Key Points
-
Auditory neuropathy impairs speech comprehension severely, beyond the extent that would be expected on the basis of increased threshold of audibility
-
Auditory neuropathy encompasses a range of disease mechanisms that typically disrupt the synaptic encoding and/or neural transmission of auditory information in the cochlea and auditory nerve
-
Auditory synaptopathy, impaired sound encoding at the synapses between inner hair cells and spiral ganglion neurons, results from genetic defects or insults such as exposure to loud noise
-
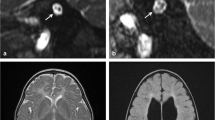
Advanced physiological and psychophysical testing combined with molecular genetic analysis facilitate diagnostics of auditory synaptopathy and neuropathy
-
Although traditional hearing aids often do not provide substantial benefit for patients with auditory synaptopathy or neuropathy, cochlear implants can provide effective hearing rehabilitation depending on the site(s) of disorder
Abstract
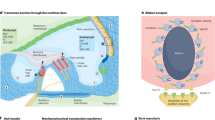
Sensorineural hearing impairment is the most common form of hearing loss, and encompasses pathologies of the cochlea and the auditory nerve. Hearing impairment caused by abnormal neural encoding of sound stimuli despite preservation of sensory transduction and amplification by outer hair cells is known as 'auditory neuropathy'. This term was originally coined for a specific type of hearing impairment affecting speech comprehension beyond changes in audibility: patients with this condition report that they “can hear but cannot understand”. This type of hearing impairment can be caused by damage to the sensory inner hair cells (IHCs), IHC ribbon synapses or spiral ganglion neurons. Human genetic and physiological studies, as well as research on animal models, have recently shown that disrupted IHC ribbon synapse function — resulting from genetic alterations that affect presynaptic glutamate loading of synaptic vesicles, Ca2+ influx, or synaptic vesicle exocytosis — leads to hearing impairment termed 'auditory synaptopathy'. Moreover, animal studies have demonstrated that sound overexposure causes excitotoxic loss of IHC ribbon synapses. This mechanism probably contributes to hearing disorders caused by noise exposure or age-related hearing loss. This Review provides an update on recently elucidated sensory, synaptic and neural mechanisms of hearing impairment, their corresponding clinical findings, and discusses current rehabilitation strategies as well as future therapies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
World Health Organization. Primary ear and hearing care training resource. Advanced level. [online], (2006).
Starr, A., Picton, T. W., Sininger, Y., Hood, L. J. & Berlin, C. I. Auditory neuropathy. Brain 119, 741–754 (1996). Starr and colleagues first coined the term 'auditory neuropathy' and provided a detailed auditory phenotype for hereditary sensory and motor neuropathy.
Zeng, F.-G., Kong, Y.-Y., Michalewski, H. J. & Starr, A. Perceptual consequences of disrupted auditory nerve activity. J. Neurophysiol. 93, 3050–3063 (2005).
Moser, T. et al. Diagnostik und therapie der auditorischen synaptopathie/neuropathie. HNO 54, 833–841 (in German) (2006).
Sutton, G. J. et al. Assessment and management of auditory neuropathy/auditory dys-synchrony: a recommended protocol. Newborn Hearing Screening Programme England) [online], (2004).
Starr, A., Zeng, F. G., Michalewski, H. J. & Moser, T. in The Senses: A Comprehensive Reference Vol 3. Ch. 23 (eds Basbaum, A. I. et al.) 397–412 (Academic Press, 2008).
Penido, R. C. & Isaac, M. L. Prevalence of auditory neuropathy spectrum disorder in an auditory health care service. Braz. J. Otorhinolaryngol. 79, 429–433 (2013).
Rance, G. et al. Clinical findings for a group of infants and young children with auditory neuropathy. Ear Hear. 20, 238–252 (1999).
Foerst, A. et al. Prevalence of auditory neuropathy/synaptopathy in a population of children with profound hearing loss. Int. J. Pediatr. Otorhinolaryngol. 70, 1415–1422 (2006).
Rodríguez-Ballesteros, M. et al. A multicenter study on the prevalence and spectrum of mutations in the otoferlin gene (OTOF) in subjects with nonsyndromic hearing impairment and auditory neuropathy. Hum. Mutat. 29, 823–831 (2008).
