Abstract
The pathological process underlying amyotrophic lateral sclerosis (ALS) is associated with the formation of cytoplasmic inclusions consisting mainly of phosphorylated 43-kDa transactive response DNA-binding protein (pTDP-43), which plays an essential part in the pathogenesis of ALS. Preliminary evidence indicates that neuronal involvement progresses at different rates, but in a similar sequence, in different patients with ALS. This observation supports the emerging concept of prion-like propagation of abnormal proteins in noninfectious neurodegenerative diseases. Although the distance between involved regions is often considerable, the affected neurons are connected by axonal projections, indicating that physical contacts between nerve cells along axons are important for dissemination of ALS pathology. This article posits that the trajectory of the spreading pattern is consistent with the induction and dissemination of pTDP-43 pathology chiefly from cortical neuronal projections, via axonal transport, through synaptic contacts to the spinal cord and other regions of the brain.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Halliday, G., Hely, M., Reid, W. & Morris, J. The progress of pathology in longitudinally followed patients with Parkinson's disease. Acta Neuropathol. 115, 409–415 (2008).
Savica, R., Rocca, W. A. & Ahlskog, J. E. When does Parkinson disease start? Arch. Neurol. 67, 798–801 (2010).
Kiernan, M. C. et al. Amyotrophic lateral sclerosis. Lancet 377, 942–955 (2011).
Nakano, T., Nakaso, K., Nakashima, K. & Ohama, E. Expression of ubiquitin-binding protein p62 in ubiquitin-immunoreactive intraneuronal inclusions in amyotrophic lateral sclerosis with dementia: analysis of five autopsy cases with broad clinicopathological spectrum. Acta Neuropathol. 107, 359–364 (2004).
Neumann, M. et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science 314, 130–133 (2006).
Mackenzie, I. et al. Pathological TDP-43 distinguishes sporadic amyotrophic lateral sclerosis from amyotrophic lateral sclerosis with SOD1 mutations. Ann. Neurol. 61, 427–434 (2007).
Lee, E. B., Lee, V. M. & Trojanowski, J. Q. Gains or losses: molecular mechanisms of TDP43-mediated neurodegeneration. Nat. Rev. Neurosci. 13, 38–50 (2011).
Aguzzi, A. & Rajendran, L. The transcellular spread of cytosolic amyloids, prions, and prionoids. Neuron 64, 783–790 (2009).
Lee, S. J., Desplats, P., Sigurdson, C., Tsigelny, I. & Masliah, E. Cell-to-cell transmission of non-prion protein aggregates. Nat. Rev. Neurol. 6, 702–706 (2010).
Kanouchi, T., Ohkubo, T. & Yokota, T. Can regional spreading of amyotrophic lateral sclerosis motor symptoms be explained by prion-like propagation? J. Neurol. Neurosurg. Psychiatry 83, 739–745 (2012).
Kfoury, H., Holmes, B. B., Holtzman, D. M. & Diamond, M. I. Trans-cellular propagation of tau aggregation by fibrillar species. J. Biol. Chem. 287, 19440–19451 (2012).
Lee, S., Kim, W., Li, Z. & Hall, G. F. Accumulation of vesicle-associated human tau in distal dendrites drives degeneration and tau secretion in an in situ cellular tauopathy model. Int. J. Alzheimers Dis. 2012, 172837 (2012).
Constanzo, M. & Zurzolo, C. The cell biology of prion-like spread of protein aggregates: mechanisms and implication in neurodegeneration. Biochem. J. 452, 1–17 (2013).
Dunning, C. J., George, S. & Brundin, P. What's to like about the prion-like hypothesis for the spreading of aggregated α-synuclein in Parkinson disease? Prion 7, 92–97 (2013).
Jucker, M. & Walker, L. C. Self-propagation of pathogenic protein aggregates in neurodegenerative diseases. Nature 501, 45–51 (2013).
Nonaka, T. et al. Prion-like properties of pathological TDP-43 aggregates from diseased brains. Cell Rep. 4, 124–134 (2013).
Ravits, J. M. & La Spada, A. R. ALS motor phenotype heterogeneity, focality, and spread: deconstructing motor neuron degeneration. Neurology 73, 805–811 (2009).
