Abstract
The recognition of a central role for the endothelium in the development of kidney disease or the development of vascular lesions in patients with established renal dysfunction has led to the emergence of methods to test different aspects of endothelium function, including in endothelium injury and repair. Endothelial-cell activation is associated with the shedding of components of the glycocalyx, adhesion molecules and endothelial microparticles into the circulation. This process may eventually result in the detachment of endothelial cells and recruitment of circulating myeloid and progenitor cells that are involved in vascular remodeling and repair. Circulating markers of endothelium activation may therefore represent novel markers of vessel wall injury. This Review describes the biology of these circulating markers of vessel wall injury, the methodologies used to measure them, and their possible relevance to patients with kidney disease.
Key Points
-
Endothelial-cell activation precedes and may stimulate the development of atherosclerotic lesions
-
The very specialized and variable phenotypes of the kidney endothelium contribute to its tendency to be a target organ in systemic disease
-
Activation of endothelial cells is accompanied by the formation and shedding of membrane microparticles and leukocyte adhesion molecules
-
Circulating CD146+ endothelial cells have been described in conditions that are associated with extensive endothelium injury
-
CD34+ progenitor cells are recruited to sites of endothelial injury and their kinetics can potentially be used as a biomarker of vascular injury
-
The clinical value of circulating markers of endothelial activation will depend on the development of standardized protocols for their measurement and insight into their quantitative relationship with clinical outcome
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Deanfield, J. E., Halcox, J. P. & Rabelink, T. J. Endothelial function and dysfunction: testing and clinical relevance. Circulation 115, 1285–1295 (2007).
Csiszar, A. et al. Regulation of bone morphogenetic protein-2 expression in endothelial cells: role of nuclear factor-κB activation by tumor necrosis factor-α, H2O2, and high intravascular pressure. Circulation 111, 2364–2372 (2005).
Demer, L. L., Tintut, Y. & Parhami, F. Novel mechanisms in accelerated vascular calcification in renal disease patients. Curr. Opin. Nephrol. Hypertens. 11, 437–443 (2002).
Shao, J. S., Cheng, S. L., Sadhu, J. & Towler, D. A. Inflammation and the osteogenic regulation of vascular calcification: a review and perspective. Hypertension 55, 579–592 (2010).
Haraldsson, B., Nyström, J. & Deen, W. M. Properties of the glomerular barrier and mechanisms of proteinuria. Physiol. Rev. 88, 451–487 (2008).
Eremina, V. et al. Glomerular-specific alterations of VEGF-A expression lead to distinct congenital and acquired renal diseases. J. Clin. Invest. 111, 707–716 (2003).
Pannabecker, T. L. & Dantzler, W. H. Three-dimensional architecture of inner medullary vasa recta. Am. J. Physiol. Renal Physiol. 290, F1355–F1366 (2006).
Moffat, D. B. The fine structure of the blood vessels of the renal medulla with particular reference to the control of the medullary circulation. J. Ultrastruct. Res. 19, 532–545 (1967).
Nangaku, M. & Couser, W. G. Mechanisms of immune-deposit formation and the mediation of immune renal injury. Clin. Exp. Nephrol. 9, 183–191 (2005).
Okuda, T. et al. Targeted disruption of Gb3/CD77 synthase gene resulted in the complete deletion of globo-series glycosphingolipids and loss of sensitivity to verotoxins. J. Biol. Chem. 281, 10230–10235 (2006).
Govers, R. & Rabelink, T. J. Cellular regulation of endothelial nitric oxide synthase. Am. J. Physiol. Renal Physiol. 280, F193–F206 (2001).
Stamler, J. S., Lamas, S. & Fang, F. C. Nitrosylation. the prototypic redox-based signaling mechanism. Cell 106, 675–683 (2001).
Rabelink, T. J. & Luscher, T. F. Endothelial nitric oxide synthase: host defense enzyme of the endothelium? Arterioscler. Thromb. Vasc. Biol. 26, 267–271 (2006).