Thirlwall, A. S., Brown, D. J., McMillan, P. M., Barker, S. E. & Lesperance, M. M. Phenotypic characterization of hereditary hearing impairment linked to DFNA25. Arch. Otolaryngol. Head Neck Surg. 129, 830–835 (2003).
Matthews, G. & Fuchs, P. The diverse roles of ribbon synapses in sensory neurotransmission. Nat. Rev. Neurosci. 11, 812–822 (2010).
Bech-Hansen, N. T. et al. Loss-of-function mutations in a calcium-channel α1-subunit gene in Xp11.23 cause incomplete X-linked congenital stationary night blindness. Nat. Genet. 19, 264–267 (1998).
Strom, T. M. et al. An L-type calcium-channel gene mutated in incomplete X-linked congenital stationary night blindness. Nat. Genet. 19, 260–263 (1998).
Zeitz, C. et al. Mutations in CABP4, the gene encoding the Ca2+-binding protein 4, cause autosomal recessive night blindness. Am. J. Hum. Genet. 79, 657–667 (2006).
Khimich, D. et al. Hair cell synaptic ribbons are essential for synchronous auditory signalling. Nature 434, 889–894 (2005). Using mouse mutants with inner hair cell synapses deficient in the scaffold protein Bassoon and the synaptic ribbon, Khimich et al . demonstrated how high rates of presynaptic vesicle exocytosis are required for synchronous activation of the spiral ganglion neurons, reflected by the compound action potential.
Buran, B. N. et al. Onset coding is degraded in auditory nerve fibers from mutant mice lacking synaptic ribbons. J. Neurosci. 30, 7587–7597 (2010).
Jung, S. et al. Disruption of adaptor protein 2 (AP-2) in cochlear hair cells impairs vesicle reloading of synaptic release sites and hearing. EMBO J. 34, 2686–2702 (2015). Near-complete restoration of hearing in a knockout mouse model of auditory synaptopathy by a postnatal gene transfer via injection of a viral vector into the cochlea.
Pangrsic, T. et al. Hearing requires otoferlin-dependent efficient replenishment of synaptic vesicles in hair cells. Nat. Neurosci. 13, 869–876 (2010). This study demonstrated that reduced otoferlin levels disrupt vesicle replenishment and, therefore, impair indefatigable transmitter release from inner hair cells.
Parkinson, N. J. et al. Mutant β-spectrin 4 causes auditory and motor neuropathies in quivering mice. Nat. Genet. 29, 61–65 (2001).
Lacas-Gervais, S. et al. βIVΣ1 spectrin stabilizes the nodes of Ranvier and axon initial segments. J. Cell Biol. 166, 983–990 (2004).
Wichmann, C. & Moser, T. Relating structure and function of inner hair cell ribbon synapses. Cell Tissue Res. 361, 95–114 (2015).
Fuchs, P. A. Time and intensity coding at the hair cell's ribbon synapse. J. Physiol. 566, 7–12 (2005).
Moser, T., Neef, A. & Khimich, D. Mechanisms underlying the temporal precision of sound coding at the inner hair cell ribbon synapse. J. Physiol. 576, 55–62 (2006).
Pangrs˘ic˘, T., Reisinger, E. & Moser, T. Otoferlin: a multi-C2 domain protein essential for hearing. Trends Neurosci. 35, 671–680 (2012). A review of the molecular physiology of inner hair cell ribbon synapses, with a focus on otoferlin.
Nouvian, R. et al. Exocytosis at the hair cell ribbon synapse apparently operates without neuronal SNARE proteins. Nat. Neurosci. 14, 411–413 (2011).
Strenzke, N. et al. Complexin-I is required for high-fidelity transmission at the endbulb of held auditory synapse. J. Neurosci. 29, 7991–8004 (2009).
Uthaiah, R. C. & Hudspeth, A. J. Molecular anatomy of the hair cell's ribbon synapse. J. Neurosci. 30, 12387–12399 (2010).
Vogl, C. et al. Unconventional molecular regulation of synaptic vesicle replenishment in cochlear inner hair cells. J. Cell. Sci. 128, 638–644 (2015).
Roux, I. et al. Otoferlin, defective in a human deafness form, is essential for exocytosis at the auditory ribbon synapse. Cell 127, 277–289 (2006). This study describes the auditory phenotype of otoferlin knockout mice and demonstrates that otoferlin has an essential role in inner hair cell exocytosis.
