Key Points
-
Neuropsychiatric sequelae of stroke are often disabling, have a negative effect on stroke recovery, and decrease quality of life
-
Neuropsychiatric disorders after stroke are relatively common: one-third of stroke survivors experience depression, anxiety or apathy; recovery from these disorders is only moderate, and the risk of recurrence is high
-
Some of these disorders are treatable; for example, antidepressants reduce the number and severity of depressive symptoms and episodes and decrease anxiety scores in patients with stroke
-
Research into the pathophysiology of stroke-associated neuropsychiatric disturbances would greatly benefit from improved study design, including incorporation of control groups in functional imaging studies and specification of working hypotheses
-
Pilot studies on the effects of behavioural interventions and large-scale randomized trials of drugs that are safe to use in patients with stroke would improve the management of neuropsychiatric sequelae of stroke
Abstract
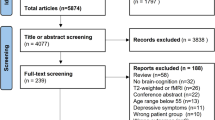
Stroke survivors are often affected by psychological distress and neuropsychiatric disturbances. About one-third of stroke survivors experience depression, anxiety or apathy, which are the most common neuropsychiatric sequelae of stroke. Neuropsychiatric sequelae are disabling, and can have a negative influence on recovery, reduce quality of life and lead to exhaustion of the caregiver. Despite the availability of screening instruments and effective treatments, neuropsychiatric disturbances attributed to stroke are currently underdiagnosed and undertreated. Stroke severity, stroke-related disabilities, cerebral small vessel disease, previous psychiatric disease, poor coping strategies and unfavourable psychosocial environment influence the presence and severity of the psychiatric sequelae of stroke. Although consistent associations between psychiatric disturbances and specific stroke locations have yet to be confirmed, functional MRI studies are beginning to unveil the anatomical networks that are disrupted in stroke-associated psychiatric disorders. Evidence regarding biochemical and genetic biomarkers for stroke-associated psychiatric disorders is still limited, and better understanding of the biological determinants and pathophysiology of these disorders is needed. Investigation into the management of these conditions must be continued, and should include pilot studies to assess the benefits of innovative behavioural interventions and large-scale cooperative randomized controlled pharmacological trials of drugs that are safe to use in patients with stroke.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Feigin, V. L. et al. Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 383, 245–254 (2014).
Bejot, Y., Daubail, B. & Giroud, M. Epidemiology of stroke and transient ischemic attacks: current knowledge and perspectives. Rev. Neurol. (Paris) 172, 59–68 (2016).
Hackett, M. L., Kohler, S., O'Brien, J. T. & Mead, G. E. Neuropsychiatric outcomes of stroke. Lancet Neurol. 13, 525–534 (2014).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
Piechowski-Jozwiak, B. & Bogousslavsky, J. Neurobehavioral syndromes. Front. Neurol. Neurosci. 30, 57–60 (2012).
Ferro, J. Neuropsychiatric Symptoms of Cerebrovascular Diseases (Springer, 2013).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders-TR 4th edn (American Psychiatric Association, 2002).
Caeiro, L., Ferro, J., Santos, C. & Figueira, M. Depression in acute stroke. J. Psychiatry Neurosci. 31, 377–383 (2006).
Spalletta, G., Ripa, A. & Caltagirone, C. Symptom profile of DSM-IV major and minor depressive disorders in first-ever stroke patients. Am. J. Geriatr. Psychiatry 13, 108–115 (2005).
Robinson, R. G. & Jorge, R. E. Post-stroke depression: a review. Am. J. Psychiatry 173, 221–231 (2016).
Sheehan, D. V. et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 59 (Suppl. 20), 22–33 (1998).
Robinson, R. G. & Spalletta, G. Poststroke depression: a review. Can. J. Psychiatry 55, 341–349 (2010).
Montgomery, S. A. & Asberg, M. A new depression scale designed to be sensitive to change. Br. J. Psychiatry 134, 382–389 (1979).
Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–62 (1960).
Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67, 361–370 (1983).
Beck, A. T., Ward, C. H., Mendelson, M., Mock, J. & Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 4, 561–571 (1961).
