Key Points
-
Migraine affects up to one in four women of reproductive age, but migraine will often improve spontaneously during pregnancy
-
Nonpharmacological approaches should always be tried as first-line treatment for migraine during pregnancy
-
Several effective acute antimigraine medications are reasonably safe to use for pregnant and breastfeeding women
-
In pregnancy, preventive drug therapy should be considered only in the most severe migraine cases
-
Periconceptional counselling is important to promote a safe and healthy pregnancy and postpartum period for the mother and child
Abstract
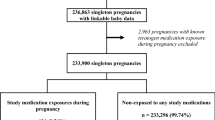
Migraine affects up to 25% of women of reproductive age. In the majority of these women, migraine improves progressively during pregnancy, but symptoms generally recur shortly after delivery. As suboptimally treated migraine in pregnancy could have negative consequences for both mother and fetus, the primary aim of clinicians should be to provide optimal treatment according to stage of pregnancy, while minimising possible risks related to drug therapy. Nonpharmacological approaches are always first-line treatment, and should also be used to complement any required drug treatment. Paracetamol is the preferred drug for acute treatment throughout pregnancy. If paracetamol is not sufficiently effective, sporadic use of sumatriptan can be considered. NSAIDs such as ibuprofen can also be used under certain circumstances, though their intake in the first and third trimesters is associated with specific risks and contraindications. Preventive treatment should only be considered in the most severe cases. In women contemplating pregnancy, counselling is essential to promote a safe and healthy pregnancy and postpartum period for the mother and child, and should involve a dialogue addressing maternal concerns and expectations about drug treatment. This Review summarizes current evidence of the safety of the most common antimigraine medications during pregnancy and breastfeeding, and provides treatment recommendations for use in clinical practice.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Change history
19 March 2015
In the section discussing treatment options during pregnancy, the last sentence under the subheading 'Antidepressants' should cite reference 83, not 84. The correction has been made to the print and online versions of the article.
03 April 2015
In the section discussing treatment options during pregnancy, subheadings 'Ergot alkaloids' and 'Antidepressants' should cite reference 25, not 23. In the section discussing treatment options during breastfeeding, subheading 'Paracetamol' and 'Opioid analgesics' should cite reference 24, not 21; subheading 'Ergot alkaloids' should cite reference 19, not 24. The corrections have been made to the print and online versions of the article.
References
Stovner, L. J., Zwart, J. A., Hagen, K., Terwindt, G. M. & Pascual, J. Epidemiology of headache in Europe. Eur. J. Neurol. 13, 333–345 (2006).
Lipton, R. B. et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 68, 343–349 (2007).
Sacco, S., Ricci, S., Degan, D. & Carolei, A. Migraine in women: the role of hormones and their impact on vascular diseases. J. Headache Pain 13, 177–189 (2012).
Sances, G. et al. Course of migraine during pregnancy and postpartum: a prospective study. Cephalalgia 23, 197–205 (2003).
Maggioni, F., Alessi, C., Maggino, T. & Zanchin, G. Headache during pregnancy. Cephalalgia 17, 765–769 (1997).
Nappi, R. E. et al. Headaches during pregnancy. Curr. Pain Headache Rep. 15, 289–294 (2011).
Aube, M. Migraine in pregnancy. Neurology 53, S26–S28 (1999).
Wright, G. D. & Patel, M. K. Focal migraine and pregnancy. Br. Med. J. (Clin. Res. Ed.) 293, 1557–1558 (1986).
Hoshiyama, E. et al. Postpartum migraines: a long-term prospective study. Intern. Med. 51, 3119–3123 (2012).
Kvisvik, E., Stovner, L., Helde, G., Bovim, G. & Linde, M. Headache and migraine during pregnancy and puerperium: the MIGRA-study. J. Headache Pain 12, 443–451 (2011).
Contag, S. A. & Bushnell, C. Contemporary management of migrainous disorders in pregnancy. Curr. Opin. Obstet. Gynecol. 22, 437–445 (2010).