Seal, R. P. et al. Sensorineural deafness and seizures in mice lacking vesicular glutamate transporter 3. Neuron 57, 263–275 (2008). This Slc17a8 -knockout mouse study demonstrated that VGluT3 has an essential role in sound encoding at the inner hair cell ribbon synapse.
Ruel, J. et al. Impairment of SLC17A8 encoding vesicular glutamate transporter-3, VGLUT3, underlies nonsyndromic deafness DFNA25 and inner hair cell dysfunction in null mice. Am. J. Hum. Genet. 83, 278–292 (2008). This study revealed that a mutation in Vglut3 underlies autosomal dominant deafness-25 and showed the requirement of VGluT3 in sound encoding at the inner hair cell ribbon synapse.
Platzer, J. et al. Congenital deafness and sinoatrial node dysfunction in mice lacking class D L-type Ca2+ channels. Cell 102, 89–97 (2000).
Brandt, A., Striessnig, J. & Moser, T. Cav1. 3 channels are essential for development and presynaptic activity of cochlear inner hair cells. J. Neurosci. 23, 10832–10840 (2003).
Geisler, C. D. From Sound to Synapse: Physiology of the Mammalian Ear (Oxford Univ. Press, 1998).
Rutherford, M. A. & Moser, T. in The Primary Auditory Neurons of the Mammalian Cochlea (eds Dabdoub, A. et al.) 117–156 (Springer-Verlag, 2016). This book chapter is part of a recently published textbook on spiral ganglion neurons, and provides a comprehensive overview on the inner hair cell–spiral ganglion neuron synapse.
Mo, Z. L., Adamson, C. L. & Davis, R. L. Dendrotoxin-sensitive K+ currents contribute to accommodation in murine spiral ganglion neurons. J. Physiol. 542, 763 (2002).
Rutherford, M. A., Chapochnikov, N. M. & Moser, T. Spike encoding of neurotransmitter release timing by spiral ganglion neurons of the cochlea. J. Neurosci. 32, 4773–4789 (2012).
Glowatzki, E. & Fuchs, P. A. Transmitter release at the hair cell ribbon synapse. Nat. Neurosci. 5, 147–154 (2002). The first postsynaptic patch-clamp recording from the inner hair cell ribbon synapse of the rat demonstrates massive heterogeneity in size and shape of the excitatory postsynaptic currents, interpreted to reflect synchronous release of multiple vesicles despite the absence of a presynaptic action potential.
Chapochnikov, N. M. et al. Uniquantal release through a dynamic fusion pore is a candidate mechanism of hair cell exocytosis. Neuron 17, 1389–1403 (2014).
Hossain, W. A., Antic, S. D., Yang, Y., Rasband, M. N. & Morest, D. K. Where is the spike generator of the cochlear nerve? Voltage-gated sodium channels in the mouse cochlea. J. Neurosci. 25, 6857–6868 (2005).
Yasunaga, S. et al. A mutation in OTOF, encoding otoferlin, a FER-1-like protein, causes DFNB9, a nonsyndromic form of deafness. Nat. Genet. 21, 363–369 (1999).
Varga, R. et al. OTOF mutations revealed by genetic analysis of hearing loss families including a potential temperature sensitive auditory neuropathy allele. J. Med. Genet. 43, 576–581 (2006).
Marlin, S. et al. Temperature-sensitive auditory neuropathy associated with an otoferlin mutation: deafening fever! Biochem. Biophys. Res. Commun. 394, 737–742 (2010).
Wang, D.-Y. et al. Screening mutations of OTOF gene in Chinese patients with auditory neuropathy, including a familial case of temperature-sensitive auditory neuropathy. BMC Med. Genet. 11, 79 (2010).
Romanos, J. et al. Novel OTOF mutations in Brazilian patients with auditory neuropathy. J. Hum. Genet. 54, 382–385 (2009).
Matsunaga, T. et al. A prevalent founder mutation and genotype–phenotype correlations of OTOF in Japanese patients with auditory neuropathy. Clin. Genet. 82, 425–432 (2012).
McNeil, P. L. & Kirchhausen, T. An emergency response team for membrane repair. Nat. Rev. Mol. Cell. Biol. 6, 499–505 (2005).
Liu, J. et al. Dysferlin, a novel skeletal muscle gene, is mutated in Miyoshi myopathy and limb girdle muscular dystrophy. Nat. Genet. 20, 31–36 (1998).
