Abstract
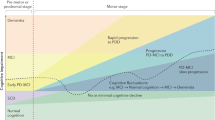
Optimal management of chronic diseases not only requires tackling of the primary disease processes, but also necessitates timely recognition and treatment of comorbid conditions. In this article, we illustrate this two-pronged approach for two common age-related disorders: Parkinson disease (PD) and cerebrovascular disease (CVD). We first discuss the pathophysiological mechanisms that could provide a link between PD and CVD. Patients with PD have a series of risk factors that could promote development of CVD, but also have several protective factors. We then review the available clinical, radiological and neuropathological evidence to support an association between these two conditions. We conclude by discussing the potential implications for clinical practice, highlighting how comorbid CVD could alter the clinical presentation of PD and reviewing the possibilities for prevention and secondary prophylaxis. Additional research will be needed to fully evaluate the prevalence and clinical relevance of comorbid CVD in PD. Pending further evidence, we recommend that cerebral neuroimaging should be considered if patients with initially uncomplicated PD develop—either acutely or chronically—prominent and/or treatment-resistant gait impairment, postural instability, depression, cognitive decline, or urinary incontinence. Finding comorbid CVD in such patients could have prognostic implications, and could necessitate treatment to arrest further progression of CVD.
Key Points
-
Patients with Parkinson disease (PD) could have an increased risk of developing comorbid cerebrovascular disease (CVD), although systematic research is lacking
-
The pathophysiology underlying the relationship between PD and CVD is complex and multifactorial, with both risk factors and protective mechanisms at play
-
Comorbid CVD usually presents not as overt acute stroke, but by producing or exacerbating symptoms such as postural instability, gait impairment, falls, depression, cognitive decline, or urinary incontinence
-
Neuroimaging should be considered when patients with PD develop any of these symptoms, particularly early in the disease process
-
If patients with PD develop a clinically manifest transient ischemic attack or ischemic stroke, they should be treated according to established protocols for these conditions
-
Additional well-designed and adequately powered studies are required to improve our understanding of the relationship between PD and CVD, as well as the possible therapeutic consequences
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Langston, J. W. The Parkinson's complex: parkinsonism is just the tip of the iceberg. Ann. Neurol. 59, 591–596 (2006).
Feinstein, A. The pre-therapeutic classification of comorbidity in chronic disease. J. Chron. Dis. 23, 455–468 (1970).
van Eijkeren, F. J. et al. Nordic walking improves mobility in Parkinson's disease. Mov. Disord. 23, 2239–2243 (2008).
Kadoglou, N. P., Iliadis, F. & Liapis, C. Exercise and carotid atherosclerosis. Eur. J. Vasc Endovasc. Surg. 35, 264–272 (2008).
Alves, G., Kurz, M., Lie, S. A. & Larsen, J. P. Cigarette smoking in Parkinson's disease: influence on disease progression. Mov. Disord. 19, 1087–1092 (2004).
Zijlmans, J. C., Daniel, S. E., Hughes, A. J., Révész, T. & Lees, A. J. Clinicopathological investigation of vascular parkinsonism, including clinical criteria for diagnosis. Mov. Disord. 19, 630–640 (2004).
Gelb, D. J., Oliver, E. & Gilman, S. Diagnostic criteria for Parkinson disease. Arch. Neurol. 56, 33–39 (1999).
Solfrizzi, V. et al. Vascular risk factors, incidence of MCI, and rates of progression to dementia. Neurology 63, 1882–1891 (2004).
Struck, L. K., Rodnitzky, R. L. & Dobson, J. K. Stroke and its modification in Parkinson's disease. Stroke 21, 1395–1399 (1990).
Marttila, R. J. & Rinne, U. K. Smoking and Parkinson's disease. Acta Neurol. Scand. 62, 322–325 (1980).
Nataraj, A. & Rajput, A. H. Parkinson's disease, stroke, and related epidemiology. Mov. Disord. 20, 1476–1480 (2005).
van Dijk, E. J. et al. Progression of cerebral small vessel disease in relation to risk factors and cognitive consequences: Rotterdam Scan study. Stroke 39, 2712–2719 (2008).
Longstreth, W. T. Jr, et al. Incidence, manifestations, and predictors of worsening white matter on serial cranial magnetic resonance imaging in the elderly: the Cardiovascular Health Study. Stroke 36, 56–61 (2005).