Selemidis, S., Sobey, C. G., Wingler, K., Schmidt, H. H. & Drummond, G. R. NADPH oxidases in the vasculature: molecular features, roles in disease and pharmacological inhibition. Pharmacol. Ther. 120, 254–291 (2008).
Wever, R. M., van Dam, T., van Rijn, H. J., de Groot, F. & Rabelink, T. J. Tetrahydrobiopterin regulates superoxide and nitric oxide generation by recombinant endothelial nitric oxide synthase. Biochem. Biophys. Res. Commun. 237, 340–344 (1997).
Werner, E. R., Gorren, A. C., Heller, R., Werner-Felmayer, G. & Mayer, B. Tetrahydrobiopterin and nitric oxide: mechanistic and pharmacological aspects. Exp. Biol. Med. (Maywood) 228, 1291–1302 (2003).
Chalupsky, K. & Cai, H. Endothelial dihydrofolate reductase: critical for nitric oxide bioavailability and role in angiotensin II uncoupling of endothelial nitric oxide synthase. Proc. Natl Acad. Sci. USA 102, 9056–9061 (2005).
Crabtree, M. J., Tatham, A. L., Hale, A. B., Alp, N. J. & Channon, K. M. Critical role for tetrahydrobiopterin recycling by dihydrofolate reductase in regulation of endothelial nitric-oxide synthase coupling: relative importance of the de novo biopterin synthesis versus salvage pathways. J. Biol. Chem. 284, 28128–28136 (2009).
Ryter, S. W., Alam, J. & Choi, A. M. Heme oxygenase-1/carbon monoxide: from basic science to therapeutic applications. Physiol. Rev. 86, 583–650 (2006).
Topper, J. N., Cai, J., Falb, D. & Gimbrone, M. A. Jr. Identification of vascular endothelial genes differentially responsive to fluid mechanical stimuli: cyclooxygenase-2, manganese superoxide dismutase, and endothelial cell nitric oxide synthase are selectively up-regulated by steady laminar shear stress. Proc. Natl Acad. Sci. USA 93, 10417–10422 (1996).
Hojo, Y. et al. Fluid shear stress attenuates hydrogen peroxide-induced c-Jun NH2-terminal kinase activation via a glutathione reductase-mediated mechanism. Circ. Res. 91, 712–718 (2002).
Cai, H. & Harrison, D. G. Endothelial dysfunction in cardiovascular diseases: the role of oxidant stress. Circ. Res. 87, 840–844 (2000).
Baylis, C. Nitric oxide deficiency in chronic kidney disease. Am. J. Physiol. Renal Physiol. 294, F1–F9 (2008).
Dimmeler, S., Haendeler, J., Rippmann, V., Nehls, M. & Zeiher, A. M. Shear stress inhibits apoptosis of human endothelial cells. FEBS Lett. 399, 71–74 (1996).
Dekker, R. J. et al. Prolonged fluid shear stress induces a distinct set of endothelial cell genes, most specifically lung Krüppel-like factor (KLF2). Blood 100, 1689–1698 (2002).
Chen, X. L. et al. Laminar flow induction of antioxidant response element-mediated genes in endothelial cells. A novel anti-inflammatory mechanism. J. Biol. Chem. 278, 703–711 (2003).
Fledderus, J. O. et al. KLF2 primes the antioxidant transcription factor Nrf2 for activation in endothelial cells. Arterioscler. Thromb. Vasc. Biol. 28, 1339–1346 (2008).
Kraft, A. D., Johnson, D. A. & Johnson, J. A. Nuclear factor E2-related factor 2-dependent antioxidant response element activation by tert-butylhydroquinone and sulforaphane occurring preferentially in astrocytes conditions neurons against oxidative insult. J. Neurosci. 24, 1101–1112 (2004).