Bansal, D. et al. Defective membrane repair in dysferlin-deficient muscular dystrophy. Nature 423, 168–172 (2003).
Jiménez, J. L. & Bashir, R. In silico functional and structural characterisation of ferlin proteins by mapping disease-causing mutations and evolutionary information onto three-dimensional models of their C2 domains. J. Neurol. Sci. 260, 114–123 (2007).
Johnson, C. P. & Chapman, E. R. Otoferlin is a calcium sensor that directly regulates SNARE-mediated membrane fusion. J. Cell Biol. 191, 187–197 (2010).
Padmanarayana, M. et al. Characterization of the lipid binding properties of Otoferlin reveals specific interactions between PI(4,5)P2 and the C2C and C2F domains. Biochemistry 53, 5023–5033 (2014).
Ramakrishnan, N. A., Drescher, M. J. & Drescher, D. G. Direct interaction of otoferlin with syntaxin 1A, SNAP-25, and the L-type voltage-gated calcium channel Cav1.3. J. Biol. Chem. 284, 1364–1372 (2009).
Helfmann, S. et al. The crystal structure of the C2A domain of otoferlin reveals an unconventional top loop region. J. Mol. Biol. 406, 479–490 (2011).
Fuson, K. et al. Alternate splicing of dysferlin C2A confers Ca2+-dependent and Ca2+-independent binding for membrane repair. Structure 22, 104–115 (2014).
Santarelli, R., del Castillo, I., Cama, E., Scimemi, P. & Starr, A. Audibility, speech perception and processing of temporal cues in ribbon synaptic disorders due to OTOF mutations. Hear. Res. 330 (Pt B), 200–212 (2015).
Reisinger, E. et al. Probing the functional equivalence of otoferlin and synaptotagmin 1 in exocytosis. J. Neurosci. 31, 4886–4895 (2011).
Dulon, D., Safieddine, S., Jones, S. M. & Petit, C. Otoferlin is critical for a highly sensitive and linear calcium-dependent exocytosis at vestibular hair cell ribbon synapses. J. Neurosci. 29, 10474–10487 (2009).
Varga, R. et al. Non-syndromic recessive auditory neuropathy is the result of mutations in the otoferlin (OTOF) gene. J. Med. Genet. 40, 45–50 (2003).
Schwander, M. et al. A forward genetics screen in mice identifies recessive deafness traits and reveals that pejvakin is essential for outer hair cell function. J. Neurosci. 27, 2163–2175 (2007).
Wynne, D. P. et al. Loudness adaptation accompanying ribbon synapse and auditory nerve disorders. Brain 136, 1626–1638 (2013).
Duncker, S. V. et al. Otoferlin couples to clathrin-mediated endocytosis in mature cochlear inner hair cells. J. Neurosci. 33, 9508–9519 (2013).
Greene, C. C. et al. DFNA25, a novel locus for dominant nonsyndromic hereditary hearing impairment, maps to 12q21-24. Am. J. Hum. Genet. 68, 254–260 (2001).
Obholzer, N. et al. Vesicular glutamate transporter 3 is required for synaptic transmission in zebrafish hair cells. J. Neurosci. 28, 2110–2118 (2008).
Petek, E. et al. Molecular characterization of a 12q22-q24 deletion associated with congenital deafness: confirmation and refinement of the DFNA25 locus. Am. J. Med. Genet. A 117A, 122–126 (2003).
Baig, S. M. et al. Loss of Cav1.3 (CACNA1D) function in a human channelopathy with bradycardia and congenital deafness. Nat. Neurosci. 14, 77–84 (2011). The first report of a human deafness syndrome attributed to a loss-of-function mutation in CACNA1D.
Surmeier, D. J. Calcium, ageing, and neuronal vulnerability in Parkinson's disease. Lancet Neurol. 6, 933–938 (2007).
McKinney, B. C. & Murphy, G. G. The L-Type voltage-gated calcium channel Cav1.3 mediates consolidation, but not extinction, of contextually conditioned fear in mice. Learn. Mem. 13, 584–589 (2006).
Neef, J. et al. The Ca2+ channel subunit β2 regulates Ca2+ channel abundance and function in inner hair cells and is required for hearing. J. Neurosci. 29, 10730 (2009).
Wycisk, K. A. et al. Mutation in the auxiliary calcium-channel subunit CACNA2D4 causes autosomal recessive cone dystrophy. Am. J. Hum. Genet. 79, 973–977 (2006).