Wolf, P. A., D'Agostino, R. B., Kannel, W. B., Bonita, R. & Belanger, A. J. Cigarette smoking as a risk factor for stroke. The Framingham Study. JAMA 259, 1025–1029 (1988).
Howard, G. et al. Cigarette smoking and other risk factors for silent cerebral infarction in the general population. Stroke 29, 913–917 (1998).
Howard, G. et al. Cigarette smoking and progression of atherosclerosis: The Atherosclerosis Risk in Communities (ARIC) Study. JAMA 279, 119–124 (1998).
Swan, G. E. & Lessov-Schlaggar, C. N. The effects of tobacco smoke and nicotine on cognition and the brain. Neuropsychol. Rev. 17, 259–273 (2007).
Scigliano, G., Ronchetti, G., Girotto, F. & Musicco, M. Sympathetic modulation by levodopa reduces vascular risk factors in Parkinson disease. Parkinsonism Relat. Disord. 15, 138–143 (2009).
Laverty, R. Catecholamines: role in health and disease. Drugs 16, 418–440 (1978).
Bouhaddi, M. et al. Impaired cardiovascular autonomic control in newly and long-term-treated patients with Parkinson's disease: involvement of L-dopa therapy. Auton. Neurosci. 116, 30–38 (2004).
Iwasaki, S., Hamaguchi, K., Iwasaki, A., Takakusagi, M. & Narabayashi, Y. Hypotensive effect of long-term levodopa in patients with Parkinson's disease. Eur. Neurol. 30, 194–199 (1990).
Saito, I. et al. Effect of L-dopa in young patients with hypertension. Angiology 42, 691–695 (1991).
van Dijk, J. G. et al. Autonomic nervous system dysfunction in Parkinson's disease: relationships with age, medication, duration, and severity. J. Neurol. Neurosurg. Psychiatry 56, 1090–1095 (1993).
Durrieu, G. et al. Blood pressure and plasma catecholamines in never-treated parkinsonian patients: effect of a selective D1 agonist (CY 208–243). Neurology 40, 707–709 (1990).
Mannelli, M. et al. In vivo evidence that endogenous dopamine modulates sympathetic activity in man. Hypertension 34, 398–402 (1999).
Low, P. A. & Singer, W. Management of neurogenic orthostatic hypotension: an update. Lancet Neurol. 7, 451–458 (2008).
Shannon, J. R. et al. Sympathetically mediated hypertension in autonomic failure. Circulation 101, 2710–2715 (2000).
Goldstein, D. S., Pechnik, S., Holmes, C., Eldabah, B. & Sharabi, Y. Association between supine hypertension and orthostatic hypotension in autonomic failure. Hypertension 42, 136–142 (2003).
Schoenberger, J. A. Drug-induced orthostatic hypotension. Drug Saf. 6, 402–407 (1991).
Senard, J. M., Brefel-Courbon, C., Rascol, O. & Montastruc, J. L. Orthostatic hypotension in patients with Parkinson's disease: pathophysiology and management. Drugs Aging 18, 495–505 (2001).
Verhaeverbeke, I. & Mets, T. Drug-induced orthostatic hypotension in the elderly: avoiding its onset. Drug Saf. 17, 105–118 (1997).
Lees, A. Alternatives to levodopa in the initial treatment of early Parkinson's disease. Drugs Aging 22, 731–740 (2005).
de Leeuw, F. E. et al. Hypertension and cerebral white matter lesions in a prospective cohort study. Brain 125, 765–772 (2002).
Eigenbrodt, M. L. et al. Orthostatic hypotension as a risk factor for stroke: the atherosclerosis risk in communities (ARIC) study, 1987–1996. Stroke 31, 2307–2313 (2000).
Manolio, T. A., Kronmal, R. A., Burke, G. L., O'Leary, D. H. & Price, T. R. Short-term predictors of incident stroke in older adults. The Cardiovascular Health Study. Stroke 27, 1479–1486 (1996).
Marcus, B. H. et al. Physical activity intervention studies: what we know and what we need to know: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity); Council on Cardiovascular Disease in the Young; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Circulation 114, 2739–2752 (2006).
Warburton, D. E., Nicol, C. W. & Bredin, S. S. Health benefits of physical activity: the evidence. CMAJ 174, 801–809 (2006).
Fertl, E., Doppelbauer, A. & Auff, E. Physical activity and sports in patients suffering from Parkinson's disease in comparison with healthy seniors. J. Neural Transm. Park. Dis. Dement. Sect. 5, 157–161 (1993).