Turner, A. et al. Depression screening in stroke: a comparison of alternative measures with the structured diagnostic interview for the diagnostic and statistical manual of mental disorders, fourth edition (major depressive episode) as criterion standard. Stroke 43, 1000–1005 (2012).
Starkstein, S. E. & Robinson, R. G. Affective disorders and cerebral vascular disease. Br. J. Psychiatry 154, 170–182 (1989).
Santos, C., Caeiro, L., Ferro, J. & Figueira, M. Mania and stroke: a systematic review. Cerebrovasc. Dis. 32, 11–21 (2011).
Hackett, M. L. & Pickles, K. Part I: frequency of depression after stroke: an updated systematic review and meta-analysis of observational studies. Int. J. Stroke 9, 1017–1025 (2014).
Ayerbe, L., Ayis, S., Wolfe, C. D. & Rudd, A. G. Natural history, predictors and outcomes of depression after stroke: systematic review and meta-analysis. Br. J. Psychiatry 202, 14–21 (2013).
Ayerbe, L., Ayis, S., Crichton, S., Wolfe, C. D. & Rudd, A. G. The natural history of depression up to 15 years after stroke: the South London Stroke Register. Stroke 44, 1105–1110 (2013).
Wu, K. Y., Liu, C. Y., Chau, Y. L. & Chang, C. M. Transient ischemic attack and incidence of depression in old age: evidence from a population-based analysis in Taiwan. Am. J. Geriatr. Psychiatry 18, 382–387 (2010).
Luijendijk, H. J. et al. Transient ischemic attack and incident depression. Stroke 42, 1857–1861 (2011).
El Husseini, N. et al. Depression and antidepressant use after stroke and transient ischemic attack. Stroke 43, 1609–1616 (2012).
Broomfield, N. M., Quinn, T. J., Abdul-Rahim, A. H., Walters, M. R. & Evans, J. J. Depression and anxiety symptoms post-stroke/TIA: prevalence and associations in cross-sectional data from a regional stroke registry. BMC Neurol. 14, 198 (2014).
Schramke, C. J., Stowe, R. M., Ratcliff, G., Goldstein, G. & Condray, R. Poststroke depression and anxiety: different assessment methods result in variations in incidence and severity estimates. J. Clin. Exp. Neuropsychol. 20, 723–737 (1998).
Berg, A., Lonnqvist, J., Palomaki, H. & Kaste, M. Assessment of depression after stroke: a comparison of different screening instruments. Stroke 40, 523–529 (2009).
Kutlubaev, M. A. & Hackett, M. L. Part II: predictors of depression after stroke and impact of depression on stroke outcome: an updated systematic review of observational studies. Int. J. Stroke 9, 1026–1036 (2014).
Starkstein, S. E., Robinson, R. G. & Price, T. R. Comparison of cortical and subcortical lesions in the production of poststroke mood disorders. Brain 110, 1045–1059 (1987).
Carson, A. J. et al. Depression after stroke and lesion location: a systematic review. Lancet 356, 122–126 (2000).
Wei, N. et al. Post-stroke depression and lesion location: a systematic review. J. Neurol. 262, 81–90 (2015).
Zhang, T. et al. A prospective cohort study of lesion location and its relation to post-stroke depression among Chinese patients. J. Affect. Disord. 136, e83–87 (2012).
Wu, R. H., Li, Q., Tan, Y., Liu, X. Y. & Huang, J. Depression in silent lacunar infarction: a cross-sectional study of its association with location of silent lacunar infarction and vascular risk factors. Neurol. Sci. 35, 1553–1559 (2014).
Yasuno, F. et al. Microstructural abnormality in white matter, regulatory T lymphocytes, and depressive symptoms after stroke. Psychogeriatrics 14, 213–221 (2014).
Pavlovic, A. M. et al. Baseline characteristic of patients presenting with lacunar stroke and cerebral small vessel disease may predict future development of depression. Int. J. Geriatr. Psychiatry 31, 58–65 (2016).
Tang, W. K. et al. Cerebral microbleeds and depression in lacunar stroke. Stroke 42, 2443–2446 (2011).
