Key Points
-
Epilepsies are characterized by recurrent seizures, which can cause motor, sensory, cognitive, psychic or autonomic disturbances. The seizures are the clinical manifestation of an underlying transient abnormality of cortical neuronal activity, and their phenotypic expression is determined by the point of origin of the hyperexcitability and its degree of spread in the brain.
-
Causes of sporadic or recurrent seizures include acquired structural brain damage, altered metabolic states and inborn brain malformations. However, about 1% of people develop recurrent unprovoked seizures for no obvious reason. These 'idiopathic' epilepsies are assumed to be mainly genetic in origin.
-
Idiopathic epilepsies are caused predominantly by mutations in genes that code for ion channels or their accessory subunits. The channels that are involved belong to either the class of voltage-gated ion channels, which are important for action potential generation and control, or the ligand-gated ion channels, which are mainly involved in synaptic transmission. Epilepsy syndromes that have been attributed to ion channel defects include familial nocturnal frontal lobe epilepsy, benign familial neonatal convulsions, and generalized epilepsy with febrile seizures plus (GEFS+).
-
Although ion channels undoubtedly have an important role in idiopathic epilepsies, other pathways can also lead to neuronal hyperexcitability. Mutant forms of any gene that is involved in neuronal plasticity, development of neuronal networks or neuronal metabolism are potential candidates for causing epileptogenesis.
-
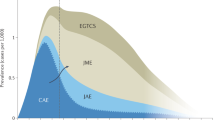
In childhood and adolescence, about 30–40% of all epilepsies belong to the group of idiopathic generalized epilepsies (IGE). Little is known about the genes that underlie epileptogenesis in IGE, although linkage studies and association approaches have highlighted numerous candidate regions in the genome, including chromosomal region 3q26, which contains the voltage-gated chloride channel gene CLCN2.
-
More than 200 inherited syndromes are known in which epileptic seizures are a prominent clinical feature. The epilepsy is often accompanied by other neurological symptoms, such as mental retardation, dementia or ataxia. The genes that underlie these syndromes are involved in tasks as different as glycogen metabolism, respiratory chain activity and brain development.
-
It is difficult to predict how many more genes that are associated with epilepsy are waiting to be discovered in the human genome. Learning about the gene families that can cause epilepsy will not only help us to understand the complex pathways that underlie neuronal hyperexcitability, but should also lead to the development of more powerful and precise treatment strategies.
Abstract
Genetic factors can cause recurrent abnormal synchronization and episodic hyperexcitability of neuronal networks through various mechanisms. Many of the genes that have been implicated in idiopathic epilepsies code for ion channels, whereas syndromes with epilepsy as a main feature are caused by genes that are involved in functions as diverse as cortical development, mitochondrial function and cell metabolism. Each 'epilepsy gene' that is identified provides new and fascinating insights into the molecular basis of neuronal excitability and brain function.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Steinlein, O. et al. A missense mutation in the neuronal nicotinic acetylcholine receptor α4 subunit is associated with autosomal dominant nocturnal frontal lobe epilepsy. Nature Genet. 11, 201–203 (1995). This paper described the identification of the first gene that was found to be responsible for idiopathic epilepsy in humans.
Fusco, M. D. et al. The nicotinic receptor β2 subunit is mutant in nocturnal frontal lobe epilepsy. Nature Genet. 26, 275–276 (2000).
Biervert, C. et al. A potassium channel mutation in neonatal human epilepsy. Science 279, 403–406 (1998).
Singh, N. A. et al. A novel potassium channel gene, KCNQ2, is mutated in an inherited epilepsy of newborns. Nature Genet. 18, 25–29 (1998).
Charlier, C. et al. A pore mutation in a novel KQT-like potassium channel gene in an idiopathic epilepsy family. Nature Genet. 18, 53–55 (1998).
Wallace, R. H. et al. Febrile seizures and generalized epilepsy associated with a mutation in the Na+-channel β1 subunit gene SCN1B. Nature Genet. 19, 366–370 (1998).
Escayg, A. et al. Mutations of SCN1A, encoding a neuronal sodium channel, in two families with GEFS+2. Nature Genet. 24, 343–345 (2000).
Sugawara, T. et al. A missense mutation of the Na+ channel αII subunit gene Na v 1.2 in a patient with febrile and afebrile seizures causes channel dysfunction. Proc. Natl Acad. Sci. USA 98, 6384–6389 (2001).
Baulac, S. et al. First genetic evidence of GABAA receptor dysfunction in epilepsy: a mutation in the γ2-subunit gene. Nature Genet. 28, 46–48 (2001).
