Key Points
-
Prion diseases are progressive, transmissible neurodegenerative disorders with an invariably fatal outcome. Prions, the infectious agent of prion diseases, accumulate in the central nervous system, in organs of the secondary lymphoid system and in blood.
-
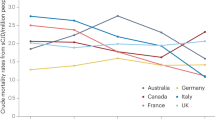
Examples of prion diseases include bovine spongiform encephalopathy (BSE) in cows, scrapie in sheep and goat, chronic wasting disease in deer and elk, and sporadic and variant Creutzfeldt–Jakob disease in humans.
-
Neuronal cytotoxicity of PrPSc depends on the expression of PrPC. Evidence indicates that the conversion of PrPC to PrPSc is deleterious, but the mechanisms of neural degeneration are still unclear.
-
In this article, we describe the role of the immune system in prion diseases and review our current understanding of cellular and molecular mechanisms involved in peripheral prion replication and transport.
-
Several prion diseases are transmitted by peripheral prion uptake (for example, ingestion of prion-contaminated food). After prion uptake, a replication phase occurs in lymphoid tissue before neuroinvasion.
-
In the peripheral regions of the host, the abnormally folded, aggregated PrPSc, is amplified by cells of the immune system (for example, follicular dendritic cells) in the germinal centres, located in B-cell follicles of the spleen or lymph nodes.
-
Depletion of mature follicular dendritic cells delays the development of prion disease following intraperitoneal inoculation. This could form the basis of a post-exposure prophylactic strategy.
-
Recent findings indicate that chronic inflammation can induce the deposition of prion infectivity in organs previously believed to be prion free.
Abstract
The prion, a conformational variant of a host protein, is the infectious particle responsible for transmissible spongiform encephalopathy (TSE), a fatal neurodegenerative disease of humans and animals. The principal target of prion pathology is the brain, yet most TSEs also display prion replication at extra-cerebral locations, including secondary lymphoid organs and sites of chronic inflammation. Despite significant progress in our understanding of this infectious agent, many fundamental questions relating to the nature of the prion, including the mechanism of replication and the molecular events underlying brain damage, remain unanswered. Here we focus on the unresolved issues pertaining to prion pathogenesis, particularly on the role played by the immune system.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Gajdusek, D. C. & Zigas, V. Degenerative disease of the central nervous system in New Guinea; the endemic occurrence of 'kuru' in the native population. N. Engl. J. Med. 257, 974–978 (1957).
Collinge, J. et al. Kuru in the 21st century — an acquired human prion disease with very long incubation periods. Lancet 367, 2068–2074 (2006).
Will, R. G. et al. A new variant of Creutzfeldt-Jakob disease in the UK. Lancet 347, 921–925 (1996).
Hill, A. M., Cane, D. E., Mau, C. J. D. & West, C. A. High level expression of Ricinus communis casbene synthase in Escherichia coli and characterization of the recombinant enzyme. Arch. Biochem. Biophys. 336, 283–289 (1996).
Collinge, J., Sidle, K. C., Meads, J., Ironside, J. & Hill, A. F. Molecular analysis of prion strain variation and the aetiology of 'new variant' CJD. Nature 383, 685–690 (1996).
Aguzzi, A. & Polymenidou, M. Mammalian prion biology. One century of evolving concepts. Cell 116, 313–327 (2004).
Llewelyn, C. A. et al. Possible transmission of variant Creutzfeldt-Jakob disease by blood transfusion. Lancet 363, 417–421 (2004).
Mead, S. et al. Balancing selection at the prion protein gene consistent with prehistoric kurulike epidemics. Science 300, 640–643 (2003).
Sekercioglu, C. H. Prion diseases and a penchant for brains. Science 305, 342–343 (2004).
Soldevila, M. et al. The prion protein gene in humans revisited: lessons from a worldwide resequencing study. Genome Res. 16, 231–239 (2006).
Kreitman, M. & Di Rienzo, A. Balancing claims for balancing selection. Trends Genet. 20, 300–304 (2004).
Glatzel, M., Abela, E., Maissen, M. & Aguzzi, A. Extraneural pathologic prion protein in sporadic Creutzfeldt-Jakob disease. N. Engl. J. Med. 349, 1812–1820 (2003).
Angers, R. C. et al. Prions in skeletal muscles of deer with chronic wasting disease. Science 311, 1117 (2006).
Heikenwalder, M. et al. Chronic lymphocytic inflammation specifies the organ tropism of prions. Science 307, 1107–1110 (2005).
