Abstract
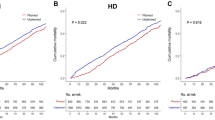
Over the past two decades, most guidelines have advocated early initiation of dialysis on the basis of studies showing improved survival in patients starting dialysis early. These recommendations led to an increase in the proportion of patients initiating dialysis with an estimated glomerular filtration rate (eGFR) >10 ml/min/1.73 m2, from 20% in 1996 to 52% in 2008. During this period, the percentage of patients starting dialysis with an eGFR ≥15 ml/min/1.73 m2 increased from 4% to 17%. However, recent studies have failed to substantiate a benefit of early dialysis initiation and some data have suggested worse outcomes for patients starting dialysis with a higher eGFR. Several reasons for this seemingly paradoxical observation have been suggested, including the fact that patients requiring early dialysis are likely to have more severe symptoms and comorbidities, leading to confounding by indication, as well as biological mechanisms that causally relate early dialysis therapy to adverse outcomes. Patients with a failing renal allograft who reinitiate dialysis encounter similar problems. However, unique factors associated with a failed allograft means that the optimal timing of dialysis initiation in failed transplant patients might differ from that in transplant-naive patients with chronic kidney disease. In this Review, we discuss studies of dialysis initiation and compare risks and benefits of early versus late initiation and reinitiation of dialysis therapy.
Key Points
-
Late initiation of dialysis is not associated with worse mortality in transplant-naive patients with chronic kidney disease compared with mortality in patients who start dialysis early
-
Current guidelines suggest that the majority of transplant-naive patients will be symptomatic and need to start dialysis with an estimated glomerular filtration rate (eGFR) in the 6–9 ml/min/1.73 m2 range
-
In patients with a failing kidney transplant, there is a paucity of evidence for or against early reinitiation of dialysis treatment
-
Factors such as predialysis care, late referral, dialysis dose, timing of immunosuppression reduction and residual function of the renal allograft might modify the association between dialysis reinitiation and outcomes in failed transplant recipients
-
Several biological factors, including hemodynamic instability, loss of residual renal function and a high infection rate, might contribute to the increased mortality risk associated with dialysis initiation
-
Starting dialysis early solely based on eGFR is not justified and could in fact be harmful in some cases; therefore, alternative and more reliable measures of a patient's clinical condition are required
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
[No authors listed] NKF-DOQI clinical practice guidelines for peritoneal dialysis adequacy. National Kidney Foundation. Am. J. Kidney Dis. 30, S67–S136 (1997).
National Kidney Foundation. KDOQI clinical practice guidelines and clinical practice recommendations for 2006 updates: hemodialysis adequacy, peritoneal dialysis adequacy, vascular access. Am. J. Kidney Dis. 48 (Suppl. 1), S1–S322 (2006).
European Best Practice Guidelines Expert Group on Hemodialysis, European Renal Association. European Best Practice Guidelines for Haemodialysis (Part 1). When to start dialysis. Nephrol. Dial. Transplant. 17 (Suppl. 7), S10–S11 (2002).
Tattersall, J. et al. on behalf of the ERBP Advisory Board. When to start dialysis: updated guidance following publication of the Initiating Dialysis Early and Late (IDEAL) study. Nephrol. Dial. Transplant. 26, 2082–2086 (2011).
US Renal Data System. USRDS 2010 Annual Data Report [online], (2010).
Rosansky, S. J., Eggers, P., Jackson, K., Glassock, R. & Clark, W. F. Early start of hemodialysis may be harmful. Arch. Intern. Med. 171, 396–403 (2011).
US Renal Data System. USRDS 2009 Annual Data Report [online], (2009).
Korevaar, J. C. et al. for the Netherlands Cooperative Study on the Adequacy of Dialysis Study Group. When to initiate dialysis: effect of proposed US guidelines on survival. Lancet 358, 1046–1050 (2001).
Traynor, J. P., Simpson, K., Geddes, C. C., Deighan, C. J. & Fox, J. G. Early initiation of dialysis fails to prolong survival in patients with end-stage renal failure. J. Am. Soc. Nephrol. 13, 2125–2132 (2002).
