Key Points
-
The hallmark fever response during infection and disease has been maintained throughout hundreds of millions of years in endothermic (warm-blooded) and ectothermic (cold-blooded) species.
-
Febrile temperatures boost the probability of an effective immune response by stimulating both the innate and the adaptive arms of the immune system.
-
The pyrogenic cytokine interleukin-6 (IL-6) contributes to two phases of the febrile response: it elevates the core body temperature via thermoregulatory autonomic mechanisms, and it also serves as a thermally sensitive effector molecule that amplifies lymphocyte trafficking into lymphoid organs.
-
There is emerging evidence that adrenergic signalling pathways associated with thermogenesis can greatly influence immune cell function.
-
Thus, the thermal element of fever serves as a systemic alert system that broadly promotes immune surveillance in the setting of infection and disease.
Abstract
Fever is a cardinal response to infection that has been conserved in warm-blooded and cold-blooded vertebrates for more than 600 million years of evolution. The fever response is executed by integrated physiological and neuronal circuitry and confers a survival benefit during infection. In this Review, we discuss our current understanding of how the inflammatory cues delivered by the thermal element of fever stimulate innate and adaptive immune responses. We further highlight the unexpected multiplicity of roles of the pyrogenic cytokine interleukin-6 (IL-6), both during fever induction and during the mobilization of lymphocytes to the lymphoid organs that are the staging ground for immune defence. We also discuss the emerging evidence suggesting that the adrenergic signalling pathways associated with thermogenesis shape immune cell function.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Celsus, A. C. A. Cornelius Celsus of Medicine: in Eight Books (ed. Grieve, J.) (D. Wilson & T. Durham, 1756). This set of books summarizes the work of Celsus (approximately 25 BC to 50 AD), who described the four cardinal signs of inflammation.
Kluger, M. J. Phylogeny of fever. Fed. Proc. 38, 30–34 (1979).
Earn, D. J., Andrews, P. W. & Bolker, B. M. Population-level effects of suppressing fever. Proc. Biol. Sci. 281, 20132570 (2014).
Schulman, C. I. et al. The effect of antipyretic therapy upon outcomes in critically ill patients: a randomized, prospective study. Surg. Infect. (Larchmt) 6, 369–375 (2005). References 3 and 4 show that treatment of fever using antipyretic drugs has a detrimental effect on patient outcome during infection.
Ryan, M. & Levy, M. M. Clinical review: fever in intensive care unit patients. Crit. Care 7, 221–225 (2003).
Kurosawa, S., Kobune, F., Okuyama, K. & Sugiura, A. Effects of antipyretics in rinderpest virus infection in rabbits. J. Infect. Dis. 155, 991–997 (1987).
Liu, E. et al. Naturally occurring hypothermia is more advantageous than fever in severe forms of lipopolysaccharide- and Escherichia coli-induced systemic inflammation. Am. J. Physiol. Regul. Integr. Comp. Physiol. 302, R1372–R1383 (2012).
Romanovsky, A. A. Thermoregulation: some concepts have changed. Functional architecture of the thermoregulatory system. Am. J. Physiol. Regul. Integr. Comp. Physiol. 292, R37–R46 (2007).
Romanovsky, A. A., Shido, O., Sakurada, S., Sugimoto, N. & Nagasaka, T. Endotoxin shock: thermoregulatory mechanisms. Am. J. Physiol. 270, R693–R703 (1996).
Almeida, M. C., Steiner, A. A., Branco, L. G. & Romanovsky, A. A. Cold-seeking behavior as a thermoregulatory strategy in systemic inflammation. Eur. J. Neurosci. 23, 3359–3367 (2006).
Launey, Y., Nesseler, N., Malledant, Y. & Seguin, P. Clinical review: fever in septic ICU patients—friend or foe? Crit. Care 15, 222 (2011).
Polderman, K. H. Induced hypothermia and fever control for prevention and treatment of neurological injuries. Lancet 371, 1955–1969 (2008).
Bernheim, H. A. & Kluger, M. J. Fever: effect of drug-induced antipyresis on survival. Science 193, 237–239 (1976).
Vaughn, L. K., Bernheim, H. A. & Kluger, M. J. Fever in the lizard Dipsosaurus dorsalis. Nature 252, 473–474 (1974).
Covert, J. B. & Reynolds, W. W. Survival value of fever in fish. Nature 267, 43–45 (1977).
Reynolds, W. W., Casterlin, M. E. & Covert, J. B. Behavioural fever in teleost fishes. Nature 259, 41–42 (1976). References 13–16 reveal that ectothermic vertebrates (lizards and fish) develop fever through behavioural changes and that fever is associated with a survival benefit.
Simone-Finstrom, M., Foo, B., Tarpy, D. R. & Starks, P. T. Impact of food availability, pathogen exposure, and genetic diversity on thermoregulation in honey bees (Apis mellifera). J. Insect Behav. 27, 527–539 (2014).
Blanford, S. & Thomas, M. B. Adult survival, maturation, and reproduction of the desert locust Schistocerca gregaria infected with the fungus Metarhizium anisopliae var acridum. J. Invertebr. Pathol. 78, 1–8 (2001).
Mackowiak, P. A. Fever: blessing or curse? A unifying hypothesis. Ann. Intern. Med. 120, 1037–1040 (1994).
Cabanac, M. Fever in the leech, Nephelopsis obscura (Annelida). J. Comp. Physiol. B 159, 281–285 (1989).
Yarwood, C. E. Heat of respiration of injured and diseased leaves. Phytopathology 43, 675–681 (1953).
Zhu, Y. et al. Regulation of thermogenesis in plants: the interaction of alternative oxidase and plant uncoupling mitochondrial protein. J. Integr. Plant Biol. 53, 7–13 (2011).
