, T., Jette, N., Frolkis, A. & Steeves, T. D. The prevalence of Parkinson's disease: a systematic review and meta-analysis. Mov. Disord. 29, 1583–1590 (2014).
Gasser, T. Mendelian forms of Parkinson's disease. Biochim. Biophys. Acta 1792, 587–596 (2009).
Wirdefeldt, K., Adami, H. O., Cole, P., Trichopoulos, D. & Mandel, J. Epidemiology and etiology of Parkinson's disease: a review of the evidence. Eur. J. Epidemiol. 26, 1–58 (2011).
Curtze, C., Nutt, J. G., Carlson-Kuhta, P., Mancini, M. & Horak, F. B. Levodopa is a double-edged sword for balance and gait in people with Parkinson's disease. Mov. Disord. 30, 1361–1370 (2015).
van der Marck, M. A. et al. Consensus-based clinical practice recommendations for the examination and management of falls in patients with Parkinson's disease. Parkinsonism Relat. Disord. 20, 360–369 (2014).
Fox, S. H. et al. The Movement Disorder Society Evidence-Based Medicine review update: treatments for the motor symptoms of Parkinson's disease. Mov. Disord. 26, S2–S41 (2011).
Allen, N. E., Sherrington, C., Paul, S. S. & Canning, C. G. Balance and falls in Parkinson's disease: a meta-analysis of the effect of exercise and motor training. Mov. Disord. 26, 1605–1615 (2011).
Shen, X., Wong-Yu, I. S. & Mak, M. K. Effects of exercise on falls, balance, and gait ability in Parkinson's disease: a meta-analysis. Neurorehabil. Neural Repair. 30, 512–527 (2016).
Tomlinson, C. L. et al. Physiotherapy intervention in Parkinson's disease: systematic review and meta-analysis. BMJ 345, e5004 (2012).
Allen, N. E., Canning, C. G., Sherrington, C. & Fung, V. S. Bradykinesia, muscle weakness and reduced muscle power in Parkinson's disease. Mov. Disord. 24, 1344–1351 (2009).
Bridgewater, K. J. & Sharpe, M. H. Trunk muscle performance in early Parkinson's disease. Phys. Ther. 78, 566 (1998).
Kakinuma, S., Nogaki, H., Pramanik, B. & Morimatsu, M. Muscle weakness in Parkinson's disease: isokinetic study of the lower limbs. Eur. Neurol. 39, 218–222 (1998).
Koller, W. & Kase, S. Muscle strength testing in Parkinson's disease. Eur. Neurol. 25, 130–133 (1986).
Nallegowda, M. et al. Role of sensory input and muscle strength in maintenance of balance, gait, and posture in Parkinson's disease: a pilot study. Am. J. Phys. Med. Rehabil. 83, 898–908 (2004).
Inkster, L. M., Eng, J. J., MacIntyre, D. L. & Stoessl, A. J. Leg muscle strength is reduced in Parkinson's disease and relates to the ability to rise from a chair. Mov. Disord. 18, 157–162 (2003).
Nocera, J. R., Buckley, T., Waddell, D., Okun, M. S. & Hass, C. J. Knee extensor strength, dynamic stability, and functional ambulation: are they related in Parkinson's disease? Arch. Phys. Med. Rehabil. 91, 589–595 (2010).
Allen, N. E. et al. The effects of an exercise program on fall risk factors in people with Parkinson's disease: a randomized controlled trial. Mov. Disord. 25, 1217–1225 (2010).
Latt, M. D., Lord, S. R., Morris, J. G. L. & Fung, V. S. Clinical and physiological assessments for elucidating falls risk in Parkinson's disease. Mov. Disord. 24, 1280–1289 (2009).
Berardelli, A., Rothwell, J. C., Thompson, P. D. & Hallett, M. Pathophysiology of bradykinesia in Parkinson's disease. Brain 124, 2131–2146 (2001).
David, F. J. et al. Progressive resistance exercise and Parkinson's disease: a review of potential mechanisms. Parkinsons Dis. 2012, 124527 (2012).
Glendinning, D. S. & Enoka, R. M. Motor unit behavior in Parkinson's disease. Phys. Ther. 74, 61–70 (1994).
Katzel, L. I. et al. Repeatability of aerobic capacity measurements in Parkinson disease. Med. Sci. Sports Exerc. 43, 2381 (2011).
