Abstract
Sepsis is the most common and severe cause of morbidity and mortality among critically ill patients. Multiple organ dysfunction syndrome often complicates sepsis, leading to a worse prognosis that is proportional to the severity and number of damaged organs. Acute kidney injury (AKI) also complicates sepsis, with a linear relationship between the severity of kidney damage and sepsis prognosis. The management of sepsis and septic AKI involves intensive proactive preventive measures, medical and extracorporeal treatment of established sepsis, support of failing organs and rehabilitation of the residual effects left by this devastating syndrome. Unfortunately, although some innovations in the clinical management of sepsis are now available, their beneficial effects on renal function are still uncertain. The aim of this Review is to provide an update on the current state of interventions in sepsis-related AKI. Prevention, pharmacological support and extracorporeal blood purification for septic AKI will be reviewed and discussed.
Key Points
-
Sepsis has a complex pathophysiology and typically causes multiple organ dysfunction
-
Sepsis-related acute kidney injury (AKI) is an independent risk factor for mortality
-
Potential medical interventions in sepsis-related AKI have not yet been adequately validated in routine clinical practice
-
Current recommendations are that adequate resuscitation by early goal-directed therapy should be provided together with pharmacological support (vasopressor and diuretics), avoiding fluid overload
-
In patients with severe septic AKI, extracorporeal blood purification should be provided in order to support renal function and to manage fluid overload; optimal timing of renal replacement therapy has not yet been defined
-
The currently recommended dose for continuous renal replacement therapies is 25 ml/kg/h, and higher doses have not been associated with improved survival; however, such therapies should be carefully monitored and underdosing avoided
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Ronco, C., Kellum, J. A., Bellomo, R. & House, A. A. Potential interventions in sepsis-related acute kidney injury. Clin. J. Am. Soc. Nephrol. 3, 531–544 (2008).
Bernard, B. et al. Antibiotic prophylaxis for the prevention of bacterial infections in cirrhotic patients with gastrointestinal bleeding: a meta-analysis. Hepatology 29, 1655–1661 (1999).
Sharma, V. K. & Howden, C. W. Prophylactic antibiotic administration reduces sepsis and mortality in acute necrotizing pancreatitis: a meta-analysis. Pancreas 22, 28–31 (2001).
Tablan, O. C. et al. Guidelines for preventing health-care-associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recomm. Rep. 53, 1–36 (2004).
Finfer, S. et al. Intensive versus conventional glucose control in critically ill patients. N. Engl. J. Med. 360, 1283–1297 (2009).
de Jonge, E. et al. Effects of selective decontamination of digestive tract on mortality and acquisition of resistant bacteria in intensive care: a randomised controlled trial. Lancet 362, 1011–1016 (2003).
de Smet, A. M. et al. Decontamination of the digestive tract and oropharynx in ICU patients. N. Engl. J. Med. 360, 20–31 (2009).
Heyland, D. K. et al. Should immunonutrition become routine in critically ill patients? A systematic review of the evidence. JAMA 286, 944–953 (2001).
Foxwell, A. R., Cripps, A. W. & Dear, K. B. Haemophilus influenzae oral whole cell vaccination for preventing acute exacerbations of chronic bronchitis. Cochrane Database of Systematic Reviews Issue 4. Art. No.: CD001958 doi:10.1002/14651858.CD001958.pub2 (2006).
Douzinas, E. E. et al. Prevention of infection in multiple trauma patients by high-dose intravenous immunoglobulins. Crit. Care Med. 28, 8–15 (2000).
Needham, D. M., Truong, A. D. & Fan, E. Technology to enhance physical rehabilitation of critically ill patients. Crit. Care Med. 37, S436–S441 (2009).
Bagshaw, S. M. et al. Acute kidney injury in septic shock: clinical outcomes and impact of duration of hypotension prior to initiation of antimicrobial therapy. Intensive Care Med. 35, 871–881 (2009).
