Abstract
Dengue virus (DENV) is a human pathogen with a large impact on public health. Although no vaccine against DENV is currently licensed, a recombinant vaccine — chimeric yellow fever virus–DENV tetravalent dengue vaccine (CYD-TDV) — has shown efficacy against symptomatic dengue disease in two recent Phase III clinical trials. Safety observations were also recently reported for these trials. In this Opinion article, we review the data from recent vaccine clinical trials and discuss the putative mechanisms behind the observed efficacy of the vaccine against different forms of the disease, focusing on the interactions between the infecting virus, pre-existing host immunity and vaccine-induced immune responses.
Similar content being viewed by others
Main
Dengue, a mosquito-borne disease caused by one of four dengue virus serotypes (DENV-1, DENV-2, DENV-3 and DENV-4) of the genus Flavivirus, is a growing public health problem1. Although infection is mostly asymptomatic2, it can cause 'classic' dengue fever, which often presents as a flu-like syndrome. Furthermore, classic dengue fever may evolve towards severe disease in 1–3% of cases3,4. As detailed below, the development of severe dengue is multifactorial and thought to result from an immunopathological reaction involving both innate immune responses (particularly when severe disease occurs as a result of primary infection) and adaptive immune responses (particularly when severe disease occurs as a result of secondary infection).
Currently, there is no vaccine licensed to prevent dengue, and as a result, the WHO considers the development of an effective dengue vaccine to be a high priority5. Several vaccine candidates are being developed: live-attenuated vaccines, including live chimaeras based on attenuated DENV or yellow fever virus backbones; recombinant vector vaccines, such as those using adenoviruses; DNA vaccines; inactivated vaccines or subunit proteins, used in combination with adjuvants; and combinations of several of these technologies6,7,8,9,10. The most advanced candidate in clinical development is a recombinant tetravalent dengue vaccine (TDV), often referred to as the chimeric yellow fever virus–DENV (CYD) vaccine or CYD-TDV (for a review, see Ref. 11). CYD-TDV is a live-attenuated vaccine composed of four CYD vaccine viruses that each express the structural genes — encoding the membrane protein (prM) and envelope protein (E) — of one of the four DENV serotypes. These structural genes are expressed using a yellow fever virus strain 17D (YFV17D) genetic backbone, which is a well-characterized live-attenuated flavivirus vaccine for which immunogenicity and safety have been documented for several decades10. This strategy results in the generation of vaccine viruses that collectively express the structural antigens of the four DENV serotypes, and these antigens act as the targets of the host immune response involving innate immune cells, neutralizing antibodies and T cell responses.
CYD-TDV has progressed to Phase III efficacy trials, and two pivotal studies are ongoing, one in children 2–14 years of age in Asia12 and the other in children 9–16 years of age in Latin America13 (Box 1). The active phase of these two trials (the 25 months following the initial vaccination) has now been completed, and both trials reached their primary endpoint by demonstrating vaccine efficacy against virologically confirmed dengue (VCD), when overall efficacy was measured (that is, irrespective of disease severity and infecting DENV serotype) (Box 1). An acceptable safety profile, consistent with prior trials, was also demonstrated in both trials during the active surveillance period. All four serotypes contributed to the overall efficacy in both studies, and both trials also showed greater efficacy against severe disease and against disease leading to hospitalization, in comparison with the overall efficacy (Box 1). Newly published longer-term safety data have now been obtained for the first year of follow-up during the surveillance phase for the safety of participants requiring hospitalization (referred to as the hospital phase, in which the semi-passive surveillance of hospitalized individuals is carried out; Box 2), and these data provide information about the overall benefit–risk profile of CYD-TDV. Briefly, in this first year of long-term follow-up (LTFU), the benefit of vaccination was confirmed in individuals 9 years of age or older, whereas a higher incidence of hospitalization as a result of dengue fever was observed in the Asian trial for individuals younger than 9 years of age (discussed below).
Although all serotypes contributed to the overall efficacy, vaccine efficacy varied by serotype, as observed in a previous Phase IIb trial in Thailand14. Furthermore, prior exposure to wild-type DENV infection — which was defined through the measurement of DENV-neutralizing antibodies using the gold-standard DENV plaque reduction neutralization test (PRNT)11,12 — was identified as an important covariate for efficacy in both clinical trials. Vaccine efficacy was greater in participants who had previously been exposed to DENV (referred to as seropositive individuals) than in participants who had never been exposed to DENV (referred to as seronegative individuals). Efficacy also increased with participant age in the Asian trial, suggesting that age can be a covariate. However, it is not clear at the mechanistic level how age affects vaccine efficacy, and these observations could be linked to several factors, including host physiology (for example, maturity of the microvascular system or immune status15,16) or the accumulated exposure to DENV12.
In this Opinion article, we discuss the mechanisms behind the observed efficacy profile of CYD-TDV in the two most recent clinical trials. We focus on the interactions between the vaccine, the infecting virus and host immunity, and we consider how these interactions may affect short-term and long-term efficacy, and safety against the different disease forms of dengue. We also discuss how pre-immunity to DENV and serotype distribution affect vaccine efficacy and why superior protection is observed in seropositive individuals. Finally, we explore the benefit–risk profile of CYD-TDV and its potential public health impact as a result of the reduction of dengue disease.
Immunity to infection and vaccination
To understand the crucial interactions between the vaccine, the challenge virus and host immunity, the nature of the immunity induced by wild-type infection and how this compares with the immune responses elicited by CYD-TDV need to be considered. Subsequently, the differences in immunity induced by the dengue vaccine in seronegative versus seropositive individuals must be understood. Finally, it is necessary to appreciate how responses to a DENV vaccine affect the clinical outcome of DENV infection.
Immune responses to wild-type DENV infection. Primary infection with DENV (that is, an infection caused by a specific DENV serotype in a naive individual) induces potent innate immune responses, which in turn shape the adaptive immune responses, including humoral responses (that is, antibody production by B cells) and cellular responses (that is, those mediated by CD4+ T cells and CD8+ T cells). Furthermore, humoral and cellular immune responses against DENV can be either serotype-specific or cross-reactive (that is, directed against multiple DENV serotypes).