Toth, M. J., Fishman, P. S. & Poehlman, E. T. Free-living daily energy expenditure in patients with Parkinson's disease. Neurology 48, 88–91 (1997).
Wendel-Vos, G. C. et al. Physical activity and stroke. A meta-analysis of observational data. Int. J. Epidemiol. 33, 787–798 (2004).
Haapanen, N., Miilunpalo, S., Vuori, I., Oja, P. & Pasanen, M. Association of leisure time physical activity with the risk of coronary heart disease, hypertension and diabetes in middle-aged men and women. Int. J. Epidemiol. 26, 739–747 (1997).
Kenangil, G., Ozekmekçi, S., Koldas, L., Sahin, T. & Erginöz, E. Assessment of valvulopathy in Parkinson's disease patients on pergolide and/or cabergoline. Clin. Neurol. Neurosurg. 109, 350–353 (2007).
Kim, J. Y., Chung, E. J., Park, S. W. & Lee, W. Y. Valvular heart disease in Parkinson's disease treated with ergot derivative dopamine agonists. Mov. Disord. 21, 1261–1264 (2006).
Dewey, R. B. 2nd, Reimold, S. C. & O'Suilleabhain, P. E. Cardiac valve regurgitation with pergolide compared with nonergot agonists in Parkinson disease. Arch. Neurol. 64, 377–380 (2007).
Van Camp, G. et al. Treatment of Parkinson's disease with pergolide and relation to restrictive valvular heart disease. Lancet 363, 1179–1183 (2004).
Schade, R., Andersohn, F., Suissa, S., Haverkamp, W. & Garbe, E. Dopamine agonists and the risk of cardiac-valve regurgitation. N. Engl. J. Med. 356, 29–38 (2007).
Zanettini, R. et al. Valvular heart disease and the use of dopamine agonists for Parkinson's disease. N. Engl. J. Med. 356, 39–46 (2007).
Antonini, A. & Poewe, W. Fibrotic heart-valve reactions to dopamine-agonist treatment in Parkinson's disease. Lancet Neurol. 6, 826–829 (2007).
Rothman, R. B. et al. Evidence for possible involvement of 5-HT(2B) receptors in the cardiac valvulopathy associated with fenfluramine and other serotonergic medications. Circulation 102, 2836–2841 (2000).
Baseman, D. G. et al. Pergolide use in Parkinson disease is associated with cardiac valve regurgitation. Neurology 63, 301–304 (2004).
Roldan, C. A., Gelgand, E. A., Qualls, C. R. & Sibbitt, W. L. Jr . Valvular heart disease as a cause of cerebrovascular disease in patients with systemic lupus erythematosus. Am. J. Cardiol. 95, 1441–1447 (2005).
Kuhn, W. et al. Elevated plasma levels of homocysteine in Parkinson's disease. Eur. Neurol. 40, 225–227 (1998).
Kuhn, W., Roebroek, R., Blom, H., van Oppenraaij, D. & Müller, T. Hyperhomocysteinaemia in Parkinson's disease. J. Neurol. 245, 811–812 (1998).
Lamberti, P. et al. Effects of levodopa and COMT inhibitors on plasma homocysteine in Parkinson's disease patients. Mov. Disord. 20, 69–72 (2005).
Lamberti, P. et al. Hyperhomocysteinemia in L-dopa treated Parkinson's disease patients: effect of cobalamin and folate administration. Eur. J. Neurol. 12, 365–368 (2005).
Müller, T., Werne, B., Fowler, B. & Kuhn, W. Nigral endothelial dysfunction, homocysteine, and Parkinson's disease. Lancet 354, 126–127 (1999).
Bottiglieri, T., Hyland, K. & Reynolds, E. H. The clinical potential of ademetionine (S-adenosylmethionine) in neurological disorders. Drugs 48, 137–152 (1994).
Chambers, J. C., Obeid, O. A. & Kooner, J. S. Physiological increments in plasma homocysteine induce vascular endothelial dysfunction in normal human subjects. Arterioscler. Thromb. Vasc. Biol. 19, 2922–2927 (1999).
Vermeer, S. E. et al. Homocysteine, silent brain infarcts, and white matter lesions: The Rotterdam Scan Study. Ann. Neurol. 51, 285–289 (2002).
Ebbing, M. et al. Mortality and cardiovascular events in patients treated with homocysteine-lowering B vitamins after coronary angiography: a randomized controlled trial. JAMA 300, 795–804 (2008).
