Abstract
End-stage renal disease (ESRD) is an increasing health problem worldwide. Given the increasing prevalence of this disease, the high cost of hemodialysis treatment and the burden of hemodialysis on a patient's life, more research on improving the clinical outcomes and the quality of life of hemodialysis-treated patients is warranted. Sleep disturbances are much more prevalent in the dialysis population than in the general population. Several studies investigating the effect and importance of sleep problems on quality of life in dialysis patients revealed that sleep disturbances have a major influence on the vitality and general health of these patients. Sleep disturbances in this patient group are caused both by the pathology of the renal disease and by the dialysis treatment itself. This Review focuses on circadian sleep–wake rhythm disturbances in individuals with ESRD. The possible external and internal influences on sleep–wake rhythmicity in patients with ESRD, such as the effect of dialysis, medications, melatonin and biochemical parameters, are presented. In addition, possible approaches for strengthening the synchronization of the circadian sleep–wake rhythm, such as nocturnal hemodialysis, exogenous melatonin, dialyzate temperature, exogenous erythropoietin, use of bright light and exercise during dialysis treatment, are explored. Further research in this area is warranted, and a greater awareness of sleep problems is needed to improve the quality of life of patients with ESRD.
Key Points
-
Sleep disturbances are much more prevalent in patients with end-stage renal disease (ESRD) than in the general population
-
Several studies on the impact and importance of sleep problems on quality of life in patients on dialysis revealed that sleep disturbances have a major effect on the vitality and general health of these patients
-
Sleep disturbances in patients on dialysis might be caused by the pathology of the renal disease as well as by the dialysis treatment itself
-
External and internal factors that might be associated with disrupted sleep–wake rhythmicity in patients with ESRD include dialysis, medications, melatonin rhythm and biochemical parameters
-
Approaches that might be useful in treating disturbances in the circadian sleep–wake rhythm in patients with ESRD include nocturnal dialysis, exogenous melatonin, lowering dialyzate temperature, exogenous erythropoietin, bright light and intradialytic exercise
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Parker, K. P. Sleep disturbances in dialysis patients. Sleep Med. Rev. 7, 131–143 (2003).
Molzahn, A. E., Northcott, H. C. & Dossetor, J. B. Quality of life of individuals with end stage renal disease: perceptions of patients, nurses, and physicians. ANNA J. 24, 325–333 (1997).
Parker, K. P., Bliwise, D. L. & Rye, D. B. Hemodialysis disrupts basic sleep regulatory mechanisms: building hypotheses. Nurs. Res. 49, 327–332 (2000).
Cuninkova, L. & Brown, S. A. Peripheral circadian oscillators: interesting mechanisms and powerful tools. Ann. N. Y. Acad. Sci. 1129, 358–370 (2008).
Yoo, S. H. et al. PERIOD2::LUCIFERASE real-time reporting of circadian dynamics reveals persistent circadian oscillations in mouse peripheral tissues. Proc. Natl Acad. Sci. USA 101, 5339–5346 (2004).
Borbely, A. A. & Achermann, P. Concepts and models of sleep regulation: an overview. J. Sleep Res. 1, 63–79 (1992).
McGinty, D. & Szymusiak, R. Sleep promoting mechanisms in mammals. In Principles and Practice of Sleep Medicine (Eds Kryger, M. H., Roth, T. & Dement, W. C.) 169–184 (Elsevier Saunders, Philadelphia, 2005).
American Academy of Sleep Medicine. International classification of sleep disorders, Diagnostic and coding manual 2nd edn. (American Academy of Sleep Medicine, Westchester, IL, 2005).
Reid, K. J. & Zee, P. C. Circadian disorders of the sleep-wake cycle. In Principles and Practice of Sleep Medicine (Eds Kryger, M. H., Roth, T. & Dement, W. C.) 691–702 (Elsevier Saunders, Philadelphia, 2005).
Carskadon, M. A. & Dement, W. C. Normal human sleep: an overview. In Principles and Practice of Sleep Medicine (Eds Kryger, M. H., Roth, T. & Dement, W. C.) 13–23 (Elsevier Saunders, Philadelphia, 2005).