Wallace, R. H. et al. Mutant GABAA receptor γ2-subunit in childhood absence epilepsy and febrile seizures. Nature Genet. 28, 49–52 (2001).
Kalachikov, S. et al. Mutations in LGI1 cause autosomal-dominant partial epilepsy with auditory features. Nature Genet. 30, 335–341 (2002). The LGI1 gene described in this paper was the first non-ion channel gene to be implicated in human idiopathic epilepsy.
Heron, S. E. et al. Sodium-channel defects in benign familial neonatal-infantile seizures. Lancet 360, 851–852 (2002).
Nakayama, J. et al. A nonsense mutation of the MASS1 gene in a family with febrile and afebrile seizures. Ann. Neurol. 52, 654–657 (2002).
Cossette, P. et al. Mutation of GABRA1 in an autosomal dominant form of juvenile myoclonic epilepsy. Nature Genet. 31, 184–189 (2002).
Haug, K. et al. Mutations in CLCN2 encoding a voltage-gated chloride channel are associated with idiopathic generalized epilepsies. Nature Genet. 33, 527–532 (2003).
Phillips, H. A. et al. Localization of a gene for autosomal dominant nocturnal frontal lobe epilepsy to chromosome 20q13.2. Nature Genet. 10, 117–118 (1995).
Hayman, M., Scheffer, I. E., Chinvarun, Y., Berlangieri, S. U. & Berkovic, S. F. Autosomal dominant nocturnal frontal lobe epilepsy: demonstration of focal frontal onset and intrafamilial variation. Neurology 49, 969–975 (1997).
Scheffer, I. E. & Berkovic, S. F. Generalized epilepsy with febrile seizures plus. A genetic disorder with heterogeneous clinical phenotypes. Brain 120, 479–490 (1997).
Kullmann, D. M. & Hanna, M. G. Neurological disorders caused by inherited ion channel mutations. Lancet. 1, 157–166 (2002).
Scheffer, I. E. et al. Autosomal dominant nocturnal frontal lobe epilepsy: a distinctive clinical disorder. Brain 118, 61–73 (1995).
Steinlein, O. et al. An insertion mutation of the CHRNA4 gene in a family with autosomal dominant nocturnal frontal lobe epilepsy. Hum. Mol. Genet. 6, 943–947 (1997).
Hirose, S. et al. A novel mutation of CHRNA4 responsible for autosomal dominant nocturnal frontal lobe epilepsy. Neurology 53, 1749–1753 (1999).
Phillips, H. A. et al. A de novo mutation in sporadic nocturnal frontal lobe epilepsy. Ann. Neurol. 48, 264–267 (2000).
Phillips, H. A. et al. CHRNB2 is the second acetylcholine receptor subunit associated with autosomal dominant nocturnal frontal lobe epilepsy. Am. J. Hum. Genet. 68, 225–231 (2001).
Bertrand, D. et al. How mutations in the nAChRs can cause ADNFLE epilepsy. Epilepsia 43 (Suppl. 5), 112–122 (2002). The authors compare the distinct functional properties of four nAChR mutations associated with ADNFLE, and discuss their findings in the context of the latest knowledge of pyramidal cell function.
Magnusson, A., Stordal, E., Brodtkorb, E. & Steinlein, O. Schizophrenia, psychotic illness and other psychiatric symptoms in families with autosomal dominant nocturnal frontal lobe epilepsy. Psychiat. Genet. 13, 91–95 (2003).
Cho, Y. -W. et al. A korean kindred with autosomal dominant nocturnal frontal lobe epilepsy (ADNFLE) presenting as partial seizures with mental retardation. Arch. Neurol. 60, 1625–1632 (2003).
Ronen, G. M., Rosales, T. O., Connolly, M., Anderson, V. E. & Leppert, M. Seizure characteristics in chromosome 20 benign familial neonatal convulsions. Neurology 43, 1355–1360 (1993).
Wakai, S. et al. Classification of familial neonatal convulsions. Lancet 344, 1376 (1994).
Dedek, K., Fusco, L., Teloy, N. & Steinlein, O. K. Neonatal convulsions and epileptic encephalopathy in an Italian family with a missense mutation in the fifth transmembrane region of KCNQ2. Epilepsy Res. 54, 21–27 (2003).
Wang, H. S. et al. KCNQ2 and KCNQ3 potassium channel subunits: molecular correlates of the M-channel. Science 282, 1890–1893 (1998). The authors were the first to discover that the potassium channel genes associated with BFNC encode subunits of the long-known M-channel, an important modulator of neuronal excitability.