Beddhu, S. et al. Impact of timing of initiation of dialysis on mortality. J. Am. Soc. Nephrol. 14, 2305–2312 (2003).
Kazmi, W. H. et al. Effect of comorbidity on the increased mortality associated with early initiation of dialysis. Am. J. Kidney Dis. 46, 887–896 (2005).
Wilson, B. et al. Optimal timing of initiation of chronic hemodialysis? Hemodial. Int. 11, 263–269 (2007).
Stel, V. S. et al. Residual renal function at the start of dialysis and clinical outcomes. Nephrol. Dial. Transplant. 24, 3175–3182 (2009).
Sawhney, S., Djurdjev, O., Simpson, K., Macleod, A. & Levin, A. Survival and dialysis initiation: comparing British Columbia and Scotland registries. Nephrol. Dial. Transplant. 24, 3186–3192 (2009).
Lassalle, M. et al. Age and comorbidity may explain the paradoxical association of an early dialysis start with poor survival. Kidney Int. 77, 700–707 (2010).
Wright, S. et al. Timing of dialysis initiation and survival in ESRD. Clin. J. Am. Soc. Nephrol. 5, 1828–1835 (2010).
Cooper, B. A. et al. for the IDEAL Study. A randomized, controlled trial of early versus late initiation of dialysis. N. Engl. J. Med. 363, 609–619 (2010).
Evans, M. et al. No survival benefit from early-start dialysis in a population-based, inception cohort study of Swedish patients with chronic kidney disease. J. Intern. Med. 269, 289–298 (2011).
Rao, P. S. et al. Survival on dialysis post-kidney transplant failure: results from the Scientific Registry of Transplant Recipients. Am. J. Kidney Dis. 49, 294–300 (2007).
Cáldes Ruisánchez, S. et al. Dialysis after kidney transplant failure: do patients start in a worse condition than the general population with chronic kidney disease? Nefrologia 31, 51–57 (2011).
de Jonge, H., Bammens, B., Lemahieu, W., Maes, B. D. & Vanrenterghem, Y. Comparison of peritoneal dialysis and haemodialysis after renal transplant failure. Nephrol. Dial. Transplant. 21, 1669–1674 (2006).
Badve, S. V. et al. for the ANZDATA Registry PD Working Committee. Effect of previously failed kidney transplantation on peritoneal dialysis outcomes in the Australian and New Zealand patient populations. Nephrol. Dial. Transplant. 21, 776–783 (2006).
Mujais, S. & Story, K. Patient and technique survival on peritoneal dialysis in patients with failed renal allograft: a case-control study. Kidney. Int. Suppl. 103, S133–S137 (2006).
Duman, S. et al. Patients with failed renal transplant may be suitable for peritoneal dialysis. Int. Urol. Nephrol. 36, 249–252 (2004).
Sasal, J., Naimark, D., Klassen, J., Shea, J. & Bargman, J. M. Late renal transplant failure: an adverse prognostic factor at initiation of peritoneal dialysis. Perit. Dial. Int. 21, 405–410 (2001).
Davies, S. J. Peritoneal dialysis in the patient with a failing renal allograft. Perit. Dial. Int. 21 (Suppl. 3), S280–S284 (2001).
Bonomini, V. et al. Residual renal function and effective rehabilitation in chronic dialysis. Nephron 16, 89–102 (1976).
Bonomini, V., Vangelista, A. & Stefoni, S. Early dialysis in renal substitutive programs. Kidney Int. Suppl. 8, S112–S116 (1978).
Bonomini, V., Feletti, C., Scolari, M. P. & Stefoni, S. Benefits of early initiation of dialysis. Kidney. Int. Suppl. 17, S57–S59 (1985).
Ratcliffe, P. J., Phillips, R. E. & Oliver, D. O. Late referral for maintenance dialysis. Br. Med. J. (Clin. Res. Ed.) 288, 441–443 (1984).
