Key Points
-
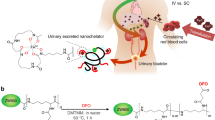
Deferasirox is an oral iron chelator with nephrotoxic potential that could result in decreased glomerular filtration requiring dialysis and in proximal tubular dysfunction
-
Although deferasirox nephrotoxicity has been reported to promote tubular cell injury, the molecular and cellular mechanisms are poorly understood
-
Postmarketing monitoring of potential long-term effects of chronic deferasirox treatment on kidney function is required
-
Careful selection and monitoring of patients treated with deferasirox might decrease the risks of serious renal adverse effects
Abstract
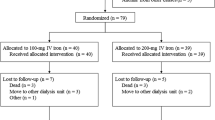
In 2005, the oral iron chelator deferasirox was approved by the FDA for clinical use as a first-line therapy for blood-transfusion-related iron overload. Nephrotoxicity is the most serious and frequent adverse effect of deferasirox treatment. This nephrotoxicity can present as an acute or chronic decrease in glomerular filtration rate (GFR). Features of proximal tubular dysfunction might also be present. In clinical trials and observational studies, GFR is decreased in 30–100% of patients treated with deferasirox, depending on dose, method of assessment and population studied. Nephrotoxicity is usually nonprogressive and/or reversible and rapid iron depletion is one of several risk factors. Scarce data are available on the molecular mechanisms of nephrotoxicity and the reasons for the specific proximal tubular sensitivity to the drug. Although deferasirox promotes apoptosis of cultured proximal tubular cells, the trigger has not been well characterized. Observational studies are required to track current trends in deferasirox prescription, assess the epidemiology of deferasirox nephrotoxicity in routine clinical practice, explore the effect on outcomes of various monitoring and dose-adjustment protocols and elucidate the long-term consequences of the different features of nephrotoxicity. Deferasirox nephrotoxicity can be more common in the elderly; thus, specific efforts should be dedicated to investigate the effect of deferasirox use in this group of patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Nick, H. et al. ICL670A: preclinical profile. Adv. Exp. Med. Biol. 509, 185–203 (2002).
Taher, A. et al. Efficacy and safety of deferasirox, an oral iron chelator, in heavily iron-overloaded patients with β-thalassaemia: the ESCALATOR study. Eur. J. Haematol. 82, 458–465 (2009).
Kwiatkowski, J. L. Real-world use of iron chelators. Hematology Am. Soc. Hematol. Educ. Program 2011, 451–458 (2011).
Food and Drug Administration. Drug Approval Package [online], (2006).
The European Medicines Agency. EPAR summary for the public [online], (2013).
Riva, A. Deferasirox's toxicity. Lancet 382, 127–128 (2013).
The European Medicines Agency. EMEA/COMP/50/02 Rev. 2 [online], (2007).
The European Medicines Agency. EPAR Product Information [online], (2014).
Vichinsky, E. et al. A randomised comparison of deferasirox versus deferoxamine for the treatment of transfusional iron overload in sickle cell disease. Br. J. Haematol. 136, 501–508 (2007).
Food and Drug Administration. Prescribing information [online], (2013).
Greenberg, P. L. et al. Prospective assessment of effects on iron-overload parameters of deferasirox therapy in patients with myelodysplastic syndromes. Leuk. Res. 34, 1560–1565 (2010).
Porter, J. et al. Relative response of patients with myelodysplastic syndromes and other transfusion-dependent anaemias to deferasirox (ICL670): a 1-yr prospective study. Eur. J. Haematol. 80, 168–176 (2008).
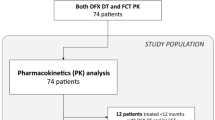
Chirnomas, D. et al. Deferasirox pharmacokinetics in patients with adequate versus inadequate response. Blood 114, 4009–4013 (2009).
Taher, A. et al. Efficacy and safety of deferasirox doses of >30 mg/kg per d in patients with transfusion-dependent anaemia and iron overload. Br. J. Haematol. 147, 752–759 (2009).