Tang, W. K. et al. Cerebral microbleeds and symptom severity of post-stroke depression: a magnetic resonance imaging study. J. Affect. Disord. 129, 354–358 (2011).
Tang, W. K. et al. Cerebral microbleeds as a predictor of 1-year outcome of poststroke depression. Stroke 45, 77–81 (2014).
Tang, W. K. et al. Pontine microbleeds and depression in stroke. J. Geriatr. Psychiatry Neurol. 27, 159–164 (2014).
van Mierlo, M. L., van Heugten, C. M., Post, M. W., de Kort, P. L. & Visser-Meily, J. M. Psychological factors determine depressive symptomatology after stroke. Arch. Phys. Med. Rehabil. 96, 1064–1070 (2015).
Visser, M. M. et al. Coping, problem solving, depression, and health-related quality of life in patients receiving outpatient stroke rehabilitation. Arch. Phys. Med. Rehabil. 96, 1492–1498 (2015).
Ouimet, M. A., Primeau, F. & Cole, M. G. Psychosocial risk factors in poststroke depression: a systematic review. Can. J. Psychiatry 46, 819–828 (2001).
Hinojosa, R., Haun, J., Hinojosa, M. S. & Rittman, M. Social isolation poststroke: relationship between race/ethnicity, depression, and functional independence. Top. Stroke Rehabil. 18, 79–86 (2011).
Ayerbe, L., Ayis, S., Crichton, S. L., Rudd, A. G. & Wolfe, C. D. Explanatory factors for the increased mortality of stroke patients with depression. Neurology 83, 2007–2012 (2014).
Glodzik-Sobanska, L. et al. Single voxel proton magnetic resonance spectroscopy in post-stroke depression. Psychiatry Res. 148, 111–120 (2006).
Wang, X. et al. Glutamate level detection by magnetic resonance spectroscopy in patients with post-stroke depression. Eur. Arch. Psychiatry Clin. Neurosci. 262, 33–38 (2012).
Brookes, R. L., Herbert, V., Lawrence, A. J., Morris, R. G. & Markus, H. S. Depression in small-vessel disease relates to white matter ultrastructural damage, not disability. Neurology 83, 1417–1423 (2014).
Lassalle-Lagadec, S. et al. Linking MRI to daily life experience: the example of poststroke depression. Neurology 78, 322–325 (2012).
Zhang, P. et al. Dysfunction of affective network in post ischemic stroke depression: a resting-state functional magnetic resonance imaging study. Biomed. Res. Int. 2014, 846830 (2014).
Pascoe, M. C. et al. Homocysteine as a potential biochemical marker for depression in elderly stroke survivors. Food Nutr. Res. http://dx.doi.org/10.3402/fnr.v56i0.14973, (2012).
Tang, W. K. et al. Association between high serum total bilirubin and post-stroke depression. Psychiatry Clin. Neurosci. 67, 259–264 (2013).
Zhan, Y. et al. Plasma-based proteomics reveals lipid metabolic and immunoregulatory dysregulation in post-stroke depression. Eur. Psychiatry 29, 307–315 (2014).
Li, Y. T., Zhao, Y., Zhang, H. J. & Zhao, W. L. The association between serum leptin and post stroke depression: results from a cohort study. PLoS ONE 9, e103137 (2014).
Cheng, S. Y. et al. Plasma levels of glutamate during stroke is associated with development of post-stroke depression. Psychoneuroendocrinology 47, 126–135 (2014).
Mak, K. K., Kong, W. Y., Mak, A., Sharma, V. K. & Ho, R. C. Polymorphisms of the serotonin transporter gene and post-stroke depression: a meta-analysis. J. Neurol. Neurosurg. Psychiatry 84, 322–328 (2013).
Kim, J. M. et al. A longitudinal study of SLC6A4 DNA promoter methylation and poststroke depression. J. Psychiatr. Res. 47, 1222–1227 (2013).
Harmandayan, M., Romanowicz, M. & Sola, C. Successful use of ECT in post-stroke depression. Gen. Hosp. Psychiatry 34, 102.e5–102.e6 (2012).