Bonaa, K. H. et al. Homocysteine lowering and cardiovascular events after acute myocardial infarction. N. Engl. J. Med. 354, 1578–1588 (2006).
Toole, J. F. et al. Lowering homocysteine in patients with ischemic stroke to prevent recurrent stroke, myocardial infarction, and death: the Vitamin Intervention for Stroke Prevention (VISP) randomized controlled trial. JAMA 291, 565–575 (2004).
Hughes, A. J., Daniel, S. E., Kilford, L. & Lees, A. J. Accuracy of clinical diagnosis of idiopathic Parkinson's disease: a clinico-pathological study of 100 cases. J. Neurol. Neurosurg. Psychiatry 55, 181–184 (1992).
Jellinger, K. Overview of morphological changes in Parkinson's disease. Adv. Neurol. 45, 1–18 (1987).
Levine, R. L., Jones, J. C. & Bee, N. Stroke and Parkinson's disease. Stroke 23, 839–842 (1992).
Beyer, M. K., Aarsland, D., Greve, O. J. & Larsen, J. P. Visual rating of white matter hyperintensities in Parkinson's disease. Mov. Disord. 21, 223–229 (2006).
Jellinger, K. A. Prevalence of cerebrovascular lesions in Parkinson's disease. A postmortem study. Acta Neuropathol. 105, 415–419 (2003).
Mastaglia, F. L., Johnsen, R. D. & Kakulas, B. A. Prevalence of stroke in Parkinson's disease: a postmortem study. Mov. Disord. 17, 772–774 (2002).
Piccini, P. et al. White matter hyperintensities in Parkinson's disease. Clinical correlations. Arch. Neurol. 52, 191–194 (1995).
Gattellaro, G. et al. White matter involvement in idiopathic Parkinson disease: a diffusion tensor imaging study. AJNR Am. J. Neuroradiol. 30, 1222–1226 (2009).
Ben-Shlomo, Y. & Marmot, M. G. Survival and cause of death in a cohort of patients with parkinsonism—possible clues to etiology. J. Neurol. Neurosurg. Psych. 58, 293–299 (1995).
Gorell, J. M., Johnson, C. C. & Rybicki, B. A. Parkinson's disease and its comorbid disorders: an analysis of Michigan mortality data, 1970 to 1990. Neurology 44, 1865–1868 (1994).
Rektor, I. et al. Vascular pathology in patients with idiopathic Parkinson's disease. Parkinsonism Relat. Disord. 15, 24–29 (2009).
Roos, R. A., Jongen, J. C. & van der Velde, E. A. Clinical course of patients with idiopathic Parkinson's disease. Mov. Disord. 11, 236–242 (1996).
Visser, M., Marinus, J., van Hilten, J. J., Schipper, R. G. & Stiggelbout, A. M. Assessing comorbidity in patients with Parkinson's disease. Mov. Disord. 19, 824–828 (2004).
Antonini, A. et al. How vascular disease affects parkinsonism: the VADO study. Mov. Disord. 21, S533 (2006).
Inzelberg, R., Bornstein, N. M., Reider, I. & Korczyn, A. D. Basal ganglia lacunes and parkinsonism. Neuroepidemiology 13, 108–112 (1994).
Papapetropoulos, S. et al. The effect of vascular disease on late onset Parkinson's disease. Eur. J. Neurol. 11, 231–235 (2004).
Bloem, B. & Bhatia, K. Basal ganglia disorders. In Clinical Disorders of Balance, Posture and Gait (Eds Bronstein, A. M. et al.) 173–206 (Arnold, London, 2004).
Aarsland, D., Tandberg, E., Larsen, J. P. & Cummings, J. L. Frequency of dementia in Parkinson disease. Arch. Neurol. 53, 538–542 (1996).
Singer, C. Urinary dysfunction in Parkinson's disease. Clin. Neurosci. 5, 78–86 (1998).
Rosano, C., Aizenstein, H. J., Studenski, S. & Newman, A. B. A regions-of-interest volumetric analysis of mobility limitations in community-dwelling older adults. J. Gerontol. A Biol. Sci. Med. Sci. 62, 1048–1055 (2007).
Baezner, H. et al. Association of gait and balance disorders with age-related white matter changes: the LADIS study. Neurology 70, 935–942 (2008).
