Key Points
-
Resistance to frontline artemisinins and partner drugs is now causing the failure of artemisinin-based combination therapies against Plasmodium falciparum in southeast Asia.
-
Triple artemisinin-based combination therapies are being developed, but their design and deployment require an understanding of background resistance and associated genetic mutations of the parasite populations being targeted.
-
P. falciparum Kelch 13 (PfKelch13), the marker for artemisinin resistance in P. falciparum malaria, is not an enzyme or a pump but rather is predicted to be a substrate adapter for a cullin E3 ligase, with a putative substrate of P. falciparum phosphatidylinositol 3-kinase (PfPI3K) and a redox sensor.
-
Mutation in pfkelch13 appears to increase parasite phosphatidylinositol-3-phosphate (PtdIns3P) as well as the unfolded protein response, and both have been proposed as mechanisms of artemisinin resistance.
-
Additional PfKelch13-independent mechanisms of artemisinin resistance have appeared in southeast Asia.
-
The identification of mechanisms of resistance to artemisinin and its partner drugs as well as of new targets for chemotherapy that can eliminate resistant infection in both symptomatic and asymptomatic populations is needed for malaria elimination.
Abstract
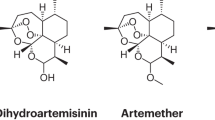
A marked decrease in malaria-related deaths worldwide has been attributed to the administration of effective antimalarials against Plasmodium falciparum, in particular, artemisinin-based combination therapies (ACTs). Increasingly, ACTs are also used to treat Plasmodium vivax, the second major human malaria parasite. However, resistance to frontline artemisinins and partner drugs is now causing the failure of P. falciparum ACTs in southeast Asia. In this Review, we discuss our current knowledge of markers and mechanisms of resistance to artemisinins and ACTs. In particular, we describe the identification of mutations in the propeller domains of Kelch 13 as the primary marker for artemisinin resistance in P. falciparum and explore two major mechanisms of resistance that have been independently proposed: the activation of the unfolded protein response and proteostatic dysregulation of parasite phosphatidylinositol 3- kinase. We emphasize the continuing challenges and the imminent need to understand mechanisms of resistance to improve parasite detection strategies, develop new combinations to eliminate resistant parasites and prevent their global spread.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
World Health Organization. World Malaria Report 2015 (WHO, 2015).
World Health Organization. World Malaria Report 2016 (WHO, 2016).
Guerra, C. A. et al. The international limits and population at risk of Plasmodium vivax transmission in 2009. PLOS Negl. Trop. Dis. 4, e774 (2010).
Haldar, K., Murphy, S. C., Milner, D. A. & Taylor, T. E. Malaria: mechanisms of erythrocytic infection and pathological correlates of severe disease. Annu. Rev. Pathol. 2, 217–249 (2007).
Milner, D. A. Jr. et al. Quantitative assessment of multiorgan sequestration of parasites in fatal pediatric cerebral Malaria. J. Infect. Dis. 212, 1317–1321 (2015).
Okell, L. C., Drakeley, C. J., Ghani, A. C., Bousema, T. & Sutherland, C. J. Reduction of transmission from malaria patients by artemisinin combination therapies: a pooled analysis of six randomized trials. Malar. J. 7, 125 (2008).
Jensen, M. & Mehlhorn, H. Seventy-five years of Resochin in the fight against malaria. Parasitol. Res. 105, 609–627 (2009).
Jong, E. C. & Nothdurft, H. D. Current drugs for antimalarial chemoprophylaxis: a review of efficacy and safety. J. Travel Med. 8, S48–S56 (2001).
Mawson, A. Mefloquine use, psychosis, and violence: a retinoid toxicity hypothesis. Med. Sci. Monit. 19, 579–583 (2013).
Verdrager, J. Epidemiology of the emergence and spread of drug-resistant falciparum malaria in South-East Asia and Australasia. J. Trop. Med. Hyg. 89, 277–289 (1986).
Verdrager, J. Localized permanent epidemics: the genesis of chloroquine resistance in Plasmodium falciparum. Southeast Asian J. Trop. Med. Public Health 26, 23–28 (1995).
Payne, D. Spread of chloroquine resistance in Plasmodium falciparum. Parasitol. Today 3, 241–246 (1987).
Gesase, S. et al. High resistance of Plasmodium falciparum to sulphadoxine/pyrimethamine in Northern Tanzania and the emergence of dhps resistance mutation at codon 581. PLOS ONE 4, e4569 (2009).