Ligios, C. et al. PrPSc in mammary glands of sheep affected by scrapie and mastitis. Nature Med. 11, 1137–1138 (2005).
Aguzzi, A. & Heikenwalder, M. Prions, cytokines, and chemokines: a meeting in lymphoid organs. Immunity 22, 145–154 (2005).
Kovacs, G. G. et al. Creutzfeldt-Jakob disease and inclusion body myositis: Abundant disease-associated prion protein in muscle. Ann. Neurol. 55, 121–125 (2004).
Seeger, H. et al. Coincident scrapie infection and nephritis lead to urinary prion excretion. Science 310, 324–326 (2005).
Aguzzi, A. & Sigurdson, C. J. Antiprion immunotherapy: to suppress or to stimulate? Nature Rev. Immunol. 4, 725–736 (2004).
Ligios, C. et al. PrPSc deposition in nervous tissues without lymphoid tissue involvement is frequently found in ARQ/ARQ Sarda breed sheep preclinically affected with natural scrapie. Arch. Virol. 20 April 2006 (doi:10.1007/s00705-006-0759-2)
Mabbott, N. A. & MacPherson, G. G. Prions and their lethal journey to the brain. Nature Rev, Microbiol, 4, 201–211 (2006).
Aguzzi, A., Heikenwalder, M. & Miele, G. Progress and problems in the biology, diagnostics, and therapeutics of prion diseases. J. Clin. Invest. 114, 153–160 (2004).
Riek, R., Hornemann, S., Wider, G., Glockshuber, R. & Wüthrich, K. NMR characterization of the full-length recombinant murine prion protein, mPrP(23–231). FEBS Lett. 413, 282–288 (1997).
Gossert, A. D., Bonjour, S., Lysek, D. A., Fiorito, F. & Wuthrich, K. Prion protein NMR structures of elk and of mouse/elk hybrids. Proc. Natl Acad. Sci. USA 102, 646–650 (2005).
Riek, R. et al. NMR structure of the mouse prion protein domain Prp (121–231). Nature 382, 180–182 (1996).
Brockes, J. P. Topics in prion cell biology. Curr. Opin. Neurobiol. 9, 571–577 (1999).
Simonic, T. et al. cDNA cloning of turtle prion protein. FEBS Lett. 469, 33–38 (2000).
Strumbo, B., Ronchi, S., Bolis, L. C. & Simonic, T. Molecular cloning of the cDNA coding for Xenopus laevis prion protein. FEBS Lett . 508, 170–174 (2001).
Miele, G. et al. Embryonic activation and developmental expression of the murine prion protein gene. Gene Expr. 11, 1–12 (2003).
Manson, J. et al. The prion protein gene: a role in mouse embryogenesis? Development 115, 117–122 (1992).
Ford, M. J., Burton, L. J., Morris, R. J. & Hall, S. M. Selective expression of prion protein in peripheral tissues of the adult mouse. Neuroscience 113, 177–192 (2002).
Moser, M., Colello, R. J., Pott, U. & Oesch, B. Developmental expression of the prion protein gene in glial cells. Neuron 14, 509–517 (1995).
Basler, K. et al. Scrapie and cellular PrP isoforms are encoded by the same chromosomal gene. Cell 46, 417–428 (1986).
Büeler, H. R. et al. Normal development and behaviour of mice lacking the neuronal cell-surface PrP protein. Nature 356, 577–582 (1992).
Zhang, C. C., Steele, A. D., Lindquist, S. & Lodish, H. F. Prion protein is expressed on long-term repopulating hematopoietic stem cells and is important for their self-renewal. Proc. Natl Acad. Sci. USA 103, 2184–2189 (2006).
Steele, A. D., Emsley, J. G., Ozdinler, P. H., Lindquist, S. & Macklis, J. D. Prion protein PrPc positively regulates neural precursor proliferation during developmental and adult mammalian neurogenesis. Proc. Natl Acad. Sci. USA 103, 3416–3421 (2006).
Mallucci, G. R. et al. Post-natal knockout of prion protein alters hippocampal CA1 properties, but does not result in neurodegeneration. EMBO J. 21, 202–210 (2002).
Solforosi, L. et al. Cross-linking cellular prion protein triggers neuronal apoptosis in vivo. Science 303, 1514–1516 (2004).
Aguzzi, A. & Heikenwalder, M. Prion diseases: cannibals and garbage piles. Nature 423, 127–129 (2003).