Pockley, A. G., Calderwood, S. K. & Santoro, M. G. Prokaryotic and Eukaryotic Heat Shock Proteins in Infectious Disease (Springer, 2010).
Lwoff, A. From protozoa to bacteria and viruses. Fifty years with microbes (André Lwoff). Annu. Rev. Microbiol. 25, 1–26 (1971).
Osawa, E. & Muschel, L. H. Studies relating to the serum resistance of certain Gram-negative bacteria. J. Exp. Med. 119, 41–51 (1964).
Hasday, J. D., Thompson, C. & Singh, I. S. Fever, immunity, and molecular adaptations. Compr. Physiol. 4, 109–148 (2014).
Morrison, S. F., Madden, C. J. & Tupone, D. Central control of brown adipose tissue thermogenesis. Front. Endocrinol. 3, 00005 (2012).
Taipale, M., Jarosz, D. F. & Lindquist, S. HSP90 at the hub of protein homeostasis: emerging mechanistic insights. Nature Rev. Mol. Cell Biol. 11, 515–528 (2010).
Akerfelt, M., Morimoto, R. I. & Sistonen, L. Heat shock factors: integrators of cell stress, development and lifespan. Nature Rev. Mol. Cell Biol. 11, 545–555 (2010).
Saper, C. B., Romanovsky, A. A. & Scammell, T. E. Neural circuitry engaged by prostaglandins during the sickness syndrome. Nature Neurosci. 15, 1088–1095 (2012).
Matsumura, K. et al. Brain endothelial cells express cyclooxygenase-2 during lipopolysaccharide-induced fever: light and electron microscopic immunocytochemical studies. J. Neurosci. 18, 6279–6289 (1998).
Yamagata, K. et al. Coexpression of microsomal-type prostaglandin E synthase with cyclooxygenase-2 in brain endothelial cells of rats during endotoxin-induced fever. J. Neurosci. 21, 2669–2677 (2001).
Engstrom, L. et al. Lipopolysaccharide-induced fever depends on prostaglandin E2 production specifically in brain endothelial cells. Endocrinology 153, 4849–4861 (2012).
Blatteis, C. M., Li, S., Li, Z., Feleder, C. & Perlik, V. Cytokines, PGE2 and endotoxic fever: a re-assessment. Prostaglandins Other Lipid Mediat. 76, 1–18 (2005).
Steiner, A. A., Chakravarty, S., Rudaya, A. Y., Herkenham, M. & Romanovsky, A. A. Bacterial lipopolysaccharide fever is initiated via Toll-like receptor 4 on hematopoietic cells. Blood 107, 4000–4002 (2006). References 34 and 35 show that expression and release of PGE2 from haematopoietic cells is required for the development of fever during LPS challenge.
Roth, J. & Blatteis, C. M. Mechanisms of fever production and lysis: lessons from experimental LPS fever. Compr. Physiol. 4, 1563–1604 (2014).
Ivanov, A. I. & Romanovsky, A. A. Prostaglandin E2 as a mediator of fever: synthesis and catabolism. Front. Biosci. 9, 1977–1993 (2004).
Furuyashiki, T. & Narumiya, S. Stress responses: the contribution of prostaglandin E2 and its receptors. Nature Rev. Endocrinol. 7, 163–175 (2011).
Engblom, D. et al. Microsomal prostaglandin E synthase-1 is the central switch during immune-induced pyresis. Nature Neurosci. 6, 1137–1138 (2003).
Lazarus, M. et al. EP3 prostaglandin receptors in the median preoptic nucleus are critical for fever responses. Nature Neurosci. 10, 1131–1133 (2007). References 39 and 40 demonstrate that responses involving EP3 prostaglandin receptors are required for the development of fever.
Nakamura, K. & Morrison, S. F. A thermosensory pathway that controls body temperature. Nature Neurosci. 11, 62–71 (2008).
Dantzer, R. & Wollman, E. Molecular mechanisms of fever: the missing links. Eur. Cytokine Netw. 9, 27–31 (1998).
Steinman, L. Nuanced roles of cytokines in three major human brain disorders. J. Clin. Invest. 118, 3557–3563 (2008).
Akira, S. & Takeda, K. Toll-like receptor signalling. Nature Rev. Immunol. 4, 499–511 (2004).
O'Neill, L. A., Golenbock, D. & Bowie, A. G. The history of Toll-like receptors — redefining innate immunity. Nature Rev. Immunol. 13, 453–460 (2013).
Elander, L., Ruud, J., Korotkova, M., Jakobsson, P. J. & Blomqvist, A. Cyclooxygenase-1 mediates the immediate corticosterone response to peripheral immune challenge induced by lipopolysaccharide. Neurosci. Lett. 470, 10–12 (2010).
Hanada, R. et al. Central control of fever and female body temperature by RANKL/RANK. Nature 462, 505–509 (2009). This study identifies a pivotal role for RANKL in the brain in generating a fever in response to LPS.
Benveniste, E. N., Sparacio, S. M., Norris, J. G., Grenett, H. E. & Fuller, G. M. Induction and regulation of interleukin-6 gene expression in rat astrocytes. J. Neuroimmunol. 30, 201–212 (1990).
Beurel, E. & Jope, R. S. Lipopolysaccharide-induced interleukin-6 production is controlled by glycogen synthase kinase-3 and STAT3 in the brain. J. Neuroinflamm. 6, 9 (2009).
Sawada, M., Suzumura, A. & Marunouchi, T. TNFα induces IL-6 production by astrocytes but not by microglia. Brain Res. 583, 296–299 (1992).
Woodroofe, M. N. et al. Detection of interleukin-1 and interleukin-6 in adult rat brain, following mechanical injury, by in vivo microdialysis: evidence of a role for microglia in cytokine production. J. Neuroimmunol. 33, 227–236 (1991).