Ravits, J., Laurie, P., Fan, Y. & Moore, D. H. Implications of ALS focality: rostral-caudal distribution of lower motor neuron loss postmortem. Neurology 68, 1576–1582 (2007).
Sekiguchi, T. et al. Spreading of amyotrophic lateral sclerosis lesions–multifocal hits and local propagation? J. Neurol. Neurosurg. Psychiatry http://dx.doi.org/10.1136/jnnp-2013-305617.
Ravits, J., Paul, P. & Jorg, C. Focality of upper and lower motor neuron degeneration at the clinical onset of ALS. Neurology 68, 1571–1575 (2007).
Brettschneider, J. et al. Stages of pTDP-43 pathology in amyotrophic lateral sclerosis. Ann. Neurol. 74, 20–38 (2013).
Saper, C. B., Wainer, B. H. & German, D. C. Axonal and transneuronal transport in the transmission of neurological disease: potential role of system degenerations, including Alzheimer's disease. Neuroscience 23, 389–398 (1987).
Brooks, B. R. The role of axonal transport in neurodegenerative disease spread: a meta-analysis of experimental and clinical poliomyelitis compares with amyotrophic lateral sclerosis. Can. J. Neurol. Sci. 18 (Suppl. 3), 435–438 (1991).
Braak, H., Rüb, U., Gai, W. P. & Del Tredici, K. Idiopathic Parkinson's disease: possible routes by which vulnerable neuronal types may be subject to neuroinvasion by an unknown pathogen. J. Neural Transm. 110, 517–536 (2003).
Fallini, C., Bassell, G. J. & Rossoll, W. The ALS disease protein TDP-43 is actively transported in motor neuron axons and regulates axon outgrowth. Hum. Mol. Genet. 21, 3703–3718 (2012).
Luk, K. C. et al. Intracerebral inoculation of pathological α-synuclein initiates a rapidly progressive neurodegenerative α-synucleinopathy in mice. J. Exp. Med. 209, 975–986 (2012).
Pan-Montojo, F. et al. Environmental toxins trigger PD-like progression via increased alpha-synuclein release from enteric neurons in mice. Sci. Rep. 2, 898 (2012).
Iba, M. et al. Synthetic tau fibrils mediate transmission of neurofibrillary tangles in a transgenic mouse model of Alzheimer's-like tauopathy. J. Neurosci. 33, 1024–1037 (2013).
Ulusoy, A. et al. Caudo-rostral brain spreading of α-synuclein through vagal connections. EMBO Mol. Med. 5, 1051–1059 (2013).
Wu, J. W. et al. Small misfolded tau species are internalized via bulk endocytosis and anterogradely and retrogradely transported in neurons. J. Biol. Chem. 288, 1856–1870 (2013).
Zhou, F. M., Wilson, C. J. & Dani, J. A. Cholinergic interneuron characteristics and nicotinic properties in the striatum. J. Neurobiol. 53, 590–605 (2002).
Smith, M. C. Nerve fibre degeneration in the brain in amyotrophic lateral sclerosis. J. Neurol. Neurosurg. Psychiatry 23, 269–282 (1960).
Ludolph, A. C. et al. Frontal lobe function in amyotrophic lateral sclerosis: a neuropsychologic and positron emission tomography study. Acta Neurol. Scand. 85, 81–89 (1992).
Piao, Y. S. et al. Neuropathology with clinical correlations of sporadic amyotrophic lateral sclerosis: 102 autopsy cases examined between 1962 and 2000. Brain Pathol. 13, 10–22 (2003).
Geser, F., Lee, V. M. & Trojanowski, J. Q. Amyotrophic lateral sclerosis and frontotemporal lobar degeneration: a spectrum of TDP-43 proteinopathies. Neuropathology 30, 103–112 (2010).
Schreiber, H. et al. Cognitive function in bulbar- and spinal-onset amyotrophic lateral sclerosis. A longitudinal study in 52 patients. J. Neurol. 252, 772–781 (2005).
van der Graaff, M. M. et al. Upper and extra-motoneuron involvement in early motoneuron disease: a diffusor tensor imaging study. Brain 134, 1211–1228 (2011).