Zahar, J. R. et al. Inappropriate prescribing of aminoglycosides: risk factors and impact of an antibiotic control team. J. Antimicrob. Chemother. 58, 651–656 (2006).
Mueller, C. et al. Incidence of contrast nephropathy in patients receiving comprehensive intravenous and oral hydration. Swiss Med. Wkly 135, 286–290 (2005).
Langenberg, C., Bagshaw, S. M., May, C. N. & Bellomo, R. The histopathology of septic acute kidney injury: a systematic review. Crit. Care 12, R38 (2008).
Redfors, B., Bragadottir, G., Sellgren, J., Swärd, K. & Ricksten, S. E. Acute renal failure is NOT an “acute renal success”—a clinical study on the renal oxygen supply/demand relationship in acute kidney injury. Crit. Care Med. 38, 1695–1701 (2010).
Wan, L., Bellomo, R., Di Giantomasso, D. & Ronco, C. The pathogenesis of septic acute renal failure. Curr. Opin. Crit. Care 9, 496–502 (2003).
Dellinger, R. P. et al. for the Surviving Sepsis Campaign Management Guidelines Committee. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit. Care Med. 32, 858–873 (2004).
Rivers, E. et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N. Engl. J. Med. 345, 1368–1377 (2001).
Payen, D. et al. A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit. Care 12, R74 (2008).
Bouchard, J. et al. for the Program to Improve Care in Acute Renal Disease (PICARD) Study Group. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 76, 422–427 (2009).
Bellomo, R., Wan, L. & May, C. Vasoactive drugs and acute kidney injury. Crit. Care Med. 36, S179–S186 (2008).
Russell, J. A. et al. for the VASST Investigators. Vasopressin versus norepinephrine infusion in patients with septic shock. N. Engl. J. Med. 358, 877–887 (2008).
Gordon, A. C. et al. The effects of vasopressin on acute kidney injury in septic shock. Intensive Care Med. 36, 83–91 (2010).
Cruz, D. N., Bagshaw, S. M., Ronco, C. & Ricci, Z. Acute kidney injury: classification and staging. Contrib. Nephrol. 164, 24–32 (2010).
Ricci, Z., Cruz, D. N. & Ronco, C. Classification and staging of acute kidney injury: beyond the RIFLE and AKIN criteria. Nat. Rev. Nephrol. doi:10.1038/nrneph.2011.14.
DeTorrente, A. et al. Effects of furosemide and acetylcholine in norepinephrine-induced acute renal failure. Am. J. Physiol. 235, F131–F136 (1978).
Cantarovich, F., Rangoonwala, B., Lorenz, H., Verho, M. & Esnault, V. L. High-dose furosemide for established ARF: a prospective, randomized, double-blind, placebo-controlled, multicenter trial. Am. J. Kidney Dis. 44, 402–409 (2004).
Uchino, S. et al. for the Beginning and Ending Supportive Therapy for the Kidney (B. E. S. T. Kidney) Investigators. Diuretics and mortality in acute renal failure. Crit. Care Med. 32, 1669–1677 (2004).
Lameire, N., Vanholder, R. & Van Biesen, W. Loop diuretics for patients with acute renal failure: helpful or harmful? JAMA 288, 2599–2601 (2002).
Bagshaw, S. M., Gibney, R. T., McAlister, F. A. & Bellomo, R. The SPARK Study: a phase II randomized blinded controlled trial of the effect of furosemide in critically ill patients with early acute kidney injury. Trials 11, 50 (2010).
Favia, I., Garisto, C., Rossi, E., Picardo, S. & Ricci, Z. Fluid management in pediatric intensive care. Contrib. Nephrol. 164, 217–226 (2010).
Morelli, A. et al. Prophylactic fenoldopam for renal protection in sepsis: a randomised, double-blind, placebo-controlled pilot trial. Crit. Care Med. 33, 2451–2456 (2005).
Tumlin, J. A. et al. Fenoldopam mesylate in early acute tubular necrosis: a randomized, double-blind, placebo-controlled clinical trial. Am. J. Kidney Dis. 46, 26–34 (2005).