Canning, C. G., Alison, J. A., Allen, N. E. & Groeller, H. Parkinson's disease: an investigation of exercise capacity, respiratory function, and gait. Arch. Phys. Med. Rehabil. 78, 199–207 (1997).
Saltin, B. & Landin, S. Work capacity, muscle strength and SDH activity in both legs of hemiparetic patients and patients with Parkinson's disease. Scand. J. Clin. Lab. Invest. 35, 531–538 (1975).
Protas, E. J., Stanley, R. K., Jankovic, J. & MacNeill, B. Cardiovascular and metabolic responses to upper-and lower-extremity exercise in men with idiopathic Parkinson's disease. Phys. Ther. 76, 34–40 (1996).
Christiansen, C. L., Schenkman, M. L., McFann, K., Wolfe, P. & Kohrt, W. M. Walking economy in people with Parkinson's disease. Mov. Disord. 24, 1481–1487 (2009).
Canning, C. G., Ada, L., Johnson, J. J. & McWhirter, S. Walking capacity in mild to moderate Parkinson's disease. Arch. Phys. Med. Rehabil. 87, 371–375 (2006).
Lord, S. et al. Ambulatory activity in incident Parkinson's: more than meets the eye? J. Neurol. 260, 2964–2972 (2013).
Rogers, M. W. Disorders of posture, balance, and gait in Parkinson's disease. Clin. Geriatr. Med. 12, 825 (1996).
Morris, M. E., Iansek, R., Matyas, T. A. & Summers, J. J. The pathogenesis of gait hypokinesia in Parkinson's disease. Brain 117, 1169–1181 (1994).
Van Emmerik, R. E., Wagenaar, R. C., Winogrodzka, A. & Wolters, E. C. Identification of axial rigidity during locomotion in Parkinson disease. Arch. Phys. Med. Rehabil. 80, 186–191 (1999).
Hausdorff, J. M., Cudkowicz, M. E., Firtion, R., Wei, J. Y. & Goldberger, A. L. Gait variability and basal ganglia disorders: stride-to-stride variations of gait cycle timing in Parkinson's disease and Huntington's disease. Mov. Disord. 13, 428–437 (1998).
Willems, A. M. et al. Turning in Parkinson's disease patients and controls: the effect of auditory cues. Mov. Disord. 22, 1871–1878 (2007).
Dennison, A. C. et al. Falling in Parkinson disease: identifying and prioritizing risk factors in recurrent fallers. Am. J. Phys. Med. Rehabil. 86, 621–632 (2007).
Ashburn, A., Stack, E., Ballinger, C., Fazakarley, L. & Fitton, C. The circumstances of falls among people with Parkinson's disease and the use of Falls Diaries to facilitate reporting. Disabil. Rehabil. 30, 1205–1212 (2008).
Rochester, L. et al. Attending to the task: interference effects of functional tasks on walking in Parkinson's disease and the roles of cognition, depression, fatigue, and balance. Arch. Phys. Med. Rehabil. 85, 1578–1585 (2004).
Yogev-Seligmann, G., Hausdorff, J. M. & Giladi, N. Do we always prioritize balance when walking? Towards an integrated model of task prioritization. Mov. Disord. 27, 765–770 (2012).
Giladi, N., Horak, F. B. & Hausdorff, J. M. Classification of gait disturbances: distinguishing between continuous and episodic changes. Mov. Disord. 28, 1469–1473 (2013).
Nutt, J. G. et al. Freezing of gait: moving forward on a mysterious clinical phenomenon. Lancet Neurol. 10, 734–744 (2011).
Leddy, A. L., Crowner, B. E. & Earhart, G. M. Utility of the mini-BESTest, BESTest, and BESTest sections for balance assessments in individuals with Parkinson disease. J. Neurol. Phys. Ther. 35, 90–97 (2011).
Mancini, M. et al. Postural sway as a marker of progression in Parkinson's disease: a pilot longitudinal study. Gait Posture 36, 471–476 (2012).
Beuter, A., Hernández, R., Rigal, R., Modolo, J. & Blanchet, P. J. Postural sway and effect of levodopa in early Parkinson's disease. Can. J. Neurol. Sci. 35, 65–68 (2008).
Švehlík, M. et al. Gait analysis in patients with Parkinson's disease off dopaminergic therapy. Arch. Phys. Med. Rehabil. 90, 1880–1886 (2009).