Pickering, R. M. et al. A meta-analysis of six prospective studies of falling in Parkinson's disease. Mov. Disord. 22, 1892–1900 (2007).
Ebersbach, G. et al. Dysequilibrium in idiopathic Parkinson disease. The effect of cerebrovascular comorbidity [German]. Nervenarzt 73, 162–165 (2002).
Selvarajah, J. et al. Potential surrogate markers of cerebral microvascular angiopathy in asymptomatic subjects at risk of stroke. Eur. Radiol. 19, 1011–1018 (2009).
de Groot, J. C. et al. Cerebral white matter lesions and depressive symptoms in elderly adults. Arch. Gen. Psychiatry 57, 1071–1076 (2000).
Krishnan, K. R., Hays, J. C. & Blazer, D. G. MRI-defined vascular depression. Am. J. Psychiatry 154, 497–501 (1997).
Alexopoulos, G. S. et al. 'Vascular depression' hypothesis. Arch. Gen. Psychiatry 54, 915–922 (1997).
Naarding, P. et al. A study on symptom profiles of late-life depression: the influence of vascular, degenerative and inflammatory risk-indicators. J. Affect. Disord. 88, 155–162 (2005).
Tiemeier, H. Biological risk factors for late life depression. Eur. J. Epidemiol. 18, 745–750 (2003).
Haugarvoll, K., Aarsland, D., Wentzel-Larsen, T. & Larsen, J. P. The influence of cerebrovascular risk factors on incident dementia in patients with Parkinson's disease. Acta Neurol. Scand. 112, 386–390 (2005).
Rodriguez-Oroz, M. C. et al. Homocysteine and cognitive impairment in Parkinson's disease: A biochemical, neuroimaging, and genetic study. Mov. Disord. 24, 1437–1444 (2009).
Slawek, J. et al. The influence of vascular risk factors and white matter hyperintensities on the degree of cognitive impairment in Parkinson's disease. Neurol. Neurochir. Pol. 42, 505–512 (2008).
de Groot, J. C. et al. Cerebral white matter lesions and subjective cognitive dysfunction: the Rotterdam Scan Study. Neurology 56, 1539–1545 (2001).
de Groot, J. C. et al. Periventricular cerebral white matter lesions predict rate of cognitive decline. Ann. Neurol. 52, 335–341 (2002).
Miranda, B. et al. Self-perceived memory impairment and cognitive performance in an elderly independent population with age-related white matter changes. J. Neurol. Neurosurg. Psychiatry 79, 869–873 (2008).
Prins, N. D. et al. Cerebral white matter lesions and the risk of dementia. Arch. Neurol. 61, 1531–1534 (2004).
Stewart, R. et al. Neuroimaging correlates of subjective memory deficits in a community population. Neurology 70, 1601–1607 (2008).
de Leeuw, F. E., Korf, E., Barkhof, F. & Scheltens, P. White matter lesions are associated with progression of medial temporal lobe atrophy in Alzheimer disease. Stroke 37, 2248–2252 (2006).
Besson, J. A., Mutch, W. J., Smith, F. W. & Corrigan, F. M. The relationship between Parkinson's disease and dementia. A study using proton NMR imaging parameters. Br. J. Psychiatry 147, 380–382 (1985).
Hirono, N., Kitagaki, H., Kazui, H., Hashimoto, M. & Mori, E. Impact of white matter changes on clinical manifestation of Alzheimer's disease: A quantitative study. Stroke 31, 2182–2188 (2000).
Sakakibara, R., Hattori, T., Uchiyama, T. & Yamanishi, T. Urinary function in elderly people with and without leukoaraiosis: relation to cognitive and gait function. J. Neurol. Neurosurg. Psychiatry 67, 658–660 (1999).
Tarvonen-Schröder, S. et al. Clinical features of leuko-araiosis. J. Neurol. Neurosurg. Psychiatry 60, 431–436 (1996).
Bennett, D. A., Gilley, D. W., Wilson, R. S., Huckman, M. S. & Fox, J. H. Clinical correlates of high signal lesions on magnetic resonance imaging in Alzheimer's disease. J. Neurol. 239, 186–190 (1992).
Elbadawi, A. Functional anatomy of the organs of micturition. Urol. Clin. North Am. 23, 177–210 (1996).
Kuo, H. K. & Lipsitz, L. A. Cerebral white matter changes and geriatric syndromes: is there a link? J. Gerontol. A Biol. Sci. Med. Sci. 59, 818–826 (2004).