Meerpohl, J. J. et al. Deferasirox for managing iron overload in people with thalassaemia. Cochrane Database of Systematic Reviews, Issue 2. Art. No.: CD007476. http://dx.doi.org/10.1002/14651858.CD007476.pub2.
Food and Drug Administration. Important drug warning [online], (2010).
Kontoghiorghes, G. J. Turning a blind eye to deferasirox's toxicity? Lancet 381, 1183–1184 (2013).
Anapol Schwartz, LLC. FDA reports [online], (2012).
eHealthMe. Review: could Exjade cause blood creatinine increased? [online], (2014).
Food and Drug Administration. New molecular entity (NME) — early safety findings [online], (2007).
Hirschberg, R., Bennett, W., Scheinman, J., Coppo, R. & Ponticelli, C. Acute kidney injury due to deferoxamine in a renal transplant patient. Nephrol. Dial. Transplant. 23, 2704–2705 (2008).
Cappellini, M. D. et al. A phase 3 study of deferasirox (ICL670), a once-daily oral iron chelator, in patients with β-thalassemia. Blood 107, 3455–3462 (2006).
Piga, A. et al. Randomized phase II trial of deferasirox (Exjade, ICL670), a once-daily, orally-administered iron chelator, in comparison to deferoxamine in thalassemia patients with transfusional iron overload. Haematologica 91, 873–880 (2006).
Galanello, R. et al. Phase II clinical evaluation of deferasirox, a once-daily oral chelating agent, in pediatric patients with β-thalassemia major. Haematologica 91, 1343–1351 (2006).
Shemesh, O., Golbetz, H., Kriss, J. P. & Myers, B. D. Limitations of creatinine as a filtration marker in glomerulopathic patients. Kidney Int. 28, 830–838 (1985).
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney jnjury. Kidney Int. Suppl. 2, 1–138 (2012).
Rafat, C., Fakhouri, F., Ribeil, J. A., Delarue, R. & Le Quintrec, M. Fanconi syndrome due to deferasirox. Am. J. Kidney Dis. 54, 931–934 (2009).
Yew, C. T. et al. Acute interstitial nephritis secondary to deferasirox causing acute renal injury needing short-term dialysis. Nephrology (Carlton) 15, 377 (2010).
Brosnahan, G., Gokden, N. & Swaminathan, S. Acute interstitial nephritis due to deferasirox: a case report. Nephrol. Dial. Transplant. 23, 3356–3358 (2008).
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 3, 1–150 (2013).
Milat, F. et al. A case of hypophosphatemic osteomalacia secondary to deferasirox therapy. J. Bone Miner. Res. 27, 219–222 (2012).
Papadopoulos, N., Vasiliki, A., Aloizos, G., Tapinis, P. & Kikilas, A. Hyperchloremic metabolic acidosis due to deferasirox in a patient with beta thalassemia major. Ann. Pharmacother. 44, 219–221 (2010).
Baum, M. Renal Fanconi syndrome secondary to deferasirox: where there is smoke there is fire. J. Pediatr. Hematol. Oncol. 32, 525–526 (2010).
Grangé, S., Bertrand, D. M., Guerrot, D., Eas, F. & Godin, M. Acute renal failure and Fanconi syndrome due to deferasirox. Nephrol. Dial. Transplant. 25, 2376–2378 (2010).
Even-Or, E., Becker-Cohen, R. & Miskin, H. Deferasirox treatment may be associated with reversible renal Fanconi syndrome. Am. J. Hematol. 85, 132–134 (2010).
Rheault, M. N., Bechtel, H., Neglia, J. P. & Kashtan, C. E. Reversible Fanconi syndrome in a pediatric patient on deferasirox. Pediatr. Blood Cancer 56, 674–676 (2011).
Chueh, H. W. et al. Iron chelation treatment with deferasirox prior to high-dose chemotherapy and autologous stem cell transplantation may reduce the risk of hepatic veno-occlusive disease in children with high-risk solid tumors. Pediatr. Blood Cancer 58, 441–447 (2012).