Fraser, H. & Dickinson, A. G. Pathogenesis of scrapie in the mouse: the role of the spleen. Nature 226, 462–463 (1970).
Eklund, C. M., Kennedy, R. C. & Hadlow, W. J. Pathogenesis of scrapie virus infection in the mouse. J. Infect. Dis. 117, 15–22 (1967).
Fraser, H. & Dickinson, A. G. Studies of the lymphoreticular system in the pathogenesis of scrapie: the role of spleen and thymus. J. Comp. Pathol. 88, 563–573 (1978).
Hill, A. F., Zeidler, M., Ironside, J. & Collinge, J. Diagnosis of new variant Creutzfeldt-Jakob disease by tonsil biopsy. Lancet 349, 99 (1997).
Kimberlin, R. H. & Walker, C. A. Pathogenesis of mouse scrapie: dynamics of agent replication in spleen, spinal cord and brain after infection by different routes. J. Comp. Pathol. 89, 551–562 (1979).
Mould, D. L., Dawson, A. M. & Rennie, J. C. Very early replication of scrapie in lymphocytic tissue. Nature 228, 779–780 (1970).
Beekes, M. & McBride, P. A. Early accumulation of pathological PrP in the enteric nervous system and gut-associated lymphoid tissue of hamsters orally infected with scrapie. Neurosci. Lett. 278, 181–184 (2000).
Bruce, M. E. Agent replication dynamics in a long incubation period model of mouse scrapie. J. Gen. Virol. 66, 2517–2522 (1985).
Büeler, H. R. et al. Mice devoid of PrP are resistant to scrapie. Cell 73, 1339–1347 (1993).
Dickinson, A. G. & Fraser, H. in Slow Transmissible Diseases of the Nervous System (eds Prusiner, S. B. & Hadlow, W. J.) 367–386 (Academic Press, New York, 1979).
Rubenstein, R. et al. Scrapie-infected spleens: analysis of infectivity, scrapie-associated fibrils, and protease-resistant proteins. J. Infect. Dis. 164, 29–35 (1991).
Clarke, M. C. & Haig, D. A. Multiplication of scrapie agent in mouse spleen. Res. Vet. Sci. 12, 195–197 (1971).
Dickinson, A. G., Fraser, H., Meikle, V. M. & Outram, G. W. Competition between different scrapie agents in mice. Nature New Biol. 237, 244–245 (1972).
McGovern, G., Brown, K. L., Bruce, M. E. & Jeffrey, M. Murine scrapie infection causes an abnormal germinal centre reaction in the spleen. J. Comp. Pathol. 130, 181–194 (2004).
Terszowski, G. et al. Evidence for a functional second thymus in mice. Science 312, 284–287 (2006).
Kimberlin, R. H. & Walker, C. A. The role of the spleen in the neuroinvasion of scrapie in mice. Virus Res. 12, 201–211 (1989).
Kimberlin, R. H. & Walker, C. A. Pathogenesis of scrapie (strain 263K) in hamsters infected intracerebrally, intraperitoneally or intraocularly. J. Gen. Virol. 67, 255–263 (1986).
Mohri, S., Handa, S. & Tateishi, J. Lack of effect of thymus and spleen on the incubation period of Creutzfeldt-Jakob disease in mice. J. Gen. Virol. 68, 1187–1189 (1987).
Tateishi, J., Ohta, M., Koga, M., Sato, Y. & Kuroiwa, Y. Transmission of chronic spongiform encephalopathy with kuru plaques from humans to small rodents. Ann. Neurol. 5, 581–584 (1979).
Clarke, M. C. & Kimberlin, R. H. Pathogenesis of mouse scrapie: distribution of agent in the pulp and stroma of infected spleens. Vet. Microbiol. 9, 215–225 (1984).
Fraser, H. & Farquhar, C. F. Ionising radiation has no influence on scrapie incubation period in mice. Vet. Microbiol. 13, 211–223 (1987).
Brandner, S. et al. Normal host prion protein PrPC is required for scrapie spread within the central nervous system. Proc. Natl Acad. Sci. USA 93, 13148–13151 (1996).
Kaeser, P. S., Klein, M. A., Schwarz, P. & Aguzzi, A. Efficient lymphoreticular prion propagation requires PrPc in stromal and hematopoietic cells. J. Virol. 75, 7097–7106. (2001).
Blättler, T. et al. PrP-expressing tissue required for transfer of scrapie infectivity from spleen to brain. Nature 389, 69–73 (1997).