Nezvalová-Henriksen, K., Spigset, O. & Nordeng, H. Maternal characteristics and migraine pharmacotherapy during pregnancy: cross-sectional analysis of data from a large cohort study. Cephalalgia 29, 1267–1276 (2009).
Gladstone, J. P., Eross, E. J. & Dodick, D. W. Migraine in special populations. Treatment strategies for children and adolescents, pregnant women, and the elderly. Postgrad. Med. 115, 39–44, 47–50 (2004).
Facchinetti, F. et al. Migraine is a risk factor for hypertensive disorders in pregnancy: a prospective cohort study. Cephalalgia 29, 286–292 (2009).
Williams, M. A. et al. Trimester-specific blood pressure levels and hypertensive disorders among pregnant migraineurs. Headache 51, 1468–1482 (2011).
Adeney, K. L. et al. Risk of preeclampsia in relation to maternal history of migraine headaches. J. Matern. Fetal Neonatal Med. 18, 167–172 (2005).
Bushnell, C. D., Jamison, M. & James, A. H. Migraines during pregnancy linked to stroke and vascular diseases: US population based case-control study. BMJ 338, b664 (2009).
Hauth, J. C. et al. Pregnancy outcomes in healthy nulliparas who developed hypertension. Calcium for Preeclampsia Prevention Study Group. Obstet. Gynecol. 95, 24–28 (2000).
Briggs, G. G. & Freeman, R. K. (eds) Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk 10th edn (Wolters Kluwer Health, 2014).
Thompson, J. M., Waldie, K. E., Wall, C. R., Murphy, R. & Mitchell, E. A. Associations between acetaminophen use during pregnancy and ADHD symptoms measured at ages 7 and 11 years. PLoS ONE 9, e108210 (2014).
Brandlistuen, R. E., Ystrøm, E., Nulman, I., Koren, G. & Nordeng, H. Prenatal paracetamol exposure and child neurodevelopment: a sibling-controlled cohort study. Int. J. Epidemiol. 42, 1702–1713 (2013).
Liew, Z., Ritz, B., Rebordosa, C., Lee, P. C. & Olsen, J. Acetaminophen use during pregnancy, behavioral problems, and hyperkinetic disorders. JAMA Pediatr. 168, 313–320 (2014).
European Medicines Agency. Pharmacovigilance Risk Assessment Committee (PRAC): minutes of the meeting on 5–8 May 2014. PRAC: Agendas, minutes and highlights [online], (2014).
Worthington, I. et al. Canadian Headache Society Guideline: acute drug therapy for migraine headache. Can. J. Neurol. Sci. 40, S1–S80 (2013).
Evers, S. et al. EFNS guideline on the drug treatment of migraine—revised report of an EFNS task force. Eur. J. Neurol. 16, 968–981 (2009).
Østensen, M. & Skomsvoll, J. Anti-inflammatory pharmacotherapy during pregnancy. Expert Opin. Pharmacother. 5, 571–580 (2004).
Koren, G., Florescu, A., Costei, A. M., Boskovic, R. & Moretti, M. E. Nonsteroidal antiinflammatory drugs during third trimester and the risk of premature closure of the ductus arteriosus: a meta-analysis. Ann. Pharmacother. 40, 824–829 (2006).
Insel, P. A. in Goodman and Gilman's The Pharmacological Basis of Therapeutics 9th edn Ch. 27 (eds Hardman, J. G. et al.) 617–657 (MacGraw–Hill, 1996).
Reese, J. et al. Coordinated regulation of fetal and maternal prostaglandins directs successful birth and postnatal adaptation in the mouse. Proc. Natl Acad. Sci. USA 97, 9759–9764 (2000).
Li, D. K., Liu, L. & Odouli, R. Exposure to non-steroidal anti-inflammatory drugs during pregnancy and risk of miscarriage: population based cohort study. BMJ 327, 368 (2003).