Dubourg, L. et al. Deferasirox-induced renal impairment in children: an increasing concern for pediatricians. Pediatr. Nephrol. 27, 2115–2122 (2012).
Wei, H. Y., Yang, C. P., Cheng, C. H. & Lo, F. S. Fanconi syndrome in a patient with β-thalassemia major after using deferasirox for 27 months. Transfusion 51, 949–954 (2011).
Yacobovich, J. et al. Acquired proximal renal tubular dysfunction in β-thalassemia patients treated with deferasirox. J. Pediatr. Hematol. Oncol. 32, 564–567 (2010).
Yusuf, B., McPhedran, P. & Brewster, U. C. Hypocalcemia in a dialysis patient treated with deferasirox for iron overload. Am. J. Kidney Dis. 52, 587–590 (2008).
European Medicines Agency. Scientific discussion [online], (2006).
Vichinsky, E. et al. Efficacy and safety of deferasirox compared with deferoxamine in sickle cell disease: Two-year results including pharmacokinetics and concomitant hydroxyurea. Am. J. Hematol. 88, 1068–1073 (2013).
European Medicines Agency. Assessment report [online], (2013).
Cancado, R. et al. Two-year analysis of efficacy and safety of deferasirox treatment for transfusional iron overload in sickle cell anemia patients. Acta Haematol. 128, 113–118 (2012).
Cappellini, M. D. et al. Iron chelation with deferasirox in adult and pediatric patients with thalassemia major: efficacy and safety during 5 years' follow-up. Blood 118, 884–893 (2011).
Gattermann, N. et al. Deferasirox in iron-overloaded patients with transfusion-dependent myelodysplastic syndromes: Results from the large 1-year EPIC study. Leuk. Res. 34, 1143–1150 (2010).
Kennedy, G. A. et al. A prospective phase II randomized study of deferasirox to prevent iatrogenic iron overload in patients undertaking induction/consolidation chemotherapy for acute myeloid leukaemia. Br. J. Haematol. 161, 794–801 (2013).
Lee, J. W. et al. Iron chelation therapy with deferasirox in patients with aplastic anemia: a subgroup analysis of 116 patients from the EPIC trial. Blood 116, 2448–2454 (2010).
List, A. F. et al. Deferasirox reduces serum ferritin and labile plasma iron in RBC transfusion-dependent patients with myelodysplastic syndrome. J. Clin. Oncol. 30, 2134–2139 (2012).
Metzgeroth, G. et al. Deferasirox in MDS patients with transfusion-caused iron overload—a phase-II study. Ann. Hematol. 88, 301–310 (2009).
Miyazawa, K. et al. A safety, pharmacokinetic and pharmacodynamic investigation of deferasirox (Exjade, ICL670) in patients with transfusion-dependent anemias and iron-overload: a phase I study in Japan. Int. J. Hematol. 88, 73–81 (2008).
Nolte, F. et al. Results from a 1-year, open-label, single arm, multi-center trial evaluating the efficacy and safety of oral deferasirox in patients diagnosed with low and int-1 risk myelodysplastic syndrome (MDS) and transfusion-dependent iron overload. Ann. Hematol. 92, 191–198 (2013).
Pennell, D. J. et al. Deferasirox for up to 3 years leads to continued improvement of myocardial T2* in patients with β-thalassemia major. Haematologica 97, 842–848 (2012).
Phatak, P. et al. A phase 1/2, dose-escalation trial of deferasirox for the treatment of iron overload in HFE-related hereditary hemochromatosis. Hepatology 52, 1671–1779 (2010).
Taher, A. T. et al. Deferasirox reduces iron overload significantly in nontransfusion-dependent thalassemia: 1-year results from a prospective, randomized, double-blind, placebo-controlled study. Blood 120, 970–977 (2012).