Hirshkowitz, M. Normal human sleep: an overview. Med. Clin. North Am. 88, 551–565 (2004).
Bonnet, M. H. Acute sleep deprivation. In Principles and Practice of Sleep Medicine (Eds Kryger, M. H., Roth, T. & Dement, W. C.) 59–60 (Elsevier Saunders, Philadelphia, 2005).
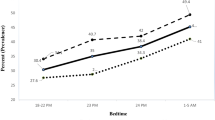
Koch, B. C., Nagtegaal, J. E., Hagen, E. C., ter Wee, P. M. & Kerkhof, G. A. Different melatonin rhythms and sleep-wake rhythms in patients on peritoneal dialysis, daytime hemodialysis and nocturnal hemodialysis. Sleep Med. (in press).
Carskadon, M. A. & Rechtschaffen, A. Monitoring and staging human sleep. In Principles and Practice of Sleep Medicine (Eds Kryger, M. H., Roth, T. & Dement, W. C.) 1359–1378 (Elsevier Saunders, Philadelphia, 2005).
Claustrat, B., Brun, J. & Chazot, G. The basic physiology and pathophysiology of melatonin. Sleep Med. Rev. 9, 11–24 (2005).
Scheer, F. A. & Czeisler, C. A. Melatonin, sleep, and circadian rhythms. Sleep Med. Rev. 9, 5–9 (2005).
Konturek, S. J., Konturek, P. C., Brzozowski, T. & Bubenik, G. A. Role of melatonin in upper gastrointestinal tract. J. Physiol. Pharmacol. 58 (Suppl. 6), 23–52 (2007).
Waldhauser, F. & Dietzel, M. Daily and annual rhythms in human melatonin secretion: role in puberty control. Ann. N. Y. Acad. Sci. 453, 205–214 (1985).
Iguichi, H., Kato, K. I. & Ibayashi, H. Age-dependent reduction in serum melatonin concentrations in healthy human subjects. J. Clin. Endocrinol. Metab. 55, 27–29 (1982).
Zhdanova, I. V. & Wurtman, R. J. Efficacy of melatonin as a sleep-promoting agent. J. Biol. Rhythms 12, 644–650 (1997).
Czeisler, C. A., Buxton, O. M. & Singh Khalsa, S. B. The human circadian timing system and sleep-wake regulation. In Principles and Practice of Sleep Medicine (Eds Kryger, M. H., Roth, T. & Dement, W. C.) 388 (Elsevier Saunders, Philadelphia, 2005).
Lewy, A. J. & Sack, R. L. The dim light melatonin onset as a marker for circadian phase position. Chronobiol. Int. 6, 93–102 (1989).
Akerstedt, T., Fröberg, J. E., Friberg, Y. & Wetterberg, L. Melatonin excretion, body temperature and subjective arousal during 64 hours of sleep deprivation. Psychoneuroendocrinology 4, 219–225 (1979).
Tzischinsky, O., Shlitner, A. & Lavie, P. l. The association between the nocturnal sleep gate and nocturnal onset of urinary 6-sulfatoxymelatonin. J. Biol. Rhythms 8, 199–209 (1993).
Nagtegaal, E. et al. Correlation between concentrations of melatonin in saliva and serum in patients with delayed sleep phase syndrome. Ther. Drug Monit. 20, 181–183 (1998).
Cagnacci, A., Elliott, J. A. & Yen, S. S. Melatonin: a major regulator of the circadian rhythm of core temperature in humans. J. Clin. Endocrinol. Metab. 75, 447–452 (1992).
Ekmekcioglu, C. Melatonin receptors in humans: biological role and clinical relevance. Biomed. Pharmacother. 60, 97–108 (2006).
Markus, R. P., Ferreira, Z. S., Fernandes, P. A. & Cecon, E. The immune-pineal axis: a shuttle between endocrine and paracrine melatonin sources. Neuroimmunomodulation 14, 126–133 (2007).