Klein, M. A. et al. A crucial role for B cells in neuroinvasive scrapie. Nature 390, 687–690 (1997).
Klein, M. A. et al. PrP expression in B lymphocytes is not required for prion neuroinvasion. Nature Med. 4, 1429–1433 (1998).
Montrasio, F. et al. B lymphocyte-restricted expression of prion protein does not enable prion replication in prion protein knockout mice. Proc. Natl Acad. Sci. USA 98, 4034–4037 (2001).
Heinen, E., Bosseloir, A. & Bouzahzah, F. Follicular dendritic cells: origin and function. Curr. Top. Microbiol. Immunol. 201, 15–47 (1995).
Kosco-Vilbois, M. H. Follicular dendritic cells: a license to tangle with scrapie. Immunol. Today 21, 468 (2000).
Taylor, P. R. et al. The follicular dendritic cell restricted epitope, FDC-M2, is complement C4; localization of immune complexes in mouse tissues. Eur. J. Immunol. 32, 1888–1896 (2002).
Huber, C. et al. Lymphotoxin-β receptor-dependent genes in lymph node and follicular dendritic cell transcriptomes. J. Immunol. 174, 5526–5536 (2005).
Shakhov, A. N. et al. Gene profiling approach in the analysis of lymphotoxin and TNF deficiencies. J. Leukoc. Biol. 68, 151–157 (2000).
Fu, Y. X. & Chaplin, D. D. Development and maturation of secondary lymphoid tissues. Annu. Rev. Immunol. 17, 399–433 (1999).
Cyster, J. G. et al. Chemokines and B-cell homing to follicles. Curr. Top. Microbiol. Immunol. 246, 87–93 (1999).
Ruddle, N. H. & Waksman, B. H. Cytotoxic effect of lymphocyte-antigen interaction in delayed hypersensitivity. Science 157, 1060–1062 (1967).
Ruddle, N. H. & Waksman, B. H. Cytotoxicity mediated by soluble antigen and lymphocytes in delayed hypersensitivity. 3. Analysis of mechanism. J. Exp. Med. 128, 1267–1279 (1968).
Locksley, R. M., Killeen, N. & Lenardo, M. J. The TNF and TNF receptor superfamilies: integrating mammalian biology. Cell 104, 487–501 (2001).
Picarella, D. E., Kratz, A., Li, C. B., Ruddle, N. H. & Flavell, R. A. Insulitis in transgenic mice expressing tumor necrosis factor β (lymphotoxin) in the pancreas. Proc. Natl Acad. Sci. USA 89, 10036–10040 (1992).
Kratz, A., Campos-Neto, A., Hanson, M. S. & Ruddle, N. H. Chronic inflammation caused by lymphotoxin is lymphoid neogenesis. J. Exp. Med. 183, 1461–1472 (1996).
Kitamoto, T., Muramoto, T., Mohri, S., Doh ura, K. & Tateishi, J. Abnormal isoform of prion protein accumulates in follicular dendritic cells in mice with Creutzfeldt-Jakob disease. J. Virol. 65, 6292–6295 (1991).
Brown, K. L. et al. Scrapie replication in lymphoid tissues depends on prion protein- expressing follicular dendritic cells. Nature Med. 5, 1308–1312 (1999).
Prinz, M. et al. Lymph nodal prion replication and neuroinvasion in mice devoid of follicular dendritic cells. Proc. Natl Acad. Sci. USA 99, 919–924 (2002).
Oldstone, M. B. et al. Lymphotoxin-α- and lymphotoxin-β-deficient mice differ in susceptibility to scrapie: evidence against dendritic cell involvement in neuroinvasion. J. Virol. 76, 4357–4363 (2002).
Gommerman, J. L. et al. Manipulation of lymphoid microenvironments in nonhuman primates by an inhibitor of the lymphotoxin pathway. J. Clin. Invest. 110, 1359–1369 (2002).
Gommerman, J. L. & Browning, J. L. Lymphotoxin/light, lymphoid microenvironments and autoimmune disease. Nature Rev. Immunol. 3, 642–655 (2003).
Montrasio, F. et al. Impaired prion replication in spleens of mice lacking functional follicular dendritic cells. Science 288, 1257–1259 (2000).
Mabbott, N. A., Mackay, F., Minns, F. & Bruce, M. E. Temporary inactivation of follicular dendritic cells delays neuroinvasion of scrapie. Nature Med. 6, 719–720 (2000).