Nielsen, G. L., Sørensen, H. T., Larsen, H. & Pedersen, L. Risk of adverse birth outcome and miscarriage in pregnant users of non-steroidal anti-inflammatory drugs: population based observational study and case-control study. BMJ 322, 266–270 (2001).
Nakhai-Pour, H. R., Broy, P., Sheehy, O. & Berard, A. Use of nonaspirin nonsteroidal anti-inflammatory drugs during pregnancy and the risk of spontaneous abortion. CMAJ 183, 1713–1720 (2011).
Hernandez, R. K., Werler, M. M., Romitti, P., Sun, L. & Anderka, M. Nonsteroidal antiinflammatory drug use among women and the risk of birth defects. Am. J. Obstet. Gynecol. 206, 228.e1–228.e8 (2012).
Ofori, B., Oraichi, D., Blais, L., Rey, E. & Berard, A. Risk of congenital anomalies in pregnant users of non-steroidal anti-inflammatory drugs: a nested case-control study. Birth Defects Res. B Dev. Reprod. Toxicol. 77, 268–279 (2006).
Ericson, A. & Källén, B. A. Nonsteroidal anti-inflammatory drugs in early pregnancy. Reprod. Toxicol. 15, 371–375 (2001).
Daniel, S. et al. Fetal exposure to nonsteroidal anti-inflammatory drugs and spontaneous abortions. CMAJ 186, E177–E182 (2014).
Edwards, D. R. et al. Periconceptional over-the-counter nonsteroidal anti-inflammatory drug exposure and risk for spontaneous abortion. Obstet. Gynecol. 120, 113–122 (2012).
Nielsen, G. L., Skriver, M. V., Pedersen, L. & Sørensen, H. T. Danish group reanalyses miscarriage in NSAID users. BMJ 328, 109 (2004).
Cassina, M. et al. First trimester diclofenac exposure and pregnancy outcome. Reprod. Toxicol. 30, 401–404 (2010).
Nezvalová-Henriksen, K., Spigset, O. & Nordeng, H. Effects of ibuprofen, diclofenac, naproxen, and piroxicam on the course of pregnancy and pregnancy outcome: a prospective cohort study. BJOG 120, 948–959 (2013).
Daniel, S. et al. Major malformations following exposure to nonsteroidal antiinflammatory drugs during the first trimester of pregnancy. J. Rheumatol. 39, 2163–2169 (2012).
van Gelder, M. M., Roeleveld, N. & Nordeng, H. Exposure to non-steroidal anti-inflammatory drugs during pregnancy and the risk of selected birth defects: a prospective cohort study. PLoS ONE 6, e22174 (2011).
Cleves, M. A. et al. Maternal use of acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs), and muscular ventricular septal defects. Birth Defects Res. A Clin. Mol. Teratol 70, 107–113 (2004).
Jensen, M. S. et al. Maternal use of acetaminophen, ibuprofen, and acetylsalicylic acid during pregnancy and risk of cryptorchidism. Epidemiology 21, 779–785 (2010).
Norton, M. E., Merrill, J., Cooper, B. A., Kuller, J. A. & Clyman, R. I. Neonatal complications after the administration of indomethacin for preterm labor. N. Engl. J. Med. 329, 1602–1607 (1993).
Vermillion, S. T., Scardo, J. A., Lashus, A. G. & Wiles, H. B. The effect of indomethacin tocolysis on fetal ductus arteriosus constriction with advancing gestational age. Am. J. Obstet. Gynecol. 177, 256–259; discussion 259–261 (1997).
Ojala, R., Ikonen, S. & Tammela, O. Perinatal indomethacin treatment and neonatal complications in preterm infants. Eur. J. Pediatr. 159, 153–155 (2000).
Doyle, N. M., Gardner, M. O., Wells, L., Qualls, C. & Papile, L. A. Outcome of very low birth weight infants exposed to antenatal indomethacin for tocolysis. J. Perinatol. 25, 336–340 (2005).