Walker, S., Fine, A. & Kryger, M. H. Sleep complaints are common in a dialysis unit. Am. J. Kidney Dis. 26, 751–756 (1995).
Mucsi, I. et al. Sleep disorders and illness intrusiveness in patients on chronic dialysis. Nephrol. Dial. Transplant. 19, 1815–1822 (2004).
Sabbatini, M. A. et al. Insomnia in maintenance haemodialysis patients. Nephrol. Dial. Transplant. 17, 852–856 (2002).
Merlino, G. et al. Sleep disorders in patients with end-stage renal disease undergoing dialysis therapy. Nephrol. Dial. Transplant. 21, 184–190 (2006).
Koch, B. C. et al. Subjective sleep efficiency of haemodialysis patients. Clin. Nephrol. 70, 411–418 (2008).
Parker, K. P., Bliwise, D. L., Bailey, J. L. & Rye, D. B. Polysomnographic measures of nocturnal sleep in patients on chronic, intermittent daytime haemodialysis vs those with chronic kidney disease. Nephrol. Dial. Transplant. 20, 1422–1428 (2005).
Mendelssohn, D. et al. Sleep disorders and quality of life in chronic kidney disease patients in the predialysis stage [abstract]. J. Am. Soc. Nephrol. 15, 132A (2004).
Barrett, B. J., Vavasour, H. M., Major, A. & Parfrey, P. S. Clinical and psychological correlates of somatic symptoms in patients on dialysis. Nephron 55, 10–15 (1990).
Holley, J. L., Nespor, S. & Rault, R. A comparison of reported sleep disorders in patients on chronic hemodialysis and continuous peritoneal dialysis. Am. J. Kidney Dis. 19, 156–161 (1992).
Bro, S. et al. A prospective, randomized multicenter study comparing APD and CAPD treatment. Perit. Dial. Int. 19, 526–533 (1999).
Tang, S. C. et al. Alleviation of sleep apnea in patients with chronic renal failure by nocturnal cycler-assisted peritoneal dialysis compared with conventional continuous ambulatory peritoneal dialysis. J. Am. Soc. Nephrol. 17, 2607–2616 (2006).
Dinarello, C. A. Interleukin-1 and tumor necrosis factor and their naturally occurring antagonists during hemodialysis. Kidney Int. Suppl. 38 (Suppl.), S68–S77 (1992).
Herbelin, A., Nguyen, A. T., Zingraff, J., Ureña, P. & Descamps-Latscha, B. Influence of uremia and hemodialysis on circulating interleukin-1 and tumor necrosis factor α. Kidney Int. 37, 116–125 (1990).
Zaoui, P. & Hakim, R. M. The effects of the dialysis membrane on cytokine release. J. Am. Soc. Nephrol. 4, 1711–1718 (1994).
Lack, L. C. & Lushington, K. The rhythms of human sleep propensity and core body temperature. J. Sleep Res. 5, 1–11 (1996).
Lack, L. C., Gradisar, M., Van Someren, E. J., Wright, H. R. & Lushington, K. The relationship between insomnia and body temperatures. Sleep Med. Rev. 12, 307–317 (2008).
Campbell, S. S., Dawson, D. & Zulley, J. When the human circadian system is caught napping: evidence for endogenous rhythms close to 24 hours. Sleep 16, 638–640 (1993).
Blagg, C. R. Acute complications associated with hemodialysis. In Replacement of Renal Function by Dialysis: a Textbook of Dialysis (Ed. Maher, J. F.) 750–771 (Kluwer Academic, Boston, 1989).
Plum, F. & Posner, J. B. Multifocal, diffuse, and metabolic brain diseases causing stupor or coma. In The Diagnosis of Stupor and Coma (Eds Plum, F. & Posner, J. B.) 177–303 (F. A. Davis, Philadelphia, 1985).
DiFresco, V., Landman, M., Jaber, B. L. & White, A. C. Dialysis disequilibrium syndrome: an unusual cause of respiratory failure in the medical intensive care unit. Intensive Care Med. 26, 628–630 (2000).