The innate immune system represents the first line of defence against DENV, and infection triggers the expression of a wide array of pro-inflammatory (and also anti-inflammatory) cytokines and chemokines. Notably, the levels and kinetics of these cytokines and chemokines shape the outcome of the disease. As this article focuses on vaccine-induced protection, innate immunity is not discussed in detail here (for reviews on innate immune responses to DENV infection, see Refs 17,18).
The DENV genome encodes three structural antigens — capsid protein (C), prM and E — and seven non-structural antigens (NS1, NS2a, NS2b, NS3, NS4a, NS4b and NS5). Antibody responses to DENV infection mainly target the structural antigens present on the surface of virions (prM and E) and the secreted glycosylated NS1 antigen. By contrast, cellular responses primarily target non-structural antigens expressed in infected cells during viral replication, particularly NS3 (Refs 19,20). Notably, immunity induced by the primary infection is believed to induce life-long protection against the infecting serotype (homotypic protection), whereas the cross-protection afforded against other serotypes (heterotypic protection) lasts, on average, several months to 3 years21,22,23,24,25,26,27. However, beyond this 'grace' period of waning cross-protection, there is an increasing risk that severe disease will result from a secondary heterologous infection (that is, infection by a different DENV serotype to that which caused the primary infection). For example, a meta-analysis estimated that an individual is approximately 24 times as likely to suffer from severe disease caused by a secondary heterologous infection than that caused by a primary infection (although severe secondary heterologous infections still represent a very low percentage of overall dengue cases)28. This increased disease risk on secondary infection has been hypothesized to be linked, in particular, to non-neutralizing enhancing antibodies that facilitate virus uptake through Fcγ receptors — a mechanism known as antibody-dependent enhancement (ADE) — or to a detrimental inflammatory or biased T cell response. ADE may also contribute to biased cytokine responses through an 'intrinsic ADE' mechanism, enhancing immunosuppressive interleukin-10 (IL-10) expression and counteracting antiviral responses (for reviews, see Refs 18,19).
During a secondary heterologous infection, memory B cell responses preferentially recall serotype-specific antibody responses against the serotype responsible for the primary infection. Secondary infection also boosts and further induces the production of cross-reactive antibodies29,30,31,32,33,34,35,36. This results in more efficient cross-protection against subsequent (that is, tertiary or quaternary) infections, which are then less likely to be severe, regardless of the infecting serotype25,37.
The protective role of broadly cross-reactive antibodies is further demonstrated by the observation that a pre-existing multitypic antibody- neutralization pattern (that is, targeting multiple serotypes) has been associated with a more favourable outcome than a pre-existing monotypic antibody- neutralization pattern23,25,38,39. Furthermore, children with pre-existing cross-neutralizing antibody responses were less likely to develop dengue fever than children with pre-existing monospecific neutralizing responses.
In addition to antibody production by B cells, T cells seem to have a protective role in both animal models and humans, depending on their level and profile40,41,42,43. Although this article focuses mostly on the role of antibodies and B cells during vaccination, the role of T cells is also discussed (for a review on the role of T cells during DENV infection, see Ref. 19).
Taken together, studies of the immune response to DENV infection suggest that a protective vaccine should preferably induce a B cell response comparable in level and quality to that induced by a secondary DENV infection, as such a response would result in more efficient cross-protection against subsequent infections with all DENV serotypes. This optimal response should include neutralizing antibodies against different serotypes, and both specific and cross-reactive neutralizing antibodies should be produced at high-enough levels and affinities to be effective. Furthermore, an optimal vaccine should induce the production of moderate levels of pro- inflammatory cytokines, type I interferons (IFNs) and other chemokines and cytokines that link the innate and adaptive immune responses. Similarly, at the T cell level, a vaccine should induce serotype-specific CD4+ T cell and/or CD8+ T cell responses directed against both structural and non-structural antigens, with no overt inflammatory profile. The amount and kinetics of the different immune mediators should also be considered; too much of a good thing is not necessarily beneficial, and some 'detrimental' factors involved in innate or T cell responses may play a positive part during disease onset or may be necessary to terminate inflammatory reactions19.
CYD-TDV-induced immune responses in seronegative individuals. Initial clinical studies have shown that the administration of three doses of CYD-TDV to seronegative volunteers induces the production of neutralizing antibodies (seroconversion) against all four DENV serotypes, as measured by PRNT, which is considered more as a quantitative than a qualitative assay. Recent investigations exploring qualitative aspects of the vaccine response suggest that the three-dose regimen induces predominantly homotypic responses dominated by specific antibodies against one or a few serotypes (usually DENV-4), whereas responses against the other serotypes are largely due to cross-reactive antibodies. These observations are consistent with previous immunogenicity trials44 and with the fact that the proportion of volunteers experiencing viraemia after the first dose is higher for CYD-4 viraemia than for viraemia with other CYD serotypes45,46. Homotypic responses against some of the other serotypes are also observed, although these responses are variable across individuals47.
The three doses of CYD-TDV also induce serotype-specific CD4+ T cell and/or CD8+ T cell responses directed against structural antigens from all four DENV serotypes. On viral stimulation, these T cells express pro-inflammatory cytokines, such as IFNγ and tumour necrosis factor (TNF) (IFNγ is produced at higher levels than TNF), and can thus be classified as T helper 1 cells (TH1 cells) and T cytotoxic 1 cells (TC1 cells), for CD4+ T cells and CD8+ T cells, respectively. Furthermore, the serotype specificity of these T cell responses has been confirmed after bivalent CYD vaccination (that is, using formulations containing only two CYD serotypes)47,48,49. In addition to T cell responses against DENV structural antigens, CYD-TDV leads to the generation of TC1 cell responses directed against the YFV17D NS3 antigen47,48,49. The generation of these T cell responses, whatever their specificity, may be triggered by CYD-TDV-mediated activation of human monocyte-derived dendritic cells (DCs), which results in the production of type 1 IFNs and moderate levels of inflammatory cytokines and chemokines that link innate and adaptive immunity50,51.