Zampieri, C., Salarian, A., Carlson-Kuhta, P., Nutt, J. G. & Horak, F. B. Assessing mobility at home in people with early Parkinson's disease using an instrumented Timed Up and Go test. Parkinsonism Relat. Disord. 17, 277–280 (2011).
Mancini, M., Rocchi, L., Horak, F. B. & Chiari, L. Effects of Parkinson's disease and levodopa on functional limits of stability. Clin. Biomech. (Bristol, Avon) 23, 450–458 (2008).
Vaugoyeau, M., Viallet, F., Mesure, S. & Massion, J. Coordination of axial rotation and step execution: deficits in Parkinson's disease. Gait Posture 18, 150–157 (2003).
Boonstra, T. A., van Kordelaar, J., Engelhart, D., van Vugt, J. P. & van der Kooij, H. Asymmetries in reactive and anticipatory balance control are of similar magnitude in Parkinson's disease patients. Gait Posture 43, 108–113 (2015).
Stack, E. L., Ashburn, A. & Jupp, K. Postural instability during reaching tasks in Parkinson's disease. Physiother. Res. Int. 10, 146–153 (2005).
Roemmich, R. T. et al. Spatiotemporal variability during gait initiation in Parkinson's disease. Gait Posture 36, 340–343 (2012).
Rogers, M. W. et al. Postural preparation prior to stepping in patients with Parkinson's disease. J. Neurophysiol. 106, 915–924 (2011).
King, L. A. & Horak, F. B. Lateral stepping for postural correction in Parkinson's disease. Arch. Phys. Med. Rehabil. 89, 492–499 (2008).
Peterson, D. S. & Horak, F. B. The effect of levodopa on improvements in protective stepping in people with Parkinson's disease. Neurorehabil. Neural Repair 30, 931–940 (2016).
Pickering, R. M. et al. A meta-analysis of six prospective studies of falling in Parkinson's disease. Mov. Disord. 22, 1892–1900 (2007).
Bloem, B. R., Grimbergen, Y. A., Cramer, M., Willemsen, M. & Zwinderman, A. H. Prospective assessment of falls in Parkinson's disease. J. Neurol. 248, 950–958 (2001).
Ashburn, A., Stack, E., Pickering, R. M. & Ward, C. D. Predicting fallers in a community-based sample of people with Parkinson's disease. Gerontology 47, 277–281 (2001).
Gray, P. & Hildebrand, K. Fall risk factors in Parkinson's disease. J. Neurosci. Nurs. 32, 222–228 (2000).
Kerr, G. K. et al. Predictors of future falls in Parkinson disease. Neurology 75, 116–124 (2010).
Wood, B. H., Bilclough, J. A., Bowron, A. & Walker, R. W. Incidence and prediction of falls in Parkinson's disease: a prospective multidisciplinary study. J. Neurol. Neurosurg. Psychiatry 72, 721–725 (2002).
Lord, S. et al. Predicting first fall in newly diagnosed Parkinson's disease: insights from a fall-naïve cohort. Mov. Disord. 31, 1829–1836 (2016).
Mak, M. K. & Pang, M. Y. Fear of falling is independently associated with recurrent falls in patients with Parkinson's disease: a 1-year prospective study. J. Neurol. 256, 1689–1695 (2009).
Matinolli, M., Korpelainen, J. T., Sotaniemi, K. A., Myllylä, V. V. & Korpelainen, R. Recurrent falls and mortality in Parkinson's disease: a prospective two-year follow-up study. Acta Neurol. Scand. 123, 193–200 (2011).
Paul, S. S. et al. Three simple clinical tests to accurately predict falls in people with Parkinson's disease. Mov. Disord. 28, 655–662 (2013).
Paul, S. S., Canning, C. G., Song, J., Fung, V. S. & Sherrington, C. Leg muscle power is enhanced by training in people with Parkinson's disease: a randomized controlled trial. Clin. Rehabil. 28, 275–288 (2014).
Plotnik, M., Giladi, N., Dagan, Y. & Hausdorff, J. M. Postural instability and fall risk in Parkinson's disease: impaired dual tasking, pacing, and bilateral coordination of gait during the “ON” medication state. Exp. Brain Res. 210, 529–538 (2011).
Hely, M. A., Reid, W. G., Adena, M. A., Halliday, G. M. & Morris, J. G. The Sydney multicenter study of Parkinson's disease: the inevitability of dementia at 20 years. Mov. Disord. 23, 837–844 (2008).