Jungers, P. et al. Late referral to maintenance dialysis: detrimental consequences. Nephrol. Dial. Transplant. 8, 1089–1093 (1993).
Tattersall, J., Greenwood, R. & Farrington, K. Urea kinetics and when to commence dialysis. Am. J. Nephrol. 15, 283–289 (1995).
[No authors listed] Adequacy of dialysis and nutrition in continuous peritoneal dialysis: association with clinical outcomes. Canada-USA (CANUSA) Peritoneal Dialysis Study Group. J. Am. Soc. Nephrol. 7, 198–207 (1996).
Cooper, B. A. et al. The Initiating Dialysis Early and Late (IDEAL) study: study rationale and design. Perit. Dial. Int. 24, 176–181 (2004).
Rosansky, S. J., Clark, W. F., Eggers, P. & Glassock, R. J. Initiation of dialysis at higher GFRs: is the apparent rising tide of early dialysis harmful or helpful? Kidney Int. 76, 257–261 (2009).
McCusker, F. X., Teehan, B. P., Thorpe, K. E., Keshaviah, P. R. & Churchill, D. N. How much peritoneal dialysis is required for the maintenance of a good nutritional state? Canada-USA (CANUSA) Peritoneal Dialysis Study Group. Kidney Int. Suppl. 56, S56–S61 (1996).
Churchill, D. N. An evidence-based approach to earlier initiation of dialysis. Am. J. Kidney Dis. 30, 899–906 (1997).
Beddhu, S. et al. Creatinine production, nutrition, and glomerular filtration rate estimation. J. Am. Soc. Nephrol. 14, 1000–1005 (2003).
Kalantar-Zadeh, K. et al. The obesity paradox and mortality associated with surrogates of body size and muscle mass in patients receiving hemodialysis. Mayo Clin. Proc. 85, 991–1001 (2010).
Molnar, M. Z. et al. Associations of body mass index and weight loss with mortality in transplant-waitlisted maintenance hemodialysis patients. Am. J. Transplant. 11, 725–736 (2011).
Noori, N. et al. Novel equations to estimate lean body mass in maintenance hemodialysis patients. Am. J. Kidney Dis. 57, 130–139 (2011).
Rosansky, S., Glassock, R. J. & Clark, W. F. Early start of dialysis: a critical review. Clin. J. Am. Soc. Nephrol. 6, 1222–1228 (2011).
Cockcroft, D. W. & Gault, M. H. Prediction of creatinine clearance from serum creatinine. Nephron 16, 31–41 (1976).
Lindholm, B. & Davies, S. End-stage renal disease in 2010: Timing of dialysis initiation and choice of dialysis modality. Nat. Rev. Nephrol. 7, 66–68 (2011).
Faust, J. & Schreiner, O. Early versus late initiation of dialysis. N. Engl. J. Med. 363, 2368–2369 (2010).
Korevaar, J. C. et al. Evaluation of DOQI guidelines: early start of dialysis treatment is not associated with better health-related quality of life. Am. J. Kidney Dis. 39, 108–115 (2002).
Dhaun, N. & Kluth, D. Early versus late initiation of dialysis. N. Engl. J. Med. 363, 2369 (2010).
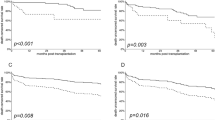
Gill, J. S., Abichandani, R., Kausz, A. T. & Pereira, B. J. Mortality after kidney transplant failure: the impact of non-immunologic factors. Kidney Int. 62, 1875–1883 (2002).
Perl, J. et al. Impact of dialysis modality on survival after kidney transplant failure. Clin. J. Am. Soc. Nephrol. 6, 582–590 (2011).
Ojo, A. et al. Prognosis after primary renal transplant failure and the beneficial effects of repeat transplantation: multivariate analyses from the United States Renal Data System. Transplantation 66, 1651–1659 (1998).
Johnston, O., Zalunardo, N., Rose, C. & Gill, J. S. Prevention of sepsis during the transition to dialysis may improve the survival of transplant failure patients. J. Am. Soc. Nephrol. 18, 1331–1337 (2007).