Claghorn, J. L., Mathew, R. J., Weinman, M. L. & Hruska, N. Daytime sleepiness in depression. J. Clin. Psychiatry 42, 342–343 (1981).
Stapleton, S. Etiologies and indicators of powerlessness in persons with end-stage renal disease. In Coping with Chronic Illness: Overcoming Powerlessness (Ed. Miller, J. F.) 163–178 (F. A. Davis, Philadelphia, 1992).
Bliwise, D. L., Kutner, N. G., Zhang, R. & Parker, K. P. Survival by time of day of hemodialysis in an elderly cohort. JAMA 286, 2690–2694 (2001).
McAinsh, J. & Cruickshank, J. M. Beta-blockers and central nervous system side effects. Pharmacol. Ther. 46, 163–197 1990).
Koch, B. C. P. et al. Prescription of hypnotics and potentially sleep-disturbing medication in haemodialysis patients [Dutch]. Pharm. Weekblad 25, 132–134 (2008).
The Merck Manual [online] (2006–2008).
Van Den Heuvel, C. J., Reid, K. J. & Dawson, D. Effect of atenolol on nocturnal sleep and temperature in young men: reversal by pharmacological doses of melatonin. Physiol. Behav. 61, 795–802 (1997).
Brismar, K., Hylander, B., Eliasson, K., Rossner, S. & Wetterberg, L. Melatonin secretion related to side effects of β-blockers from the central nervous system. Acta Med. Scand. 223, 525–530 (1988).
Qureshi, A. & Lee-Chiong, T. Jr. Medications and their effects on sleep. Med. Clin. North Am. 88, 751–766 (2004).
Nagtegaal, J. E., Kerkhof, G. A. & Smits, M. G. Chronobiological, clinical and pharmacological aspects of melatonin in human circadian rhythm dysfunction. In Treatise on Pineal Gland and Melatonin (Eds Haldar, C. et al.) 461–489 (Science Publishers, Enfield, 2002).
Glass, J., Lanctôt, K. L., Herrmann, N., Sproule, B. A. & Busto, U. E. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ 331, 1169–1176 (2005).
Vaziri, N. D. Dysregulation of melatonin metabolism in chronic renal insufficiency: role of erythropoietin-deficiency anemia. Kidney Int. 50, 653–656 (1996).
Viljoen, M., Steyn, M. E., van Rensburg, B. W. & Reinach, S. G. Melatonin in chronic renal failure. Nephron 60, 138–143 (1992).
Karasek, M., Szuflet, A., Chrzanowski, W., Zylinska, K. & Swietoslawski, J. Decreased melatonin nocturnal concentrations in hemodialyzed patients. Neuro Endocrinol. Lett. 26, 653–656 (2005).
Karasek, M., Szuflet, A., Chrzanowski, W., Zylinska, K. & Swietoslawski, J. Circadian serum melatonin profiles in patients suffering from chronic renal failure. Neuro Endocrinol. Lett. 23 (Suppl. 1), 97–102 (2002).
Vaziri, N. D., Oveisi, F., Wierszbiezki, M., Shaw, V. & Sporty, L. D. Serum melatonin and 6-sulfatoxymelatonin in end-stage renal disease: effect of hemodialysis. Artif. Organs 17, 764–769 (1993).
Geron, R. et al. Polymorphonuclear leucocyte priming in long intermittent nocturnal haemodialysis patients—is melatonin a player? Nephrol. Dial. Transplant. 21, 3196–3201 (2006).
Souchet, T. et al. Impaired regulation of β-2-adrenergic receptor density in mononuclear cells during chronic renal failure. Biochem. Pharmacol. 35, 2513–2519 (1986).
Holmes, E. W., Hojvat, S. A., Kahn, S. E. & Bermes, E. W. Jr. Testicular dysfunction in experimental chronic renal insufficiency: a deficiency of nocturnal pineal N-acetyltransferase activity. Br. J. Exp. Pathol. 70, 349–356 (1989).
Ulfberg, J., Micic, S. & Strøm, J. Afternoon serum-melatonin in sleep disordered breathing. J. Intern. Med. 244, 163–168 (1998).