Brown, D. M-currents: an update. Trends Neurosci. 11, 294–299 (1988).
Dedek, K. et al. Myokymia and neonatal epilepsy caused by a mutation in the voltage sensor of the KCNQ2 K+ channel. Proc. Natl Acad. Sci. USA 98, 12272–12277 (2001).
Watanabe, H. et al. Disruption of the epilepsy KCNQ2 gene results in neural hyperexcitability. J. Neurochem. 75, 28–33 (2000).
Sugawara, T. et al. Nav1.1 mutations cause febrile seizures associated with afebrile partial seizures. Neurology 57, 703–705 (2001).
Harkin, L. A. et al. Truncation of the GABAA-receptor γ2 subunit in a family with generalized epilepsy with febrile seizures plus. Am. J. Hum. Genet. 70, 530–536 (2002).
Kananura, C. et al. A splice-site mutation in GABRG2 associated with childhood absence epilepsy and febrile convulsions. Arch. Neurol. 59, 1137–1141 (2002).
Marini, C. et al. Childhood absence epilepsy and febrile seizures: a family with a GABAA receptor mutation. Brain 126, 230–240 (2003).
Lossin, C., Wang, D. W., Rhodes, T. H., Vanoye, C. G. & George, A. L. Molecular basis of an inherited epilepsy. Neuron 34, 877–884 (2002).
Spampanato, J., Escayg, A., Meisler, M. H. & Goldin, A. L. Functional effects of two voltage-gated sodium channel mutations that cause generalized epilepsy with febrile seizures plus type 2. J. Neurosci. 21, 7481–7490 (2001).
Lossin, C. et al. Epilepsy-associated dysfunction in the voltage-gated neuronal sodium channel SCN1A. J. Neurosci. 23, 11289–91125 (2003).
Claes, L. et al. De novo mutations in the sodium-channel gene SCN1A cause severe myoclonic epilepsy of infancy. Am. J. Hum. Genet. 68, 1327–1332 (2001).
Winawer, M. R. et al. Autosomal dominant partial epilepsy with auditory features: defining the phenotype. Neurology 54, 2173–2176 (2000).
Brodtkorb, E., Gu, W., Nakken, K. O., Fischer, C. & Steinlein, O. K. Familial temporal lobe epilepsy with aphasic seizures and linkage to chromosome 10q22–q24. Epilepsia 43, 228–235 (2002).
Gu, W., Brodtkorb, E. & Steinlein, O. K. LGI1 is mutated in familial temporal lobe epilepsy characterized by aphasic seizures. Ann. Neurol. 52, 364–367 (2002).
Morante-Redolat, J. M. et al. Mutations in the LGI1/Epitempin gene on 10q24 cause autosomal dominant lateral temporal epilepsy. Hum. Mol. Genet. 11, 1119–1128 (2002).
Pizzuti, A. et al. Epilepsy with auditory features: a LGI1 gene mutation suggests a loss-of-function mechanism. Ann. Neurol. 53, 396–399 (2003).
Fertig, E., Lincoln, A., Martinuzzi, A., Mattson, R. H. & Hisama, F. M. Novel LGI1 mutation in a family with autosomal dominant partial epilepsy with auditory features. Neurology 60, 1687–1690 (2003).
Gu, W. et al. The LGI1 gene involved in lateral temporal lobe epilepsy belongs to a new subfamily of leucine-rich repeat proteins. FEBS Lett. 519, 71–76 (2002).
Scheel, H., Tomiuk, S. & Hofmann, K. A common protein interaction domain links two recently identified epilepsy genes. Hum. Mol. Genet. 11, 1757–1762 (2002). An in silico study, which showed that LGI1 is probably not membrane-bound, and that it shares the formerly unknown epitempin repeat with another epilepsy gene, the MASS1/VLGR1 gene.
Staub, E. et al. The novel EPTP repeat defines a superfamily of proteins implicated in epileptic disorders. Trends Biochem. Sci. 27, 441–444 (2002).
Skradski, S. L. et al. A novel gene causing a mendelian audiogenic mouse epilepsy. Neuron 31, 537–544 (2001).
Chernova, O. B., Somerville, R. P. & Cowell, J. K. A novel gene, LGI1, from 10q24 is rearranged and downregulated in malignant brain tumors. Oncogene 17, 2873–2881 (1998).