Bueno, V. F., Brunoni, A. R., Boggio, P. S., Bensenor, I. M. & Fregni, F. Mood and cognitive effects of transcranial direct current stimulation in post-stroke depression. Neurocase 17, 318–322 (2011).
Anderson, C. S., Hackett, M. L. & House, A. O. Interventions for preventing depression after stroke. Cochrane Database Syst. Rev. 3, CD003689 (2004).
Hackett, M. L., Anderson, C. S., House, A. & Xia, J. Interventions for treating depression after stroke. Cochrane Database Syst. Rev. 4, CD003437 (2008).
Hackett, M. L. et al. ImProving Outcomes after STroke (POST): results from the randomized clinical pilot trial. Int. J. Stroke 8, 707–710 (2013).
Committee, E. S. O. E. E. & Committee, E. W. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc. Dis. 25, 457–507 (2008).
Mead, G. E. et al. Selective serotonin reuptake inhibitors (SSRIs) for stroke recovery. Cochrane Database Syst. Rev. 11, CD009286 (2012).
Cleare, A. et al. Evidence-based guidelines for treating depressive disorders with antidepressants: a revision of the 2008 British Association for Psychopharmacology guidelines. J. Psychopharmacol. 29, 459–525 (2015).
Sami, M. B. & Faruqui, R. The effectiveness of dopamine agonists for treatment of neuropsychiatric symptoms post brain injury and stroke. Acta Neuropsychiatr. 27, 317–326 (2015).
Almeida, O. P. et al. B-vitamins reduce the long-term risk of depression after stroke: the VITATOPS-DEP trial. Ann. Neurol. 68, 503–510 (2010).
Peng, L., Zhang, X., Kang, D. Y., Liu, X. T. & Hong, Q. Effectiveness and safety of Wuling capsule for post stroke depression: a systematic review. Complement. Ther. Med. 22, 549–566 (2014).
Zhang, G. C. et al. Meta analysis of the curative effect of acupuncture on post-stroke depression. J. Tradit. Chin. Med. 32, 6–11 (2012).
Man, S. C. et al. A pilot controlled trial of a combination of dense cranial electroacupuncture stimulation and body acupuncture for post-stroke depression. BMC Complement. Altern. Med. 14, 255 (2014).
Kim, D. S. et al. Effects of music therapy on mood in stroke patients. Yonsei Med. J. 52, 977–981 (2011).
Herrmann, N. et al. Detection and treatment of post stroke depression: results from the registry of the Canadian stroke network. Int. J. Geriatr. Psychiatry 26, 1195–1200 (2011).
Fuller-Thomson, E., Tulipano, M. J. & Song, M. The association between depression, suicidal ideation, and stroke in a population-based sample. Int. J. Stroke 7, 188–194 (2012).
Yamauchi, T. et al. Death by suicide and other externally caused injuries after stroke in Japan (1990–2010): the Japan Public Health Center-based prospective study. Psychosom. Med. 76, 452–459 (2014).
Santos, C., Caeiro, L., Ferro, J. & Figueira, M. A. Study of suicidal thoughts in acute stroke patients. J. Stroke Cerebrovasc. Dis. 21, 749–754 (2012).
Pompili, M. et al. Do stroke patients have an increased risk of developing suicidal ideation or dying by suicide? An overview of the current literature. CNS Neurosci. Ther. 18, 711–721 (2012).
Tang, W. K. et al. Is insomnia associated with suicidality in stroke? Arch. Phys. Med. Rehabil. 92, 2025–2027 (2011).
Tang, W. K. et al. Cerebral microbleeds and suicidality in stroke. Psychosomatics 53, 439–445 (2012).
Tang, W. K., Liang, H., Mok, V., Ungvari, G. S. & Wong, K. S. Is pain associated with suicidality in stroke? Arch. Phys. Med. Rehabil. 94, 863–866 (2013).
Tang, W. K. et al. Apathy and suicide-related ideation 3 months after stroke: a cross-sectional study. BMC Neurol. 15, 60 (2015).