Vichinsky, E. et al. Long-term safety and efficacy of deferasirox (Exjade) for up to 5 years in transfusional iron-overloaded patients with sickle cell disease. Br. J. Haematol. 154, 387–397 (2011).
Voskaridou, E. et al. Deferasirox effectively decreases iron burden in patients with double heterozygous HbS/β-thalassemia. Ann. Hematol. 90, 11–15 (2011).
Wood, J. C. et al. The effect of deferasirox on cardiac iron in thalassemia major: impact of total body iron stores. Blood 116, 537–543 (2010).
Al-Khabori, M. et al. Side effects of deferasirox iron chelation in patients with beta thalassemia major or intermedia. Oman. Med. J. 28, 121–124 (2013).
Economou, M. et al. Renal dysfunction in patients with beta-thalassemia major receiving iron chelation therapy either with deferoxamine and deferiprone or with deferasirox. Acta Haematol. 123, 148–152 (2010).
Efthimia, V. et al. Nephrolithiasis in beta thalassemia major patients treated with deferasirox: an advent or an adverse event? A single Greek center experience. Ann. Hematol. 92, 263–265 (2013).
Tunç, B. et al. Deferasirox therapy in children with Fanconi aplastic anemia. J. Pediatr. Hematol. Oncol. 34, 247–251 (2012).
Unal, S., Hazirolan, T., Eldem, G. & Gumruk, F. The effects of deferasirox on renal, cardiac and hepatic iron load in patients with β-thalassemia major: preliminary results. Pediatr. Hematol. Oncol. 28, 217–221 (2011).
Cermak, J. et al. A comparative study of deferasirox and deferiprone in the treatment of iron overload in patients with myelodysplastic syndromes. Leuk. Res. 37, 1612–1615 (2013).
Ktena, Y. P., Athanasiadou, A., Lambrou, G., Adamaki, M. & Moschovi, M. Iron chelation with deferasirox for the treatment of secondary hemosiderosis in pediatric oncology patients: a single-center experience. J. Pediatr. Hematol. Oncol. 35, 447–450 (2013).
Karimi, M. et al. Iranian experience of deferasirox (Exjade®) in transfusion-dependent patients with iron overload: what is the most effective dose based on serum ferritin levels? Hematology 17, 367–371 (2012).
Aydinok, Y. et al. Observational study comparing long-term safety and efficacy of deferasirox with desferrioxamine therapy in chelation-naïve children with transfusional iron overload. Eur. J. Haematol. 88, 431–438 (2012).
Panigrahi, I., Vaidya, P. C., Bansal, D. & Marwaha, R. K. Efficacy of deferasirox in North Indian β-thalassemia major patients: a preliminary report. J. Pediatr. Hematol. Oncol. 34, 51–53 (2012).
Gattermann, N. et al. Deferasirox treatment of iron-overloaded chelation-naïve and prechelated patients with myelodysplastic syndromes in medical practice: results from the observational studies eXtend and eXjange. Eur. J. Haematol. 88, 260–268 (2012).
Eshghi, P. et al. Efficacy and safety of Iranian made deferasirox (Osveral®) in Iranian major thalassemic patients with transfusional iron overload: A one year prospective multicentric open-label non-comparative study. Daru 19, 240–248 (2011).
Chang, H. H. et al. Improved efficacy and tolerability of oral deferasirox by twice-daily dosing for patients with transfusion-dependent β-thalassemia. Pediatr. Blood Cancer 56, 420–424 (2011).
Pennell, D. J. et al. A 1-year randomized controlled trial of deferasirox versus deferoxamine for myocardial iron removal in β-thalassemia major (CORDELIA). Blood 123, 1447–1454 (2014).
Fernandez-Fernandez, B. et al. Tenofovir nephrotoxicity: 2011 update. AIDS Res. Treat. 2011, 354908 (2011).
Ortiz, A. et al. Tubular cell apoptosis and cidofovir-induced acute renal failure. Antivir. Ther. 10, 185–190 (2005).