Overall, the three-dose vaccination strategy in seronegative volunteers maximizes the immune response and may partially mimic an attenuated and subclinical primary infection (Fig. 1a). It should be noted that CYD-TDV vaccination has different features to a true primary infection, given the presence of YFV17D NS antigens and the tetravalent nature of the vaccine, so the mimicry of a primary infection could only be partial.
a | Chimeric yellow fever–dengue virus (DENV) tetravalent dengue vaccine (CYD-TDV) responses in seronegative individuals. Vaccination of seronegative individuals with CYD-TDV (which includes CYD-1, CYD-2, CYD-3 and CYD-4) induces the production of neutralizing antibodies against all four DENV serotypes. This response is dominated by specific antibodies against one or a few serotypes, whereas responses against the other serotypes are largely due to cross-reactive antibodies. Vaccination in this population also induces serotype-specific and cross-reactive T cell responses against DENV structural antigens. Therefore, vaccination of seronegative individuals may represent a subclinical attenuated 'primary-like' infection. The consequences of vaccination in these individuals at the immunological level vary according to the serotype (that is, the induction of serotype-specific neutralizing responses). This will result in limited cross-protection in seronegative individuals compared with cross-protection elicited by vaccination in seropositive individuals. Nevertheless, subsequent infection with DENV (true primary infection) may act as a 'secondary-like' infection, boosting the vaccine-induced response resulting in a better and longer cross-protection against subsequent infection or infections. b | CYD-TDV responses in seropositive individuals. Wild-type DENV infection induces DENV-specific antibodies against the infecting serotype, but also induces cross-reactive neutralizing antibodies, which will contribute to short-term cross-protection. Wild-type infection also induces serotype-specific and cross-reactive T cells. On subsequent infection with a heterologous DENV serotype, there will be a boost to the DENV-specific responses against the serotype responsible for primary infection, and also to the cross-reactive responses. Furthermore, heterologous infection will result in the limited induction of anti-DENV-specific responses directed against the serotype responsible for secondary infection. Such a boost will result in more efficacious subsequent cross-protection. Therefore, CYD-TDV vaccination of seropositive individuals may represent an attenuated heterotypic secondary-like infection, resulting in better and longer cross-protection than that induced by vaccination of seronegative individuals. Furthermore, vaccination of seropositive individuals enables the boosting of T cell responses against DENV nonstructural antigens.
CYD-TDV-induced immune responses in seropositive individuals. The higher PRNT responses observed on a three-dose regimen in seropositive individuals12,13,52,53, and in animal models54, suggest that vaccination boosts pre-vaccine immunity by inducing a recall response in the existing memory B cells and T cells (which were generated during the primary DENV infection). At the qualitative level, recent preliminary findings suggest that this response is both specific to the first infecting DENV serotype and cross-reactive against all four serotypes46. Additional responses to serotypes other than that responsible for the primary infection are also induced to some extent; this is possibly due to bystander help from recalled memory T cell responses, both cross-reactive and specific for the first infecting serotype, and/or the fact that pre-existing cross-reactive memory B cells can act as potent antigen-presenting cells (APCs) that participate in the generation of B cell responses against all four DENV serotypes present in CYD-TDV.
Importantly, a broader T cell response has also been detected in seropositive individuals, including a boost of the T cell responses directed against DENV NS3 (Ref. 49). As seen in seronegative individuals, the vaccine induces a cellular response with a TH1 and TC1 cell profile.
Overall, the administration of three CYD-TDV doses in seropositive individuals mimics an attenuated and subclinical secondary infection with a heterotypic DENV serotype (Fig. 1b).
Pre-immunity and vaccine efficacy
CYD-TDV vaccination in seropositive individuals results in a boost in both the level and quality of the immune response, and this boost is similar to that observed following a secondary wild-type infection. The boost probably contributes to the increased protection from infection observed in these patients, compared with seronegative volunteers, during the active phase of the two Phase III clinical trials11,12 (Fig. 1).
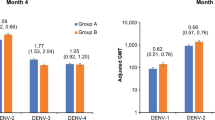
At the quantitative level, logistic regression analyses of the relationship between the PRNT response for each serotype and protection suggest that higher antibody titres are associated with a lower probability of disease55. However, a different level of protection may be required for different serotypes. For example, a cluster study suggested that the threshold required to protect against DENV-2 is higher than that required to protect against DENV-1 or DENV-4 (Ref. 56). This could partially explain the lower level of efficacy of CYD-TDV against DENV-2 than against the other serotypes12,13,14.
Compared with vaccination of seropositive individuals, vaccination of seronegative individuals results in the production of lower levels of antibodies57, which could explain the lower efficacy of CYD-TDV against primary infection in naive individuals12,13. Indeed, both Phase III trials showed a lower vaccine efficacy in seronegative subjects during the active phase12,13 but, as discussed below, this needs to be further addressed through long-term surveillance studies58.
Importantly, vaccination in young seronegative individuals may temporarily increase the frequency of a subsequent symptomatic or severe infection (see below) (Boxes 1,2). Nevertheless, vaccination in seronegative individuals will probably boost vaccine-induced immunity in the longer term by expanding the population and number of memory serotype-specific and cross-reactive B cells and T cells, irrespective of the clinical picture. In this case, a primary infection of a vaccinated seronegative individual might act similarly to a secondary infection in unvaccinated individuals, therefore improving protection against subsequent infections (Fig. 1a). In support of this hypothesis, neutralizing antibody responses against wild-type DENV infection are stronger in vaccinated monkeys than in naive monkeys (although it is important to note that this species is not a model for dengue disease)59,60. In addition, unpublished ongoing statistical analyses of the active phase of the two Phase III efficacy trials indicate that seronegative individuals who received CYD-TDV mount a greater response after primary wild-type infection and more frequently develop a multitypic response than seronegative controls (B.G. and N.J., unpublished observations); such multitypic responses are usually considered more favourable in the case of sequential wild-type infections22,24,37,38. Preliminary statistical analyses in the Asian trial also show that more controls than vaccinated individuals had two consecutive infections during the active phase.
Overall, although the immunity induced by CYD-TDV in seronegative individuals may not result in optimal protection against a symptomatic primary infection, and in younger age groups the frequency of symptomatic primary infections may even be higher in vaccinated individuals than in controls (Boxes 1,2), the vaccine could still provide superior protection against subsequent infections. Boosting of vaccine-elicited responses by a primary infection may then improve the benefit–risk profile in this subpopulation (Fig. 1a).