Nishida, N., Hata, Y., Yoshida, K. & Kinoshita, K. Neuropathologic features of suicide victims who presented with acute poststroke depression: significance of association with neurodegenerative disorders. J. Neuropathol. Exp. Neurol. 74, 401–410 (2015).
Podawiltz, A. A review of current bipolar disorder treatment guidelines. J. Clin. Psychiatry 73, e12 (2012).
Vataja, R. & Kaste, M. in Neuropsychiatric Symptoms of Cerebrovascular Disease Neuropsychiatric Symptoms of Neurological Disease (ed. Ferro, J. M.) 81–108 (Springer, 2013).
Campbell Burton, C. A. et al. Frequency of anxiety after stroke: a systematic review and meta-analysis of observational studies. Int. J. Stroke 8, 545–559 (2013).
Ayerbe, L., Ayis, S. A., Crichton, S., Wolfe, C. D. & Rudd, A. G. Natural history, predictors and associated outcomes of anxiety up to 10 years after stroke: the South London Stroke Register. Age Ageing 43, 542–547 (2014).
Morrison, V., Pollard, B., Johnston, M. & MacWalter, R. Anxiety and depression 3 years following stroke: demographic, clinical, and psychological predictors. J. Psychosom. Res. 59, 209–213 (2005).
Tang, W. K., Lau, C. G., Mok, V., Ungvari, G. S. & Wong, K. S. Impact of anxiety on health-related quality of life after stroke: a cross-sectional study. Arch. Phys. Med. Rehabil. 94, 2535–2541 (2013).
Tang, W. K. et al. Frontal infarcts and anxiety in stroke. Stroke 43, 1426–1428 (2012).
Chi, S. et al. Tryptophan hydroxylase 2 gene polymorphisms and poststroke anxiety disorders. J. Affect. Disord. 144, 179–182 (2013).
Stein, M. B. & Sareen, J. Generalized anxiety disorder. N. Engl. J. Med. 373, 2059–2068 (2015).
Campbell Burton, C. A. et al. Interventions for treating anxiety after stroke. Cochrane Database Syst. Rev. 12, CD008860 (2011).
Kneebone, I., Walker-Samuel, N., Swanston, J. & Otto, E. Relaxation training after stroke: potential to reduce anxiety. Disabil. Rehabil. 36, 771–774 (2014).
Golding, K., Kneebone, I. & Fife-Schaw, C. Self-help relaxation for post-stroke anxiety: a randomised, controlled pilot study. Clin. Rehabil. 30, 174–180 (2016).
Kiphuth, I. C., Utz, K. S., Noble, A. J., Kohrmann, M. & Schenk, T. Increased prevalence of posttraumatic stress disorder in patients after transient ischemic attack. Stroke 45, 3360–3366 (2014).
Weiss, D. & Marmar, C. in Assessing Psychological Trauma and PTSD (eds Wilson, J. & Keane, T. M.) 168–189 (The Guilford Press, 2004).
Favrole, P. et al. Frequency and predictors of post-traumatic stress disorder after stroke: a pilot study. J. Neurol. Sci. 327, 35–40 (2013).
Goldfinger, J. Z. et al. Correlates of post-traumatic stress disorder in stroke survivors. J. Stroke Cerebrovasc. Dis. 23, 1099–1105 (2014).
Bruggimann, L. et al. Chronic posttraumatic stress symptoms after nonsevere stroke. Neurology 66, 513–516 (2006).
Letamendia, C. et al. Peritraumatic distress predicts acute posttraumatic stress disorder symptoms after a first stroke. Gen Hosp Psychiatry 35, e11–e13 (2012).
Kronish, I. M., Edmondson, D., Goldfinger, J. Z., Fei, K. & Horowitz, C. R. Posttraumatic stress disorder and adherence to medications in survivors of strokes and transient ischemic attacks. Stroke 43, 2192–2197 (2012).
Roy, M. J., Costanzo, M. E., Blair, J. R. & Rizzo, A. A. Compelling evidence that exposure therapy for PTSD normalizes brain function. Stud. Health Technol. Inform. 199, 61–65 (2014).