Mixson-Hayden, T. et al. Evidence of selective sweeps in genes conferring resistance to chloroquine and pyrimethamine in Plasmodium falciparum isolates in India. Antimicrob. Agents Chemother. 54, 997–1006 (2009).
Shah, N. K. et al. Antimalarial drug resistance of Plasmodium falciparum in India: changes over time and space. Lancet. Infect. Dis. 11, 57–64 (2011).
Meshnick, S. R., Taylor, T. E. & Kamchonwongpaisan, S. Artemisinin and the antimalarial endoperoxides: from herbal remedy to targeted chemotherapy. Microbiol. Rev. 60, 301–315 (1996).
Djimde, A. et al. A molecular marker for chloroquine-resistant falciparum malaria. N. Engl. J. Med. 344, 257–263 (2001).
Ariey, F. et al. A molecular marker of artemisinin resistant Plasmodium falciparum malaria. Nature 505, 50–55 (2014). This study presents the identification of the first marker of artemisinin resistance in P. falciparum malaria, which was shown to be causal in later genetic studies.
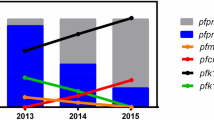
Ashley, E. A. et al. Spread of artemisinin resistance in Plasmodium falciparum malaria. N. Engl. J. Med. 371, 411–423 (2014). This is the first of a series of clinical and epidemiological studies showing that delayed clearance time of artemisinin resistance in patients was associated with mutations in the β-propeller domain of PfKelch13 and with their spread in southeast Asia.
Takala-Harrison, S. et al. Independent emergence of artemisinin resistance mutations among Plasmodium falciparum in Southeast Asia. J. Infect. Dis. 211, 670–679 (2015).
Tun, K. M. et al. Spread of artemisinin-resistant Plasmodium falciparum in Myanmar: a cross-sectional survey of the K13 molecular marker. Lancet Infect. Dis. 15, 415–421 (2015).
Cheeseman, I. H. et al. A major genome region underlying artemisinin resistance in malaria. Science 336, 79–82 (2012).
Miotto, O. et al. Genetic architecture of artemisinin-resistant Plasmodium falciparum. Nat. Genet. 47, 226–234 (2015). This GWAS identifies the population structure of clinically resistant parasites and the genomic complexity of artemisinin resistance in southeast Asia.
Fidock, D. A., Rosenthal, P. J., Croft, S. L., Brun, R. & Nwaka, S. Antimalarial drug discovery: efficacy models for compound screening. Nat. Rev. Drug Discov. 3, 509–520 (2004).
Fidock, A. D. et al. Mutations in the P. falciparum digestive vacuole transmembrane protein PfCRT and evidence for their role in chloroquine resistance. Mol. Cell 6, 861–871 (2000).
Sidhu, A. B. S., Verdier-Pinard, D. & Fidock, D. A. Chloroquine resistance in Plasmodium falciparum malaria parasites conferred by pfcrt mutations. Science 298, 210–213 (2002).
Triglia, T., Wang, P., Sims, P. F., Hyde, J. E. & Cowman, A. F. Allelic exchange at the endogenous genomic locus in Plasmodium falciparum proves role of dihydropteroate synthase in sulfadoxine-resistant malaria. EMBO J. 17, 3807–3815 (1998).
Korsinczky, M. et al. Mutations in Plasmodium falciparum Cytochrome b that are associated with atovaquone resistance are located at a putative drug-binding site. Antimicrob. Agents Chemother. 44, 2100–2108 (2000).
Ismail, H. M. et al. Artemisinin activity-based probes identify multiple molecular targets within the asexual stage of the malaria parasites Plasmodium falciparum 3D7. Proc. Natl Acad. Sci. 113, 2080–2085 (2016). This study, together with reference 30, suggests 'proteopathic' toxicity of artemisinins.
Wang, J. et al. Haem-activated promiscuous targeting of artemisinin in Plasmodium falciparum. Nat. Commun. 6, 10111 (2015).
Ghorbal, M. et al. Genome editing in the human malaria parasite Plasmodium falciparum using the CRISPR-Cas9 system. Nat. Biotechnol. 32, 819–821 (2014). This is the first report of the use of CRISPR–Cas9 in P. falciparum to engineer a single point mutation in the genome of the sensitive African strain PfNF54 to yield a PfNF54 strain with the PfKelch13-C580Y mutation, which shows an RSA value of 13–14; this study also proves that the pfkelch13 mutation was causal for artemisinin resistance.