Gaengel, K., Genové, G., Armulik, A. & Betsholtz, C. Endothelial-mural cell signaling in vascular development and angiogenesis. Arterioscler. Thromb. Vasc. Biol. 29, 630–638 (2009).
Díaz-Flores, L. et al. Pericytes. Morphofunction, interactions and pathology in a quiescent and activated mesenchymal cell niche. Histol. Histopathol. 24, 909–969 (2009).
Yao, D. et al. High glucose increases angiopoietin-2 transcription in microvascular endothelial cells through methylglyoxal modification of mSin3A. J. Biol. Chem. 282, 31038–31045 (2007).
Chen, J. X. & Stinnett, A. Disruption of Ang-1/Tie-2 signaling contributes to the impaired myocardial vascular maturation and angiogenesis in type II diabetic mice. Arterioscler. Thromb. Vasc. Biol. 28, 1606–1613 (2008).
Lee, K. W., Lip, G. Y. & Blann, A. D. Plasma angiopoietin-1, angiopoietin-2, angiopoietin receptor tie-2, and vascular endothelial growth factor levels in acute coronary syndromes. Circulation 110, 2355–2360 (2004).
Pfister, F. et al. Pericyte migration: a novel mechanism of pericyte loss in experimental diabetic retinopathy. Diabetes 57, 2495–2502 (2008).
Ferrario, F. & Rastaldi, M. P. Histopathological atlas of renal diseases: diabetic nephropathy. J. Nephrol. 19, 1–5 (2006).
Hidai, C., Kawana, M., Kitano, H. & Kokubun, S. Discoidin domain of Del1 protein contributes to its deposition in the extracellular matrix. Cell Tissue Res. 330, 83–95 (2007).
Weinbaum, S., Tarbell, J. M. & Damiano, E. R. The structure and function of the endothelial glycocalyx layer. Annu. Rev. Biomed. Eng. 9, 121–167 (2007).
Tarbell, J. M. & Ebong, E. E. The endothelial glycocalyx: a mechano-sensor and -transducer. Sci. Signal 1, pt8 (2008).
Henry, C. B. & Duling, B. R. TNF-α increases entry of macromolecules into luminal endothelial cell glycocalyx. Am. J. Physiol. Heart Circ. Physiol. 279, H2815–H2823 (2000).
Mulivor, A. W. & Lipowsky, H. H. Inflammation- and ischemia-induced shedding of venular glycocalyx. Am. J. Physiol. Heart Circ. Physiol. 286, H1672–H1680 (2004).
Fitzgerald, M. L., Wang, Z., Park, P. W., Murphy, G. & Bernfield, M. Shedding of syndecan-1 and -4 ectodomains is regulated by multiple signaling pathways and mediated by a TIMP-3-sensitive metalloproteinase. J. Cell Biol. 148, 811–824 (2000).
Colburn, P., Kobayashi, E. & Buonassisi, V. Depleted level of heparan sulfate proteoglycan in the extracellular matrix of endothelial cell cultures exposed to endotoxin. J. Cell Physiol. 159, 121–130 (1994).
Bruegger, D. et al. Shedding of the endothelial glycocalyx during cardiac surgery: on-pump versus off-pump coronary artery bypass graft surgery. J. Thorac. Cardiovasc. Surg. 138, 1445–1447 (2009).
Wang, J. B. et al. Insulin increases shedding of syndecan-1 in the serum of patients with type 2 diabetes mellitus. Diabetes Res. Clin. Pract. 86, 83–88 (2009).
Bardin, N. et al. Soluble CD146, a novel endothelial marker, is increased in physiopathological settings linked to endothelial junctional alteration. Thromb. Haemost. 90, 915–920 (2003).
Blankenberg, S. et al. Circulating cell adhesion molecules and death in patients with coronary artery disease. Circulation 104, 1336–1342 (2001).
Frijns, C. J. et al. Soluble adhesion molecules reflect endothelial cell activation in ischemic stroke and in carotid atherosclerosis. Stroke 28, 2214–2218 (1997).