Klein, M. A. et al. Complement facilitates early prion pathogenesis. Nature Med. 7, 488–492. (2001).
Mabbott, N. A., Bruce, M. E., Botto, M., Walport, M. J. & Pepys, M. B. Temporary depletion of complement component C3 or genetic deficiency of C1q significantly delays onset of scrapie. Nature Med. 7, 485–487 (2001).
Kovacs, G. G. et al. Complement activation in human prion disease. Neurobiol. Dis. 15, 21–28 (2004).
Blanquet-Grossard, F., Thielens, N. M., Vendrely, C., Jamin, M. & Arlaud, G. J. Complement protein C1q recognizes a conformationally modified form of the prion protein. Biochemistry 44, 4349–4356 (2005).
Felten, S. Y. et al. Noradrenergic sympathetic innervation of lymphoid organs. Prog. Allergy 43, 14–36 (1988).
Cole, S. & Kimberlin, R. H. Pathogenesis of mouse scrapie: dynamics of vacuolation in brain and spinal cord after intraperitoneal infection. Neuropathol. Appl. Neurobiol. 11, 213–227 (1985).
McBride, P. A. & Beekes, M. Pathological PrP is abundant in sympathetic and sensory ganglia of hamsters fed with scrapie. Neurosci. Lett. 265, 135–138 (1999).
Haik, S. et al. The sympathetic nervous system is involved in variant Creutzfeldt-Jakob disease. Nature Med. 9, 1121–1122 (2003).
Glatzel, M., Heppner, F. L., Albers, K. M. & Aguzzi, A. Sympathetic innervation of lymphoreticular organs is rate limiting for prion neuroinvasion. Neuron 31, 25–34. (2001).
Prinz, M. et al. Positioning of follicular dendritic cells within the spleen controls prion neuroinvasion. Nature 425, 957–962 (2003).
Forster, R. et al. A putative chemokine receptor, BLR1, directs B cell migration to defined lymphoid organs and specific anatomic compartments of the spleen. Cell 87, 1037–1047 (1996).
Denzer, K., Kleijmeer, M. J., Heijnen, H. F., Stoorvogel, W. & Geuze, H. J. Exosome: from internal vesicle of the multivesicular body to intercellular signaling device. J. Cell Sci. 113, 3365–3374 (2000).
Denzer, K. et al. Follicular dendritic cells carry MHC class II-expressing microvesicles at their surface. J. Immunol. 165, 1259–1265 (2000).
Leblanc, P. et al. Retrovirus infection strongly enhances scrapie infectivity release in cell culture. EMBO J. 25, 2674–2685 (2006).
Banks, W. A., Niehoff, M. L., Adessi, C. & Soto, C. Passage of murine scrapie prion protein across the mouse vascular blood-brain barrier. Biochem. Biophys. Res. Commun. 318, 125–130 (2004).
Mabbott, N. A., McGovern, G., Jeffrey, M. & Bruce, M. E. Temporary blockade of the tumor necrosis factor receptor signaling pathway impedes the spread of scrapie to the brain. J. Virol. 76, 5131–5139 (2002).
Takemura, S. et al. Lymphoid neogenesis in rheumatoid synovitis. J. Immunol. 167, 1072–1080 (2001).
Kaiserling, E. Newly-formed lymph nodes in the submucosa in chronic inflammatory bowel disease. Lymphology 34, 22–29 (2001).
Hogg, J. C. et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N. Engl. J. Med. 350, 2645–2653 (2004).
Drayton, D. L., Liao, S., Mounzer, R. H. & Ruddle, N. H. Lymphoid organ development: from ontogeny to neogenesis. Nature Immunol. 7, 344–353 (2006).
Alavaikko, M. J., Hansmann, M. L., Nebendahl, C., Parwaresch, M. R. & Lennert, K. Follicular dendritic cells in Hodgkin's disease. Am. J. Clin. Pathol. 95, 194–200 (1991).
Petrasch, S., Stein, H., Kosco, M. H. & Brittinger, G. Follicular dendritic cells in non-Hodgkin lymphomas: localisation, characterisation and pathophysiological aspects. Eur. J. Cancer 27, 1052–1056 (1991).
Magliozzi, R., Columba-Cabezas, S., Serafini, B. & Aloisi, F. Intracerebral expression of CXCL13 and BAFF is accompanied by formation of lymphoid follicle-like structures in the meninges of mice with relapsing experimental autoimmune encephalomyelitis. J. Neuroimmunol 148, 11–23 (2004).