Blok, B. F., Willemsen, A. T. & Holstege, G. A PET study on brain control of micturition in humans. Brain 120, 111–121 (1997).
Blok, B. F. & Holstege, G. The central nervous system control of micturition in cats and humans. Behav. Brain Res. 92, 119–125 (1998).
Winge, K. & Fowler, C. J. Bladder dysfunction in Parkinsonism: mechanisms, prevalence, symptoms, and management. Mov. Disord. 21, 737–745 (2006).
Winge, K., Skau, A. M., Stimpel, H., Nielsen, K. K. & Werdelin, L. Prevalence of bladder dysfunction in Parkinsons disease. Neurourol. Urodyn. 25, 116–122 (2006).
Balash, Y. et al. Falls in outpatients with Parkinson's disease: frequency, impact and identifying factors. J. Neurol. 252, 1310–1315 (2005).
Sacco, R. L. et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Circulation 113, e409–e449 (2006).
Adams, R. J. et al. Update to the AHA/ASA recommendations for the prevention of stroke in patients with stroke and transient ischemic attack. Stroke 39, 1647–1652 (2008).
Bloem, B. R. et al. Idiopathic senile gait disorders are signs of subclinical disease. J. Am. Geriatr. Soc. 48, 1098–1101 (2000).
Roman, G. C. New insight into Binswanger disease. Arch. Neurol. 56, 1061–1062 (1999).
Thijs, R. D., Bloem, B. R. & van Dijk, J. G. Falls, faints, fits and funny turns. J. Neurol. 256, 155–167 (2009).
Peris, A., Martín-González, R., Valiente, E., Ruiz, A. & Vioque, J. Quality and life style as risk factors in acute cerebrovascular disease [Spanish]. Rev. Neurol. 25, 1866–1871 (1997).
Crizzle, A. M. & Newhouse, I. J. Is physical exercise beneficial for persons with Parkinson's disease? Clin. J. Sport Med. 16, 422–425 (2006).
de Goede, C. J., Keus, S. H., Kwakkel, G. & Wagenaar, R. C. The effects of physical therapy in Parkinson's disease: a research synthesis. Arch. Phys. Med. Rehabil. 82, 509–515 (2001).
Keus, S. H. et al. Evidence-based analysis of physical therapy in Parkinson's disease with recommendations for practice and research. Mov. Disord. 22, 451–460 (2007).
Baatile, J., Langbein, W. E., Weaver, F., Maloney, C. & Jost, M. B. Effect of exercise on perceived quality of life of individuals with Parkinson's disease. J. Rehabil. Res. Dev. 37, 529–534 (2000).
Reuter, I., Leone, P., Schwed, M. & Oechsner, M. Effect of Nordic walking in Parkinson's disease. Mov. Disord. 21, S567 (2006).
Dupuy, D., Lesbre, J. P., Gérard, P., Andrejak, M. & Godefroy, O. Valvular heart disease in patients with Parkinson's disease treated with pergolide. Course following treatment modifications. J. Neurol. 255, 1045–1048 (2008).
Acknowledgements
This work was supported by a ZonMw VIDI research grant (number 016.076.352) to B. R. Bloem. W. Nanhoe-Mahabier was supported by the Fred Akkerman stipend. F.-E. de Leeuw received a personal fellowship from the Dutch Brain Foundation (H04-12) and a clinical fellowship from the Netherlands Organization for Scientific Research (project no. 40-00703-97-07197).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Nanhoe-Mahabier, W., de Laat, K., Visser, J. et al. Parkinson disease and comorbid cerebrovascular disease. Nat Rev Neurol 5, 533–541 (2009). https://doi.org/10.1038/nrneurol.2009.136
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2009.136
This article is cited by
-
Exercise Made Accessible: the Merits of Community-Based Programs for Persons with Parkinson’s Disease
Current Neurology and Neuroscience Reports (2023)
-
Current Perspectives on Aerobic Exercise in People with Parkinson's Disease
Neurotherapeutics (2020)
-
Retinal vessel diameter obtained by optical coherence tomography is spared in Parkinson’s disease
International Ophthalmology (2019)
-
Neurological disorders of gait, balance and posture: a sign-based approach
Nature Reviews Neurology (2018)
-
Guidelines on the clinical use for the detection of neutralizing antibodies (NAbs) to IFN beta in multiple sclerosis therapy: report from the Italian Multiple Sclerosis Study group
Neurological Sciences (2014)