Ringheim, G. E., Burgher, K. L. & Heroux, J. A. Interleukin-6 mRNA expression by cortical neurons in culture: evidence for neuronal sources of interleukin-6 production in the brain. J. Neuroimmunol. 63, 113–123 (1995).
Vallieres, L. & Rivest, S. Regulation of the genes encoding interleukin-6, its receptor, and gp130 in the rat brain in response to the immune activator lipopolysaccharide and the proinflammatory cytokine interleukin-1β. J. Neurochem. 69, 1668–1683 (1997).
Cartmell, T., Poole, S., Turnbull, A. V., Rothwell, N. J. & Luheshi, G. N. Circulating interleukin-6 mediates the febrile response to localised inflammation in rats. J. Physiol. 526, 653–661 (2000).
Chai, Z., Gatti, S., Toniatti, C., Poli, V. & Bartfai, T. Interleukin (IL)-6 gene expression in the central nervous system is necessary for fever response to lipopolysaccharide or IL-1β: a study on IL-6-deficient mice. J. Exp. Med. 183, 311–316 (1996).
Kozak, W. et al. IL-6 and IL-1β in fever. Studies using cytokine-deficient (knockout) mice. Ann. NY Acad. Sci. 856, 33–47 (1998).
Hamzic, N. et al. Interleukin-6 primarily produced by non-hematopoietic cells mediates the lipopolysaccharide-induced febrile response. Brain Behav. Immun. 33, 123–130 (2013). References 55–57 highlight that loss of IL-6 signalling alone abrogates fever in response in LPS- or IL-1-induced inflammatory models.
Nilsberth, C., Hamzic, N., Norell, M. & Blomqvist, A. Peripheral lipopolysaccharide administration induces cytokine mRNA expression in the viscera and brain of fever-refractory mice lacking microsomal prostaglandin E synthase-1. J. Neuroendocrinol. 21, 715–721 (2009).
Jiang, Q. et al. Exposure to febrile temperature upregulates expression of pyrogenic cytokines in endotoxin-challenged mice. Am. J. Physiol. 276, R1653–R1660 (1999).
Ostberg, J. R., Taylor, S. L., Baumann, H. & Repasky, E. A. Regulatory effects of fever-range whole-body hyperthermia on the LPS-induced acute inflammatory response. J. Leukoc. Biol. 68, 815–820 (2000).
Rice, P. et al. Febrile-range hyperthermia augments neutrophil accumulation and enhances lung injury in experimental gram-negative bacterial pneumonia. J. Immunol. 174, 3676–3685 (2005). This report establishes that febrile temperatures drive CXCL8 expression to initiate neutrophil infiltration in the lungs.
Grupp, S. A. et al. Chimeric antigen receptor-modified T cells for acute lymphoid leukemia. N. Engl. J. Med. 368, 1509–1518 (2013).
Teachey, D. T. et al. Cytokine release syndrome after blinatumomab treatment related to abnormal macrophage activation and ameliorated with cytokine-directed therapy. Blood 121, 5154–5157 (2013).
Cao, C., Matsumura, K., Yamagata, K. & Watanabe, Y. Endothelial cells of the rat brain vasculature express cyclooxygenase-2 mRNA in response to systemic interleukin-1β: a possible site of prostaglandin synthesis responsible for fever. Brain Res. 733, 263–272 (1996).
Konsman, J. P., Vigues, S., Mackerlova, L., Bristow, A. & Blomqvist, A. Rat brain vascular distribution of interleukin-1 type-1 receptor immunoreactivity: relationship to patterns of inducible cyclooxygenase expression by peripheral inflammatory stimuli. J. Comp. Neurol. 472, 113–129 (2004).
Rummel, C., Sachot, C., Poole, S. & Luheshi, G. N. Circulating interleukin-6 induces fever through a STAT3-linked activation of COX-2 in the brain. Am. J. Physiol. Regul. Integr. Comp. Physiol. 291, R1316–R1326 (2006).
Turnbull, A. V., Prehar, S., Kennedy, A. R., Little, R. A. & Hopkins, S. J. Interleukin-6 is an afferent signal to the hypothalamo-pituitary-adrenal axis during local inflammation in mice. Endocrinology 144, 1894–1906 (2003).
Sundgren-Andersson, A. K., Ostlund, P. & Bartfai, T. IL-6 is essential in TNF-α-induced fever. Am. J. Physiol. 275, R2028–R2034 (1998).
Li, S., Goorha, S., Ballou, L. R. & Blatteis, C. M. Intracerebroventricular interleukin-6, macrophage inflammatory protein-1β and IL-18: pyrogenic and PGE2-mediated? Brain Res. 992, 76–84 (2003).
Nilsberth, C. et al. The role of interleukin-6 in lipopolysaccharide-induced fever by mechanisms independent of prostaglandin E2 . Endocrinology 150, 1850–1860 (2009).
Kong, Y. Y. et al. OPGL is a key regulator of osteoclastogenesis, lymphocyte development and lymph-node organogenesis. Nature 397, 315–323 (1999).
Hashizume, M. & Mihara, M. The roles of interleukin-6 in the pathogenesis of rheumatoid arthritis. Arthritis 2011, 765624 (2011).
Soehnlein, O. & Lindbom, L. Phagocyte partnership during the onset and resolution of inflammation. Nature Rev. Immunol. 10, 427–439 (2010).
Girard, J. P., Moussion, C. & Forster, R. HEVs, lymphatics and homeostatic immune cell trafficking in lymph nodes. Nature Rev. Immunol. 12, 762–773 (2012).
von Andrian, U. H. & Mempel, T. R. Homing and cellular traffic in lymph nodes. Nature Rev. Immunol. 3, 867–878 (2003).