Protection against severe disease
Many aspects of dengue pathology have not been fully elucidated19. In particular, the direct cause of plasma leakage, a central event in severe dengue cases, remains unclear. Severe disease has been suggested to be multifactorial and to be mediated by an immunopathological mechanism that starts early after infection and involves multiple aspects of the immune system, including innate and adaptive immune cells19. For example, inadequate, low-affinity responses to the infecting serotype may drive the immune response towards an inflammatory profile, with the release of inflammatory cytokines and chemokines, such as TNF and IL-8, which can lead to impaired endothelial permeability and plasma leakage. Similarly, a TH2 cell-biased or even immunosuppressive response involving the production of IL-10 may impair the development of a beneficial TH1- or TC1-type response19. Therefore, to prevent severe disease, vaccination must elicit an immune response that, when activated by an infection, would not be harmful.
In the Phase III efficacy trials, efficacy rates for CYD-TDV during the active phase were high against severe disease and hospitalization (Box 1). Also, during the active phase of the Asian trial, when all dengue cases were considered, plasma leakage with clinical signs and thrombocytopaenia were significantly less severe in vaccinated individuals than in controls11. These data suggest that in vaccinated individuals, infection during the 25-month follow-up period may rapidly recall or induce an adequate response involving multiple components of the immune system, preventing the development of severe disease.
Different explanations could account for the observed superior protection against severe disease compared with protection against infection or mild but symptomatic disease in the active phase. Protection against infection or mild but symptomatic disease requires antibodies that inhibit viral replication or that lower viraemia and viral dissemination. Therefore, by enabling a faster recall response by B cells, CYD-TDV could cause a more rapid production of antibodies, resulting in protection against severe disease (Fig. 2).
Individuals who are vaccinated with the chimeric yellow fever–dengue virus (DENV) tetravalent dengue vaccine (CYD-TDV) could respond differently to infection with wild-type DENV. For example, pre-existing neutralizing antibodies and T cell responses, which are induced at different levels and qualities by vaccination of seronegative versus seropositive individuals, can block viral entry and replication, or at least keep viral replication below a 'clinical' threshold, resulting in protection against DENV infection or dengue disease. Alternatively, pre-existing immunity may not be potent enough to prevent a symptomatic outcome. In this case, antibodies, if they are not cross-protective, may enhance antibody-dependent infection (through viral uptake mediated by Fcγ receptors (FcγR)) and may thus increase the frequency of severe disease or hospitalization. This is called the antibody-dependent enhancement (ADE) hypothesis. By contrast, infection can rapidly recall or trigger additional B cell and T cell responses, which can also modulate innate responses and effectors. For example, B cells may produce protective antibodies; CD4+ T cells, in addition to providing B cell and CD8+ T cell help, may produce T helper 1 cell (TH1 cell)-associated cytokines; and CD8+ type 1 cytotoxic T cells (TC1 cells) may kill infected cells. Collectively, these multiple players may act in a synergistic way to prevent progression towards severe disease and hospitalization.
Vaccination may also preferentially protect seropositive individuals, who may be at higher risk than naive individuals of developing severe disease on secondary infection. In this regard, the vaccine mimics an attenuated asymptomatic secondary infection, so subsequent infections would correspond to tertiary or quaternary exposures, which are less likely to be severe37. Conversely, according to the ADE hypothesis, non-neutralizing or waning antibodies, if they are not cross-protective, may enhance infection61; this could increase the frequency of severe disease in some age groups (see below) (Fig. 2).
The vaccine could also protect from severe disease owing to the generation of protective T cell responses. In fact, an infection with sufficient dissemination and viraemia to cause symptomatic disease may trigger a rapid recall of several memory mechanisms, including both B cell and T cell responses to structural and non-structural antigens from all serotypes. T cells could act as a second line of defence through cytotoxic activity or by rapidly triggering innate mechanisms through the release of cytokines. These cytokines can activate innate immune cells and other immune effector cells, such as tissue-resident memory cells62, which may also contribute to protection in dengue, as has been recently proposed63. Therefore, the rapid induction or recall of multitypic T cell responses could further contribute to protection against severe disease (Fig. 2).
In agreement with a protective role for T cells following vaccination, both CD4+ T cells and CD8+ T cells seem to have a protective role in animal models and humans40,41,42,43. In animal models, even CD8+ T cell responses restricted to the envelope help protect against lethal DENV infection and prevent the potentially harmful effect of antibodies42. CD8+ T cells can also mediate short-term cross-protection64. Therefore, following vaccination, the development of severe disease on infection may be prevented by the recall stimulation of both B cell and T cell effector mechanisms (including neutralizing antibodies, TH-type responses and TC cell-mediated killing of infected cells), as well as by the induction of TH1 cell-associated cytokines (Fig. 2). For example, this is known to occur on infection with the measles virus (a member of the Paramyxoviridae family), when CD8+ T cells facilitate clearance of the virus even though they do not prevent infection65.
The superior protection observed during the active phase against severe disease in individuals vaccinated with CYD-TDV may also be linked to a narrower case definition that requires the identification of additional clinical parameters, as seen, for instance, in the case of acellular pertussis vaccine or as modelled for Lyme disease66,67.
The hospital phase
The clinical development programme for CYD-TDV includes a 4-year LTFU phase to assess safety, in line with the WHO guidelines (that is, 5 years after completion of the vaccination schedule)68 (Box 2). Taking into consideration the relative risk of hospitalization during the hospital phase (including for severe dengue), the cumulative dengue cases across the active and hospital phases, and the pooled efficacy data for the two Phase III trials, the ongoing LTFU phase indicates that CYD-TDV vaccination results in a favourable clinical profile with a high efficacy for preventing VCD and has an acceptable post-vaccination safety profile for individuals 9 years of age or older. Although the clinical profile of disease is the same in the active phase and thehospital phase, the first year of the LTFU hospital phase in the Asian trial recorded an imbalance in the number of individuals who were younger than 9 years of age and were hospitalized because of dengue or had severe dengue disease. This finding requires further follow-up and investigation. Several non-mutually exclusive hypotheses have been proposed to explain such observations (see below). Notably, on-site investigations have shown that major forms of bias (for example, unblinding) are unlikely to explain the imbalance, and a chance event is also unlikely (although it is still difficult to explain the lower-than-expected level of individuals with severe dengue or who were hospitalized in the placebo group, despite it being a 'quiet' epidemiological period across most of Asia for the period of LTFU reported).