Idjadi, J. A. et al. Hip fracture outcomes in patients with Parkinson's disease. Am. J. Orthop. (Belle Mead NJ) 34, 341–346 (2005).
Bloem, B. R., Hausdorff, J. M., Visser, J. E. & Giladi, N. Falls and freezing of gait in Parkinson's disease: a review of two interconnected, episodic phenomena. Mov. Disord. 19, 871–884 (2004).
Melton, L. J. et al. Fracture risk after the diagnosis of Parkinson's disease: influence of concomitant dementia. Mov. Disord. 21, 1361–1367 (2006).
Keus, S. H., Munneke, M., Nijkrake, M. J., Kwakkel, G. & Bloem, B. R. Physical therapy in Parkinson's disease: evolution and future challenges. Mov. Disord. 24, 1–14 (2009).
Keus, S. et al. European Physiotherapy Guideline for Parkinson's Disease. (KNGF/ParkinsonNet, 2014).
Tomlinson, C. L. et al. Physiotherapy for Parkinson's disease: a comparison of techniques. Cochrane Database Syst. Rev. 6, CD002815 (2014).
Ellis, T. et al. Efficacy of a physical therapy program in patients with Parkinson's disease: a randomized controlled trial. Arch. Phys. Med. Rehabil. 86, 626–632 (2005).
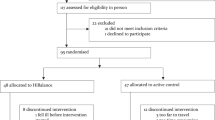
Schenkman, M. et al. Exercise for people in early- or mid-stage Parkinson disease: a 16-month randomized controlled trial. Phys. Ther. 92, 1395 (2012).
Frazzitta, G. et al. Intensive rehabilitation treatment in early Parkinson's disease: a randomized pilot study with a 2-year follow-up. Neurorehabil. Neural Repair. 29, 123–131 (2015).
Chung, C. L., Thilarajah, S. & Tan, D. Effectiveness of resistance training on muscle strength and physical function in people with Parkinson's disease: a systematic review and meta-analysis. Clin. Rehabil. 30, 11–23 (2016).
Lima, L. O., Scianni, A. & Rodrigues-de-Paula, F. Progressive resistance exercise improves strength and physical performance in people with mild to moderate Parkinson's disease: a systematic review. J. Physiother. 59, 7–13 (2013).
Lamotte, G. et al. Effects of endurance exercise training on the motor and non-motor features of Parkinson's disease: a review. J. Parkinsons Dis. 5, 21–41 (2015).
Shen, X. & Mak, M. K. Technology-assisted balance and gait training reduces falls in patients with Parkinson's disease: a randomized controlled trial with 12-month follow-up. Neurorehabil. Neural Repair. 29, 103–111 (2015).
Carvalho, A. et al. Comparison of strength training, aerobic training, and additional physical therapy as supplementary treatments for Parkinson's disease: pilot study. Clin. Interv. Aging 10, 183 (2015).
Corcos, D. et al. A two-year randomized controlled trial of progressive resistance exercise for Parkinson's disease. Mov. Disord. 28, 1230–1240 (2013).
Shulman, L. M. et al. Randomized clinical trial of 3 types of physical exercise for patients with Parkinson disease. JAMA Neurol. 70, 183–191 (2013).
Silva-Batista, C. et al. Resistance training with instability for patients with Parkinson's disease. Med. Sci. Sports Exerc. 48, 1678–1687 (2016).
Ni, M., Signorile, J. F., Balachandran, A. & Potiaumpai, M. Power training induced change in bradykinesia and muscle power in Parkinson's disease. Parkinsonism Relat. Disord. 23, 37–44 (2016).
Ni, M. et al. Comparative effect of power training and high-speed yoga on motor function in older patients with Parkinson disease. Arch. Phys. Med. Rehabil. 97, 345–354.e15 (2016).
Dibble, L. E., Hale, T. F., Marcus, R. L., Gerber, J. P. & LaStayo, P. C. High intensity eccentric resistance training decreases bradykinesia and improves quality of life in persons with Parkinson's disease: a preliminary study. Parkinsonism Relat. Disord. 15, 752–757 (2009).
Dibble, L. E., Foreman, K. B., Addison, O., Marcus, R. L. & LaStayo, P. C. Exercise and medication effects on persons with Parkinson disease across the domains of disability: a randomized clinical trial. J. Neurol. Phys. Ther. 39, 85 (2015).