Vernau, W., Jacobs, R. M., Valli, V. E. & Heeney, J. L. The immunophenotypic characterization of bovine lymphomas. Vet. Pathol. 34, 222–225 (1997).
Tuo, W. et al. Prpc and PrpSc at the fetal-maternal interface. J. Biol. Chem. 276, 18229–18234 (2001).
Aguzzi, A. Prions and the immune system: a journey through gut, spleen, and nerves. Adv. Immunol. 81, 123–171 (2003).
Prinz, M. et al. Oral prion infection requires normal numbers of Peyer's patches but not of enteric lymphocytes. Am. J. Pathol. 162, 1103–1111 (2003).
Houston, F., Foster, J. D., Chong, A., Hunter, N. & Bostock, C. J. Transmission of BSE by blood transfusion in sheep. Lancet 356, 999–1000 (2000).
Sigurdson, C. J. et al. PrP(CWD) lymphoid cell targets in early and advanced chronic wasting disease of mule deer. J. Gen. Virol. 83, 2617–2628 (2002).
Heggebo, R. et al. Detection of PrPSc in lymphoid tissues of lambs experimentally exposed to the scrapie agent. J. Comp. Pathol. 128, 172–181 (2003).
Mabbott, N. A., Young, J., McConnell, I. & Bruce, M. E. Follicular dendritic cell dedifferentiation by treatment with an inhibitor of the lymphotoxin pathway dramatically reduces scrapie susceptibility. J. Virol. 77, 6845–6854 (2003).
Neutra, M. R., Frey, A. & Kraehenbuhl, J. P. Epithelial M cells: gateways for mucosal infection and immunization. Cell 86, 345–348 (1996).
Jeffrey, M. et al. Transportation of prion protein across the intestinal mucosa of scrapie-susceptible and scrapie-resistant sheep. J. Pathol. 209, 4–14 (2006).
Kerneis, S., Bogdanova, A., Kraehenbuhl, J. P. & Pringault, E. Conversion by Peyer's patch lymphocytes of human enterocytes into M cells that transport bacteria. Science 277, 949–952 (1997).
Heppner, F. L. et al. Transepithelial prion transport by M cells. Nature Med. 7, 976–977 (2001).
Huang, F. P., Farquhar, C. F., Mabbott, N. A., Bruce, M. E. & MacPherson, G. G. Migrating intestinal dendritic cells transport PrPSc from the gut. J. Gen. Virol. 83, 267–271 (2002).
Aucouturier, P. et al. Infected splenic dendritic cells are sufficient for prion transmission to the CNS in mouse scrapie. J. Clin. Invest. 108, 703–708 (2001).
Hunter, N. et al. Transmission of prion diseases by blood transfusion. J. Gen. Virol. 83, 2897–2905 (2002).
Aguzzi, A. & Glatzel, M. vCJD tissue distribution and transmission by transfusion — a worst-case scenario coming true? Lancet 363, 411–412 (2004).
Peden, A. H., Head, M. W., Ritchie, D. L., Bell, J. E. & Ironside, J. W. Preclinical vCJD after blood transfusion in a PRNP codon 129 heterozygous patient. Lancet 364, 527–529 (2004).
Fischer, M. B., Roeckl, C., Parizek, P., Schwarz, H. P. & Aguzzi, A. Binding of disease-associated prion protein to plasminogen. Nature 408, 479–483 (2000).
Prinz, M. et al. Prion pathogenesis in the absence of Toll-like receptor signalling. EMBO Rep. 4, 195–199 (2003).
Adachi, O. et al. Targeted disruption of the MyD88 gene results in loss of IL-1- and IL-18-mediated function. Immunity 9, 143–150 (1998).
Hemmi, H. et al. A Toll-like receptor recognizes bacterial DNA. Nature 408, 740–745 (2000).
Sethi, S., Lipford, G., Wagner, H. & Kretzschmar, H. Postexposure prophylaxis against prion disease with a stimulator of innate immunity. Lancet 360, 229–230 (2002).
Heikenwalder, M. et al. Lymphoid follicle destruction and immunosuppression after repeated CpG oligodeoxynucleotide administration. Nature Med. 10, 187–192 (2004).
Beringue, V. et al. Role of spleen macrophages in the clearance of scrapie agent early in pathogenesis. J. Pathol. 190, 495–502 (2000).