Ojala, R. et al. Renal follow up of premature infants with and without perinatal indomethacin exposure. Arch. Dis. Child. Fetal Neonatal Ed. 84, F28–F33 (2001).
Benini, D., Fanos, V., Cuzzolin, L. & Tato, L. In utero exposure to nonsteroidal anti-inflammatory drugs: neonatal renal failure. Pediatr. Nephrol. 19, 232–234 (2004).
Phadke, V., Bhardwaj, S., Sahoo, B. & Kanhere, S. Maternal ingestion of diclofenac leading to renal failure in newborns. Pediatr. Nephrol. 27, 1033–1036 (2012).
Alano, M. A., Ngougmna, E., Ostrea, E. M. Jr & Konduri, G. G. Analysis of nonsteroidal antiinflammatory drugs in meconium and its relation to persistent pulmonary hypertension of the newborn. Pediatrics 107, 519–523 (2001).
Van Marter, L. J., Hernandez-Diaz, S., Werler, M. M., Louik, C. & Mitchell, A. A. Nonsteroidal antiinflammatory drugs in late pregnancy and persistent pulmonary hypertension of the newborn. Pediatrics 131, 79–87 (2013).
Tyler, C. P. et al. Brain damage in preterm newborns and maternal medication: the ELGAN Study. Am. J. Obstet. Gynecol. 207, 192.e1–192.e9 (2012).
Provost, M., Eaton, J. L. & Clowse, M. E. Fertility and infertility in rheumatoid arthritis. Curr. Opin. Rheumatol 26, 308–314 (2014).
Soldin, O. P., Dahlin, J. & O'Mara, D. M. Triptans in pregnancy. Ther. Drug Monit. 30, 5–9 (2008).
Gupta, S. et al. Functional reactivity of 5-HT receptors in human umbilical cord and maternal subcutaneous fat arteries after normotensive or pre-eclamptic pregnancy. J. Hypertens. 24, 1345–1353 (2006).
Bonnin, A. & Levitt, P. Fetal, maternal, and placental sources of serotonin and new implications for developmental programming of the brain. Neuroscience 197, 1–7 (2011).
Ephross, S. A. & Sinclair, S. M. Final results from the 16-year sumatriptan, naratriptan, and treximet pregnancy registry. Headache 54, 1158–1172 (2014).
Nezvalová-Henriksen, K., Spigset, O. & Nordeng, H. Triptan safety during pregnancy: a Norwegian population registry study. Eur. J. Epidemiol. 28, 759–769 (2013).
Berard, A. & Kori, S. Dihydroergotamine (DHE) use during gestation and the risk of adverse pregnancy outcomes. Headache 52, 1085–1093 (2012).
Merck & Co. Thirteenth/Fourteenth Annual Report from the Merck Pregnancy Registry for MAXALT (rizatriptan benzoate): covering the period from approval (June 1998) through June 12, 2012. Merck Pregnancy Registries [online], (2012).
Källén, B., Nilsson, E. & Otterblad Olausson, P. Delivery outcome after maternal use of drugs for migraine: a register study in Sweden. Drug Saf. 34, 691–703 (2011).
Nezvalová-Henriksen, K., Spigset, O. & Nordeng, H. Triptan exposure during pregnancy and the risk of major congenital malformations and adverse pregnancy outcomes: results from the Norwegian Mother and Child. Cohort Study. Headache 50, 563–575 (2010).
Källén, B. & Lygner, P. E. Delivery outcome in women who used drugs for migraine during pregnancy with special reference to sumatriptan. Headache 41, 351–356 (2001).
Olesen, C., Steffensen, F. H., Sørensen, H. T., Nielsen, G. L. & Olsen, J. Pregnancy outcome following prescription for sumatriptan. Headache 40, 20–24 (2000).