Morris, M. E. et al. A randomized controlled trial to reduce falls in people with Parkinson's disease. Neurorehabil. Neural Repair. 29, 777–785 (2015).
Schlenstedt, C. et al. Resistance versus balance training to improve postural control in Parkinson's disease: a randomized rater blinded controlled study. PLoS ONE 10, e0140584 (2015).
Li, F. et al. Tai chi and postural stability in patients with Parkinson's disease. N. Engl. J. Med. 366, 511–519 (2012).
Prodoehl, J. et al. Two-year exercise program improves physical function in Parkinson's disease the PRET-PD randomized clinical trial. Neurorehabil. Neural Repair. 29, 112–122 (2015).
Shen, X. & Mak, M. K. Balance and gait training with augmented feedback improves balance confidence in people with Parkinson's disease: a randomized controlled trial. Neurorehabil. Neural Repair. 28, 524–535 (2014).
Sage, M. D. & Almeida, Q. J. Symptom and gait changes after sensory attention focused exercise versus aerobic training in Parkinson's disease. Mov. Disord. 24, 1132–1138 (2009).
Nadeau, A., Pourcher, E. & Corbeil, P. Effects of 24 weeks of treadmill training on gait performance in Parkinson disease. Med. Sci. Sports Exerc. 46, 645–655 (2013).
Cugusi, L. et al. Effects of a Nordic walking program on motor and non-motor symptoms, functional performance and body composition in patients with Parkinson's disease. NeuroRehabilitation 37, 245–254 (2015).
Reuter, I. et al. Effects of a flexibility and relaxation programme, walking, and Nordic walking on Parkinson's disease. J. Aging Res. 2011, 232473 (2011).
Bridgewater, K. J. & Sharpe, M. H. Aerobic exercise and early Parkinson's disease. J. Neurol. Rehabil. 10, 233–241 (1996).
Morris, M. E., Iansek, R., Matyas, T. A. & Summers, J. J. Stride length regulation in Parkinson's disease. Brain 119, 551–568 (1996).
Spaulding, S. J. et al. Cueing and gait improvement among people with Parkinson's disease: a meta-analysis. Arch. Phys. Med. Rehabil. 94, 562–570 (2013).
Morris, M. E., Iansek, R. & Kirkwood, B. A randomized controlled trial of movement strategies compared with exercise for people with Parkinson's disease. Mov. Disord. 24, 64–71 (2009).
Martin, T., Weatherall, M., Anderson, T. J. & MacAskill, M. R. randomized controlled feasibility trial of a specific cueing program for falls management in persons with Parkinson disease and freezing of gait. J. Neurol. Phys. Ther. 39, 179–184 (2015).
de Bruin, N. et al. Walking with music is a safe and viable tool for gait training in Parkinson's disease: the effect of a 13-week feasibility study on single and dual task walking. Parkinsons Dis. 2010, 483530 (2010).
Frazzitta, G., Maestri, R., Uccellini, D., Bertotti, G. & Abelli, P. Rehabilitation treatment of gait in patients with Parkinson's disease with freezing: a comparison between two physical therapy protocols using visual and auditory cues with or without treadmill training. Mov. Disord. 24, 1139–1143 (2009).
Miyai, I. et al. Long-term effect of body weight–supported treadmill training in Parkinson's disease: a randomized controlled trial. Arch. Phys. Med. Rehabil. 83, 1370–1373 (2002).
Picelli, A. et al. Robot-assisted gait training versus equal intensity treadmill training in patients with mild to moderate Parkinson's disease: a randomized controlled trial. Parkinsonism Relat. Disord. 19, 605–610 (2013).
Carda, S. et al. Robotic gait training is not superior to conventional treadmill training in Parkinson disease: a single-blind randomized controlled trial. Neurorehabil. Neural Repair. 26, 1027–1034 (2012).
Mehrholz, J. et al. Treadmill training for patients with Parkinson's disease. Cochrane Database Syst. Rev. 1, CD007830 (2010).
Goodwin, V. A., Richards, S. H., Taylor, R. S., Taylor, A. H. & Campbell, J. L. The effectiveness of exercise interventions for people with Parkinson's disease: a systematic review and meta-analysis. Mov. Disord. 23, 631–640 (2008).
Ashburn, A. et al. A randomised controlled trial of a home based exercise programme to reduce the risk of falling among people with Parkinson's disease. J. Neurol. Neurosurg. Psychiatry 78, 678–684 (2007).