Griffith, J. W., Sokol, C. L. & Luster, A. D. Chemokines and chemokine receptors: positioning cells for host defense and immunity. Annu. Rev. Immunol. 32, 659–702 (2014).
Ostberg, J. R., Ertel, B. R. & Lanphere, J. A. An important role for granulocytes in the thermal regulation of colon tumor growth. Immunol. Invest. 34, 259–272 (2005).
Takada, Y. et al. Granulocyte-colony stimulating factor enhances anti-tumour effect of hyperthermia. Int. J. Hyperthermia 16, 275–286 (2000).
Bernheim, H. A., Bodel, P. T., Askenase, P. W. & Atkins, E. Effects of fever on host defense mechanisms after infection in the lizard Dipsosaurus dorsalis. Br. J. Exp. Pathol. 59, 76–84 (1978).
Ellis, G. S. et al. G-CSF, but not corticosterone, mediates circulating neutrophilia induced by febrile-range hyperthermia. J. Appl. Physiol. 98, 1799–1804 (2005).
Hasday, J. D. et al. Febrile-range hyperthermia augments pulmonary neutrophil recruitment and amplifies pulmonary oxygen toxicity. Am. J. Pathol. 162, 2005–2017 (2003).
Capitano, M. L. et al. Elevating body temperature enhances hematopoiesis and neutrophil recovery after total body irradiation in an IL-1-, IL-17-, and G-CSF-dependent manner. Blood 120, 2600–2609 (2012). This study demonstrates that fever-range hyperthermia promotes neutrophil release from the bone marrow and is protective following irradiation-induced neutropenia in mice.
Ostberg, J. R. & Repasky, E. A. Comparison of the effects of two different whole body hyperthermia protocols on the distribution of murine leukocyte populations. Int. J. Hyperthermia 16, 29–43 (2000).
Tulapurkar, M. E. et al. Febrile-range hyperthermia modifies endothelial and neutrophilic functions to promote extravasation. Am. J. Respir. Cell. Mol. Biol. 46, 807–814 (2012).
Singh, I. S. et al. Heat shock co-activates interleukin-8 transcription. Am. J. Respir. Cell Mol. Biol. 39, 235–242 (2008).
Zanker, K. S. & Lange, J. Whole body hyperthermia and natural killer cell activity. Lancet 1, 1079–1080 (1982).
Shen, R. N., Hornback, N. B., Shidnia, H., Shupe, R. E. & Brahmi, Z. Whole-body hyperthermia decreases lung metastases in lung tumor-bearing mice, possibly via a mechanism involving natural killer cells. J. Clin. Immunol. 7, 246–253 (1987).
Burd, R. et al. Tumor cell apoptosis, lymphocyte recruitment and tumor vascular changes are induced by low temperature, long duration (fever-like) whole body hyperthermia. J. Cell. Physiol. 177, 137–147 (1998).
Kappel, M., Stadeager, C., Tvede, N., Galbo, H. & Pedersen, B. K. Effects of in vivo hyperthermia on natural killer cell activity, in vitro proliferative responses and blood mononuclear cell subpopulations. Clin. Exp. Immunol. 84, 175–180 (1991).
Ostberg, J. R., Dayanc, B. E., Yuan, M., Oflazoglu, E. & Repasky, E. A. Enhancement of natural killer (NK) cell cytotoxicity by fever-range thermal stress is dependent on NKG2D function and is associated with plasma membrane NKG2D clustering and increased expression of MICA on target cells. J. Leukoc. Biol. 82, 1322–1331 (2007).
Multhoff, G., Botzler, C., Wiesnet, M., Eissner, G. & Issels, R. CD3− large granular lymphocytes recognize a heat-inducible immunogenic determinant associated with the 72-kD heat shock protein on human sarcoma cells. Blood 86, 1374–1382 (1995).
Shi, H. et al. Hyperthermia enhances CTL cross-priming. J. Immunol. 176, 2134–2141 (2006).
Jiang, Q. et al. Febrile core temperature is essential for optimal host defense in bacterial peritonitis. Infect. Immun. 68, 1265–1270 (2000).
Hasday, J. D., Fairchild, K. D. & Shanholtz, C. The role of fever in the infected host. Microbes Infect. 2, 1891–1904 (2000).
Lee, C. T., Zhong, L., Mace, T. A. & Repasky, E. A. Elevation in body temperature to fever range enhances and prolongs subsequent responsiveness of macrophages to endotoxin challenge. PLoS ONE 7, e30077 (2012).
Lee, C. T. & Repasky, E. A. Opposing roles for heat and heat shock proteins in macrophage functions during inflammation: a function of cell activation state? Front. Immunol. 3, 140 (2012).
Pritchard, M. T., Li, Z. & Repasky, E. A. Nitric oxide production is regulated by fever-range thermal stimulation of murine macrophages. J. Leukoc. Biol. 78, 630–638 (2005).
Gupta, A. et al. Toll-like receptor agonists and febrile range hyperthermia synergize to induce heat shock protein 70 expression and extracellular release. J. Biol. Chem. 288, 2756–2766 (2013).
Multhoff, G. Heat shock protein 70 (Hsp70): membrane location, export and immunological relevance. Methods 43, 229–237 (2007).
Vega, V. L. et al. Hsp70 translocates into the plasma membrane after stress and is released into the extracellular environment in a membrane-associated form that activates macrophages. J. Immunol. 180, 4299–4307 (2008).
Noessner, E. et al. Tumor-derived heat shock protein 70 peptide complexes are cross-presented by human dendritic cells. J. Immunol. 169, 5424–5432 (2002).
Basu, S., Binder, R. J., Ramalingam, T. & Srivastava, P. K. CD91 is a common receptor for heat shock proteins gp96, hsp90, hsp70, and calreticulin. Immunity 14, 303–313 (2001).