Hypothesis 1: waning protection leads to reduced efficacy, particularly in seronegative individuals. The LTFU study was designed to assess vaccine safety. However, comparing the counts of individuals requiring hospitalization for dengue in the active phase versus the hospital phase, one can postulate that the protective effect of the vaccine against hospitalization may have declined by the hospital phase in individuals younger than 9 years of age. Humoral immunity is likely to wane more rapidly in seronegative than in seropositive vaccinated individuals, as the recall response in seropositive vaccinated individuals gives rise to a stronger immune response than is seen in their seronegative counterparts (Fig. 1). Given that younger age groups have a higher chance of being seronegative than older age groups (as the likelihood of being exposed to a primary infection increases with age), waning immunity is more probable in the youngest vaccinated individuals. Consequently, their neutralizing responses are more likely to rapidly fall below protective thresholds for all four DENV serotypes and to present a monotypic pattern that is less likely to be cross-protective25,38,39.
Hypothesis 2: younger vaccinated individuals are more susceptible to severe infection. Age-related differences in vaccine efficacy may also be explained by differences in physiology that influence susceptibility to severe infection. For example, age differences at the microvascular and vascular levels could be associated with higher chances of plasma leakage, which is thought to contribute to severe disease15. In addition, younger children could be less able to recover from dengue-induced disorders, increasing their chances of requiring hospitalization. Furthermore, some qualitative differences at the immunological level were seen between children 5–10 years of age and those who were older16. These differences may affect innate immune responses, the diversity of the repertoire of B cells and T cells that are mobilized or the affinity of B cell clones, thus influencing the duration and quality of the CYD-TDV-induced specific responses in younger children versus older children. In agreement with there being an independent age effect, pooled efficacy analyses showed a significant vaccine efficacy in seronegative individuals 9 years of age or older, whereas the vaccine was not significantly effective in younger seronegative individuals68.
The risk of developing severe disease is higher for individuals with a secondary heterotypic infection than for those with a primary infection28. This may be mimicked by CYD-TDV vaccination of seronegative individuals, whereby vaccination represents a 'primary-like' infection dominated by one or a few serotypes, and diminishing responses lead to only short-term cross-protection. As cross-protection wanes (potentially rapidly, owing to low antibody titres), so vaccine efficacy is reduced, as discussed above. Furthermore, vaccinated individuals could be at greater risk of developing a severe or symptomatic 'secondary-like' infection the first time they contract DENV: the vaccine could act as their primary infection, and the subsequent true primary wild-type DENV infection (which would otherwise be typically less severe) could simulate a secondary wild-type infection (which is typically more severe).This situation is also more likely to occur in younger vaccinated individuals.
If this hypothesis is correct, an associated question is whether a vaccination mimicking a primary infection would induce an equivalent risk, a lower risk or a higher risk of developing a severe secondary-like infection than the risk induced by a real primary infection with wild-type DENV. Although it seems unlikely that a higher risk would be afforded by vaccination, only expanded surveillance of the ongoing LTFU studies will enable this point to be addressed, through the comparison of well-defined populations (that is, seronegative vaccinated individuals developing a primary wild-type infection versus seropositive placebo recipients developing a secondary infection). In this regard, it should be noted that for individuals who were hospitalized because of dengue, the clinical picture and viraemia were no different between vaccinated individuals and placebo recipients in both active and hospital phases, and the overall immune profiles in more than 200 sera collected from both groups were also comparable (Ref. 68 and B.G. and N.J., unpublished observations).
Hypothesis 3: susceptibility in vaccinated individuals is temporally clustered. The fact that vaccination of seronegative individuals may represent an attenuated subclinical primary infection means that in the efficacy trials, such a primary infection has been temporally clustered in vaccinated individuals. This clustering occurred in a short period of time because of the condensed enrolment periods of the trials, whereas subjects who received the placebo are exposed to a primary wild-type infection over a longer period of time. Therefore, differences in seasonality and endemicity may mean that the primary infection and the subsequent secondary exposure to a heterologous serotype (with a potentially more severe outcome) are more spread out in time for control subjects than for vaccinated individuals. As a consequence, during a given period of time, one would observe more dengue-related hospitalizations for vaccinated individuals than for controls; however, this imbalance may be only temporary, occurring during a limited period of time, after which more severe cases would be accrued in placebo recipients (Fig. 3). Such a temporary imbalance is suggested by data from the LTFU of the Phase IIb study, in which the first year of the hospital phase has shown a neutral estimate of vaccinated individuals being hospitalized owing to dengue, whereas the tendency was reversed in the subsequent year. A permanent predisposition to sensitization in seronegative vaccinated individuals is not compatible with the postulation behind this clustering hypothesis, and in particular such sensitization would no longer be present after a secondary-like infection has developed, in agreement with observations in the field showing a lower risk of developing severe disease on tertiary and quaternary infections25,37.
Immunological priming is clustered in vaccinated individuals, but not in placebo recipients. In seronegative individuals, vaccination with chimeric yellow fever–dengue virus (DENV) tetravalent dengue vaccine (CYD-TDV) may represent an attenuated subclinical 'primary-like' infection, which means that in the efficacy trials, this initial infection has been temporally clustered in all vaccinated individuals (including those belonging to the younger age groups). Vaccination induces short-term cross-protection, but results in the clustering of the 'secondary-like' infection (which is the primary infection with wild-type DENV); this infection is potentially more severe and occurs earlier in vaccinated individuals than in those who received the placebo. In individuals given a placebo, the primary infection (with wild-type DENV) is non-clustered (can occur over a much longer time period), which potentially results in longer cross-protection seen across the group as a whole. The secondary infection (with wild-type DENV), which potentially results in more severe disease and hospitalization, will also be non-clustered. Therefore, a consequence of the cluster hypothesis is that the imbalance observed between individuals given the vaccine and those given a placebo may be only temporary, occurring during a limited period of time, after which more severe cases would be accrued in placebo recipients ('catch-up' events). Therefore, vaccine efficacy may evolve with time. This 'instantaneous' vaccine efficacy may be temporarily negative after a few years post-vaccination, although later 'catch-up' events in placebo recipients may lower or even suppress the differences observed at the earlier time points between vaccinated and non-vaccinated individuals. The combination of the 'catch-up' events in placebo recipients and the booster effect afforded by natural infection in vaccinated individuals would then result, after some time, in an increased (or at least neutral) vaccine efficacy in vaccinated versus non-vaccinated individuals. This increase in efficacy is dependent on epidemiological factors and the age at which children were vaccinated, and could take months to years.