Hanly, P. Sleep apnea and daytime sleepiness in end-stage renal disease. Semin. Dial. 17, 109–114 (2004).
Hanly, P., Gabor, J. Y., Chan, C. & Pierratos, A. Daytime sleepiness in patients with CRF: impact of nocturnal hemodialysis. Am. J. Kidney Dis. 41, 403–410 (2003).
Ferchland, A. et al. Effects of uremic plasma on α- and β-adrenoceptor subtypes. Nephron 80, 46–50 (1998).
Unruh, M. L., Hartunian, M. G., Chapman, M. M. & Jaber, B. L. Sleep quality and clinical correlates in patients on maintenance dialysis. Clin. Nephrol. 59, 280–288 (2003).
Wide, L., Bengtsson, C. & Birgegård, G. Circadian rhythm of erythropoietin in human serum. Br. J. Haematol. 72, 85–90 (1989).
Koopman, M. G. et al. Circadian rhythm of glomerular filtration rate in normal individuals. Clin. Sci. (Lond.) 77, 105–111 (1989).
Roberts, D. & Smith, D. J. Erythropoietin does not demonstrate circadian rhythm in healthy men. J. Appl. Physiol. 80, 847–851 (1996).
Buemi, M. et al. The circadian rhythm of erythropoietin in subjects with pre-terminal uremia. Clin. Nephrol. 37, 159–160 (1992).
Hanly, P., Chan, C. & Pierratos, A. The impact of nocturnal hemodialysis on sleep apnea in ESRD patients. Nephrol. News Issues 17, 19–21 (2003).
Hanly, P. J. & Pierratos, A. Improvement of sleep apnea in patients with chronic renal failure who undergo nocturnal hemodialysis. N. Engl. J. Med. 344, 102–107 (2001).
Koch, B. C. et al. Effects of nocturnal hemodialysis on melatonin rhythm and sleep-wake behavior: an uncontrolled trial. Am. J. Kidney Dis. 53, 658–664 (2009).
Kunz, D. & Bes, F. Exogenous melatonin in periodic limb movement disorder: an open clinical trial and a hypothesis. Sleep 24, 183–187 (2001).
Nagtegaal, J. E., Kerkhof, G. A., Smits, M. G., Swart, A. C. & Van Der Meer, Y. G. Delayed sleep phase syndrome: a placebo-controlled cross-over study on the effects of melatonin administered five hours before the individual dim light melatonin onset. J. Sleep Res. 7, 135–143 (1998).
Andrade, C., Srihari, B. S., Reddy, K. P. & Chandramma, L. Melatonin in medically ill patients with insomnia: a double-blind, placebo-controlled study. J. Clin. Psychiatry 62, 41–45 (2001).
Arendt, J. & Skene, D. J. Melatonin as a chronobiotic. Sleep Med. Rev. 9, 25–39 (2005).
Koch, B. C. et al. The effects of melatonin on sleep-wake rhythm of daytime haemodialysis patients: a randomized, placebo-controlled, cross-over study (EMSCAP study). Br. J. Clin. Pharmacol. 67, 68–75 (2009).
Pérgola, P. E., Habiba, N. M. & Johnson, J. M. Body temperature regulation during hemodialysis in long-term patients: is it time to change dialysate temperature prescription? Am. J. Kidney Dis. 44, 155–165 (2004).
Parker, K. P., Bailey, J. L., Rye, D. B., Bliwise, D. L. & Van Someren, E. J. Lowering dialysate temperature improves sleep and alters nocturnal skin temperature in patients on chronic hemodialysis. J. Sleep Res. 16, 42–50 (2007).
Ramirez, G., Bittle, P. A., Sanders, H. & Bercu, B. B. Hypothalamo-hypophyseal, thyroid and gonadal function before and after erythropoietin therapy in dialysis patients. J. Clin. Endocrinol. Metab. 74, 517–524 (1992).