Krex, D. et al. Physical and functional characterization of the human LGI1 gene and its possible role in glioma development. Acta Neuropathol. 103, 255–266 (2002).
Brodtkorb, E., Nakken, K. O. & Steinlein, O. K. No evidence for a seriously increased malignancy risk in LGI1-caused epilepsy. Epilepsy Res. 56, 205–208 (2003).
Berkovic, S. F., Howell, R. A., Hay, D. A. & Hopper, J. L. Epilepsies in twins: genetics of the major epilepsy syndromes. Ann. Neurol. 43, 435–445 (1998).
Zara, F. et al. Mapping of genes predisposing to idiopathic generalized epilepsy. Hum. Mol. Genet. 4, 1201–1207 (1995).
Chioza, B. et al. Haplotype and linkage disequilibrium analysis to characterise a region in the calcium channel gene CACNA1A associated with idiopathic generalised epilepsy. Eur. J. Hum. Genet. 10, 857–864 (2002).
Sander, T., Toliat, M. R., Heils, A., Becker, C. & Nurnberg, P. Failure to replicate an allelic association between an exon 8 polymorphism of the human α1A calcium channel gene and common syndromes of idiopathic generalized epilepsy. Epilepsy Res. 49, 173–177 (2002).
Chen, Y. et al. Association between genetic variation of CACNA1H and childhood absence epilepsy. Ann. Neurol. 54, 239–243 (2003).
Sander, T. et al. Genome search for susceptibility loci of common idiopathic generalised epilepsies. Hum. Mol. Genet. 9, 1465–1472 (2000). A genome scan involving a larger number of families with common forms of idiopathic epilepsy, which led to the discovery of a mutated gene (see also reference 15).
Sander, T. et al. Genetic variation of the human μ-opioid receptor and susceptibility to idiopathic absence epilepsy. Epilepsy Res. 39, 57–61 (2000).
Wilkie, H. et al. Association of μ-opioid receptor subunit gene and idiopathic generalized epilepsy. Neurology 59, 724–728 (2002).
Koskiniemi, M., Donner, M., Majuri, H., Haltia, M. & Norio, R. Progressive myoclonus epilepsy. A clinical and histopathological study. Acta Neurol. Scan. 50, 307–332 (1974).
Haltia, M., Kristensson, K. & Sourander, P. Neuropathological studies in three Scandinavian cases of progressive myoclonus epilepsy. Acta Neurol. Scan. 45, 63–77 (1969).
Lafreniere, R. G. et al. Unstable insertion in the 5′ flanking region of the cystatin B gene is the most common mutation in progressive myoclonus epilepsy type 1 EPM1. Nature Genet. 15, 298–302 (1997).
Pennacchio, L. A. et al. Progressive ataxia, myoclonic epilepsy and cerebellar apoptosis in cystatin B-deficient mice. Nature Genet. 20, 251–258 (1998).
Lieuallen, K., Pennacchio, L. A., Park, M., Myers, R. M. & Lennon, G. G. Cystatin B-deficient mice have increased expression of apoptosis and glial activation genes. Hum. Mol. Genet. 10, 1867–1871 (2001).
Minassian, B. A. et al. Mutations in a gene encoding a novel protein tyrosine phosphatase cause progressive myoclonus epilepsy. Nature Genet. 20, 171–174 (1998).
Chan, E. M. et al. Mutations in NHLRC1 cause progressive myoclonus epilepsy. Nature Genet. 35, 125–127 (2003).
Fernandez-Sanchez, M. E. et al. Laforin, the dual-phosphatase responsible for Lafora disease, interacts with R5 (PTG), a regulatory subunit of protein phosphatase-1 that enhances glycogen accumulation. Hum. Mol. Genet. 12, 3161–3171 (2003).
Gleeson, J. G. et al. Doublecortin, a brain-specific gene mutated in human X-linked lissencephaly and double cortex syndrome, encodes a putative signalling protein. Cell 92, 63–72 (1998).
Corbo, J. C. et al. Doublecortin is required in mice for lamination of the hippocampus but not the neocortex. J. Neurosci. 22, 7548–7557 (2002).
Bai, J. et al. RNAi reveals doublecortin is required for radial migration in rat neocortex. Nature Neurosci. 6, 1277–1283 (2003). A report that highlights the limitations of gene knockout approaches and provides new insight into the mechanisms that underlie neuronal migration during embryogenesis.
Shoffner, J. M. et al. Myoclonic epilepsy and ragged-red fiber disease (MERRF) is associated with a mitochondrial DNA tRNALYS mutation. Cell 61, 931–937 (1990).