Explaining LTFU observations. In conclusion, one can propose interconnected hypotheses to explain the LTFU safety observations. Predominantly, temporally clustered vaccination, especially in seronegative individuals, may result in a smaller cross-reactive immune response, which is prone to rapid waning in a condensed period of time. This situation is more likely to occur in children less than 9 years of age, given their lower chance of seropositivity before vaccination. A subsequent primary wild-type infection (typically less likely to be severe in children) then occurs in an immunological setting created by vaccination, resulting in this primary infection resembling a secondary infection (typically more likely to be severe). This situation may occur in particular in the youngest children, who have a less-developed vascular physiology and partially immature immune responses, which results in younger vaccinated individuals being hospitalized more frequently than their control counterparts for a certain period. However, this imbalance is potentially only temporary.
Outlook
Results of Phase III efficacy trials conducted in Asia and Latin America have demonstrated that the CYD-TDV vaccine is efficacious against all four DENV serotypes during the active phase and has an acceptable safety profile. However, DENV serotype distribution throughout the population and an individual's DENV serostatus before vaccination seem to affect vaccine efficacy. Furthermore, prior exposure to DENV is hypothesized to have an important role in the longer-term (hospital phase) safety observations. Therefore, additional studies are required to determine the long-term effect of differences in protection according to baseline serological status, and to elucidate the underlying immunological mechanisms associated with the enhanced protection observed in seropositive individuals. Finally, important additional points have to be considered regarding vaccine efficacy, such as the level of response required to protect against each serotype55,56, the role of circulating genotypes and their interplay with pre-immunity69, genetic factors70,71 and the potential role of indirect protection afforded by vaccination.
In children younger than 9 years of age, who are more likely to be seronegative, vaccination may present immunological similarities to an attenuated subclinical primary infection; this potentially increases the chances of their developing symptomatic dengue disease on subsequent wild-type infection. This may explain the current imbalance observed in the younger vaccinated individuals, which may be only temporary; additional data are required to address this point. Although the immunity induced by CYD-TDV in seronegative individuals may not result in optimal protection against a primary wild-type infection, CYD-TDV does offer significant efficacy in seronegative individuals older than 9 years of age, on the basis of pooled efficacy analyses. Furthermore, the vaccine may provide a benefit during subsequent challenges, owing to the fact that the primary infection boosts vaccine-elicited memory responses.
Overall, although additional data are needed to determine the effect of vaccinating children younger than 9 years of age, these results and hypotheses support a positive benefit–risk profile for vaccinating individuals older than 9 years of age, with recorded high vaccine efficacy for all endpoints during the active surveillance period and a lower risk of hospitalization for VCD during the first years of the LTFU period. Furthermore, the predefined risk management plan for the vaccine is designed to confirm its safety profile and evaluate its effectiveness in a real-world use setting, following its implementation in countries with different epidemiological backgrounds. Importantly, successful vaccination of children older than 9 years of age has the potential to significantly reduce the dengue burden in endemic countries and may contribute to achieving the WHO objectives of reducing dengue-induced mortality by 50% and morbidity by 25% by 2020.
References
Bhatt, S. et al. The global distribution and burden of dengue. Nature 496, 504–507 (2013).
Grange, L. et al. Epidemiological risk factors associated with high global frequency of inapparent dengue virus infections. Front. Immunol. 5, 280 (2014).
Malavige, G. N., Fernando, S., Fernando, D. J. & Seneviratne, S. L. Dengue viral infections Postgrad. Med. J. 80, 588–601 (2004).
World Health Organization. Dengue guidelines for diagnosis, treatment, prevention and control (WHO, 2009).
World Health Organization. Dengue. WHO [online], (2014).
Osorio, J. E., Huang, C. Y., Kinney, R. M. & Stinchcomb, D. T. Development of DENVax: a chimeric dengue-2 PDK-53-based tetravalent vaccine for protection against dengue fever. Vaccine 29, 7251–7260. (2011)
Durbin, A. P., Kirkpatrick, B. D., Pierce, K. K., Schmidt, A. C. & Whitehead, S. S. Development and clinical evaluation of multiple investigational monovalent DENV vaccines to identify components for inclusion in a live attenuated tetravalent DENV vaccine. Vaccine 29, 7242–7250 (2011).
Murphy, B. R. & Whitehead, S. S. Immune response to dengue virus and prospects for a vaccine. Annu. Rev. Immunol. 29, 587–619 (2011).
Coller, B. A., Barrett, A. D. & Thomas, S. J. The development of dengue vaccines. Introduction. Vaccine 29, 7219–7220 (2011).
Fernandez, S. et al. An adjuvanted, tetravalent dengue virus purified inactivated vaccine candidate induces long-lasting and protective antibody responses against dengue challenge in rhesus macaques. Am. J. Trop. Med. Hyg. 92, 698–708 (2015).
Guy, B. et al. From research to phase III: preclinical, industrial and clinical development of the Sanofi Pasteur tetravalent dengue vaccine. Vaccine 29, 7229–7241 (2011).
Capeding, M. R. et al. Clinical efficacy and safety of a novel tetravalent dengue vaccine in healthy children in Asia: a phase 3, randomised, observer-masked, placebo-controlled trial. Lancet 384, 1358–1365 (2014).
Villar, L. et al. Efficacy of a tetravalent dengue vaccine in children in Latin America. N. Engl. J. Med. 372, 113–123 (2015).
Sabchareon, A. et al. Protective efficacy of the recombinant, live-attenuated, CYD tetravalent dengue vaccine in Thai schoolchildren: a randomised, controlled phase 2b trial. Lancet 380, 1559–1567 (2012).
Gamble, J. et al. Age-related changes in microvascular permeability: a significant factor in the susceptibility of children to shock? Clin. Sci. (Lond.). 98, 211–216 (2000).
Hanna-Wakim, R. et al. Age-related increase in the frequency of CD4+ T cells that produce interferon-γ in response to staphylococcal enterotoxin B during childhood. J. Infect. Dis. 200, 1921–1927 (2009).