Wright, A. G. et al. Stability of the DSM-5 Section III pathological personality traits and their longitudinal associations with psychosocial functioning in personality disordered individuals. J. Abnorm. Psychol. 124, 199–207 (2015).
Guiraud, V. & Touzé, E. in Neuropsychiatric Symptoms of Cerebrovascular Diseases Neuropsychiatric Symptoms of Neurological Disease (ed. Ferro, J. M.) 255–298 (Springer, 2013).
Afanasiev, S., Aharon-Peretz, J. & Granot, M. Personality type as a predictor for depressive symptoms and reduction in quality of life among stroke survivals. Am. J. Geriatr. Psychiatry 21, 832–839 (2013).
Jokela, M., Pulkki-Raback, L., Elovainio, M. & Kivimaki, M. Personality traits as risk factors for stroke and coronary heart disease mortality: pooled analysis of three cohort studies. J. Behav. Med. 37, 881–889 (2014).
Votruba, K. L., Rapport, L. J., Whitman, R. D., Johnson, A. & Langenecker, S. Personality differences among patients with chronic aphasia predict improvement in speech–language therapy. Top. Stroke Rehabil. 20, 421–431 (2013).
Jokela, M., Hakulinen, C., Singh-Manoux, A. & Kivimaki, M. Personality change associated with chronic diseases: pooled analysis of four prospective cohort studies. Psychol. Med. 44, 2629–2640 (2014).
Marijnissen, R. M. et al. Depression in context of low neuroticism is a risk factor for stroke: a 9-year cohort study. Neurology 83, 1692–1698 (2014).
Cummings, J. L. et al. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology 44, 2308–2314 (1994).
Starkstein, S. E. & Leentjens, A. F. The nosological position of apathy in clinical practice. J. Neurol. Neurosurg. Psychiatry 79, 1088–1092 (2008).
Habib, M. in Behavior and Mood Disorders in Focal Brain Lesions (eds Bogousslavsky, J. & Cummings, J. L.) 261–284 (Cambridge Univ. Press, 2000).
Caeiro, L., Ferro, J., e Melo, T., Canhao, P. & Figueira, M. Post-stroke apathy: an exploratory longitudinal study. Cerebrovasc. Dis. 35, 507–513 (2013).
Caeiro, L., Ferro, J. & Figueira, M. Apathy in acute stroke patients. Eur. J. Neurol. 19, 291–297 (2012).
van Dalen, J. W., Moll van Charante, E. P., Nederkoorn, P. J., van Gool, W. A. & Richard, E. Poststroke apathy. Stroke 44, 851–860 (2013).
Withall, A., Brodaty, H., Altendorf, A. & Sachdev, P. S. A longitudinal study examining the independence of apathy and depression after stroke: the Sydney Stroke Study. Int. Psychogeriatr. 23, 264–273 (2011).
Caeiro, L., Ferro, J. & Costa, J. Apathy secondary to stroke: a systematic review and meta-analysis. Cerebrovasc. Dis. 35, 23–39 (2013).
van Almenkerk, S., Smalbrugge, M., Depla, M. F., Eefsting, J. A. & Hertogh, C. M. Apathy among institutionalized stroke patients: prevalence and clinical correlates. Am. J. Geriatr. Psychiatry 23, 180–188 (2015).
Brodaty, H. et al. Frequency and clinical, neuropsychological and neuroimaging correlates of apathy following stroke — the Sydney Stroke Study. Psychol. Med. 35, 1707–1716 (2005).
Hama, S. et al. Depression or apathy and functional recovery after stroke. Int. J. Geriatr. Psychiatry 22, 1046–1051 (2007).
Santa, N. et al. Apathy and functional recovery following first-ever stroke. Int. J. Rehabil. Res. 31, 321–326 (2008).
Marin, R. S., Biedrzycki, R. C. & Firinciogullari, S. Reliability and validity of the Apathy Evaluation Scale. Psychiatry Res. 38, 143–162 (1991).
Martin, R., Watson, D. & Wan, C. K. A three-factor model of trait anger: dimensions of affect, behavior, and cognition. J. Pers 68, 869–897 (2000).