Straimer, J. et al. Drug resistance. K13-propeller mutations confer artemisinin resistance in Plasmodium falciparum clinical isolates. Science 347, 428–431 (2015). In this study, zinc-finger nuclease technology is used to rapidly introduce or remove PfKelch13 β-propeller mutations in P. falciparum reference strains and clinical isolates from Cambodia to prove that different mutations cause different levels of resistance (as measured by the RSA), the extent of which is sensitive to the genetic backgrounds of the parasites.
Gupta, V. A. & Beggs, A. H. Kelch proteins: emerging roles in skeletal muscle development and diseases. Skelet. Muscle 4, 11 (2014).
Nikesitch, N. & Ling, S. C. Molecular mechanisms in multiple myeloma drug resistance. J. Clin. Pathol. 69, 97–101 (2016).
Mok, S. et al. Population transcriptomics of human malaria parasites reveals the mechanism of artemisinin resistance. Science 347, 431–435 (2015). This study presents transcriptomic signatures of 1,000 clinical strains to reveal that the induction of the parasite UPR is associated with artemisinin resistance.
Mbengue, A. et al. A molecular mechanism of artemisinin resistance in Plasmodium falciparum malaria. Nature 520, 683–687 (2015). This study shows that mutations of PfKelch13 increase PfPI3K to elevate PtdIns3P and confer artemisinin resistance.
Amato, R. et al. Genetic markers associated with dihydroartemisinin–piperaquine failure in Plasmodium falciparum malaria in Cambodia: a genotype-phenotype association study. Lancet Infect. Dis. 17, 164–173 (2017). This study, together with reference 38, identifies the molecular markers associated with P. falciparum that are dually resistant to ACT with artemisinins and PPQ.
Witkowski, B. et al. A surrogate marker of piperaquine-resistant Plasmodium falciparum malaria: a phenotype–genotype association study. Lancet Infect. Dis. 17, 174–183 (2017).
Ataide, R. et al. Host immunity to Plasmodium falciparum and the assessment of emerging artemisinin resistance in a multinational cohort. Proc. Natl Acad. Sci. USA 114, 3515–3520 (2017). This is the first study investigating the effect of immunity on the parasite clearance rates associated with artemisinin resistance.
Tumwebaze, P. et al. Changing antimalarial drug resistance patterns identified by surveillance at three sites in Uganda. J. Infect. Dis. 215, 631–635 (2017).
Costa, G. L. et al. Assessment of copy number variation in genes related to drug resistance in Plasmodium vivax and Plasmodium falciparum isolates from the Brazilian Amazon and a systematic review of the literature. Malar. J. 16, 152 (2017).
Peterson, D. S., Walliker, D. & Wellems, T. E. Evidence that a point mutation in dihydrofolate reductase-thymidylate synthase confers resistance to pyrimethamine in falciparum malaria. Proc. Natl Acad. Sci. USA 85, 9114–9118 (1988).
Gregson, A. & Plowe, C. V. Mechanisms of resistance of malaria parasites to antifolates. Pharmacol. Rev. 57, 117–145 (2005).
Mishra, N. et al. Declining efficacy of artesunate plus sulphadoxine-pyrimethamine in northeastern India. Malar. J. 13, 284 (2014).
Srivastava, I. K. & Vaidya, A. B. A mechanism for the synergistic antimalarial action of atovaquone and proguanil. Antimicrob. Agents Chemother. 43, 1334–1339 (1999).
Vaidya, A. B. in Treatment and Prevention of Malaria: Antimalarial Drug Chemistry, Action and Use (eds Henry Staines, M. & Sanjeev Krishna) 127–139 (Springer Basel, 2012).
Goodman, C. D. & Buchanan, H. D. & McFadden, G. I. Is the mitochondrion a good malaria drug target? Trends Parasitol. 33, 185–193 (2017).
Sigala, P. A. & Goldberg, D. E. The peculiarities and paradoxes of Plasmodium heme metabolism. Annu. Rev. Microbiol. 68, 259–278 (2014).
Nkrumah, L. J. et al. Probing the multifactorial basis of Plasmodium falciparum quinine resistance: evidence for a strain-specific contribution of the sodium–proton exchanger PfNHE. Mol. Biochem. Parasitol. 165, 122–131 (2009).