Harrington, E. O., Stefanec, T., Newton, J. & Rounds, S. Release of soluble E-selectin from activated endothelial cells upon apoptosis. Lung 184, 259–266 (2006).
Hwang, S. J. et al. Circulating adhesion molecules VCAM-1, ICAM-1, and E-selectin in carotid atherosclerosis and incident coronary heart disease cases: the Atherosclerosis Risk In Communities (ARIC) study. Circulation 96, 4219–4225 (1997).
Tzoulaki, I. et al. C-reactive protein, interleukin-6, and soluble adhesion molecules as predictors of progressive peripheral atherosclerosis in the general population: Edinburgh Artery Study. Circulation 112, 976–983 (2005).
Arici, M. et al. Association of mineral metabolism with an increase in cellular adhesion molecules: another link to cardiovascular risk in maintenance haemodialysis? Nephrol. Dial. Transplant. 21, 999–1005 (2006).
Malatino, L. S. et al. Circulating E-selectin as a risk marker in patients with end-stage renal disease. J. Intern. Med. 262, 479–487 (2007).
May, A. E. et al. Engagement of glycoprotein IIb/IIIa (αIIbβ3) on platelets upregulates CD40L and triggers CD40L-dependent matrix degradation by endothelial cells. Circulation 106, 2111–2117 (2002).
de Boer, H. C. et al. Fibrin and activated platelets cooperatively guide stem cells to a vascular injury and promote differentiation towards an endothelial cell phenotype. Arterioscler. Thromb. Vasc. Biol. 26, 1653–1659 (2006).
Langer, H. F. et al. Platelet-induced differentiation of endothelial progenitor cells. Semin. Thromb. Hemost. 33, 136–143 (2007).
Massberg, S. et al. Platelets secrete stromal cell-derived factor 1α and recruit bone marrow-derived progenitor cells to arterial thrombi in vivo. J. Exp. Med. 203, 1221–1233 (2006).
von Hundelshausen, P. & Weber, C. Platelets as immune cells: bridging inflammation and cardiovascular disease. Circ. Res. 100, 27–40 (2007).
Hugel, B., Martínez, M. C., Kunzelmann, C. & Freyssinet, J. M. Membrane microparticles: two sides of the coin. Physiology (Bethesda) 20, 22–27 (2005).
Leventis, P. A. & Grinstein, S. The distribution and function of phosphatidylserine in cellular membranes. Annu. Rev. Biophys. doi:10.101146/annurev.biophys.093008.131234.
Morel, O. et al. Procoagulant microparticles: disrupting the vascular homeostasis equation? Arterioscler. Thromb. Vasc. Biol. 26, 2594–2604 (2006).
Combes, V. et al. In vitro generation of endothelial microparticles and possible prothrombotic activity in patients with lupus anticoagulant. J. Clin. Invest. 104, 93–102 (1999).
Leroyer, A. S. et al. Cellular origins and thrombogenic activity of microparticles isolated from human atherosclerotic plaques. J. Am. Coll. Cardiol. 49, 772–777 (2007).
Sapet, C. et al. Thrombin-induced endothelial microparticle generation: identification of a novel pathway involving ROCK-II activation by caspase-2. Blood 108, 1868–1876 (2006).
Simoncini, S. et al. TRAIL/Apo2L mediates the release of procoagulant endothelial microparticles induced by thrombin in vitro: a potential mechanism linking inflammation and coagulation. Circ. Res. 104, 943–951 (2009).
Sabatier, F. et al. Interaction of endothelial microparticles with monocytic cells in vitro induces tissue factor-dependent procoagulant activity. Blood 99, 3962–3970 (2002).
Duval, A. et al. Endothelial dysfunction in systemic lupus patients with low disease activity: evaluation by quantification and characterization of circulating endothelial microparticles, role of anti-endothelial cell antibodies. Rheumatology (Oxford) doi:10.1093/rheumatology/keq041.