Gill, J. S., Abichandani, R., Khan, S., Kausz, A. T. & Pereira, B. J. Opportunities to improve the care of patients with kidney transplant failure. Kidney Int. 61, 2193–2200 (2002).
Almond, M. K., Tailor, D., Marsh, F. P., Raftery, M. J. & Cunningham, J. Increased erythropoietin requirements in patients with failed renal transplants returning to a dialysis programme. Nephrol. Dial. Transplant. 9, 270–273 (1994).
López-Gómez, J. M. et al. Presence of a failed kidney transplant in patients who are on hemodialysis is associated with chronic inflammatory state and erythropoietin resistance. J. Am. Soc. Nephrol. 15, 2494–2501 (2004).
Wanner, C., Zimmermann, J., Schwedler, S. & Metzger, T. Inflammation and cardiovascular risk in dialysis patients. Kidney Int. Suppl. 80, 99–102 (2002).
Molnar, M. Z. et al. Association of the malnutrition-inflammation score with clinical outcomes in kidney transplant recipients. Am. J. Kidney Dis. 58, 101–108 (2011).
Rambod, M. et al. Association of malnutrition-inflammation score with quality of life and mortality in hemodialysis patients: a 5-year prospective cohort study. Am. J. Kidney Dis. 53, 298–309 (2009).
Perl, J. & Bargman, J. M. The importance of residual kidney function for patients on dialysis: a critical review. Am. J. Kidney Dis. 53, 1068–1081 (2009).
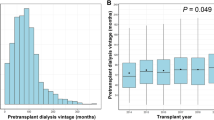
Molnar, M. Z. et al. Estimated glomerular filtration rate at re-initiation of dialysis and mortality in failed kidney transplant recipients. Nephrol. Dial. Transplant. (in press).
Mendelssohn, D. C., Malmberg, C. & Hamandi, B. An integrated review of “unplanned” dialysis initiation: reframing the terminology to “suboptimal” initiation. BMC Nephrol. 10, 22 (2009).
Chan, M. R., Dall, A. T., Fletcher, K. E., Lu, N. & Trivedi, H. Outcomes in patients with chronic kidney disease referred late to nephrologists: a meta-analysis. Am. J. Med. 120, 1063–1070 (2007).
Johnston, O., Rose, C., Landsberg, D., Gourlay, W. A. & Gill, J. S. Nephrectomy after transplant failure: current practice and outcomes. Am. J. Transplant. 7, 1961–1967 (2007).
Bloembergen, W. E. et al. Relationship of dialysis membrane and cause-specific mortality. Am. J. Kidney Dis. 33, 1–10 (1999).
Chavers, B. M., Solid, C. A., Gilbertson, D. T. & Collins, A. J. Infection-related hospitalization rates in pediatric versus adult patients with end-stage renal disease in the United States. J. Am. Soc. Nephrol. 18, 952–959 (2007).
Allon, M. et al. for the HEMO Study Group. Impact of dialysis dose and membrane on infection-related hospitalization and death: results of the HEMO Study. J. Am. Soc. Nephrol. 14, 1863–1870 (2003).
Orofino, L. et al. Epidemiology of symptomatic hypotension in hemodialysis: is cool dialysate beneficial for all patients? Am. J. Nephrol. 10, 177–180 (1990).
Cukor, D. et al. Depression and anxiety in urban hemodialysis patients. Clin. J. Am. Soc. Nephrol. 2, 484–490 (2007).
Liberek, T. et al. When to initiate dialysis—is early start always better? Nephrol. Dial. Transplant. 26, 2087–2091 (2011).
Grootendorst, D. C. et al. for the NECOSAD Study Group. The MDRD formula does not reflect GFR in ESRD patients. Nephrol. Dial. Transplant. 26, 1932–1937 (2011).
Noori, N. et al. Survival predictability of lean and fat mass in men and women undergoing maintenance hemodialysis. Am. J. Clin. Nutr. 92, 1060–1070 (2010).