Cooper, R. A. et al. Alternative mutations at position 76 of the vacuolar transmembrane protein PfCRT are associated with chloroquine resistance and unique stereospecific quinine and quinidine responses in Plasmodium falciparum. Mol. Pharmacol. 61, 35–42 (2002).
Cooper, R. A. et al. Mutations in transmembrane domains 1, 4 and 9 of the Plasmodium falciparum chloroquine resistance transporter alter susceptibility to chloroquine, quinine and quinidine. Mol. Microbiol. 63, 270–282 (2007).
Petersen, I. et al. Balancing drug resistance and growth rates via compensatory mutations in the Plasmodium falciparum chloroquine resistance transporter. Mol. Microbiol. 97, 381–395 (2015).
Veiga, M. I. et al. Globally prevalent PfMDR1 mutations modulate Plasmodium falciparum susceptibility to artemisinin-based combination therapies. Nat. Commun. 7, 11553 (2016).
Pascual, A. et al. In vitro piperaquine susceptibility is not associated with the Plasmodium falciparum chloroquine resistance transporter gene. Malar. J. 12, 431 (2013).
Dhingra, S. K. et al. A variant PfCRT isoform can contribute to Plasmodium falciparum resistance to the first-line partner drug piperaquine. mBio 8, e00303–00317 (2017).
Venkatesan, M. et al. Polymorphisms in Plasmodium falciparum chloroquine resistance transporter and multidrug resistance 1 genes: parasite risk factors that affect treatment outcomes for P. falciparum malaria after artemether-lumefantrine and artesunate-amodiaquine. Am. J. Trop. Med. Hyg. 91, 833–843 (2014).
Blasco, B., Leroy, D. & Fidock, D. A. Antimalarial drug resistance: linking Plasmodium falciparum parasite biology to the clinic. Nat. Med. 23, 917–928 (2017).
Takala-Harrison, S. et al. Genetic loci associated with delayed clearance of Plasmodium falciparum following artemisinin treatment in Southeast Asia. Proc. Natl Acad. Sci. USA 110, 240–245 (2013).
Miotto, O. et al. Multiple populations of artemisinin resistant Plasmodium falciparum in Cambodia. Nat. Genet. 45, 648–655 (2013).
Mok, S. et al. Artemisinin resistance in Plasmodium falciparum is associated with an altered temporal pattern of transcription. BMC Genomics 12, 391 (2011).
Ménard, D. et al. A worldwide map of Plasmodium falciparum K13-propeller polymorphisms. N. Engl. J. Med. 374, 2453–2464 (2016). This study provides a summary of the distribution of polymorphisms of pfkelch13 that are linked to artemisinin resistance (or not) on a global scale.
Huang, F. et al. A single mutation in K13 predominates in Southern China and is associated with delayed clearance of Plasmodium falciparum following artemisinin treatment. J. Infect. Dis. 212, 1629–1635 (2015).
Tun, K. M. et al. Parasite clearance rates in Upper Myanmar indicate a distinctive artemisinin resistance phenotype: a therapeutic efficacy study. Malar. J. 15, 185 (2016).
Mishra, N. et al. Surveillance for artemisinin resistance in Plasmodium falciparum in India using the kelch13 molecular marker. Antimicrob. Agents Chemother. 59, 2548–2553 (2015).
Mishra, N. et al. Emerging polymorphisms in falciparum Kelch 13 gene in Northeastern region of India. Malar. J. 15, 583 (2016).
Korenromp, E. L., Williams, B. G., Gouws, E., Dye, C. & Snow, R. W. Measurement of trends in childhood malaria mortality in Africa: an assessment of progress toward targets based on verbal autopsy. Lancet Infect. Dis. 3, 349–358 (2003).
Trape, J. F. et al. Impact of chloroquine resistance on malaria mortality. C. R. Acad. Sci. III 321, 689–697 (1998).
World Health Organization. Global report on antimalarial drug efficacy and drug resistance: 2000–2010. (WHO, 2010).
Noedl, H. et al. Evidence of artemisinin-resistant malaria in western Cambodia. N. Engl. J. Med. 359, 2619–2620 (2008).
Dondorp, A. M. et al. Artemisinin resistance in Plasmodium falciparum malaria. N. Engl. J. Med. 361, 1714 (2009).
Barnes, K. I. et al. Effect of artemether-lumefantrine policy and improved vector control on malaria burden in KwaZulu-Natal, South Africa. PLOS Med. 2, e330 (2005).