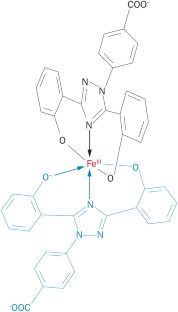
Hider, R. C. Charge states of deferasirox-ferric iron complexes. Am. J. Kidney Dis. 55, 614–615 (2010).
Huang, X. P., Thiessen, J. J., Spino, M. & Templeton, D. M. Transport of iron chelators and chelates across MDCK cell monolayers: implications for iron excretion during chelation therapy. Int. J. Hematol. 91, 401–412 (2010).
Sánchez-González, P. D., López-Hernandez, F. J., Morales, A. I., Macías-Nuñez, J. F. & López-Novoa, J. M. Effects of deferasirox on renal function and renal epithelial cell death. Toxicol. Lett. 203, 154–161 (2011).
Goldstein, D. J. et al. Cyclosporine-associated end-stage nephropathy after cardiac transplantation: incidence and progression. Transplantation 63, 664–668 (1997).
Klein, I. H. et al. Different effects of tacrolimus and cyclosporine on renal hemodynamics and blood pressure in healthy subjects. Transplantation 73, 732–736 (2002).
Oexle, H., Gnaiger, E. & Weiss, G. Iron-dependent changes in cellular energy metabolism: influence on citric acid cycle and oxidative phosphorylation. Biochim. Biophys. Acta 1413, 99–107 (1999).
Gattermann, N. et al. Impact on Iron removal of dose reduction for non-progressive serum creatinine increases during treatment with the once-daily, oral iron chelator deferasirox (Exjade®, ICL670) [abstract]. Blood 108, a3824 (2006).
Baliga, R., Zhang, Z., Baliga, M., Ueda, N. & Shah, S. V. In vitro and in vivo evidence suggesting a role for iron in cisplatin-induced nephrotoxicity. Kidney Int. 53, 394–401 (1998).
Dixon, S. J. et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell 149, 1060–1072 (2012).
Cianciulli, P. et al. Acute renal failure occurring during intravenous desferrioxamine therapy: recovery after haemodialysis. Haematologica 77, 514–515 (1992).
Food and Drug Administration. Safety [online], (2012).
Food and Drug Administration. Safety [online], (2010).
Walker, P. D. & Shah, S. V. Evidence suggesting a role for hydroxyl radical in gentamicin-induced acute renal failure in rats. J. Clin. Invest. 81, 334–341 (1988).
Koren, G., Kochavi-Atiya, Y., Bentur, Y. & Olivieri, N. F. The effects of subcutaneous deferoxamine administration on renal function in thalassemia major. Int. J. Hematol. 54, 371–375 (1991).
Clajus, C. et al. Acute kidney injury due to deferoxamine in a renal transplant patient. Nephrol. Dial. Transplant. 23, 1061–1064 (2008).
Yoon, Y. S., Byun, H. O., Cho, H., Kim, B. K. & Yoon, G. Complex II defect via down-regulation of iron-sulfur subunit induces mitochondrial dysfunction and cell cycle delay in iron chelation-induced senescence-associated growth arrest. J. Biol. Chem. 278, 51577–51586 (2003).
Justo, P., Lorz, C., Sanz, A., Egido, J. & Ortiz, A. Intracellular mechanisms of cyclosporin A-induced tubular cell apoptosis. J. Am. Soc. Nephrol. 14, 3072–3080 (2003).
Molitoris, B. A. et al. siRNA targeted to p53 attenuates ischemic and cisplatin-induced acute kidney injury. J. Am. Soc. Nephrol. 20, 1754–1764 (2009).
Kelly, K. J., Plotkin, Z., Vulgamott, S. L. & Dagher, P. C. P53 mediates the apoptotic response to GTP depletion after renal ischemia-reperfusion: protective role of a p53 inhibitor. J. Am. Soc. Nephrol. 14, 128–138 (2003).