Landoni, G. et al. Fenoldopam reduces the need for renal replacement therapy and in-hospital death in cardiovascular surgery: a meta-analysis. J. Cardiothorac. Vasc. Anesth. 22, 27–33 (2008).
Bellomo, R. How to feed patients with renal dysfunction. Blood Purif. 20, 296–230 (2002).
Btaiche, I. F., Mohammad, R. A., Alaniz, C. & Mueller, B. A. Amino acid requirements in critically ill patients with acute kidney injury treated with continuous renal replacement therapy. Pharmacotherapy 28, 600–613 (2008).
Liu, K. D. et al. Timing of initiation of dialysis in critically ill patients with acute kidney injury. Clin. J. Am. Soc. Nephrol. 1, 915–919 (2006).
Bagshaw, S. M., Cruz, D. N., Gibney, R. T. & Ronco, C. A proposed algorithm for initiation of renal replacement therapy in adult critically ill patients. Crit. Care 13, 317 (2009).
Uchino, S. What is 'BEST' RRT practice? Contrib. Nephrol. 165, 244–250 (2010).
Ostermann, M. & Chang, R. W. Correlation between parameters at initiation of renal replacement therapy and outcome in patients with acute kidney injury. Crit. Care 13, R175 (2009).
Vinsonneau, C. et al. Continuous venovenous haemodiafiltration versus intermittent haemodialysis for acute renal failure in patients with multiple-organ dysfunction syndrome: a multicentre randomised trial. Lancet 368, 379–385 (2006).
RENAL Replacement Therapy Study Investigators. Intensity of continuous renal-replacement therapy in critically ill patients. N. Engl. J. Med. 361, 1627–1638 (2009).
VA/NIH Acute Renal Failure Trial Network. Intensity of renal support in critically ill patients with acute kidney injury. N. Engl. J. Med. 359, 7–20 (2008).
Kellum, J. A. & Ronco, C. Dialysis: results of RENAL—what is the optimal CRRT target dose? Nat. Rev. Nephrol. 6, 191–192 (2010).
Vesconi, S. et al. for the DOse REsponse Multicentre International collaborative Initiative (DO-RE-MI Study Group). Delivered dose of renal replacement therapy and mortality in critically ill patients with acute kidney injury. Crit. Care 13, R57 (2009).
Ronco, C. Recent evolution of renal replacement therapy in the critically ill patient. Crit. Care 10, 123 (2006).
Honore, P. M., Joannes-Boyau, O., Boer, W. & Collin, V. High-volume hemofiltration in sepsis and SIRS: current concepts and future prospects. Blood Purif. 28, 1–11 (2009).
Ricci, Z. et al. Practice patterns in the management of acute renal failure in the critically ill patient: an international survey. Nephrol. Dial. Transplant. 21, 690–696 (2006).
Cole, L. et al. A phase II randomized, controlled trial of continuous hemofiltration in sepsis. Crit. Care Med. 30, 100–106 (2002).
Payen, D. et al. Impact of continuous venovenous hemofiltration on organ failure during the early phase of severe sepsis: a randomized controlled trial. Crit. Care Med. 37, 803–810 (2009).
Van Wert, R., Friedrich, J. O., Scales, D. C., Wald, R., Adhikari, N. K. for the University of Toronto Acute Kidney Injury Research Group. High-dose renal replacement therapy for acute kidney injury: systematic review and meta-analysis. Crit. Care Med. 38, 1360–1369 (2010).
Morgera, S. et al. Pilot study on the effects of high cutoff hemofiltration on the need for norepinephrine in septic patients with acute renal failure. Crit. Care Med. 34, 2099–2104 (2006).
Morgera, S. et al. Renal replacement therapy with high-cutoff hemofilters: impact of convection and diffusion on cytokine clearances and protein status. Am. J. Kidney Dis. 43, 444–453 (2004).