Hsiao, K. K. et al. Serial transmission in rodents of neurodegeneration from transgenic mice expressing mutant prion protein. Proc. Natl Acad. Sci. USA 91, 9126–9130 (1994).
Lasmezas, C. I. et al. Transmission of the BSE agent to mice in the absence of detectable abnormal prion protein. Science 275, 402–405 (1997).
Tagliavini, F. et al. Amyloid fibrils in Gerstmann-Straussler-Scheinker disease (Indiana and Swedish kindreds) express only PrP peptides encoded by the mutant allele. Cell 79, 695–703 (1994).
Soto, C. Diagnosing prion diseases: needs, challenges and hopes. Nature Rev. Microbiol. 2, 809–819 (2004).
Polymenidou, M. et al. Coexistence of multiple PrPSc types in individuals with Creutzfeldt-Jakob disease. Lancet Neurol. 4, 805–814 (2005).
Saborio, G. P., Permanne, B. & Soto, C. Sensitive detection of pathological prion protein by cyclic amplification of protein misfolding. Nature 411, 810–813 (2001).
Soto, C. et al. Pre-symptomatic detection of prions by cyclic amplification of protein misfolding. FEBS Lett. 579, 638–642 (2005).
Castilla, J., Saa, P. & Soto, C. Detection of prions in blood. Nature Med. 11, 982–985 (2005).
Saa, P., Castilla, J. & Soto, C. Presymptomatic detection of prions in blood. Science 313, 92–94 (2006).
Duguid, J. R. & Dinauer, M. C. Library subtraction of in vitro cDNA libraries to identify differentially expressed genes in scrapie infection. Nucleic Acids Res. 18, 2789–2792 (1990).
Duguid, J. & Trzepacz, C. Major histocompatibility complex genes have an increased brain expression after scrapie infection. Proc. Natl Acad. Sci. USA 90, 114–117 (1993).
Dandoy-Dron, F. et al. Gene expression in scrapie. Cloning of a new scrapie-responsive gene and the identification of increased levels of seven other mRNA transcripts. J. Biol. Chem. 273, 7691–7697 (1998).
Miele, G., Manson, J. & Clinton, M. A novel erythroid-specific marker of transmissible spongiform encephalopathies. Nature Med. 7, 361–364 (2001).
Hsich, G., Kinney, K., Gibbs, C. J., Lee, K. H. & Harrington, M. G. The 14–3–3 brain protein in cerebrospinal fluid as a marker for transmissible spongiform encephalopathies. N. Engl. J. Med. 335, 924–930 (1996).
Beaudry, P. et al. 14–3–3 protein, neuron-specific enolase, and S-100 protein in cerebrospinal fluid of patients with Creutzfeldt-Jakob disease. Dement. Geriatr. Cogn. Disord. 10, 40–46 (1999).
Flechsig, E. et al. Prion protein devoid of the octapeptide repeat region restores susceptibility to scrapie in PrP knockout mice. Neuron 27, 399–408 (2000).
Klohn, P. C., Stoltze, L., Flechsig, E., Enari, M. & Weissmann, C. A quantitative, highly sensitive cell-based infectivity assay for mouse scrapie prions. Proc. Natl Acad. Sci. USA 100, 11666–11671 (2003).
Traggiai, E. et al. Development of a human adaptive immune system in cord blood cell-transplanted mice. Science 304, 104–107 (2004).
Macchiarini, F., Manz, M. G., Palucka, A. K. & Shultz, L. D. Humanized mice: are we there yet? J. Exp. Med. 202, 1307–1311 (2005).
Silveira, J. R. et al. The most infectious prion protein particles. Nature 437, 257–261 (2005).
Dickinson, A. G. & Meikle, V. M. Host-genotype and agent effects in scrapie incubation: change in allelic interaction with different strains of agent. Mol. Gen. Genet. 112, 73–79 (1971).
Weissmann, C. A 'unified theory' of prion propagation. Nature 352, 679–683 (1991).
King, C. Y. & Diaz-Avalos, R. Protein-only transmission of three yeast prion strains. Nature 428, 319–323 (2004).
Tanaka, M., Chien, P., Naber, N., Cooke, R. & Weissman, J. S. Conformational variations in an infectious protein determine prion strain differences. Nature 428, 323–328 (2004).
Tanaka, M., Collins, S. R., Toyama, B. H. & Weissman, J. S. The physical basis of how prion conformations determine strain phenotypes. Nature 442, 585–589 (2006).
Nonno, R. et al. Efficient transmission and characterization of Creutzfeldt-Jakob disease strains in bank voles. PLoS Pathog. 2, e12 (2006).