Binder, R. J. & Srivastava, P. K. Essential role of CD91 in re-presentation of gp96-chaperoned peptides. Proc. Natl Acad. Sci. USA 101, 6128–6133 (2004).
Berwin, B. et al. Scavenger receptor-A mediates gp96/GRP94 and calreticulin internalization by antigen-presenting cells. EMBO J. 22, 6127–6136 (2003).
Becker, T., Hartl, F. U. & Wieland, F. CD40, an extracellular receptor for binding and uptake of Hsp70-peptide complexes. J. Cell Biol. 158, 1277–1285 (2002).
Arnouk, H. et al. Tumour secreted grp170 chaperones full-length protein substrates and induces an adaptive anti-tumour immune response in vivo. Int. J. Hyperthermia 26, 366–375 (2010).
Asea, A. et al. Novel signal transduction pathway utilized by extracellular HSP70: role of Toll-like receptor (TLR) 2 and TLR4. J. Biol. Chem. 277, 15028–15034 (2002).
Facciponte, J. G., Wang, X. Y. & Subjeck, J. R. Hsp110 and Grp170, members of the Hsp70 superfamily, bind to scavenger receptor-A and scavenger receptor expressed by endothelial cells-I. Eur. J. Immunol. 37, 2268–2279 (2007).
Lehner, T. et al. Heat shock proteins generate β-chemokines which function as innate adjuvants enhancing adaptive immunity. Eur. J. Immunol. 30, 594–603 (2000).
Panjwani, N. N., Popova, L. & Srivastava, P. K. Heat shock proteins gp96 and hsp70 activate the release of nitric oxide by APCs. J. Immunol. 168, 2997–3003 (2002).
Snyder, Y. M., Guthrie, L., Evans, G. F. & Zuckerman, S. H. Transcriptional inhibition of endotoxin-induced monokine synthesis following heat shock in murine peritoneal macrophages. J. Leukoc. Biol. 51, 181–187 (1992).
Yenari, M. A. et al. Antiapoptotic and anti-inflammatory mechanisms of heat-shock protein protection. Ann. NY Acad. Sci. 1053, 74–83 (2005).
Chen, H. et al. Hsp70 inhibits lipopolysaccharide-induced NF-κB activation by interacting with TRAF6 and inhibiting its ubiquitination. FEBS Lett. 580, 3145–3152 (2006).
Schmitt, E., Gehrmann, M., Brunet, M., Multhoff, G. & Garrido, C. Intracellular and extracellular functions of heat shock proteins: repercussions in cancer therapy. J. Leukoc. Biol. 81, 15–27 (2007).
Manzella, J. P. & Roberts, N. J. Jr. Human macrophage and lymphocyte responses to mitogen stimulation after exposure to influenza virus, ascorbic acid, and hyperthermia. J. Immunol. 123, 1940–1944 (1979).
Postic, B., DeAngelis, C., Breinig, M. K. & Monto, H. O. Effect of temperature on the induction of interferons by endotoxin and virus. J. Bacteriol. 91, 1277–1281 (1966).
Knippertz, I. et al. Mild hyperthermia enhances human monocyte-derived dendritic cell functions and offers potential for applications in vaccination strategies. Int. J. Hyperthermia 27, 591–603 (2011).
van Bruggen, I., Robertson, T. A. & Papadimitriou, J. M. The effect of mild hyperthermia on the morphology and function of murine resident peritoneal macrophages. Exp. Mol. Pathol. 55, 119–134 (1991).
Bachleitner-Hofmann, T. et al. Heat shock treatment of tumor lysate-pulsed dendritic cells enhances their capacity to elicit antitumor T cell responses against medullary thyroid carcinoma. J. Clin. Endocrinol. Metab. 91, 4571–4577 (2006).
Yan, X. et al. Fever range temperature promotes TLR4 expression and signaling in dendritic cells. Life Sci. 80, 307–313 (2007).
Hatzfeld-Charbonnier, A. S. et al. Influence of heat stress on human monocyte-derived dendritic cell functions with immunotherapeutic potential for antitumor vaccines. J. Leukoc. Biol. 81, 1179–1187 (2007). This reference shows that the exposure of human monocyte-derived DCs to febrile temperatures improves their migratory response to chemokines in vitro and their ability to stimulate naive T cell activation.
Ostberg, J. R., Kaplan, K. C. & Repasky, E. A. Induction of stress proteins in a panel of mouse tissues by fever-range whole body hyperthermia. Int. J. Hyperthermia 18, 552–562 (2002).
Peng, J. C. et al. Monocyte-derived DC primed with TLR agonists secrete IL-12p70 in a CD40-dependent manner under hyperthermic conditions. J. Immunother. 29, 606–615 (2006).
Ostberg, J. R., Gellin, C., Patel, R. & Repasky, E. A. Regulatory potential of fever-range whole body hyperthermia on Langerhans cells and lymphocytes in an antigen-dependent cellular immune response. J. Immunol. 167, 2666–2670 (2001).
Tal, O. et al. DC mobilization from the skin requires docking to immobilized CCL21 on lymphatic endothelium and intralymphatic crawling. J. Exp. Med. 208, 2141–2153 (2011).
Schumann, K. et al. Immobilized chemokine fields and soluble chemokine gradients cooperatively shape migration patterns of dendritic cells. Immunity 32, 703–713 (2010).
Weber, M. et al. Interstitial dendritic cell guidance by haptotactic chemokine gradients. Science 339, 328–332 (2013).
Ulvmar, M. H. et al. The atypical chemokine receptor CCRL1 shapes functional CCL21 gradients in lymph nodes. Nature Immunol. 15, 623–630 (2014). References 125–128 describe the role of CCR7 in sensing CCL21 gradients that direct the migration of mature DCs into the afferent lymphatics and within draining lymph nodes.
von Andrian, U. H. Intravital microscopy of the peripheral lymph node microcirculation in mice. Microcirculation 3, 287–300 (1996).