Moraes, C. T. et al. Two novel pathogenic mitochondrial DNA mutations affecting organelle number and protein synthesis. Is the tRNALeu(UUR) gene an etiologic hot spot? J. Clin. Invest. 92, 2906–2915 (1993).
Feng, Y. & Walsh, C. A. Protein–protein interactions, cytoskeletal regulation and neuronal migration. Nature Rev. Neurosci. 2, 408–416 (2001).
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The author declares no competing financial interests.
Related links
Related links
DATABASES
Entrez Gene
OMIM
grand mal epilepsy on awakening
Lafora progressive myoclonus epilepsy
FURTHER INFORMATION
Encyclopedia of Life Sciences
Glossary
- ABSENCE EPILEPSY
-
A non-convulsive form of epilepsy that is characterized by a sudden, brief impairment of consciousness.
- MYOCLONUS
-
Brief, involuntary twitching of a muscle or a group of muscles. Familiar examples of normal myoclonus include hiccups and jerks experienced when drifting off to sleep.
- FRAGILE X SYNDROME
-
A genetic condition, commonly transmitted from mother to son, that is associated with mental retardation, abnormal facial features and enlarged testicles.
- ANGELMAN'S SYNDROME
-
A genetic disorder that is caused by deletion or disruption of UBE3A (E6-AP). The symptoms of Angelman's syndrome include hyperactivity, ataxia, problems with speech and language, and an unusually happy demeanour.
- AUTOSOMAL
-
A term that refers to any chromosome in a cell that is not a sex chromosome.
- PARAMYOTONIA CONGENITA
-
A rare autosomal dominant disorder in which muscle fibres are slow to relax after contraction.
- PATCH CLAMP
-
Technique whereby a very small electrode tip is sealed onto a patch of cell membrane, making it possible to record the flow of current through individual ion channels or pores within the patch.
- MISSENSE MUTATION
-
A mutation that results in the substitution of an amino acid in a protein.
- β-PROPELLER
-
A protein domain that consists of an array of β-sheet motifs, which are configured in a ring to resemble the blades of a propeller.
- G PROTEIN
-
A heterotrimeric GTP-binding and -hydrolysing protein that interacts with cell-surface receptors, often stimulating or inhibiting the activity of a downstream enzyme. G proteins consist of three subunits: the α-subunit, which contains the guanine-nucleotide-binding site; and the β- and γ-subunits, which function as a heterodimer.
- FRINGS MOUSE MODEL
-
An inbred mouse strain with a seizure phenotype that is characterized by wild running, loss of righting reflex, tonic flexion and tonic extension in response to high-intensity sound stimulation.
- AUDIOGENIC EPILEPSY
-
A form of epilepsy in which the seizures are provoked by auditory stimuli.
- INTENTION TREMOR
-
A tremor that is exacerbated by voluntary goal-directed movements; for example, trying to put a key in a lock.
- DYSARTHRIA
-
A speech impairment that is caused by damage to the nerves or muscles that control speech articulation. Although the speech is difficult to understand, it is usually linguistically normal, thereby distinguishing this condition from language disorders.
- RNA INTERFERENCE
-
(RNAi). A method by which double-stranded RNA that is encoded on an exogenous vector can be used to interfere with normal RNA processing, causing rapid degradation of the endogenous RNA and thereby precluding translation. This provides a simple way of studying the effects of the absence of a gene product in simple organisms and in cells.
Rights and permissions
About this article
Cite this article
Steinlein, O. Genetic mechanisms that underlie epilepsy. Nat Rev Neurosci 5, 400–408 (2004). https://doi.org/10.1038/nrn1388
Issue Date:
DOI: https://doi.org/10.1038/nrn1388
This article is cited by
-
Therapeutic efficacy of voltage-gated sodium channel inhibitors in epilepsy
Acta Epileptologica (2023)
-
Invertebrate neurons as a simple model to study the hyperexcitable state of epileptic disorders in single cells, monosynaptic connections, and polysynaptic circuits
Biophysical Reviews (2022)
-
Ameliorating Effect of Umbilical Cord Mesenchymal Stem Cells in a Human Induced Pluripotent Stem Cell Model of Dravet Syndrome
Molecular Neurobiology (2022)
-
Interictal autonomic dysfunction in patients with epilepsy
The Egyptian Journal of Neurology, Psychiatry and Neurosurgery (2021)
-
ALG13 participates in epileptogenesis via regulation of GABAA receptors in mouse models
Cell Death Discovery (2020)