Heise, C. & Kayalioglu, G. in The Spinal Cord: A Christopher and Dana Reeve Foundation Text and Atlas 1st edn Vol. 1 Ch. 6 (eds Watson, C. et al.) 64–93 (Academic Press, 2009).
Horn, A. K. & Leigh, R. J. The anatomy and physiology of the ocular motor system. Handb. Clin. Neurol. 102, 21–69 (2011).
Aston-Jones, G. & Cohen, J. D. Adaptive gain and the role of the locus coeruleus-norepinephrine system in optimal performance. J. Comp. Neurol. 493, 99–110 (2005).
Holstege, G. The mesopontine rostromedial tegmental nucleus and the emotional motor system: role in basic survival behavior. J. Comp. Neurol. 513, 559–565 (2009).
Braak, H. et al. Staging of brain pathology related to sporadic Parkinson's disease. Neurobiol. Aging 24, 197–211 (2003).
Braak, H. & Del Tredici, K. Where, when, and in what form does sporadic Alzheimer's disease begin? Curr. Opin. Neurol. 25, 708–714 (2012).
Sengul, G. & Watson, C. in The Human Nervous System 3rd edn Vol. 1 Ch. 7 (eds Mai, J. K. & Paxinos, G.) 233–258 (Academic Press, 2012).
Braak, H., Rüb, U. & Del Tredici, K. Involvement of precerebellar nuclei in multiple system atrophy. Neuropathol. Appl. Neurobiol. 29, 60–76 (2003).
Saint-Cyr, J. A. The projection from the motor cortex to the inferior olive in the cat. An experimental study using axonal transport techniques. Neuroscience 10, 667–684 (1983).
Burman, K., Darien-Smith, C. & Darien-Smith, I. Macaque red nucleus: origins of spinal and olivary projections and terminations of cortical inputs. J. Comp. Neurol. 423, 179–196 (2000).
Habas, C. & Cabanis, E. A. Cortical projections to the human red nucleus: a diffusion tensor tractography study with a 1.5-T MRI machine. Neuroradiology 48, 755–762 (2006).
Zhang, H. et al. TDP-43 immunoreactive neuronal and glial inclusions in the neostriatum in amyotrophic lateral sclerosis with and without dementia. Acta Neuropathol. 115, 115–122 (2008).
Jones, E. G., Coulter, J. D., Burton, H. & Porter, R. Cells of origin and terminal distribution of corticostriatal fibers arising in the sensory-motor cortex of monkeys. J. Comp. Neurol. 173, 53–80 (1977).
Haber, S. N., Adler, A. & Bergmann, H. in The Human Nervous System, 3rd edn Vol. 1 Ch. 20 (eds Mai, J. K. & Paxinos, G.) 678–738 (Academic Press, 2012).
Jones, E. G. Thalamic organization and function after Cajal. Prog. Brain Res. 136, 333–357 (2002).
Behrens, T. E. et al. Non-invasive mapping of connections between human thalamus and cortex using diffusion imaging. Nat. Neurosci. 6, 750–757 (2003).
Briggs, F. & Usrey, W. M. Emerging views of corticothalamic function. Curr. Opin. Neurobiol. 18, 403–407 (2008).
Braak, H. Architectonics of the Human Telencephalic Cortex (Studies of Brain Functions) Vol. 4 (Springer, 1980).
Wightman, G. et al. Hippocampal and neocortical ubiquitin-immunoreactive inclusions in amyotrophic lateral sclerosis with dementia. Neurosci. Lett. 139, 269–274 (1992).
Braak, H., Braak, E., Yilmazer, D. & Bohl, J. Functional anatomy of human hippocampal formation and related structures. J. Child. Neurol. 11, 265–275 (1996).
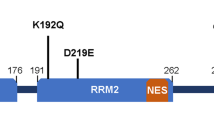
Ayala, Y. M. et al. Structural determinants of the cellular localization and shuttling of TDP-43. J. Cell Sci. 121, 3778–3785 (2008).