Canning, C. G. et al. Exercise for falls prevention in Parkinson disease: a randomized controlled trial. Neurology 84, 304–312 (2015).
Sparrow, D. et al. Highly challenging balance program reduces fall rate in Parkinson disease. J. Neurol. Phys. Ther. 40, 24–30 (2016).
Wong-Yu, I. S. & Mak, M. K. Multi-dimensional balance training programme improves balance and gait performance in people with Parkinson's disease: a pragmatic randomised controlled trial with 12-month follow-up. Parkinsonism Relat. Disord. 21, 615–621 (2015).
Palamara, G. et al. Land plus aquatic therapy versus land-based rehabilitation alone for the treatment of balance dysfunction in Parkinson disease: a randomized controlled study with 6-month follow-up. Arch. Phys. Med. Rehabil. 98, 1077–1085 (2017).
Ni, X., Liu, S., Lu, F., Shi, X. & Guo, X. Efficacy and safety of Tai Chi for Parkinson's disease: a systematic review and meta-analysis of randomized controlled trials. PLoS ONE 9, e99377 (2014).
Amano, S. et al. The effect of tai chi exercise on gait initiation and gait performance in persons with Parkinson's disease. Parkinsonism Relat. Disord. 19, 955–960 (2013).
Gao, Q. et al. Effects of tai chi on balance and fall prevention in Parkinson's disease: a randomized controlled trial. Clin. Rehabil. 28, 748–753 (2014).
Hackney, M. E. & Earhart, G. M. Tai chi improves balance and mobility in people with Parkinson disease. Gait Posture 28, 456–460 (2008).
Li, F. et al. A randomized controlled trial of patient-reported outcomes with tai chi exercise in Parkinson's disease. Mov. Disord. 29, 539–545 (2014).
Choi, H. J. et al. Therapeutic effects of tai chi in patients with Parkinson's disease. ISRN Neurol. 2013, 548240 (2013).
Duncan, R. P. & Earhart, G. M. Randomized controlled trial of community-based dancing to modify disease progression in Parkinson disease. Neurorehabil. Neural Repair. 26, 132–143 (2012).
Hackney, M. E. & Earhart, G. M. Effects of dance on movement control in Parkinson's disease: a comparison of Argentine tango and American ballroom. J. Rehabil. Med. 41, 475–481 (2009).
Hackney, M. E. & Earhart, G. M. Health-related quality of life and alternative forms of exercise in Parkinson disease. Parkinsonism Relat. Disord. 15, 644–648 (2009).
Hackney, M. E., Kantorovich, S., Levin, R. & Earhart, G. M. Effects of tango on functional mobility in Parkinson's disease: a preliminary study. J. Neurol. Phys. Ther. 31, 173 (2007).
Romenets, S. R., Anang, J., Fereshtehnejad, S.-M., Pelletier, A. & Postuma, R. Tango for treatment of motor and non-motor manifestations in Parkinson's disease: a randomized control study. Complement. Ther. Med. 23, 175–184 (2015).
Volpe, D., Signorini, M., Marchetto, A., Lynch, T. & Morris, M. E. A comparison of Irish set dancing and exercises for people with Parkinson's disease: a phase II feasibility study. BMC Geriatr. 13, 1 (2013).
Mujika, I. & Padilla, S. Detraining: loss of training-induced physiological & performance adaptations. Part I: short term insufficient training stimulus. Sports Med. 30, 79–87 (2000).
Garber, C. E. et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med. Sci. Sports Exerc. 43, 1334–1359 (2011).
Steffen, T. & Seney, M. Test-retest reliability and minimal detectable change on balance and ambulation tests, the 36-item short-form health survey, and the unified Parkinson disease rating scale in people with Parkinsonism. Phys. Ther. 88, 733 (2008).
Muslimovic, D., Post, B., Speelman, J. D. & Schmand, B. Motor procedural learning in Parkinson's disease. Brain 130, 2887–2897 (2007).
Shulman, L. M. et al. The clinically important difference on the unified Parkinson's disease rating scale. Arch. Neurol. 67, 64–70 (2010).
Fisher, B. E. et al. Treadmill exercise elevates striatal dopamine D2 receptor binding potential in patients with early Parkinson's disease. Neuroreport 24, 509–514 (2013).
Svensson, M., Lexell, J. & Deierborg, T. Effects of physical exercise on neuroinflammation, neuroplasticity, neurodegeneration, and behavior: what we can learn from animal models in clinical settings. Neurorehabil. Neural Repair. 29, 577–589 (2015).