O'Quinn, S. et al. Pregnancy and perinatal outcomes in migraineurs using sumatriptan: a prospective study. Arch. Gynecol. Obstet. 263, 7–12 (1999).
Shuhaiber, S. B. et al. Pregnancy outcome following first trimester exposure to sumatriptan. Neurology 51, 581–583 (1998).
Nezvalová-Henriksen, K., Spigset, O. & Nordeng, H. M. Triptan exposure during pregnancy and the risk of major congenital malformations and adverse pregnancy outcomes: results from the Norwegian Mother and Child Cohort Study [erratum]. Headache 52, 1319–1320 (2012).
Broussard, C. S. et al. Maternal treatment with opioid analgesics and risk for birth defects. Am. J. Obstet. Gynecol. 204, 314.e1–314.e11 (2011).
Nezvalová-Henriksen, K., Spigset, O. & Nordeng, H. Effects of codeine on pregnancy outcome: results from a large population-based cohort study [erratum]. Eur. J. Clin. Pharmacol. 68, 1689–1690 (2012).
Cassina, M., Di Gianantonio, E., Toldo, I., Battistella, P. A. & Clementi, M. Migraine therapy during pregnancy and lactation. Expert Opin. Drug Saf. 9, 937–948 (2010).
Banhidy, F., Acs, N., Puho, E. & Czeizel, A. E. Ergotamine treatment during pregnancy and a higher rate of low birthweight and preterm birth. Br. J. Clin. Pharmacol. 64, 510–516 (2007).
Schulman, E. A. & Dermott, K. F. Sumatriptan plus metoclopramide in triptan-nonresponsive migraineurs. Headache 43, 729–733 (2003).
MacGregor, E. A. Anti-emetics. Curr. Med. Res. Opin. 17 (Suppl. 1), S22–S25 (2001).
Pasternak, B., Svanstrom, H., Molgaard-Nielsen, D., Melbye, M. & Hviid, A. Metoclopramide in pregnancy and risk of major congenital malformations and fetal death. JAMA 310, 1601–1611 (2013).
[No authors listed] Domperidone: QT prolongation in infants. Prescrire Int. 20, 14 (2011).
Holland, S. et al. Evidence-based guideline update: NSAIDs and other complementary treatments for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology 78, 1346–1353 (2012).
Silberstein, S. D. et al. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology 78, 1337–1345 (2012).
Yakoob, M. Y. et al. The risk of congenital malformations associated with exposure to beta-blockers early in pregnancy: a meta-analysis. Hypertension 62, 375–381 (2013).
Bateman, B. T. et al. Chronic hypertension in pregnancy and the risk of congenital malformations: a cohort study. Am. J. Obstet. Gynecol. 212, 337.e1–337.e14.
MacGregor, E. A. Headache in pregnancy. Continuum (Minneap. Minn.) 20, 128–147 (2014).
Wadelius, M., Darj, E., Frenne, G. & Rane, A. Induction of CYP2D6 in pregnancy. Clin. Pharmacol. Ther. 62, 400–407 (1997).
Meador, K. J. et al. Fetal antiepileptic drug exposure and cognitive outcomes at age 6 years (NEAD study): a prospective observational study. Lancet Neurol. 12, 244–252 (2013).
Christensen, J. et al. Prenatal valproate exposure and risk of autism spectrum disorders and childhood autism. JAMA 309, 1696–1703 (2013).
Banach, R., Boskovic, R., Einarson, T. & Koren, G. Long-term developmental outcome of children of women with epilepsy, unexposed or exposed prenatally to antiepileptic drugs: a meta-analysis of cohort studies. Drug Saf. 33, 73–79 (2010).
European Medicines Agency. CMDh agrees to strengthen warnings on the use of valproate medicines in women and girls. European Medicines Agency news and press release archive [online], (2014).
Mines, D. et al. Topiramate use in pregnancy and the birth prevalence of oral clefts. Pharmacoepidemiol. Drug Saf. 23, 1017–1025 (2014).