Giordana, M. T. et al. TDP-43 redistribution is an early event in sporadic amyotrophic lateral sclerosis. Brain Pathol. 20, 351–360 (2010).
Ling, S. C., Polymenidou, M. & Cleveland, D. W. Converging mechanisms in ALS and FTD: disrupted RNA and protein homeostasis. Neuron 79, 416–438 (2013).
Guo, Y. et al. HO-1 induction in motor cortex and intestinal dysfunction in TDP-43 A315T transgenic mice. Brain Res. 1460, 388–495 (2012).
Arnold, E. S. et al. ALS-linked TDP-43 mutations produce aberrant RNA splicing and adult-onset motor neuron disease without aggregation or loss of nuclear TDP-43. Proc. Natl Acad. Sci. USA 110, E736–E745 (2013).
Esmaeili, M. A., Panahi, M., Yadav, S., Hennings, L. & Kiaei, M. Premature death of TDP-43 (A315T) transgenic mice due to gastrointestinal complications prior to development of full neurological symptoms of amyotrophic lateral sclerosis. Int. J. Exp. Pathol. 94, 56–64 (2013).
Chiang, P.-M. et al. Deletion of TDP-43 down-regulates Tbc1d1, a gene linked to obesity, and alters body fat metabolism. Proc. Natl Acad. Sci. USA 107, 16320–16324 (2010).
Kraemer, B. C. et al. Loss of murine TDP-43 disrupts motor function and plays an essential role in embryogenesis. Acta Neuropathol. 119, 409–419 (2010).
Igaz, L. M. et al. Dysregulation of the ALS-associated gene TDP-43 leads to neuronal death and degeneration in mice. J. Clin. Invest. 121, 726–738 (2011).
Wils, H. et al. TDP-43 transgenic mice develop spastic paralysis and neuronal inclusions characteristic of ALS and frontotemporal lobar degeneration. Proc. Natl Acad. Sci. USA 107, 3858–3863 (2010).
Mackenzie, I. R. et al. A harmonized classification system for FTLD-TDP pathology. Acta Neuropathol. 122, 111–113 (2011).
Acknowledgements
The authors' research was made possible by grants from the Wyncote Foundation, the Koller Family Foundation, NIH grants AG033101, AG017586, AG010124, AG032953, AG039510, and NS044266 (V. M. Lee, J. Q. Trojanowski), as well as the Deutsche Forschungsgemeinschaft grant number TR 1000/1-1 (H. Braak, K. Del Tredici). The authors thank D. Ewert (University of Ulm) for assistance with preparation of the original artwork.
Author information
Authors and Affiliations
Contributions
H. Braak researched the data for the article. All authors made substantial contribution to discussion of the article content, to writing of the article, and to review and/or editing of the manuscript prior to submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Table 1
Main types of nerve cells susceptible to development of pTDP-43 pathology in ALS (DOC 34 kb)
Supplementary Table 2
Neuronal types that develop no or very mild pTDP-43 pathology in ALS (DOC 30 kb)
Rights and permissions
About this article
Cite this article
Braak, H., Brettschneider, J., Ludolph, A. et al. Amyotrophic lateral sclerosis—a model of corticofugal axonal spread. Nat Rev Neurol 9, 708–714 (2013). https://doi.org/10.1038/nrneurol.2013.221
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2013.221
This article is cited by
-
Choroid plexus enlargement in amyotrophic lateral sclerosis patients and its correlation with clinical disability and blood-CSF barrier permeability
Fluids and Barriers of the CNS (2024)
-
Cognitive function in amyotrophic lateral sclerosis: a cross-sectional and prospective pragmatic clinical study with review of the literature
Neurological Sciences (2024)
-
Guideline “Motor neuron diseases” of the German Society of Neurology (Deutsche Gesellschaft für Neurologie)
Neurological Research and Practice (2023)
-
Neuronal dysfunction caused by FUSR521G promotes ALS-associated phenotypes that are attenuated by NF-κB inhibition
Acta Neuropathologica Communications (2023)
-
Patterns of synaptic loss in human amyotrophic lateral sclerosis spinal cord: a clinicopathological study
Acta Neuropathologica Communications (2023)