Mallat, Z. et al. Elevated levels of shed membrane microparticles with procoagulant potential in the peripheral circulating blood of patients with acute coronary syndromes. Circulation 101, 841–843 (2000).
Erdbruegger, U. et al. Diagnostic role of endothelial microparticles in vasculitis. Rheumatology (Oxford) 47, 1820–1825 (2008).
Koga, H. et al. Elevated levels of VE-cadherin-positive endothelial microparticles in patients with type 2 diabetes mellitus and coronary artery disease. J. Am. Coll. Cardiol. 45, 1622–1630 (2005).
Amabile, N. et al. Circulating endothelial microparticles are associated with vascular dysfunction in patients with end-stage renal failure. J. Am. Soc. Nephrol. 16, 3381–3388 (2005).
Faure, V. et al. Elevation of circulating endothelial microparticles in patients with chronic renal failure. J. Thromb. Haemost. 4, 566–573 (2006).
Al-Massarani, G. et al. Kidney transplantation decreases the level and procoagulant activity of circulating microparticles. Am. J. Transplant. 9, 550–557 (2009).
Amabile, N., Boulanger, C. M., Guerin, A. P., Tedgui, A. & London, G. M. Circulating endothelial microparticles: a novel biomarker for prediction of subsequent death and cardiovascular events in end-stage renal disease [abstract 4871]. Circulation 120, S1010 (2009).
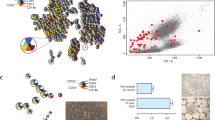
Mancuso, P. et al. Validation of a standardized method for enumerating circulating endothelial cells and progenitors: flow cytometry and molecular and ultrastructural analyses. Clin. Cancer Res. 15, 267–273 (2009).
Blann, A. D. et al. Circulating endothelial cells. Biomarker of vascular disease. Thromb. Haemost. 93, 228–235 (2005).
Woywodt, A. et al. Circulating endothelial cells as markers for ANCA-associated small-vessel vasculitis. Lancet 361, 206–210 (2003).
Elshal, M. F., Khan, S. S., Takahashi, Y., Solomon, M. A. & McCoy, J. P. Jr. CD146 (Mel-CAM), an adhesion marker of endothelial cells, is a novel marker of lymphocyte subset activation in normal peripheral blood. Blood 106, 2923–2924 (2005).
Sorrentino, A. et al. Isolation and characterization of CD146+ multipotent mesenchymal stromal cells. Exp. Hematol. 36, 1035–1046 (2008).
Woywodt, A. et al. Isolation and enumeration of circulating endothelial cells by immunomagnetic isolation: proposal of a definition and a consensus protocol. J. Thromb. Haemost. 4, 671–677 (2006).
Koç, M., Bihorac, A. & Segal, M. S. Circulating endothelial cells as potential markers of the state of the endothelium in hemodialysis patients. Am. J. Kidney Dis. 42, 704–712 (2003).
Woywodt, A. et al. Elevated numbers of circulating endothelial cells in renal transplant recipients. Transplantation 76, 1–4 (2003).
Woywodt, A. et al. Circulating endothelial cells are a novel marker of cyclosporine-induced endothelial damage. Hypertension 41, 720–723 (2003).
Mohamed, A. S. et al. Circulating endothelial cells in renal transplant recipients. Transplant. Proc. 37, 2387–2390 (2005).
Al-Massarani, G. et al. Impact of immunosuppressive treatment on endothelial biomarkers after kidney transplantation. Am. J. Transplant. 8, 2360–2367 (2008).
Asahara, T. et al. Isolation of putative progenitor endothelial cells for angiogenesis. Science 275, 964–967 (1997).
Hristov, M. & Weber, C. Endothelial progenitor cells in vascular repair and remodeling. Pharmacol. Res. 58, 148–151 (2008).