Bhattarai, A. et al. Impact of artemisinin-based combination therapy and insecticide-treated nets on malaria burden in Zanzibar. PLOS Med. 4, e309 (2007).
Phommasone, K. et al. Asymptomatic Plasmodium infections in 18 villages of southern Savannakhet Province, Lao PDR (Laos). Malar. J. 15, 296 (2016).
Worldwide Antimalarial Resistance Network. Tracking resistance to artemisinin collaboration II. WWARN http://www.wwarn.org/Working-Together/Partner-Projects/Tracking-Resistance-Artemisinin-Collaboration-ii (2017).
Imwong, M. et al. The spread of artemisinin-resistant Plasmodium falciparum in the Greater Mekong subregion: a molecular epidemiology observational study. Lancet. Infect. Dis. 5, 491–497 (2017).
Srimuang, K. et al. Analysis of anti-malarial resistance markers in pfmdr1 and pfcrt across Southeast Asia in the tracking resistance to artemisinin collaboration. Malar. J. 15, 541 (2016).
Xie, S. C. et al. Haemoglobin degradation underpins the sensitivity of early ring stage Plasmodium falciparum to artemisinins. J. Cell Sci. 129, 406–416 (2016).
Mukherjee, A. et al. Artemisinin resistance without pfkelch13 mutations in Plasmodium falciparum isolates from Cambodia. Malar. J. 16, 195 (2017).
Cerqueira, G. C. et al. Longitudinal genomic surveillance of Plasmodium falciparum malaria parasites reveals complex genomic architecture of emerging artemisinin resistance. Genome Biol. 18, 78 (2017).
Price, R. N. et al. Vivax malaria: neglected and not benign. Am. J. Trop. Med. Hyg. 77, 79–87 (2007).
Suwanarusk, R. et al. Amplification of pvmdr1 associated with multidrug-resistant Plasmodium vivax. J. Infect. Dis. 198, 1558–1564 (2008).
Imwong, M. et al. Gene amplification of the multidrug resistance 1 gene of Plasmodium vivax isolates from Thailand, Laos, and Myanmar. Antimicrob. Agents Chemother. 52, 2657–2659 (2008).
Lu, F. et al. Mutations in the antifolate-resistance-associated genes dihydrofolate reductase and dihydropteroate synthase in Plasmodium vivax isolates from malaria-endemic countries. Am. J. Trop. Med. Hyg. 83, 474–479 (2010).
Price, R. N. et al. Global extent of chloroquine-resistant Plasmodium vivax: a systematic review and meta-analysis. Lancet. Infect. Dis. 14, 982–991 (2014).
Douglas, N. M., Anstey, N. M., Angus, B. J., Nosten, F. & Price, R. N. Artemisinin combination therapy for vivax malaria? Lancet Infect. Dis. 10, 405–416 (2010).
Witkowski, B. et al. Novel phenotypic assays for the detection of artemisinin-resistant Plasmodium falciparum malaria in Cambodia: in-vitro and ex-vivo drug-response studies. Lancet. Infect. Dis. 13, 1043–1049 (2013). This study presents the development of an in vitro correlate of in vivo P. falciparum artemisinin-resistant malaria.
Taguchi, K. & Yamamoto, M. The KEAP1-NRF2 System in Cancer. Front. Oncol. 7, 85 (2017).
Fairhurst, R. M. & Dondorp, A. M. Artemisinin-Resistant Plasmodium falciparum Malaria. Microbiol. Spectr. 4, 3 (2016).
Paloque, L., Ramadani, A. P., Mercereau-Puijalon, O., Augereau, J. M. & Benoit-Vical, F. Plasmodium falciparum: multifaceted resistance to artemisinins. Malar. J. 15, 149 (2016).
Sambuughin, N. et al. KBTBD13 interacts with Cullin 3 to form a functional ubiquitin ligase. Biochem. Biophys. Res. Commun. 421, 743–749 (2012).
Geyer, R., Wee, S., Anderson, S., Yates, J. & Wolf, D. A. BTB/POZ domain proteins are putative substrate adaptors for cullin 3 ubiquitin ligases. Mol. Cell 12, 783–790 (2003).
Canning, P. et al. Structural basis for Cul3 protein assembly with the BTB-Kelch family of E3 ubiquitin ligases. J. Biol. Chem. 288, 7803–7814 (2013).