Green, A. M., Beatty, P. R., Hadjilaou, A. & Harris, E. Innate immunity to dengue virus infection and subversion of antiviral responses. J. Mol. Biol. 426, 1148–1160 (2014).
Guzman, M. G. & Harris, E. Dengue. Lancet 385, 453–465 (2015).
Rothman, A. L. Immunity to dengue virus: a tale of original antigenic sin and tropical cytokine storms. Nat. Rev. Immunol. 11, 532–543 (2011).
de Alwis, R. et al. Identification of human neutralizing antibodies that bind to complex epitopes on dengue virions. Proc. Natl Acad. Sci. USA 109, 7439–7444 (2012).
Endy, T. P. et al. Determinants of inapparent and symptomatic dengue infection in a prospective study of primary school children in Kamphaeng Phet, Thailand. PLoS Negl. Trop. Dis. 5, e975 (2011).
Reich, N. G. et al. Interactions between serotypes of dengue highlight epidemiological impact of cross-immunity. J. R. Soc. Interface 10, 20130414 (2013).
Anderson, K. B. et al. A shorter time interval between first and second dengue infections is associated with protection from clinical illness in a school-based cohort in Thailand. J. Infect. Dis. 209, 360–368 (2014).
Montoya, M. et al. Symptomatic versus inapparent outcome in repeat dengue virus infections is influenced by the time interval between infections and study year. PLoS Negl. Trop. Dis. 7, e2357 (2013).
Olkowski, S. et al. Reduced risk of disease during postsecondary dengue virus infections. J. Infect. Dis. 208, 1026–1033 (2013).
Sabin, A. B. Research on dengue during World War II. Am. J. Trop. Med. Hyg. 1, 30–50 (1952).
Snow, G. E., Haaland, B., Ooi, E. E. & Gubler, D. J. Research on dengue during World War II revisited. Am. J. Trop. Med. Hyg. 91, 1203–1217 (2014).
Mizumoto, K., Ejima, K., Yamamoto, T. & Nishiura, H. On the risk of severe dengue during secondary infection: a systematic review coupled with mathematical modeling. J. Vector Borne Dis. 51, 153–164 (2014).
Mathew, A. et al. B-cell responses during primary and secondary dengue virus infections in humans. J. Infect. Dis. 204, 1514–1522 (2011).
Zompi, S., Montoya, M., Pohl, M. O., Balmaseda, A. & Harris, S. Dominant cross-reactive B cell response during secondary acute dengue virus infection in humans. PLoS Negl. Trop. Dis. 6, e1568 (2012).
Tsai, W. Y. et al. High-avidity and potently neutralizing cross-reactive human monoclonal antibodies derived from secondary dengue virus infection. J. Virol. 87, 12562–12575 (2013).
Lai, C. Y. et al. Analysis of cross-reactive antibodies recognizing the fusion loop of envelope protein and correlation with neutralizing antibody titers in Nicaraguan dengue cases. PLoS Negl. Trop. Dis. 7, e2451 (2013).
Smith, S. A. et al. The potent and broadly neutralizing human dengue virus-specific monoclonal antibody 1C19 reveals a unique cross-reactive epitope on the bc loop of domain II of the envelope protein. mBio 4, e00873-13 (2013).
Smith, S. A. et al. Isolation of dengue virus-specific memory B cells with live virus antigen from human subjects following natural infection reveals the presence of diverse novel functional groups of antibody clones. J. Virol. 88, 12233–12241 (2014).
Toh, Y. X. et al. Dengue serotype cross-reactive, anti-e protein antibodies confound specific immune memory for 1 year after infection. Front. Immunol. 5, 388 (2014).
Patel, B., Sapparapu, G., Crowe, J. B., Baric, R. & de Silva, A. M. Characterization of neutralizing antibody responses following natural secondary dengue virus infections. Am. J. Trop. Med. Hyg. 91 (Suppl. 1), abstr. 626 (2014).
Gibbons, R. V. et al. Analysis of repeat hospital admissions for dengue to estimate the frequency of third or fourth dengue infections resulting in admissions and dengue hemorrhagic fever, and serotype sequences. Am. J. Trop. Med. Hyg. 77, 910–913 (2007).
Endy, T. P. et al. Relationship of preexisting dengue virus (DV) neutralizing antibody levels to viremia and severity of disease in a prospective cohort study of DV infection in Thailand. J. Infect. Dis. 189, 990–1000 (2004).
Corbett, K. S. et al. Preexisting neutralizing antibody responses distinguish clinically inapparent and apparent dengue virus infections in a Sri Lankan pediatric cohort. J. Infect. Dis. 211, 590–599 (2015).
Zompi, S., Santich, B. H., Beatty, P. R. & Harris, E. Protection from secondary dengue virus infection in a mouse model reveals the role of serotype cross-reactive B and T cells. J. Immunol. 188, 404–416 (2012).
Zellweger, R. M. et al. Role of humoral versus cellular responses induced by a protective dengue vaccine candidate. PLoS Pathog. 9, e1003723 (2013).
Zellweger, R. M., Eddy, W. E., Tang, W. W., Miller, R. & Shresta, S. CD8+ T cells prevent antigen-induced antibody-dependent enhancement of dengue disease in mice. J. Immunol. 193, 4117–4124 (2014).
Weiskopf, D. et al. Comprehensive analysis of dengue virus-specific responses supports an HLA-linked protective role for CD8+ T cells. Proc. Natl Acad. Sci. USA 110, 2046–2053 (2013).
Villar, L. A. et al. Safety and immunogenicity of a recombinant tetravalent dengue vaccine in 9–16 year olds: a randomized, controlled, phase II trial in Latin America. Pediatr. Infect. Dis. J. 32, 1102–1109 (2013).
Morrison, D. et al. A novel tetravalent dengue vaccine is well tolerated and immunogenic against all 4 serotypes in flavivirus-naive adults. J. Infect. Dis. 201, 370–377 (2010).
Guy, B. et al. Assessment of the qualitative immune response induced by the CYD tetravalent vaccine in human volunteers. Am. J. Trop. Med. Hyg. 91 (Suppl. 1), abstr. 575 (2014).
Guy, B. et al. Cell-mediated immunity induced by chimeric tetravalent dengue vaccine in naive or flavivirus-primed subjects. Vaccine 26, 5712–5721 (2008).