Rookmaaker, M. B. et al. Bone-marrow-derived cells contribute to glomerular endothelial repair in experimental glomerulonephritis. Am. J. Pathol. 163, 553–562 (2003).
Li, J., Deane, J. A., Campanale, N. V., Bertram, J. F. & Ricardo, S. D. Blockade of p38 mitogen-activated protein kinase and TGF-β1/Smad signaling pathways rescues bone marrow-derived peritubular capillary endothelial cells in adriamycin-induced nephrosis. J. Am. Soc. Nephrol. 17, 2799–2811 (2006).
Walter, D. H. et al. Statin therapy accelerates reendothelialization: a novel effect involving mobilization and incorporation of bone marrow-derived endothelial progenitor cells. Circulation 105, 3017–3024 (2002).
Foteinos, G., Hu, Y., Xiao, Q., Metzler, B. & Xu, Q. Rapid endothelial turnover in atherosclerosis-prone areas coincides with stem cell repair in apolipoprotein E-deficient mice. Circulation 117, 1856–1863 (2008).
Tepper, O. M. et al. Adult vasculogenesis occurs through in situ recruitment, proliferation, and tubulization of circulating bone marrow-derived cells. Blood 105, 1068–1077 (2005).
Gao, D. et al. Endothelial progenitor cells control the angiogenic switch in mouse lung metastasis. Science 319, 195–198 (2008).
Purhonen, S. et al. Bone marrow-derived circulating endothelial precursors do not contribute to vascular endothelium and are not needed for tumor growth. Proc. Natl Acad. Sci. USA 105, 6620–6625 (2008).
Perry, T. E. et al. Bone marrow-derived cells do not repair endothelium in a mouse model of chronic endothelial cell dysfunction. Cardiovasc. Res. 84, 317–325 (2009).
Aicher, A., Heeschen, C. & Dimmeler, S. The role of NOS3 in stem cell mobilization. Trends Mol. Med. 10, 421–425 (2004).
Madlambayan, G. J. et al. Bone marrow stem and progenitor cell contribution to neovasculogenesis is dependent on model system with SDF-1 as a permissive trigger. Blood 114, 4310–4319 (2009).
Hirschi, K. K., Ingram, D. A. & Yoder, M. C. Assessing identity, phenotype, and fate of endothelial progenitor cells. Arterioscler. Thromb. Vasc. Biol. 28, 1584–1595 (2008).
Kalka, C. et al. Transplantation of ex vivo expanded endothelial progenitor cells for therapeutic neovascularization. Proc. Natl Acad. Sci. USA 97, 3422–3427 (2000).
Urbich, C. et al. Relevance of monocytic features for neovascularization capacity of circulating endothelial progenitor cells. Circulation 108, 2511–2516 (2003).
Loomans, C. J. et al. Angiogenic murine endothelial progenitor cells are derived from a myeloid bone marrow fraction and can be identified by endothelial NO synthase expression. Arterioscler. Thromb. Vasc. Biol. 26, 1760–1767 (2006).
Schaper, W. Collateral circulation: past and present. Basic Res. Cardiol. 104, 5–21 (2009).
Grunewald, M. et al. VEGF-induced adult neovascularization: recruitment, retention, and role of accessory cells. Cell 124, 175–189 (2006).
Prokopi, M. et al. Proteomic analysis reveals presence of platelet microparticles in endothelial progenitor cell cultures. Blood 114, 723–732 (2009).
Sakurai, Y., Ohgimoto, K., Kataoka, Y., Yoshida, N. & Shibuya, M. Essential role of Flk-1 (VEGF receptor 2) tyrosine residue 1173 in vasculogenesis in mice. Proc. Natl Acad. Sci. USA 102, 1076–1081 (2005).
Shalaby, F. et al. Failure of blood-island formation and vasculogenesis in Flk-1-deficient mice. Nature 376, 62–66 (1995).