Dogovski, C. et al. Targeting the cell stress response of Plasmodium falciparum to overcome artemisinin resistance. PLOS Biol. 13, e1002132 (2015).
Li, H. et al. Structure- and function-based design of Plasmodium-selective proteasome inhibitors. Nature 530, 233–236 (2016).
Prasad, R. et al. Blocking Plasmodium falciparum development via dual inhibition of hemoglobin degradation and the ubiquitin proteasome system by MG132. PLOS One 8, e73530 (2013).
Zhang, M. et al. PK4, a eukaryotic initiation factor 2α (eIF2α) kinase, is essential for the development of the erythrocytic cycle of Plasmodium. Proc. Natl Acad. Sci. 109, 3956–3961 (2012).
Cheng, Q., Kyle, D. E. & Gatton, M. L. Artemisinin resistance in Plasmodium falciparum: a process linked to dormancy? Int. J. Parasitol. Drugs Drug Resist. 2, 249–255 (2012).
Vanhaesebroeck, B. et al. Synthesis and function of 3-phosphorylated inositol lipids. Annu. Rev. Biochem. 70, 535–602 (2001).
Vaid, A., Ranjan, R., Smythe, W. A., Hoppe, H. C. & Sharma, P. PfPI3K, a phosphatidylinositol-3 kinase from Plasmodium falciparum, is exported to the host erythrocyte and is involved in hemoglobin trafficking. Blood 115, 2500–2507 (2010).
Dall'Armi, C., Devereaux, Kelly, A. & Di Paolo, G. The role of lipids in the control of autophagy. Curr. Biol. 23, R33–R45 (2013).
Tawk, L. et al. Phosphatidylinositol 3-phosphate, an essential lipid in Plasmodium, localizes to the food vacuole membrane and the apicoplast. Eukaryot. Cell 9, 1519–1530 (2010).
Tawk, L. et al. Phosphatidylinositol 3-monophosphate is involved in toxoplasma apicoplast biogenesis. PLOS Pathog. 7, e1001286 (2011).
Bhattacharjee, S., Stahelin, R. V., Speicher, K. D., Speicher, D. W. & Haldar, K. Endoplasmic reticulum PI(3)P lipid binding targets malaria proteins to the host cell. Cell 148, 201–212 (2012).
Cervantes, S. et al. The multifunctional autophagy pathway in the human malaria parasite. Plasmodium falciparum. Autophagy 10, 80–92 (2014).
Kitamura, K. et al. Autophagy-related Atg8 localizes to the apicoplast of the human malaria parasite Plasmodium falciparum. PLOS ONE 7, e42977 (2012).
Cyrklaff, M. et al. Oxidative insult can induce malaria-protective trait of sickle and fetal erythrocytes. Nat. Commun. 7, 13401 (2016).
Kavishe, R. A., Koenderink, J. B. & Alifrangis, M. Oxidative stress in malaria and artemisinin combination therapy: pros and cons. FEBS J. 284, 2579–2591 (2017).
Phillips, M. A. et al. Malaria. Nat Rev. Dis. Primers 3, 17050 (2017).
Straimer, J. et al. Plasmodium falciparum K13 mutations differentially impact ozonide susceptibility and parasite fitness in vitro. mBio 8, e00172–e00117 (2017).
O'Neill, P. M. et al. A tetraoxane-based antimalarial drug candidate that overcomes PfK13-C580Y dependent artemisinin resistance. Nat. Commun. 8, 15159 (2017).
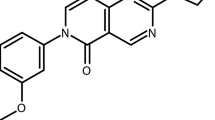
Dembele, L. et al. The Plasmodium PI(4)K inhibitor KDU691 selectively inhibits dihydroartemisinin-pretreated Plasmodium falciparum ring-stage parasites. Sci. Rep. 7, 2325 (2017). References 111–114 present several potential new therapeutics from the antimalaria discovery and development pipeline.
Le Bihan, A. et al. Characterization of novel antimalarial compound ACT-451840: preclinical assessment of activity and dose-efficacy modeling. PLOS Med. 13, e1002138 (2016).
McCarthy, J. S. et al. Safety, tolerability, pharmacokinetics, and activity of the novel long-acting antimalarial DSM265: a two-part first-in-human phase 1a/1b randomised study. Lancet. Infect. Diseases 17, 626–635 (2017).
Baragana, B. et al. A novel multiple-stage antimalarial agent that inhibits protein synthesis. Nature 522, 315–320 (2015).