Schrauwen, I. et al. A mutation in CABP2, expressed in cochlear hair cells, causes autosomal-recessive hearing impairment. Am. J. Hum. Genet. 91, 636–645 (2012). A report of a hearing impairment in a family with a CABP2 mutation, suggesting that inner hair cell synaptic dysfunction is caused by impaired presynaptic Ca2+ influx.
Haeseleer, F. et al. Essential role of Ca2+-binding protein 4, a Cav1.4 channel regulator, in photoreceptor synaptic function. Nat. Neurosci. 7, 1079–1087 (2004).
Santarelli, R. et al. OPA1-related auditory neuropathy: site of lesion and outcome of cochlear implantation. Brain 138, 563–576 (2015).
Yu-Wai-Man, P. et al. Multi-system neurological disease is common in patients with OPA1 mutations. Brain 133, 771–786 (2010).
La Morgia, C., Carbonelli, M., Barboni, P., Sadun, A. A. & Carelli, V. Medical management of hereditary optic neuropathies. Front. Neurol. 5, 141 (2014).
Alexander, C. et al. OPA1, encoding a dynamin-related GTPase, is mutated in autosomal dominant optic atrophy linked to chromosome 3q28. Nat. Genet. 26, 211–215 (2000).
Delettre, C. et al. Nuclear gene OPA1, encoding a mitochondrial dynamin-related protein, is mutated in dominant optic atrophy. Nat. Genet. 26, 207–210 (2000).
Kasahara, A. & Scorrano, L. Mitochondria: from cell death executioners to regulators of cell differentiation. Trends Cell Biol. 24, 761–770 (2014).
Ferré, M. et al. Molecular screening of 980 cases of suspected hereditary optic neuropathy with a report on 77 novel OPA1 mutations. Hum. Mutat. 30, E692–E705 (2009).
Alavi, M. V. et al. A splice site mutation in the murine Opa1 gene features pathology of autosomal dominant optic atrophy. Brain 130, 1029–1042 (2006).
Starr, A., Dong, C. J. & Michalewski, H. J. Brain potentials before and during memory scanning. Electroencephalogr. Clin. Neurophysiol. 99, 28–37 (1996).
Starr, A. Pathology and physiology of auditory neuropathy with a novel mutation in the MPZ gene (Tyr145→Ser). Brain 126, 1604–1619 (2003).
Kabzin´ska, D. et al. Late-onset Charcot−Marie−Tooth type 2 disease with hearing impairment associated with a novel Pro105Thr mutation in the MPZ gene. Am. J. Med. Genet. A 143A, 2196–2199 (2007).
Verhagen, W. I. M. et al. Sensorineural hearing impairment in patients with Pmp22 duplication, deletion, and frameshift mutations. Otol. Neurotol. 26, 405–414 (2005).
Kovach, M. J. et al. Anticipation in a unique family with Charcot−Marie−Tooth syndrome and deafness: delineation of the clinical features and review of the literature. Am. J. Med. Genet. 108, 295–303 (2002).
Rance, G. & Starr, A. Pathophysiological mechanisms and functional hearing consequences of auditory neuropathy. Brain 138, 3141–3158 (2015). In this review, Rance and Starr provide a comprehensive overview of spiral ganglion disorders and their clinical manifestations.
Delmaghani, S. et al. Mutations in the gene encoding pejvakin, a newly identified protein of the afferent auditory pathway, cause DFNB59 auditory neuropathy. Nat. Genet. 38, 770–778 (2006).
Borck, G. et al. High frequency of autosomal-recessive DFNB59 hearing loss in an isolated Arab population in Israel. Clin. Genet. 82, 271–276 (2012).
Ebermann, I. et al. Truncating mutation of the DFNB59 gene causes cochlear hearing impairment and central vestibular dysfunction. Hum. Mutat. 28, 571–577 (2007).
Hashemzadeh Chaleshtori, M. et al. Novel mutations in the pejvakin gene are associated with autosomal recessive non-syndromic hearing loss in Iranian families. Clin. Genet. 72, 261–263 (2007).
Collin, R. W. J. et al. Involvement of DFNB59 mutations in autosomal recessive nonsyndromic hearing impairment. Hum. Mutat. 28, 718–723 (2007).