Rookmaaker, M. B. et al. CD34+ cells home, proliferate, and participate in capillary formation, and in combination with CD34− cells enhance tube formation in a 3-dimensial matrix. Arterioscler. Thromb. Vasc. Biol. 25, 1843–1850 (2005).
Peichev, M. et al. Expression of VEGFR-2 and AC133 by circulating human CD34+ cells identifies a population of functional endothelial precursors. Blood 95, 952–958 (2000).
Pelosi, E. et al. Identification of the hemangioblast in postnatal life. Blood 100, 3203–3208 (2002).
Fadini, G. P. et al. Circulating CD34+ cells, metabolic syndrome, and cardiovascular risk. Eur. Heart J. 27, 2247–2255 (2006).
Bahlmann, F. H. et al. Endothelial progenitor cell proliferation and differentiation is regulated by erythropoietin. Kidney Int. 64, 1648–1652 (2003).
de Groot, K. et al. Uremia causes endothelial progenitor cell deficiency. Kidney Int. 66, 641–646 (2004).
de Groot, K. et al. Kidney graft function determines endothelial progenitor cell number in renal transplant recipients. Transplantation 79, 941–945 (2005).
Rodríguez-Ayala, E. et al. Imbalance between detached circulating endothelial cells and endothelial progenitor cells in chronic kidney disease. Blood Purif. 24, 196–202 (2006).
Surdacki, A. et al. Association between endothelial progenitor cell depletion in blood and mild-to-moderate renal insufficiency in stable angina. Nephrol. Dial. Transplant. 23, 2265–2273 (2008).
Westerweel, P. E. et al. End-stage renal disease causes an imbalance between endothelial and smooth muscle progenitor cells. Am. J. Physiol. Renal Physiol. 292, F1132–F1140 (2007).
Krenning, G. et al. Endothelial progenitor cell dysfunction in patients with progressive chronic kidney disease. Am. J. Physiol. Renal Physiol. 296, F1314–F1322 (2009).
Dimmeler, S. & Zeiher, A. M. Vascular repair by circulating endothelial progenitor cells: the missing link in atherosclerosis? J. Mol. Med. 82, 671–677 (2004).
Heissig, B. et al. Recruitment of stem and progenitor cells from the bone marrow niche requires MMP-9 mediated release of kit-ligand. Cell 109, 625–637 (2002).
Aicher, A. et al. Essential role of endothelial nitric oxide synthase for mobilization of stem and progenitor cells. Nat. Med. 9, 1370–1376 (2003).
Murphy, C. et al. Vascular dysfunction and reduced circulating endothelial progenitor cells in young healthy UK South Asian men. Arterioscler. Thromb. Vasc. Biol. 27, 936–942 (2007).
Heiss, C. et al. Impaired progenitor cell activity in age-related endothelial dysfunction. J. Am. Coll. Cardiol. 45, 1441–1448 (2005).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Rabelink, T., de Boer, H. & van Zonneveld, A. Endothelial activation and circulating markers of endothelial activation in kidney disease. Nat Rev Nephrol 6, 404–414 (2010). https://doi.org/10.1038/nrneph.2010.65
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2010.65
This article is cited by
-
VascuFit: vascular effects of non-linear periodized exercise training in sedentary adults with elevated cardiovascular risk – protocol for a randomized controlled trial
BMC Cardiovascular Disorders (2022)
-
Serum levels of the endothelial glycocalyx constituents and the early failure of forearm autologous arteriovenous fistulas in end-stage renal disease patients: a prospective cohort study
International Urology and Nephrology (2020)
-
The double edge of anti-CD40 siRNA therapy: It increases renal microcapillar density but favours the generation of an inflammatory milieu in the kidneys of ApoE−/− mice
Journal of Inflammation (2019)
-
Endothelium structure and function in kidney health and disease
Nature Reviews Nephrology (2019)
-
Chronic kidney failure mineral bone disorder leads to a permanent loss of hematopoietic stem cells through dysfunction of the stem cell niche
Scientific Reports (2018)