Blattman, J. N. et al. Estimating the precursor frequency of naive antigen-specific CD8 T cells. J. Exp. Med. 195, 657–664 (2002).
Pabst, R. & Binns, R. M. Heterogeneity of lymphocyte homing physiology: several mechanisms operate in the control of migration to lymphoid and non-lymphoid organs in vivo. Immunol. Rev. 108, 83–109 (1989).
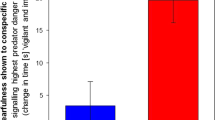
Vardam, T. D. et al. Regulation of a lymphocyte-endothelial-IL-6 trans-signaling axis by fever-range thermal stress: hot spot of immune surveillance. Cytokine 39, 84–96 (2007).
Boscacci, R. T. et al. Comprehensive analysis of lymph node stroma-expressed Ig superfamily members reveals redundant and nonredundant roles for ICAM-1, ICAM-2, and VCAM-1 in lymphocyte homing. Blood 116, 915–925 (2010).
Wang, W. C. et al. Fever-range hyperthermia enhances L-selectin-dependent adhesion of lymphocytes to vascular endothelium. J. Immunol. 160, 961–969 (1998).
Evans, S. S. et al. Dynamic association of L-selectin with the lymphocyte cytoskeletal matrix. J. Immunol. 162, 3615–3624 (1999).
Evans, S. S., Bain, M. D. & Wang, W. C. Fever-range hyperthermia stimulates α4β7 integrin-dependent lymphocyte-endothelial adhesion. Int. J. Hyperthermia 16, 45–59 (2000).
Evans, S. S. et al. Fever-range hyperthermia dynamically regulates lymphocyte delivery to high endothelial venules. Blood 97, 2727–2733 (2001).
Chen, Q. et al. Central role of IL-6 receptor signal-transducing chain gp130 in activation of L-selectin adhesion by fever-range thermal stress. Immunity 20, 59–70 (2004).
Appenheimer, M. M. et al. Conservation of IL-6 trans-signaling mechanisms controlling L-selectin adhesion by fever-range thermal stress. Eur. J. Immunol. 37, 2856–2867 (2007). References 138 and 139 identify an evolutionarily conserved role of IL-6 trans -signalling in enhancing L-selectin-dependent adhesion in lymphocytes during exposure to febrile temperatures.
Chen, Q. et al. Fever-range thermal stress promotes lymphocyte trafficking across high endothelial venules via an interleukin 6 trans-signaling mechanism. Nature Immunol. 7, 1299–1308 (2006). This study establishes that fever-range thermal stress acts through an IL-6 trans -signalling-dependent mechanism to upregulate ICAM1 expression selectively in HEVs.
Chen, Q. et al. Thermal facilitation of lymphocyte trafficking involves temporal induction of intravascular ICAM-1. Microcirculation 16, 143–158 (2009). This study reveals the restricted temporal nature of ICAM1 induction on HEV in response to fever-range hyperthermia and that restoration of normal trafficking involves a zinc-dependent metalloproteinase-dependent mechanism.
Fisher, D. T. et al. IL-6 trans-signaling licenses mouse and human tumor microvascular gateways for trafficking of cytotoxic T cells. J. Clin. Invest. 121, 3846–3859 (2011). This study demonstrates that febrile-range thermal therapy acts through IL-6 trans -signalling to promote the trafficking of CD8+ effector T cells into the tumour microenvironment and delays tumour growth.
Kraybill, W. G. et al. A phase I study of fever-range whole body hyperthermia (FR-WBH) in patients with advanced solid tumours: correlation with mouse models. Int. J. Hyperthermia 18, 253–266 (2002).
Picker, L. J. & Butcher, E. C. Physiological and molecular mechanisms of lymphocyte homing. Annu. Rev. Immunol. 10, 561–591 (1992).
Carman, C. V. & Springer, T. A. Integrin avidity regulation: are changes in affinity and conformation underemphasized? Curr. Opin. Cell Biol. 15, 547–556 (2003).
Schurpf, T. & Springer, T. A. Regulation of integrin affinity on cell surfaces. EMBO J. 30, 4712–4727 (2011).
Carman, C. V. & Springer, T. A. A transmigratory cup in leukocyte diapedesis both through individual vascular endothelial cells and between them. J. Cell Biol. 167, 377–388 (2004).
Carman, C. V. & Springer, T. A. Trans-cellular migration: cell–cell contacts get intimate. Curr. Opin. Cell Biol. 20, 533–540 (2008).
Roberts, N. J. Jr & Steigbigel, R. T. Hyperthermia and human leukocyte functions: effects on response of lymphocytes to mitogen and antigen and bactericidal capacity of monocytes and neutrophils. Infect. Immun. 18, 673–679 (1977).
Smith, J. B., Knowlton, R. P. & Agarwal, S. S. Human lymphocyte responses are enhanced by culture at 40 °C. J. Immunol. 121, 691–694 (1978).
Mace, T. A. et al. Differentiation of CD8+ T cells into effector cells is enhanced by physiological range hyperthermia. J. Leukoc. Biol. 90, 951–962 (2011). This study shows that fever-range temperatures enhance T cell activation by altering the fluidity of the plasma membrane and by pre-association of the signalling components of the TCR complex.
Mace, T. A., Zhong, L., Kokolus, K. M. & Repasky, E. A. Effector CD8+ T cell IFN-γ production and cytotoxicity are enhanced by mild hyperthermia. Int. J. Hyperthermia 28, 9–18 (2012).
Zynda, E. et al. A role for the thermal microenvironment in co-stimulation requirements during T cell activation. Cell Cycle (in the press).