Delmaghani, S. et al. Hypervulnerability to sound exposure through impaired adaptive proliferation of peroxisomes. Cell 163, 894–906 (2015). This study demonstrated that genetic disruption of pevjakin increases vulnerability of hair cells and neurons to noise exposure, providing an interesting experimental model for hearing impairment as a multifactorial disease.
Kim, T. B. et al. A gene responsible for autosomal dominant auditory neuropathy (AUNA1) maps to 13q14–21. J. Med. Genet. 41, 872 (2004).
Starr, A. et al. A dominantly inherited progressive deafness affecting distal auditory nerve and hair cells. J. Assoc. Res. Otolaryngol. 5, 411–426 (2004).
Schoen, C. J. et al. Increased activity of Diaphanous homolog 3 (DIAPH3)/diaphanous causes hearing defects in humans with auditory neuropathy and in Drosophila. Proc. Natl Acad. Sci. USA 107, 13396–13401 (2010).
Schoen, C. J., Burmeister, M. & Lesperance, M. M. Diaphanous homolog 3 (Diap3) overexpression causes progressive hearing loss and inner hair cell defects in a transgenic mouse model of human deafness. PLoS ONE 8, e56520 (2013).
Rance, G. et al. Speech perception ability in individuals with Friedreich ataxia. Brain 131, 2002–2012 (2008).
Kirkim, G., Serbetcioglu, B., Erdag, T. K. & Ceryan, K. The frequency of auditory neuropathy detected by universal newborn hearing screening program. Int. J. Pediatr. Otorhinolaryngol. 72, 1461–1469 (2008).
Schulman-Galambos, C. & Galambos, R. Brain stem evoked response audiometry in newborn hearing screening. Arch. Otolaryngol. 105, 86–90 (1979).
Oh, W. et al. Association between peak serum bilirubin and neurodevelopmental outcomes in extremely low birth weight infants. Pediatrics 112, 773–779 (2003).
Olds, C. & Oghalai, J. S. Audiologic impairment associated with bilirubin-induced neurologic damage. Semin. Fetal Neonatal Med. 20, 42–46 (2015).
Smith, C. M., Barnes, G. P., Jacobson, C. A. & Oelberg, D. G. Auditory brainstem response detects early bilirubin neurotoxicity at low indirect bilirubin values. J. Perinatol. 24, 730–732 (2004).
Amatuzzi, M. G. et al. Selective inner hair cell loss in premature infants and cochlea pathological patterns from neonatal intensive care unit autopsies. Arch. Otolaryngol. Head Neck Surg. 127, 629–636 (2001).
Uziel, A., Marot, M. & Pujol, R. The Gunn rat: an experimental model for central deafness. Acta Otolaryngol. 95, 651–656 (1983).
Haustein, M. D. et al. Acute hyperbilirubinaemia induces presynaptic neurodegeneration at a central glutamatergic synapse. J. Physiol. 588, 4683–4693 (2010).
Spencer, R. F., Shaia, W. T., Gleason, A. T., Sismanis, A. & Shapiro, S. M. Changes in calcium-binding protein expression in the auditory brainstem nuclei of the jaundiced Gunn rat. Hear. Res. 171, 129–141 (2002).
Attias, J., Raveh, E., Aizer-Dannon, A., Bloch-Mimouni, A. & Fattal-Valevski, A. Auditory system dysfunction due to infantile thiamine deficiency: long-term auditory sequelae. Audiol. Neurootol. 17, 309–320 (2012).
Oishi, K. et al. Targeted disruption of Slc19a2, the gene encoding the high-affinity thiamin transporter Thtr-1, causes diabetes mellitus, sensorineural deafness and megaloblastosis in mice. Hum. Mol. Genet. 11, 2951–2960 (2002).
Liberman, M. C., Tartaglini, E., Fleming, J. C. & Neufeld, E. J. Deletion of SLC19A2, the high affinity thiamine transporter, causes selective inner hair cell loss and an auditory neuropathy phenotype. J. Assoc. Res. Otolaryngol. 7, 211–217 (2006).
Yang, C.-H., Schrepfer, T. & Schacht, J. Age-related hearing impairment and the triad of acquired hearing loss. Front. Cell. Neurosci. 9, 276 (2015). This article, part of a special review issue of Frontiers in Cellular Neuroscience , provides a detailed update on sensory hair cell death and studies aiming at inducing hair cell regeneration.