Mohon, A. et al. Mutations in Plasmodium falciparum K13 propeller gene from Bangladesh (2009–2013). Malar. J. 13, 431 (2014).
Witkowski, B. et al. Reduced artemisinin susceptibility of Plasmodium falciparum ring stages in western Cambodia. Antimicrob. Agents Chemother. 57, 914–923 (2012).
Bhaya, D., Davison, M. & Barrangou, R. CRISPR-Cas systems in bacteria and archaea: versatile small RNAs for adaptive defense and regulation. Annu. Rev. Genet. 45, 273–297 (2011).
Straimer, J. et al. Site-specific genome editing in Plasmodium falciparum using engineered zinc-finger nucleases. Nat. Methods 9, 993–998 (2012).
Amaratunga, C. et al. Dihydroartemisinin-piperaquine resistance in Plasmodium falciparum malaria in Cambodia: a multisite prospective cohort study. Lancet Infect. Dis. 16, 357–365 (2016).
Phyo, A. P. et al. Emergence of artemisinin-resistant malaria on the western border of Thailand: a longitudinal study. Lancet 379, 1960–1966 (2012).
Thriemer, K. et al. Delayed parasite clearance after treatment with dihydroartemisinin-piperaquine in Plasmodium falciparum malaria patients in central Vietnam. Antimicrob. Agents Chemother. 58, 7049–7055 (2014).
Wang, Z. et al. Prevalence of K13-propeller polymorphisms in Plasmodium falciparum from China–Myanmar border in 2007–2012. Malar. J. 14, 168 (2015).
Ye, R. et al. Distinctive origin of artemisinin-resistant Plasmodium falciparum on the China–Myanmar border. Sci. Rep. 6, 20100 (2016).
Thanh, N. V. et al. Rapid decline in the susceptibility of Plasmodium falciparum to dihydroartemisinin–piperaquine in the south of Vietnam. Malar. J. 16, 27 (2017).
Boulle, M. et al. Artemisinin-resistant Plasmodium falciparum K13 mutant alleles, Thailand–Myanmar border. Emerg. Infect. Dis. 22, 1503–1505 (2016).
Gama, B. E., Lacerda, M. V., Daniel-Ribeiro, C. T. & Ferreira-da-Cruz Mde, F. Chemoresistance of Plasmodium falciparum and Plasmodium vivax parasites in Brazil: consequences on disease morbidity and control. Mem. Inst. Oswaldo Cruz 106, 159–166 (2011).
Goncalves, L. A., Cravo, P. & Ferreira, M. U. Emerging Plasmodium vivax resistance to chloroquine in South America: an overview. Mem. Inst. Oswaldo Cruz 109, 534–539 (2014).
Delves, M. et al. The activities of current antimalarial drugs on the life cycle stages of Plasmodium: a comparative study with human and rodent parasites. PLoS Med. 9, e1001169 (2012).
Sa, J. M. et al. Geographic patterns of Plasmodium falciparum drug resistance distinguished by differential responses to amodiaquine and chloroquine. Proc. Natl Acad. Sci. USA 106, 18883–18889 (2009).
Agrawal, S. et al. Association of a novel mutation in the Plasmodium falciparum chloroquine resistance transporter with decreased piperaquine sensitivity. J. Infect. Dis. 216, 468–476 (2017).
Madamet, M. et al. The Plasmodium falciparum chloroquine resistance transporter is associated with the ex vivo P. falciparum African parasite response to pyronaridine. Parasit. Vectors 9, 77 (2016).
Sidhu, A. B. S. et al. Decreasing pfmdr1 copy number in Plasmodium falciparum malaria heightens susceptibility to mefloquine, lumefantrine, halofantrine, quinine, and artemisinin. J. Infect. Dis. 194, 528–535 (2006).
Sisowath, C. et al. In vivo selection of Plasmodium falciparum pfmdr1 86N coding alleles by artemether-lumefantrine (Coartem). J. Infect. Dis. 191, 1014–1017 (2005).
Sidhu, A. B., Valderramos, S. G. & Fidock, D. A. pfmdr1 mutations contribute to quinine resistance and enhance mefloquine and artemisinin sensitivity in Plasmodium falciparum. Mol. Microbiol. 57, 913–926 (2005).
Price, R. N. et al. Mefloquine resistance in Plasmodium falciparum and increased pfmdr1 gene copy number. Lancet 364, 438–447 (2004).