Calabrese, L. H. & Rose-John, S. IL-6 biology: implications for clinical targeting in rheumatic disease. Nature Rev. Rheumatol. 10, 720–727 (2014).
Fisher, D. T., Appenheimer, M. M. & Evans, S. S. The two faces of IL-6 in the tumor microenvironment. Semin. Immunol. 26, 38–47 (2014).
Jostock, T. et al. Soluble gp130 is the natural inhibitor of soluble interleukin-6 receptor transsignaling responses. Eur. J. Biochem. 268, 160–167 (2001).
Atreya, R. et al. Blockade of interleukin 6 trans signaling suppresses T-cell resistance against apoptosis in chronic intestinal inflammation: evidence in Crohn disease and experimental colitis in vivo. Nature Med. 6, 583–588 (2000).
Yu, H., Pardoll, D. & Jove, R. STATs in cancer inflammation and immunity: a leading role for STAT3. Nature Rev. Cancer 9, 798–809 (2009).
Shah, A. et al. Cytokine and adhesion molecule expression in primary human endothelial cells stimulated with fever-range hyperthermia. Int. J. Hyperthermia 18, 534–551 (2002).
Lefor, A. T. et al. Hyperthermia increases intercellular adhesion molecule-1 expression and lymphocyte adhesion to endothelial cells. Surgery 116, 214–220; discussion 220–221 (1994).
Ager, A. Isolation and culture of high endothelial cells from rat lymph nodes. J. Cell Sci. 87, 133–144 (1987).
Lee, M. et al. Transcriptional programs of lymphoid tissue capillary and high endothelium reveal control mechanisms for lymphocyte homing. Nature Immunol. 15, 982–995 (2014).
Mikucki, M. E. et al. Preconditioning thermal therapy: flipping the switch on IL-6 for anti-tumour immunity. Int. J. Hyperthermia 29, 464–473 (2013).
Malhotra, D. et al. Transcriptional profiling of stroma from inflamed and resting lymph nodes defines immunological hallmarks. Nature Immunol. 13, 499–510 (2012).
Katakai, T., Hara, T., Sugai, M., Gonda, H. & Shimizu, A. Lymph node fibroblastic reticular cells construct the stromal reticulum via contact with lymphocytes. J. Exp. Med. 200, 783–795 (2004).
Inouye, S. et al. Heat shock transcription factor 1 opens chromatin structure of interleukin-6 promoter to facilitate binding of an activator or a repressor. J. Biol. Chem. 282, 33210–33217 (2007).
House, S. D. et al. Effects of heat shock, stannous chloride, and gallium nitrate on the rat inflammatory response. Cell Stress Chaperones 6, 164–171 (2001).
Ensor, J. E. et al. Differential effects of hyperthermia on macrophage interleukin-6 and tumor necrosis factor-α expression. Am. J. Physiol. 266, C967–C974 (1994).
Fairchild, K. D., Viscardi, R. M., Hester, L., Singh, I. S. & Hasday, J. D. Effects of hypothermia and hyperthermia on cytokine production by cultured human mononuclear phagocytes from adults and newborns. J. Interferon Cytokine Res. 20, 1049–1055 (2000).
Hagiwara, S., Iwasaka, H., Matsumoto, S. & Noguchi, T. Changes in cell culture temperature alter release of inflammatory mediators in murine macrophagic RAW264.7 cells. Inflamm. Res. 56, 297–303 (2007).
Cooper, Z. A. et al. Febrile-range temperature modifies cytokine gene expression in LPS-stimulated macrophages by differentially modifying NF-κB recruitment to cytokine gene promoters. Am. J. Physiol. Cell Physiol. 298, C171–C181 (2010).
Ensor, J. E., Crawford, E. K. & Hasday, J. D. Warming macrophages to febrile range destabilizes tumor necrosis factor-α mRNA without inducing heat shock. Am. J. Physiol. 269, C1140–C1146 (1995).
Singh, I. S., He, J. R., Calderwood, S. & Hasday, J. D. A high affinity HSF-1 binding site in the 5′-untranslated region of the murine tumor necrosis factor-α gene is a transcriptional repressor. J. Biol. Chem. 277, 4981–4988 (2002).
Fiuza, C. et al. Inflammation-promoting activity of HMGB1 on human microvascular endothelial cells. Blood 101, 2652–2660 (2003).
Lee, C. T. et al. Defining immunological impact and therapeutic benefit of mild heating in a murine model of arthritis. PLoS ONE 10, e0120327 (2015).
Cannon, B. & Nedergaard, J. Brown adipose tissue: function and physiological significance. Physiol. Rev. 84, 277–359 (2004).
Cannon, B. & Nedergaard, J. Nonshivering thermogenesis and its adequate measurement in metabolic studies. J. Exp. Biol. 214, 242–253 (2011).
Elenkov, I. J., Wilder, R. L., Chrousos, G. P. & Vizi, E. S. The sympathetic nerve—an integrative interface between two supersystems: the brain and the immune system. Pharmacol. Rev. 52, 595–638 (2000).
Eng, J. W. et al. A nervous tumor microenvironment: the impact of adrenergic stress on cancer cells, immunosuppression, and immunotherapeutic response. Cancer Immunol. Immunother. 63, 1115–1128 (2014).
Padgett, D. A. & Glaser, R. How stress influences the immune response. Trends Immunol. 24, 444–448 (2003).
Nakai, A., Hayano, Y., Furuta, F., Noda, M. & Suzuki, K. Control of lymphocyte egress from lymph nodes through β2-adrenergic receptors. J. Exp. Med. 211, 2583–2598 (2014).
Slota, C., Shi, A., Chen, G., Bevans, M. & Weng, N. P. Norepinephrine preferentially modulates memory CD8 T cell function inducing inflammatory cytokine production and reducing proliferation in response to activation. Brain Behav. Immun. 46, 168–179 (2015).