Allon, M., Lawson, L., Eckman, J. R., Delaney, V. & Bourke, E. Effects of nonsteroidal antiinflammatory drugs on renal function in sickle cell anemia. Kidney Int. 34, 500–506 (1988).
Lee, J. W. et al. Pharmacogenetic study of deferasirox, an iron chelating agent. PLoS One 8, e64114 (2013).
Lai, M. E. et al. Renal function in patients with β-thalassaemia major: a long-term follow-up study. Nephrol. Dial. Transplant. 27, 3547–3551 (2012).
Han, J. Y. et al. Comprehensive analysis of UGT1A polymorphisms predictive for pharmacokinetics and treatment outcome in patients with non-small-cell lung cancer treated with irinotecan and cisplatin. J. Clin. Oncol. 24, 2237–2244 (2006).
Satoh, T. et al. Genotype-directed, dose-finding study of irinotecan in cancer patients with UGT1A1*28 and/or UGT1A1*6 polymorphisms. Cancer Sci. 102, 1868–1873 (2011).
Shulman, K. et al. Clinical implications of UGT1A1*28 genotype testing in colorectal cancer patients. Cancer 117, 3156–3162 (2011).
Mathijssen, R. H. et al. Clinical pharmacokinetics and metabolism of irinotecan (CPT-11). Clin. Cancer Res. 7, 2182–2194 (2001).
Adams, R. L. & Bird, R. J. Safety and efficacy of deferasirox in the management of transfusion-dependent patients with myelodysplastic syndrome and aplastic anaemia: a perspective review. Ther. Adv. Hematol. 4, 93–102 (2013).
Ataga, K. I. & Orringer, E. P. Renal abnormalities in sickle cell disease. Am. J. Hematol. 63, 205–211 (2000).
McKie, K. T. et al. Prevalence, prevention, and treatment of microalbuminuria and proteinuria in children with sickle cell disease. J. Pediatr. Hematol. Oncol. 29, 140–144 (2007).
Vichinsky, E. Clinical application of deferasirox: practical patient management. Am. J. Hematol. 83, 398–402 (2008).
Acknowledgements
The authors' research was supported by the grants FIS PS09/00447, PI13/00047, ISCIII-RETIC REDinREN RD12/0021, Comunidad de Madrid S2010/BMD-2378, and CYTED IBERERC, by Programa Intensificación Actividad Investigadora (ISCIII) to A.O., by ERA–EDTA fellowship to L.G.E. and by Programa Interinstitucional para el Fortalecimiento de la Investigación y el Posgrado del Pacífico to J.D.D.-G.
Author information
Authors and Affiliations
Contributions
All authors researched the data for the article, provided substantial contributions to discussions of its content, wrote the article and undertook review and/or editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Table 1
Diagnostic criteria used to diagnose proximal tubular injury secondary to deferasirox (PDF 105 kb)
Supplementary Table 2
Deferasirox nephrotoxicity in RCTs (PDF 137 kb)
Supplementary Table 3
Deferasirox nephrotoxicity in clinical practice (PDF 154 kb)
Rights and permissions
About this article
Cite this article
Díaz-García, J., Gallegos-Villalobos, A., Gonzalez-Espinoza, L. et al. Deferasirox nephrotoxicity—the knowns and unknowns. Nat Rev Nephrol 10, 574–586 (2014). https://doi.org/10.1038/nrneph.2014.121
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2014.121
This article is cited by
-
Metabolic mechanisms of acute proximal tubular injury
Pflügers Archiv - European Journal of Physiology (2022)
-
Drug toxicity in the proximal tubule: new models, methods and mechanisms
Pediatric Nephrology (2022)
-
The multifaceted role of iron in renal health and disease
Nature Reviews Nephrology (2020)
-
The iron chelator Deferasirox causes severe mitochondrial swelling without depolarization due to a specific effect on inner membrane permeability
Scientific Reports (2020)
-
Thalassemia: Common Clinical Queries in Management
The Indian Journal of Pediatrics (2020)