Henry, W. R. & Mulroy, M. J. Afferent synaptic changes in auditory hair cells during noise-induced temporary threshold shift. Hear. Res. 84, 81–90 (1995).
Puel, J. L., Pujol, R., Ladrech, S. & Eybalin, M. α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid electrophysiological and neurotoxic effects in the guinea-pig cochlea. Neuroscience 45, 63–72 (1991).
Puel, J. L., Ruel, J., Gervais d'Aldin, C. & Pujol, R. Excitotoxicity and repair of cochlear synapses after noise-trauma induced hearing loss. Neuroreport 9, 2109–2114 (1998).
Stamataki, S., Francis, H. W., Lehar, M., May, B. J. & Ryugo, D. K. Synaptic alterations at inner hair cells precede spiral ganglion cell loss in aging C57BL/6J mice. Hear. Res. 221, 104–118 (2006).
Kujawa, S. G. & Liberman, M. C. Adding insult to injury: cochlear nerve degeneration after 'temporary' noise-induced hearing loss. J. Neurosci. 29, 14077 (2009). This study shows that in mice, sound overexposure that only temporarily reduces audibility can cause a permanent loss of inner hair cell ribbon synapses and subsequent loss of spiral ganglion neurons.
Sergeyenko, Y., Lall, K., Liberman, M. C. & Kujawa, S. G. Age-related cochlear synaptopathy: an early-onset contributor to auditory functional decline. J. Neurosci. 33, 13686–13694 (2013).
Kujawa, S. G. & Liberman, M. C. Synaptopathy in the noise-exposed and aging cochlea: primary neural degeneration in acquired sensorineural hearing loss. Hear. Res. 330(Pt B), 191–199 (2015). This Review is a part of a review series on auditory synapses and synaptopathies and summarizes a large body of animal work on synaptic alterations in noise-induced and age-related hearing loss.
Hakuba, N., Koga, K., Gyo, K., Usami, S. I. & Tanaka, K. Exacerbation of noise-induced hearing loss in mice lacking the glutamate transporter GLAST. J. Neurosci. 20, 8750–8753 (2000).
Meyer, A. C. et al. Tuning of synapse number, structure and function in the cochlea. Nat. Neurosci. 12, 444–453 (2009).
Furman, A. C., Kujawa, S. G. & Liberman, M. C. Noise-induced cochlear neuropathy is selective for fibers with low spontaneous rates. J. Neurophysiol. 110, 577–586 (2013).
Bourien, J. et al. Contribution of auditory nerve fibers to compound action potential of the auditory nerve. J. Neurophysiol. 112, 1025–1039 (2014).
Wan, G., Gómez-Casati, M. E., Gigliello, A. R., Liberman, M. C. & Corfas, G. Neurotrophin-3 regulates ribbon synapse density in the cochlea and induces synapse regeneration after acoustic trauma. eLIFE 3, e03564 (2014).
Schaette, R. & McAlpine, D. Tinnitus with a normal audiogram: physiological evidence for hidden hearing loss and computational model. J. Neurosci. 31, 13452–13457 (2011).
Starr, A. et al. Absence of both auditory evoked potentials and auditory percepts dependent on timing cues. Brain 114, 1157–1180 (1991).
Starr, A. et al. Cochlear receptor (microphonic and summating potentials, otoacoustic emissions) and auditory pathway (auditory brain stem potentials) activity in auditory neuropathy. Ear Hear. 22, 91 (2001).
Santarelli, R. et al. Abnormal cochlear potentials from deaf patients with mutations in the otoferlin gene. J. Assoc. Res. Otolaryngol. 10, 545–556 (2009).
Pauli-Magnus, D. et al. Detection and differentiation of sensorineural hearing loss in mice using auditory steady-state responses and transient auditory brainstem responses. Neuroscience 149, 673–684 (2007).
Shearer, A. E. & Smith, R. J. H. Massively parallel sequencing for genetic diagnosis of hearing loss: the new standard of care. Otolaryngol. Head Neck Surg. 153, 175–182 (2015).
Dean, C., Felder, G. & Kim, A. H. Analysis of speech perception outcomes among patients receiving cochlear implants with auditory neuropathy spectrum disorder. Otol. Neurotol. 34, 1610–1614 (2013).
Humphriss, R. et al. Does cochlear implantation improve speech recognition in children with auditory neuropathy spectrum disorder? A systematic review. Int. J. Audiol. 52, 442–454 (2013).