Sisowath, C. et al. The role of pfmdr1 in Plasmodium falciparum tolerance to artemether-lumefantrine in Africa. Trop. Med. Int. Health 12, 736–742 (2007).
Uhlemann, A. C. & Krishna, S. Antimalarial multi-drug resistance in Asia: mechanisms and assessment. Curr. Top. Microbiol. Immunol. 295, 39–53 (2005).
Imwong, M. et al. Limited polymorphism in the dihydropteroate synthetase gene (dhps) of Plasmodium vivax isolates from Thailand. Antimicrob. Agents Chemother. 49, 4393–4395 (2005).
Parzy, D. et al. Proguanil resistance in Plasmodium falciparum African isolates: assessment by mutation-specific polymerase chain reaction and in vitro susceptibility testing. Am. J. Trop. Med. Hyg. 57, 646–650 (1997).
Gil, J. P. et al. Detection of atovaquone and Malarone resistance conferring mutations in Plasmodium falciparum cytochrome b gene (cytb). Mol. Cell. Probes 17, 85–89 (2003).
Acknowledgements
The authors apologize to colleagues whose work could not be cited owing to the broad scope of the Review and space limitation. They thank members of the Haldar laboratory for insightful discussion. Work in the authors' laboratories was supported by the US National Institutes of Health (R01 HL069630 and HL130330) and India Government Department of Science and Technology (ECR/2015/000387) and Department of Biotechnology Ramalingaswami Re-entry Fellowship (BT/HRD/35/02/2006).
Author information
Authors and Affiliations
Contributions
K.H., S.B. and I.S. researched data for the article, made substantial contributions to discussions of the content, wrote the article and reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
DATABASES
Supplementary information
Supplementary information S1 (table)
Country/area and Antimalarial Drug Therapy used (WHO, 2016) (DOC 47 kb)
Glossary
- Sporozoites
-
A malaria parasite stage that is injected by the mosquito and that infects liver cells.
- Merozoites
-
A malaria parasite stage that infects red blood cells (also known as erythrocytes).
- Endoperoxide
-
A peroxide group (O–O) that bridges two atoms of a larger molecule and whose cleavage gives rise to reactive free radicals that can oxidize and aggregate proteins (as well as DNA and lipids).
- Proteopathy
-
A disease state where proteins become structurally abnormal and disrupt cellular function.
- Proteostasis
-
A network process or system that integrates translation, signalling pathways, molecular chaperones and protein degradation to enable cells to control the abundance and folding of the proteome.
- Parasitaemia
-
The number of infected red cells per total number of red cells.
- Autophagosome
-
A double-membraned vesicle containing cellular material slated to be degraded by autophagy.
- Macroautophagy
-
A process by which a membrane or phagophore forms near cargo and then expands until it encloses the cargo, which is subsequently degraded by autophagy. Macroautophagy depends on phosphatidylinositol 3-kinase catalytic subunit type 3 (PIK3C3) and its lipid product phosphatidylinositol-3-phosphate (PtdIns3P).
- Apicoplast
-
An organelle that is a remnant of a non-photosynthetic plastid found in many apicomplexan parasites, including Plasmodium falciparum.
- Haemoglobinopathies
-
Single-gene disorders that result in abnormal structure of the haemoglobin molecule.
Rights and permissions
About this article
Cite this article
Haldar, K., Bhattacharjee, S. & Safeukui, I. Drug resistance in Plasmodium. Nat Rev Microbiol 16, 156–170 (2018). https://doi.org/10.1038/nrmicro.2017.161
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrmicro.2017.161
This article is cited by
-
Chemoproteomics-based profiling reveals potential antimalarial mechanism of Celastrol by disrupting spermidine and protein synthesis
Cell Communication and Signaling (2024)
-
Emergence, transmission dynamics and mechanisms of artemisinin partial resistance in malaria parasites in Africa
Nature Reviews Microbiology (2024)
-
Flexible and cost-effective genomic surveillance of P. falciparum malaria with targeted nanopore sequencing
Nature Communications (2024)
-
Synthesis, docking and biological evaluation of some novel [1,2,4] triazolo [5,1-b] quinazoline Schiff base derivatives
Journal of the Iranian Chemical Society (2024)
-
A nanoparticle vaccine displaying the ookinete PSOP25 antigen elicits transmission-blocking antibody response against Plasmodium berghei
Parasites & Vectors (2023)