Margulis, A. V. et al. Use of topiramate in pregnancy and risk of oral clefts. Am. J. Obstet. Gynecol. 207, 405.e1–405.e7 (2012).
Hernandez-Diaz, S. et al. Association between topiramate and zonisamide use during pregnancy and low birth weight. Obstet. Gynecol. 123, 21–28 (2014).
Palmsten, K. et al. Antidepressant use and risk for preeclampsia. Epidemiology 24, 682–691 (2013).
Källén, B. Neonate characteristics after maternal use of antidepressants in late pregnancy. Arch. Pediatr. Adolesc. Med. 158, 312–316 (2004).
Pringsheim, T. et al. Canadian Headache Society guideline for migraine prophylaxis. Can. J. Neurol. Sci. 39 (Suppl. 2), S1–S59 (2012).
[No authors listed] ACE inhibitors, angiotensin II receptor blockers and pregnancy: fetal renal impairment. Prescrire Int. 22, 243 (2013).
Bullo, M., Tschumi, S., Bucher, B. S., Bianchetti, M. G. & Simonetti, G. D. Pregnancy outcome following exposure to angiotensin-converting enzyme inhibitors or angiotensin receptor antagonists: a systematic review. Hypertension 60, 444–450 (2012).
Cooper, W. O. et al. Major congenital malformations after first-trimester exposure to ACE inhibitors. N. Engl. J. Med. 354, 2443–2451 (2006).
Tan, M., Kim, E., Koren, G. & Bozzo, P. Botulinum toxin type A in pregnancy. Can. Fam. Physician 59, 1183–1184 (2013).
Robinson, A. Y. & Grogan, P. M. OnabotulinumtoxinA successfully used as migraine prophylaxis during pregnancy: a case report. Mil. Med. 179, e703–e704 (2014).
Doyle, L. W., Anderson, P. J., Haslam, R., Lee, K. J. & Crowther, C. School-age outcomes of very preterm infants after antenatal treatment with magnesium sulfate vs placebo. JAMA 312, 1105–1113 (2014).
Gartner, L. M. et al. Breastfeeding and the use of human milk. Pediatrics 115, 496–506 (2005).
Hale, T. W. (ed.) Medications and Mothers' Milk: A Manual of Lactational Pharmacology 16th edn (Hale Publishing, 2014).
Bitzen, P. O., Gustafsson, B., Jostell, K. G., Melander, A. & Wahlin-Boll, E. Excretion of paracetamol in human breast milk. Eur. J. Clin. Pharmacol. 20, 123–125 (1981).
Spigset, O. & Hägg, S. Analgesics and breast-feeding: safety considerations. Paediatr. Drugs 2, 223–238 (2000).
Matheson, I., Lunde, P. K. & Notarianni, L. Infant rash caused by paracetamol in breast milk? Pediatrics 76, 651–652 (1985).
Davanzo, R., Bua, J., Paloni, G. & Facchina, G. Breastfeeding and migraine drugs. Eur. J. Clin. Pharmacol. 70, 1313–1324 (2014).
Terragna, A. & Spirito, L. Thrombocytopenic purpura in an infant after administration of acetylsalicylic acid to the wet-nurse. Minerva Pediatr. 19, 613–616 (1967).
Wojnar-Horton, R. E. et al. Distribution and excretion of sumatriptan in human milk. Br. J. Clin. Pharmacol. 41, 217–221 (1996).
U. S. Food and Drug Administration. Label information Imitrex. Drugs @ FDA: FDA approved drug products [online], (2013).
David, P., Kling, J. & Starling, A. Migraine in pregnancy and lactation. Curr. Neurol. Neurosci. Rep. 14, 1–6 (2014).
Koren, G., Cairns, J., Chitayat, D., Gaedigk, A. & Leeder, S. J. Pharmacogenetics of morphine poisoning in a breastfed neonate of a codeine-prescribed mother. Lancet 368, 704 (2006).