Acknowledgements
We thank F. Baumann, C. Sigurdson and A. Schumacher for their active discussions and critical reading of this review. A. A. is supported by grants from the EU, the Swiss National Foundation, the National Centre of Competence in Research on Neural Plasticity and Repair, the Stammbach Foundation and the Ernst-Jung Foundation. M.H. is supported by the Foundation for Research at the Medical Faculty, University of Zurich, the Bonizzi-Theler Stiftung and by the Verein zur Förderung des akademischen Nachwuchses (FAN).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
Glossary
- Iatrogenic transmission
-
The transmission of infectious agents as a consequence of a medical procedure.
- Lymphoreticular system
-
The lymphoreticular system (LRS) is divided into primary and secondary lymphoid tissues. Primary lymphoid organs are anatomical sites where the cells of the LRS are generated, including the bone marrow and the thymus. Secondary lymphoid organs are sites where the LRS cells function. These sites include the spleen, the lymph nodes and mucosa associated lymphoid tissue. Tertiary lymphoid organs arise at sites of chronic inflammation.
- Peripheral prion inoculation
-
This defines any administration of the prion agent other than into the central nervous system, including intraperitoneal (ip), intravenous (iv), oral or intraocular (io) administration.
- Splenic stroma
-
The splenic stroma defines those cells in the spleen, which are of non-hematopoietic origin and are resistant to γ-irradiation.
- Splenic pulp
-
The splenic pulp can be subdivided into the red and the white splenic pulp. The splenic red pulp fills the sinuses of the spleen and its composition includes macrophages and red blood cells. The white splenic pulp is a parenchymatous tissue of the spleen consisting of compact masses of lymphatic cells and contains the germinal centres.
- Homeostatic chemokine
-
A subset of the chemokine family that are constitutively expressed in pre-formed lymphoid tissues and which promote and maintain the organization of this tissue.
- FDC-M1 positive cluster
-
A dense network of cells found in germinal centres, immunoreactive for the FDC-M1 antibody and the CD21/35 receptor. Tingible body macrophages also stain positive for FDC-M1 but are morphologically distinct.
- Lymphotoxin
-
(LT). LTα and LTβ are proinflammatory cytokines that belong to the tumour necrosis factor (TNF) superfamily. They are mainly expressed by B- and T lymphocytes, and natural killer cells. LTs exist as membrane-bound heterotrimers (LTα1β2 or LTα2β1) or as secreted homotrimers (LTα3). LTs bind TNFR1 or LTβR inducing a signalling cascade that is important for the maturation and maintenance of follicular dendritic cells.
- Ectopic expression
-
This defines the expression of a gene in an abnormal site in an organism. This phenomenon can be induced by disease or by a pathogen, but can be also induced artificially by expressing a transgene with a tissue or cell-specific promoter.
- LTβR pathway
-
Following interaction with lymphotoxin ligands, LTβR can activate an 'alternative' pathway for NFκB, inducing the expression of genes such as homeostatic chemokines and tumour necrosis superfamily members, which is important for the maintenance and maturation of follicular dendritic cells.
- Extra-neural compartment
-
This includes organs and cells that do not belong to the central or peripheral nervous system.
- Innervation pattern
-
This describes the type (qualitative and quantitative) of innervation present in a peripheral organ that does not belong to the central nervous system.
Rights and permissions
About this article
Cite this article
Aguzzi, A., Heikenwalder, M. Pathogenesis of prion diseases: current status and future outlook. Nat Rev Microbiol 4, 765–775 (2006). https://doi.org/10.1038/nrmicro1492
Issue Date:
DOI: https://doi.org/10.1038/nrmicro1492
This article is cited by
-
Classical bovine spongiform encephalopathy and chronic wasting disease: two sides of the prion coin
Animal Diseases (2023)
-
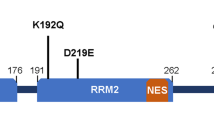
The G127V variant of the prion protein interferes with dimer formation in vitro but not in cellulo
Scientific Reports (2021)
-
Administration of FK506 from Late Stage of Disease Prolongs Survival of Human Prion-Inoculated Mice
Neurotherapeutics (2020)
-
IVIG Delays Onset in a Mouse Model of Gerstmann-Sträussler-Scheinker Disease
Molecular Neurobiology (2019)
-
Strain-dependent profile of misfolded prion protein aggregates
Scientific Reports (2016)