Koo, J. H., Cho, J. Y. & Lee, U. B. Treadmill exercise alleviates motor deficits and improves mitochondrial import machinery in an MPTP-induced mouse model of Parkinson's disease. Exp. Gerontol. 89, 20–29 (2017).
Monteiro-Junior, R. S. et al. We need to move more: neurobiological hypotheses of physical exercise as a treatment for Parkinson's disease. Med. Hypotheses 85, 537–541 (2015).
Zigmond, M. J. & Smeyne, R. J. Exercise: is it a neuroprotective and if so, how does it work? Parkinsonism Relat. Disord. 20, S123–S127 (2014).
Petzinger, G. et al. The effects of exercise on dopamine neurotransmission in Parkinson's disease: targeting neuroplasticity to modulate basal ganglia circuitry. Brain Plast. 1, 29–39 (2015).
Fisher, B. E. et al. The effect of exercise training in improving motor performance and corticomotor excitability in people with early Parkinson's disease. Arch. Phys. Med. Rehabil. 89, 1221–1229 (2008).
Frazzitta, G. et al. Intensive rehabilitation increases BDNF serum levels in Parkinsonian patients: a randomized study. Neurorehabil. Neural Repair. 28, 163–168 (2014).
Fontanesi, C. et al. Intensive rehabilitation enhances lymphocyte BDNF–TrkB signaling in patients with Parkinson's disease. Neurorehabil. Neural Repair. 30, 411–418 (2016).
Sehm, B. et al. Structural brain plasticity in Parkinson's disease induced by balance training. Neurobiol. Aging 35, 232–239 (2014).
Duchesne, C. et al. Influence of aerobic exercise training on the neural correlates of motor learning in Parkinson's disease individuals. Neuroimage Clin. 12, 559–569 (2016).
Abbruzzese, G., Marchese, R., Avanzino, L. & Pelosin, E. Rehabilitation for Parkinson's disease: current outlook and future challenges. Parkinsonism Relat. Disord. 22, S60–S64 (2016).
Speelman, A. D., van Nimwegen, M., Bloem, B. R. & Munneke, M. Evaluation of implementation of the ParkFit program: a multifaceted intervention aimed to promote physical activity in patients with Parkinson's disease. Physiotherapy 100, 134–141 (2014).
Ellis, T. et al. Barriers to exercise in people with Parkinson disease. Phys. Ther. 93, 628 (2013).
Cress, M. E. et al. Best practices for physical activity programs and behavior counseling in older adult populations. J. Aging. Phys. Act. 13, 61–74 (2005).
Rosser, B. A., Vowles, K. E., Keogh, E., Eccleston, C. & Mountain, G. A. Technologically-assisted behaviour change: a systematic review of studies of novel technologies for the management of chronic illness. J. Telemed. Telecare 15, 327–338 (2009).
Barry, G., Galna, B. & Rochester, L. The role of exergaming in Parkinson's disease rehabilitation: a systematic review of the evidence. J. Neuroeng. Rehabil. 11, 33 (2014).
Moore, C. G. et al. Study in Parkinson disease of exercise (SPARX): translating high-intensity exercise from animals to humans. Contemp. Clin. Trials 36, 90–98 (2013).
Earhart, G. M., Duncan, R. P., Huang, J. L., Perlmutter, J. S. & Pickett, K. A. Comparing interventions and exploring neural mechanisms of exercise in Parkinson disease: a study protocol for a randomized controlled trial. BMC Neurol. 15, 9 (2015).
Angelucci, F. et al. The effects of motor rehabilitation training on clinical symptoms and serum BDNF levels in Parkinson's disease subjects. Can. J. Physiol. Pharmacol. 94, 455–461 (2016).
Ferraye, M. U., Fraix, V., Pollak, P., Bloem, B. R. & DebÛ, B. The laser-shoe: a new form of continuous ambulatory cueing for patients with Parkinson's disease. Parkinsonism Relat. Disord. 29, 127 (2016).
Zhao, Y. et al. Feasibility of external rhythmic cueing with the Google Glass for improving gait in people with Parkinson's disease. J. Neurol. 263, 1156–1165 (2016).
Horak, F. B., King, L. & Mancini, M. Role of body-worn movement monitor technology for balance and gait rehabilitation. Phys. Ther. 95, 461–470 (2015).