Ishikawa, S. & Raine, A. in Neuropsychiatry (eds Schiffer, R. B. et al.) 660–678 (Lippincott Williams & Wilkins, 2003).
Ghika-Schmid, F., van Melle, G., Guex, P. & Bogousslavsky, J. Subjective experience and behavior in acute stroke: the Lausanne Emotion in Acute Stroke Study. Neurology 52, 22–28 (1999).
Santos, C., Caeiro, L., Ferro, J., Albuquerque, R. & Figueira, M. Anger, hostility and aggression in the first days of acute stroke. Eur. J. Neurol. 13, 351–358 (2006).
Carota, A., Bogousslavsky, J. & Calabrese, P. in Neuropsychiatric Symptoms of Cerebrovascular Diseases Neuropsychiatric Symptoms of Neurological Disease (ed. Ferro, J. M.) 161–188 (Springer, 2013).
Moran, P. et al. Personality disorder and cardiovascular disease: results from a national household survey. J. Clin. Psychiatry 68, 69–74 (2007).
Wermer, M. J., Kool, H., Albrecht, K. W. & Rinkel, G. J. Subarachnoid hemorrhage treated with clipping: long-term effects on employment, relationships, personality, and mood. Neurosurgery 60, 91–97; discussion 97–98 (2007).
Ramos-Perdigues, S., Mane-Santacana, A. & Pintor-Perez, L. Prevalence and associated factors of anger post stroke: a systematic review. Rev. Neurol. 60, 481–489 (in Spanish) (2015).
Brodaty, H., Liu, Z., Withall, A. & Sachdev, P. S. The longitudinal course of post-stroke apathy over five years. J. Neuropsychiatry Clin. Neurosci. 25, 283–291 (2013).
Kang, S. Y. & Kim, J. S. Anterior cerebral artery infarction: stroke mechanism and clinical-imaging study in 100 patients. Neurology 70, 2386–2393 (2008).
Bogousslavsky, J. et al. Loss of psychic self-activation with bithalamic infarction. Acta Neurol. Scand. 83, 309–316 (1991).
Caeiro, L., Santos, C., Ferro, J. & Figueira, M. Neuropsychiatric disturbances in acute subarachnoid haemorrhage. Eur. J. Neurol. 18, 857–864 (2011).
Tang, W. K. et al. Location of infarcts and apathy in ischemic stroke. Cerebrovasc. Dis. 35, 566–571 (2013).
Mayo, N. E., Fellows, L. K., Scott, S. C., Cameron, J. & Wood-Dauphinee, S. A longitudinal view of apathy and its impact after stroke. Stroke 40, 3299–3307 (2009).
Angelelli, P. et al. Development of neuropsychiatric symptoms in poststroke patients: a cross-sectional study. Acta Psychiatr. Scand. 110, 55–63 (2004).
Matsuoka, K. et al. Delayed atrophy in posterior cingulate cortex and apathy after stroke. Int. J. Geriatr. Psychiatry 30, 566–572 (2015).
Siegel, J. S. et al. The circuitry of abulia: insights from functional connectivity MRI. NeuroImage Clin. 6, 320–326 (2014).
Yang, S. R., Shang, X. Y., Tao, J., Liu, J. Y. & Hua, P. Voxel-based analysis of fractional anisotropy in post-stroke apathy. PLoS ONE 10, e116168 (2015).
Rochat, L. et al. Poor reward sensitivity and apathy after stroke: implication of basal ganglia. Neurology 81, 1674–1680 (2013).
Murakami, T. et al. Neuroanatomic pathways associated with poststroke affective and apathetic depression. Am. J. Geriatr. Psychiatry 21, 840–847 (2013).
Raine, A. & Yang, Y. Neural foundations to moral reasoning and antisocial behavior. Soc. Cogn. Affect. Neurosci. 1, 203–213 (2006).
Wong, G. K. et al. Neuropsychiatric disturbance after aneurysmal subarachnoid hemorrhage. J. Clin. Neurosci. 21, 1695–1698 (2014).