Harenberg, A. et al. Persistence of Th1/Tc1 responses one year after tetravalent dengue vaccination in adults and adolescents in Singapore. Hum. Vaccin. Immunother. 9, 2317–2325 (2013).
Dayan, G. et al. Assessment of bivalent and tetravalent dengue vaccine formulations in flavivirus-naïve adults in Mexico. Hum. Vaccin. Immunother. 10, 2853–2863 (2014).
Deauvieau, F. et al. Innate immune responses in human dendritic cells upon infection by chimeric Yellow fever Dengue vaccines serotype 1 to 4. Am. J. Trop. Med. Hyg. 76, 144–154 (2007).
Balas, C. et al. Different innate signatures induced in human monocyte-derived dendritic cells by wild-type dengue 3 virus, attenuated but reactogenic dengue 3 vaccine virus, or attenuated nonreactogenic dengue 1–4 vaccine virus strains. J. Infect. Dis. 203, 103–108 (2011).
Capeding, M. R. et al. Live-attenuated, tetravalent dengue vaccine in children, adolescents and adults in a dengue endemic country: randomized controlled phase I trial in the Philippines. Vaccine 29, 3863–3872 (2011).
Qiao, M., Shaw, D., Forrat, R., Wartel-Tram, A. & Lang, J. Priming effect of dengue and yellow fever vaccination on the immunogenicity, infectivity, and safety of a tetravalent dengue vaccine in humans. Am. J. Trop. Med. Hyg. 85, 724–731 (2011).
Guy, B. et al. Evaluation of interferences between dengue vaccine serotypes in a monkey model. Am. J. Trop. Med. Hyg. 80, 302–311 (2009).
Jackson, N. et al. Investigations of the observed efficacy of the CYD tetravalent dengue vaccine in the phase 2b trial in Ratchaburi, Thailand. Am. J. Trop. Med. Hyg. 91 (Suppl. 1), abstr. 576 (2014).
Buddhari, D. et al. Dengue virus neutralizing antibody levels associated with protection from infection in thai cluster studies. PLoS Negl. Trop. Dis. 8, e3230 (2014).
Poo, J. et al. Live-attenuated tetravalent dengue vaccine in dengue-naïve children, adolescents, and adults in Mexico City: randomized controlled phase 1 trial of safety and immunogenicity. Pediatr. Infect. Dis. J. 30, e9–17 (2011).
Thomas, S. J. Preventing dengue – is the possibility now a reality? N. Engl. J. Med. 372, 172–173 (2015).
Barban, V. et al. Protective immunity induced against DENV-2 intravenous challenge in non-human primates immunized with CYD vaccine clinical lots. Am. J. Trop. Med. Hyg. 91, (Suppl. 1), abstr. LB-3233 (2014).
Guirakhoo, F. et al. Safety and efficacy of chimeric yellow fever-dengue virus tetravalent vaccine formulations in nonhuman primates. J. Virol. 78, 4761–4775 (2004).
Guzman, M. G. et al. Dengue: a continuing global threat. Nat. Rev. Microbiol. 12, S7–S16 (2010).
Carbone, F. R. & Gebhardt, T. Immunology. A neighborhood watch upholds local immune protection. Science. 346, 40–41 (2014).
Rivino, L. et al. Virus-specific T lymphocytes home to the skin during natural dengue infection. Sci. Transl. Med. 7, 278ra35 (2015).
Zellweger, R. M. et al. CD8+ T cells can mediate short-term protection against heterotypic dengue virus reinfection in mice. J. Virol. 89, 6494–6505 (2015).
Lin, W. H, Pan, C. H., Adams, R. J., Laube, B. L. & Griffin, D. E. Vaccine-induced measles virus-specific T cells do not prevent infection or disease but facilitate subsequent clearance of viral RNA. mBio. 5, e01047 (2014).
Blackwelder, W. C., Storsaeter, J., Olin, P. & Hallander, H. O. Acellular pertussis vaccines: efficacy and evaluation of clinical case definitions. Am. J. Dis. Child. 145, 1285–1289 (1991).
Lachenbruch, P. A. Sensitivity, specificity, and vaccine efficacy. Control. Clin. Trials 19, 569–574 (1998).
Hadinegoro, S. R. S. et al. Efficacy and long-term safety of a dengue vaccine in regions of endemic disease. N. Engl. J. Med. 373, 1195–1206 (2015).
OhAinle, M. et al. Dynamics of dengue disease severity determined by the interplay between viral genetics and serotype-specific immunity. Sci. Transl. Med. 3, 114ra128 (2011).
Whitehorn, J. et al. Genetic variants of MICB and PLCE1 and associations with non-severe dengue. PLoS ONE 8, e59067 (2013).
Stephens, H. A. HLA and other gene associations with dengue disease severity. Curr. Top. Microbiol. Immunol. 338, 99–114 (2010).
Acknowledgements
The authors thank P. Leventhal (4Clinics, Paris, France) for help with scientific editing, funded by Sanofi Pasteur. The authors acknowledge colleagues at Sanofi Pasteur (C. Nelson, K. Kester, M. Saville, V. Delore, N. Tornieporth, S. Gurunathan, J. Lang and P. Commander) for critical reading of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
B.G. and N.J. are employees of Sanofi Pasteur.
Rights and permissions
About this article
Cite this article
Guy, B., Jackson, N. Dengue vaccine: hypotheses to understand CYD-TDV-induced protection. Nat Rev Microbiol 14, 45–54 (2016). https://doi.org/10.1038/nrmicro.2015.2
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrmicro.2015.2
This article is cited by
-
Is new dengue vaccine efficacy data a relief or cause for concern?
npj Vaccines (2023)
-
Characterization of B-cell and T-cell responses to a tetravalent dengue purified inactivated vaccine in healthy adults
npj Vaccines (2022)
-
Natural immunogenic properties of bioinformatically predicted linear B-cell epitopes of dengue envelope and pre-membrane proteins
BMC Immunology (2021)
-
Computational screening of medicinal plant phytochemicals to discover potent pan-serotype inhibitors against dengue virus
Scientific Reports (2019)
-
Dengue virus nonstructural 3 protein interacts directly with human glyceraldehyde-3-phosphate dehydrogenase (GAPDH) and reduces its glycolytic activity
Scientific Reports (2019)