Herrera, J., Nava, M., Romero, F. & Rodríguez-Iturbe, B. Melatonin prevents oxidative stress resulting from iron and erythropoietin administration. Am. J. Kidney Dis. 37, 750–757 (2001).
Benz, R. L., Pressman, M. R., Hovick, E. T. & Peterson, D. D. A preliminary study of the effects of correction of anemia with recombinant human erythropoietin therapy on sleep, sleep disorders, and daytime sleepiness in hemodialysis patients (The Sleepo study). Am. J. Kidney Dis. 34, 1089–1095 (1999).
Zilberman, M. et al. Improvement of anemia with erythropoietin and intravenous iron reduces sleep-related breathing disorders and improves daytime sleepiness in anemic patients with congestive heart failure. Am. Heart J. 154, 870–876 (2007).
Painter, P., Carlson, L., Carey, S., Paul, S. M. & Myll, J. Physical functioning and health-related quality-of-life changes with exercise training in hemodialysis patients. Am. J. Kidney Dis. 35, 482–492 (2000).
Farese, S. et al. Effect of transcutaneous electrical muscle stimulation and passive cycling movements on blood pressure and removal of urea and phosphate during hemodialysis. Am. J. Kidney Dis. 52, 745–752 (2008).
Sakkas, G. K. et al. Intradialytic aerobic exercise training ameliorates symptoms of restless legs syndrome and improves functional capacity in patients on hemodialysis: a pilot study. ASAIO J. 54, 185–190 (2008).
Mauvieux, B., Gouthière, L., Sesboüe, B. & Davenne, D. A study comparing circadian rhythm and sleep quality of athletes and sedentary subjects engaged in night work [French]. Can. J. Appl. Physiol. 28, 831–887 (2003).
Van Someren, E. J., Riemersma, R. F. & Swaab, D. F. Functional plasticity of the circadian timing system in old age: light exposure. Prog. Brain Res. 138, 205–231 (2002).
Campbell, S. S., Dawson, D. & Anderson, M. W. Alleviation of sleep maintenance insomnia with timed exposure to bright light. J. Am. Geriatr. Soc. 41, 829–836 (1993).
Lack, L. et al. The treatment of early-morning awakening insomnia with 2 evenings of bright light. Sleep 28, 616–623 (2005).
Friedman, L. et al. Scheduled bright light for treatment of insomnia in older adults. J. Am. Geriatr. Soc. 57, 441–452 (2009).
Liu, A. C., Lewis, W. G. & Kay, S. A. l. Mammalian circadian signaling networks and therapeutic targets. Nat. Chem. Biol. 3, 630–639 (2007).
Czeisler, C. A., Buxton, O. M. & Singh Khalsa, S. B. The human circadian timing system and sleep-wake regulation. In Principles and Practice of Sleep Medicine (Eds Kryger, M. H., Roth, T. & Dement, W. C.) 375–394 (Elsevier Saunders, Philadelphia, 2005).
Acknowledgements
The authors would like to thank the Dutch Kidney Foundation for supporting our work and Inzicht Graphic Design, Arnhem, The Netherlands, for their assistance with the figures.
Charles P. Vega, University of California, Irvine, CA, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the MedscapeCME-accredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Koch, B., Nagtegaal, J., Kerkhof, G. et al. Circadian sleep–wake rhythm disturbances in end-stage renal disease. Nat Rev Nephrol 5, 407–416 (2009). https://doi.org/10.1038/nrneph.2009.88
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2009.88
This article is cited by
-
Effect of intradialytic exercise on daily physical activity and sleep quality in maintenance hemodialysis patients
International Urology and Nephrology (2018)
-
Understanding the Two Faces of Low-Salt Intake
Current Hypertension Reports (2017)
-
Analyses of melatonin, cytokines, and sleep in chronic renal failure
Sleep and Breathing (2016)
-
Exogenous Melatonin for Delirium Prevention: a Meta-analysis of Randomized Controlled Trials
Molecular Neurobiology (2016)
-
Circadian variation in plasma 5-fluorouracil concentrations during a 24 hour constant-rate infusion
BMC Cancer (2015)