Kalantar-Zadeh, K. et al. Diets and enteral supplements for improving outcomes in chronic kidney disease. Nat. Rev. Nephrol. 7, 369–384 (2011).
Noori, N. et al. Mid-arm muscle circumference and quality of life and survival in maintenance hemodialysis patients. Clin. J. Am. Soc. Nephrol. 5, 2258–2268 (2010).
Gaspari, F. et al. on behalf of the MY. S. S. Study Investigators. Performance of different prediction equations for estimating renal function in kidney transplantation. Am. J. Transplant. 4, 1826–1835 (2004).
Coresh, J., Walser, M. & Hill, S. Survival on dialysis among chronic renal failure patients treated with a supplemented low-protein diet before dialysis. J. Am. Soc. Nephrol. 6, 1379–1385 (1995).
Barreto, F. C. et al. on behalf of the European Uremic Toxin Work Group (EUTox). Serum indoxyl sulfate is associated with vascular disease and mortality in chronic kidney disease patients. Clin. J. Am. Soc. Nephrol. 4, 1551–1558 (2009).
Niwa, T. et al. The protein metabolite hypothesis, a model for the progression of renal failure: an oral adsorbent lowers indoxyl sulfate levels in undialyzed uremic patients. Kidney Int. Suppl. 62, S23–S28 (1997).
Niwa, T. Uremic toxicity of indoxyl sulfate. Nagoya J. Med. Sci. 72, 1–11 (2010).
Pergola, P. E. et al. for the BEAM Study Investigators. Bardoxolone methyl and kidney function in CKD with type 2 diabetes. N. Engl. J. Med. 365, 327–336 (2011).
de Brito-Ashurst, I., Varagunam, M., Raftery, M. J. & Yaqoob, M. M. Bicarbonate supplementation slows progression of CKD and improves nutritional status. J. Am. Soc. Nephrol. 20, 2075–2084 (2009).
Phisitkul, S., Hacker, C., Simoni, J., Tran, R. M. & Wesson, D. E. Dietary protein causes a decline in the glomerular filtration rate of the remnant kidney mediated by metabolic acidosis and endothelin receptors. Kidney Int. 73, 192–199 (2008).
Mahajan, A. et al. Daily oral sodium bicarbonate preserves glomerular filtration rate by slowing its decline in early hypertensive nephropathy. Kidney Int. 78, 303–309 (2010).
Acknowledgements
M. Z. Molnar received grants from the National Development Agency (KTIA-OTKA-EU 7KP-HUMAN-MB08-A-81231) from the Research and Technology Innovation Fund, and was also supported by the Hungarian Kidney Foundation. K. Kalantar-Zadeh was supported by research grants from the National Institute of Diabetes, Digestive and Kidney Diseases of the National Institutes of Health (K24 DK091419 and R01 DK078106) and a philanthropic grant from H. Simmons.
Author information
Authors and Affiliations
Contributions
M. Z. Molnar and K. Kalantar-Zadeh researched data to include in the manuscript. M. Z. Molnar, C. P. Kovesdy and K. Kalantar-Zadeh contributed to discussion of content for the article. All authors contributed equally to the writing of the article and to the reviewing and editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Molnar, M., Ojo, A., Bunnapradist, S. et al. Timing of dialysis initiation in transplant-naive and failed transplant patients. Nat Rev Nephrol 8, 284–292 (2012). https://doi.org/10.1038/nrneph.2012.36
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2012.36
This article is cited by
-
Dialysis after kidney transplant failure: how to deal with this daunting task?
Journal of Nephrology (2023)
-
First-year mortality in incident dialysis patients: results of the Peridialysis study
BMC Nephrology (2022)
-
Hemodialysis reinitiation using a resurrected mummy fistula: a case report
BMC Nephrology (2018)
-
Cardiovascular disease in haemodialysis: role of the intravascular innate immune system
Nature Reviews Nephrology (2017)
-
Risk of chronic kidney disease after cancer nephrectomy
Nature Reviews Nephrology (2014)