Ekker, M. S., Janssen, S., Nonnekes, J., Bloem, B. R. & de Vries, N. M. Neurorehabilitation for Parkinson's disease: future perspectives for behavioural adaptation. Parkinsonism Relat. Disord. 22, S73–S77 (2016).
Hely, M. A., Morris, J. G., Reid, W. G. & Trafficante, R. Sydney multicenter study of Parkinson's disease: non L-dopa responsive problems dominate at 15 years. Mov. Disord. 20, 190–199 (2005).
Seppi, K. et al. The Movement Disorder Society Evidence-Based Medicine review update: treatments for the non-motor symptoms of Parkinson's disease. Mov. Disord. 26, S42–S80 (2011).
Cusso, M. E., Donald, K. J. & Khoo, T. K. The impact of physical activity on non-motor symptoms in Parkinson's disease: a systematic review. Front. Med. (Lausanne) 3, 35 (2016).
Duchesne, C. et al. Enhancing both motor and cognitive functioning in Parkinson's disease: aerobic exercise as a rehabilitative intervention. Brain Cogn. 99, 68–77 (2015).
Reynolds, G. O., Otto, M. W., Ellis, T. D. & Cronin-Golomb, A. The therapeutic potential of exercise to improve mood, cognition, and sleep in Parkinson's disease. Mov. Disord. 31, 23–38 (2016).
Van der Kolk, N. M. et al. Design of the Park-in-Shape study: a phase II double blind randomized controlled trial evaluating the effects of exercise on motor and non-motor symptoms in Parkinson's disease. BMC Neurol. 15, 56 (2015).
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the researching, discussion writing and review of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary information S1 (table)
Study characteristics (DOC 151 kb)
Glossary
- Walking economy
-
The steady-state aerobic demand for a given sub-maximal speed of walking, as measured by VO2 uptake.
- Walking capacity
-
The distance a person is capable of walking over a period of time, typically measured by 6-min walk distance.
- Hoehn and Yahr rating scale
-
A commonly used scale (from stages 1 to 5) for describing how the symptoms of Parkinson disease progress.
- Double-support phase
-
A phase in the gait cycle when the body weight is supported by both legs.
- Set-shifting
-
The ability to move back and forth between tasks in response to changing goals or environmental experiences.
- Limit of stability
-
A measurement of the maximum centre of pressure displacement with respect to a person's base of support.
- Anticipatory postural adjustments
-
The automatic feedforward postural activities to counteract the destabilizing effects of voluntary movements.
- Reactive postural responses
-
The automatic postural responses against external perturbation with or without a change in a person's base of support.
- Supervised programme
-
Any training that was supervised by either a physical therapist or exercise trainer in a one-to-one or small-group basis.
- Progressive resistance training
-
A style of strength training exercise that involves the steady utilization of resistance via a loading source.
- Aerobic endurance training
-
An exercise training method to improve cardiopulmonary fitness.
- Nordic walking
-
A total body version of walking activity using specially designed walking poles (similar to ski poles).
- Minimal detectable change
-
A statistical estimate of the smallest amount of change that can be detected by a measure that corresponds to a noticeable change in ability.
- Exergaming
-
A term used for video games that are also a form of exercise.
Rights and permissions
About this article
Cite this article
Mak, M., Wong-Yu, I., Shen, X. et al. Long-term effects of exercise and physical therapy in people with Parkinson disease. Nat Rev Neurol 13, 689–703 (2017). https://doi.org/10.1038/nrneurol.2017.128
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2017.128
This article is cited by
-
The PD-Ballet study: study protocol for a randomised controlled single-blind hybrid type 2 clinical trial evaluating the effects of ballet dancing on motor and non-motor symptoms in Parkinson’s disease
BMC Complementary Medicine and Therapies (2024)
-
Effects of virtual reality versus motor imagery versus routine physical therapy in patients with parkinson’s disease: a randomized controlled trial
BMC Geriatrics (2024)
-
Association of health behaviors with function and health-related quality of life among patients with Parkinson’s disease
Israel Journal of Health Policy Research (2024)
-
Effect of Conditioned Medium from Human Adipose-Derived Mesenchymal Stem Cells on Human Sperm Quality During Cryopreservation
Reproductive Sciences (2024)
-
Impacts of gait freeze on quality of life in Parkinson’s disease, from the perspectives of patients and their carers
Irish Journal of Medical Science (1971 -) (2024)