Madadi, P. et al. Guidelines for maternal codeine use during breastfeeding. Can. Fam. Physician 55, 1077–1078 (2009).
Hendrickson, R. G. & McKeown, N. J. Is maternal opioid use hazardous to breast-fed infants? Clin. Toxicol. (Phila.) 50, 1–14 (2012).
Kauppila, A. et al. Metoclopramide and breast feeding: transfer into milk and the newborn. Eur. J. Clin. Pharmacol. 25, 819–823 (1983).
Bauer, J. H., Pape, B., Zajicek, J. & Groshong, T. Propranolol in human plasma and breast milk. Am. J. Cardiol. 43, 860–862 (1979).
Sandström, B. & Regårdh, C. G. Metoprolol excretion into breast milk. Br. J. Clin. Pharmacol. 9, 518–519 (1980).
Kulas, J., Lunell, N. O., Rosing, U., Steen, B. & Rane, A. Atenolol and metoprolol. A comparison of their excretion into human breast milk. Acta Obstet. Gynecol. Scand. Suppl. 118, 65–69 (1984).
Shannon, M. E., Malecha, S. E. & Cha, A. J. Beta blockers and lactation: an update. J. Hum. Lact. 16, 240–245 (2000).
Hägg, S. & Spigset, O. Anticonvulsant use during lactation. Drug Saf. 22, 425–440 (2000).
Öhman, I., Vitols, S., Luef, G., Söderfeldt, B. & Tomson, T. Topiramate kinetics during delivery, lactation, and in the neonate: preliminary observations. Epilepsia 43, 1157–1160 (2002).
Spigset, O. & Hägg, S. Excretion of psychotropic drugs into breast milk. CNS Drugs 9, 111–134 (1998).
Cruikshank, D. P., Varner, M. W. & Pitkin, R. M. Breast milk magnesium and calcium concentrations following magnesium sulfate treatment. Am. J. Obstet. Gynecol. 143, 685–688 (1982).
Author information
Authors and Affiliations
Contributions
O.S., S.A., H.N. and K.N.-H. wrote the article. All authors researched data for the article, provided substantial contribution to discussion of content and reviewed/edited manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
L.J.S. has received a speaker's fee from GlaxoSmithKline. The other authors declare no competing interests.
Supplementary information
Supplementary Table 1
Overview of observational studies on associations of NSAID exposure in the first trimester and miscarriage and congenital malformations (DOCX 44 kb)
Supplementary Table 2
Overview of observational studies on associations of NSAID exposure in the second and/or third trimester and other pregnancy outcomes (DOCX 31 kb)
Supplementary Table 3
Overview of observational studies on associations of triptan exposure during pregnancy and adverse pregnancy outcomes (DOCX 34 kb)
Supplementary further reading
Recommended resources on safety of medications during pregnancy and lactation (DOCX 22 kb)
PowerPoint slides
Rights and permissions
About this article
Cite this article
Amundsen, S., Nordeng, H., Nezvalová-Henriksen, K. et al. Pharmacological treatment of migraine during pregnancy and breastfeeding. Nat Rev Neurol 11, 209–219 (2015). https://doi.org/10.1038/nrneurol.2015.29
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2015.29
This article is cited by
-
Migräne und Schwangerschaft
Der Nervenarzt (2024)
-
Acute Treatment of Migraine: Expert Consensus Statements from the United Arab Emirates (UAE)
Neurology and Therapy (2024)
-
The Role of the Combination Paracetamol/Caffeine in Treatment of Acute Migraine Pain: A Narrative Review
Pain and Therapy (2024)
-
Health equity, care access and quality in headache – part 2
The Journal of Headache and Pain (2023)
-
A systematic review and meta-analyses on the prevalence of pregnancy outcomes in migraine treated patients: a contribution from the IMI2 ConcePTION project
Journal of Neurology (2022)