Oishi, K. et al. Critical role of the right uncinate fasciculus in emotional empathy. Ann. Neurol. 77, 68–74 (2015).
Leigh, R. et al. Acute lesions that impair affective empathy. Brain 136, 2539–2549 (2013).
Skidmore, E. R. Training to optimize learning after traumatic brain injury. Curr. Phys. Med. Rehabil. Rep. 3, 99–105 (2015).
Mikami, K. et al. Prevention of poststroke apathy using escitalopram or problem-solving therapy. Am. J. Geriatr. Psychiatry 21, 855–862 (2013).
Kohno, N. et al. Successful treatment of post-stroke apathy by the dopamine receptor agonist ropinirole. J. Clin. Neurosci. 17, 804–806 (2010).
Robinson, R. G., Jorge, R. E., Clarence-Smith, K. & Starkstein, S. Double-blind treatment of apathy in patients with poststroke depression using nefiracetam. J. Neuropsychiatry Clin. Neurosci. 21, 144–151 (2009).
Waldemar, G. et al. Effect of donepezil on emergence of apathy in mild to moderate Alzheimer's disease. Int. J. Geriatr. Psychiatry 26, 150–157 (2011).
Frakey, L. L., Salloway, S., Buelow, M. & Malloy, P. A randomized, double-blind, placebo-controlled trial of modafinil for the treatment of apathy in individuals with mild-to-moderate Alzheimer's disease. J. Clin. Psychiatry 73, 796–801 (2012).
Rosenberg, P. B. et al. Safety and efficacy of methylphenidate for apathy in Alzheimer's disease: a randomized, placebo-controlled trial. J. Clin. Psychiatry 74, 810–816 (2013).
Autret, K., Arnould, A., Mathieu, S. & Azouvi, P. Transient improvement of poststroke apathy with zolpidem: a single-case, placebo-controlled double-blind study. BMJ Case Rep. http://dx.doi.org/10.1136/bcr-2012-007816, (2013).
Luaute, J., Plantier, D., Wiart, L. & Tell, L. Care management of the agitation or aggressiveness crisis in patients with TBI. Systematic review of the literature and practice recommendations. Ann. Phys. Rehabil. Med. 59, 58–67 (2016).
Choi-Kwon, S. et al. Fluoxetine treatment in poststroke depression, emotional incontinence, and anger proneness: a double-blind, placebo-controlled study. Stroke 37, 156–161 (2006).
Mead, G. et al. The FOCUS, AFFINITY and EFFECTS trials studying the effect(s) of fluoxetine in patients with a recent stroke: a study protocol for three multicentre randomised controlled trials. Trials 16, 369 (2015).
Acknowledgements
This review was partially supported by a post-doctoral grant (“Rehabilitation of apathetic stroke patients”, SFRH/BPD/100399/2014) from the Fundação para Ciência e Tecnologia to Lara Caeiro.
Author information
Authors and Affiliations
Contributions
All authors contributed substantially to the discussion of the content and researched the data for the article. J.M.F. and L.C. wrote and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Ferro, J., Caeiro, L. & Figueira, M. Neuropsychiatric sequelae of stroke. Nat Rev Neurol 12, 269–280 (2016). https://doi.org/10.1038/nrneurol.2016.46
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2016.46
This article is cited by
-
Stroke Experiences and Unmet Needs of Individuals of African Descent Living in High-Income Economy Countries: a Qualitative Meta-Synthesis
Journal of Racial and Ethnic Health Disparities (2023)
-
Development and validation of the Health Education Adherence Scale for Stroke Patients: a cross-sectional study
BMC Neurology (2022)
-
The burden of stroke and its attributable risk factors in the Middle East and North Africa region, 1990–2019
Scientific Reports (2022)
-
Analysis of medical service utilization for post-stroke sequelae in Korea between 2016 and 2018: a cross-sectional study
Scientific Reports (2022)
-
Associations between suicidal ideation and health-related quality of life among community-dwelling stroke survivors: 2013–2017 Korea National Health and Nutrition Examination Survey
Quality of Life Research (2022)