Roush, P., Frymark, T., Venediktov, R. & Wang, B. Audiologic management of auditory neuropathy spectrum disorder in children: a systematic review of the literature. Am. J. Audiol. 20, 159–170 (2011).
Giraudet, F. & Avan, P. Auditory neuropathies: understanding their pathogenesis to illuminate intervention strategies. Curr. Opin. Neurol. 25, 50–56 (2012).
Rance, G. & Barker, E. J. Speech and language outcomes in children with auditory neuropathy/dys-synchrony managed with either cochlear implants or hearing aids. Int. J. Audiol. 48, 313–320 (2009).
Ching, T. Y. C. et al. Impact of the presence of auditory neuropathy spectrum disorder (ANSD) on outcomes of children at three years of age. Int. J. Audiol. 52, S55–S64 (2013).
Hall, R. D. Estimation of surviving spiral ganglion cells in the deaf rat using the electrically evoked auditory brainstem response. Hear. Res. 49, 155–168 (1990).
Hall, R. D. Estimation of surviving spiral ganglion cells in the deaf rat using the electrically evoked auditory brainstem response. Hear. Res. 45, 123–136 (1990).
Zhou, R., Abbas, P. J. & Assouline, J. G. Electrically evoked auditory brainstem response in peripherally myelin-deficient mice. Hear Res. 88, 98–106 (1995).
Rouillon, I. et al. Results of cochlear implantation in two children with mutations in the OTOF gene. Int. J. Pediatr. Otorhinolaryngol. 70, 689–696 (2006).
Hernandez, V. H. et al. Optogenetic stimulation of the auditory pathway. J. Clin. Invest. 124, 1114–1129 (2014).
Jeschke, M. & Moser, T. Considering optogenetic stimulation for cochlear implants. Hear. Res. 322, 224–234 (2015).
Akil, O. et al. Restoration of hearing in the VGLUT3 knockout mouse using virally mediated gene therapy. Neuron 75, 283–293 (2012). This mouse study demonstrated a near-complete restoration of hearing in a knockout mouse model of auditory synaptopathy by a postnatal gene transfer via injection of a viral vector into the cochlea.
US National Library of Medicine. ClinicalTrials.gov[online] (2015).
Author information
Authors and Affiliations
Contributions
Both authors researched the literature, assembled the Figures, and wrote, edited and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
- Auditory neuropathy
-
A hearing impairment found in individuals with hereditary motor and sensory neuropathy; impairs speech comprehension beyond what would be expected on the basis of pure tone audiograms.
- Ribbon synapses
-
Highly specialized synapses between the inner hair cells and spiral ganglion neurons, with an electron-dense structure — the synaptic ribbon — at the presynaptic active zone that mediates neurotransmitter release.
- Cochlear microphone potentials
-
Outer hair cells generate local cochlear potentials that follow the sound stimulus so precisely that they are called 'microphone potentials'.
- Otoacoustic emission
-
Sound generated from within the inner ear that can be measured with a sensitive microphone in the external ear canal to assess outer hair cell function.
- Auditory brainstem responses
-
Evoked potentials in response to repetitive acoustic stimulation that are recorded from scalp EEG electrodes and typically have five peaks, referred to as waves I–V.
- Spiral ganglion compound action potential
-
The first auditory brainstem response peak, wave I, reflects the spiral ganglion compound action potential; this potential can be recorded with better resolution using electrocochleography.
- Auditory synaptopathy
-
Hearing impairment caused by dysfunction or loss of ribbon synapses in the inner hair cells; has been termed auditory synaptopathy and can show clinical findings similar to those described above for auditory neuropathy.
- Organ of Corti
-
The organ of Corti is the end organ of the sense of hearing that harbours the sensory inner and outer hair cells, as well as afferent and efferent nerve fibres and various types of supporting cells.
- Compound action potential
-
Reflects the synchronized firing of spiral ganglion neurons; assessed by intrameatal or transtympanic electrocochleography.
- Glutamate excitotoxicity
-
Excessive presynaptic glutamate release leading to massive depolarization and subsequent synapse loss.
Rights and permissions
About this article
Cite this article
Moser, T., Starr, A. Auditory neuropathy — neural and synaptic mechanisms. Nat Rev Neurol 12, 135–149 (2016). https://doi.org/10.1038/nrneurol.2016.10
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2016.10