Naka, T., Haase, M. & Bellomo, R. 'Super high-flux' or 'high cut-off' hemofiltration and hemodialysis. Contrib. Nephrol. 166, 181–189 (2010).
Ronco, C., Piccinni, P. & Kellum, J. Rationale of extracorporeal removal of endotoxin in sepsis: theory, timing and technique. Contrib. Nephrol. 167, 25–23 (2010).
De Nitti, C. et al. Choosing new adsorbents for endogenous ultrapure infusion fluid: performances, safety and flow distribution. Int. J. Artif. Organs 24, 765–776 (2001).
Kellum, J. A., Song, M. & Venkataraman, R. Hemoadsorption removes tumor necrosis factor, interleukin-6, and interleukin-10, reduces nuclear factor-κB DNA binding, and improves short-term survival in lethal endotoxemia. Crit. Care Med. 32, 801–805 (2004).
Hanasawa, K. et al. Selective removal of endotoxin from the blood by extracorporeal hemoperfusion with polymyxin B immobilized fiber. Prog. Clin. Biol. Res. 264, 337–341 (1988).
Cruz, D. N. et al. Effectiveness of polymyxin B-immobilized fiber column in sepsis: a systematic review. Crit. Care 11, R47 (2007).
Vincent, J. L. et al. A pilot-controlled study of a polymyxin B-immobilized hemoperfusion cartridge in patients with severe sepsis secondary to intra-abdominal infection. Shock 23, 400–405 (2005).
Cruz, D. N. et al. Early use of polymyxin B hemoperfusion in abdominal septic shock: the EUPHAS randomized controlled trial. JAMA 301, 2445–2452 (2009).
Kida, Y. Polymyxin B hemoperfusion and mortality in abdominal septic shock. JAMA 302, 1969; author reply 1969–1970 (2009).
Kellum, J. A. & Uchino, S. International differences in the treatment of sepsis: are they justified? JAMA 301, 2496–2497 (2009).
Bellomo, R., Tetta, C. & Ronco, C. Coupled plasma filtration adsorption. Intensive Care Med. 29, 1222–1228 (2003).
Formica, M. et al. Hemodynamic response to coupled plasmafiltration-adsorption in human septic shock. Intensive Care Med. 29, 703–708 (2003).
Cantaluppi, V. et al. Protective effect of resin adsorption on septic plasma-induced tubular injury. Crit. Care 14, R4 (2010).
Ronco, C. & Ricci, Z. Renal replacement therapies: physiological review. Intensive Care Med. 34, 2139–2146 (2008).
Ricci, Z. & Ronco, C. Year in review 2008: critical care—nephrology. Crit. Care 13, 227 (2009).
Author information
Authors and Affiliations
Contributions
Z. Ricci, Angelo Polito and Andrea Polito researched data for this article. C. Ronco and Andrea Polito made a substantial contribution to discussion of the content. Z. Ricci and Angelo Polito wrote the article, and C. Ronco reviewed/edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Ricci, Z., Polito, A., Polito, A. et al. The implications and management of septic acute kidney injury. Nat Rev Nephrol 7, 218–225 (2011). https://doi.org/10.1038/nrneph.2011.15
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2011.15
This article is cited by
-
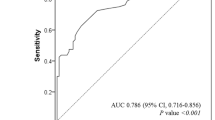
Machine learning algorithm to predict mortality in critically ill patients with sepsis-associated acute kidney injury
Scientific Reports (2023)
-
Maresin conjugates in tissue regeneration-1 suppresses ferroptosis in septic acute kidney injury
Cell & Bioscience (2021)
-
A clinical score to predict mortality in septic acute kidney injury patients requiring continuous renal replacement therapy: the HELENICC score
BMC Anesthesiology (2017)
-
Circulating levels of soluble Fas (sCD95) are associated with risk for development of a nonresolving acute kidney injury subphenotype
Critical Care (2017)
-
Sepsis and septic shock
Nature Reviews Disease Primers (2016)