Nguyen, K. D. et al. Alternatively activated macrophages produce catecholamines to sustain adaptive thermogenesis. Nature 480, 104–108 (2011).
Kokolus, K. M. et al. Baseline tumor growth and immune control in laboratory mice are significantly influenced by subthermoneutral housing temperature. Proc. Natl Acad. Sci. USA 110, 20176–20181 (2013). References 183 and 184 establish that noradrenaline-driven thermogenesis shapes the phenotype of the immune response by altering macrophage differentiation and antitumour immunity.
Kokolus, K. M. et al. Stressful presentations: mild cold stress in laboratory mice influences phenotype of dendritic cells in naive and tumor-bearing mice. Front. Immunol. 5, 23 (2014).
Eng, J. W. et al. Housing temperature-induced stress drives therapeutic resistance in murine tumour models through β2-adrenergic receptor activation. Nature Commun. 6, 6426 (2015).
Glaser, R. & Kiecolt-Glaser, J. K. Stress-induced immune dysfunction: implications for health. Nature Rev. Immunol. 5, 243–251 (2005).
Karp, C. L. & Murray, P. J. Non-canonical alternatives: what a macrophage is 4. J. Exp. Med. 209, 427–431 (2012).
Di, Y. P., Repasky, E. A. & Subjeck, J. R. Distribution of HSP70, protein kinase C, and spectrin is altered in lymphocytes during a fever-like hyperthermia exposure. J. Cell. Physiol. 172, 44–54 (1997).
Tulapurkar, M. E., Asiegbu, B. E., Singh, I. S. & Hasday, J. D. Hyperthermia in the febrile range induces HSP72 expression proportional to exposure temperature but not to HSF-1 DNA-binding activity in human lung epithelial A549 cells. Cell Stress Chaperones 14, 499–508 (2009).
Gothard, L. Q., Ruffner, M. E., Woodward, J. G., Park-Sarge, O. K. & Sarge, K. D. Lowered temperature set point for activation of the cellular stress response in T-lymphocytes. J. Biol. Chem. 278, 9322–9326 (2003).
Rossi, A., Coccia, M., Trotta, E., Angelini, M. & Santoro, M. G. Regulation of cyclooxygenase-2 expression by heat: a novel aspect of heat shock factor 1 function in human cells. PLoS ONE 7, e31304 (2012).
Chatterjee, M. et al. STAT3 and MAPK signaling maintain overexpression of heat shock proteins 90α and β in multiple myeloma cells, which critically contribute to tumor-cell survival. Blood 109, 720–728 (2007).
Marubayashi, S. et al. HSP90 is a therapeutic target in JAK2-dependent myeloproliferative neoplasms in mice and humans. J. Clin. Invest. 120, 3578–3593 (2010).
Sato, N. et al. Involvement of heat-shock protein 90 in the interleukin-6-mediated signaling pathway through STAT3. Biochem. Biophys. Res. Commun. 300, 847–852 (2003).
Shang, L. & Tomasi, T. B. The heat shock protein 90-CDC37 chaperone complex is required for signaling by types I and II interferons. J. Biol. Chem. 281, 1876–1884 (2006).
Weigert, O. et al. Genetic resistance to JAK2 enzymatic inhibitors is overcome by HSP90 inhibition. J. Exp. Med. 209, 259–273 (2012).
Patapoutian, A., Peier, A. M., Story, G. M. & Viswanath, V. ThermoTRP channels and beyond: mechanisms of temperature sensation. Nature Rev. Neurosci. 4, 529–539 (2003).
Ramsey, I. S., Delling, M. & Clapham, D. E. An introduction to TRP channels. Annu. Rev. Physiol. 68, 619–647 (2006).
Trepel, J., Mollapour, M., Giaccone, G. & Neckers, L. Targeting the dynamic HSP90 complex in cancer. Nature Rev. Cancer 10, 537–549 (2010).
Zou, J., Guo, Y., Guettouche, T., Smith, D. F. & Voellmy, R. Repression of heat shock transcription factor HSF1 activation by HSP90 (HSP90 complex) that forms a stress-sensitive complex with HSF1. Cell 94, 471–480 (1998).
Ahn, S. G. & Thiele, D. J. Redox regulation of mammalian heat shock factor 1 is essential for Hsp gene activation and protection from stress. Genes Dev. 17, 516–528 (2003).
Whitesell, L. & Lindquist, S. L. HSP90 and the chaperoning of cancer. Nature Rev. Cancer 5, 761–772 (2005).
Neckers, L. & Workman, P. Hsp90 molecular chaperone inhibitors: are we there yet? Clin. Cancer Res. 18, 64–76 (2012).
Muralidharan, S. & Mandrekar, P. Cellular stress response and innate immune signaling: integrating pathways in host defense and inflammation. J. Leukoc. Biol. 94, 1167–1184 (2013).
Chu, K. F. & Dupuy, D. E. Thermal ablation of tumours: biological mechanisms and advances in therapy. Nature Rev. Cancer 14, 199–208 (2014).
Repasky, E. A., Evans, S. S. & Dewhirst, M. W. Temperature matters! And why it should matter to tumor immunologists. Cancer Immunol. Res. 1, 210–216 (2013).
Haemmerich, D. & Laeseke, P. F. Thermal tumour ablation: devices, clinical applications and future directions. Int. J. Hyperthermia 21, 755–760 (2005).
Issels, R. D. et al. Neo-adjuvant chemotherapy alone or with regional hyperthermia for localised high-risk soft-tissue sarcoma: a randomised phase 3 multicentre study. Lancet Oncol. 11, 561–570 (2010).
Wessalowski, R. et al. Regional deep hyperthermia for salvage treatment of children and adolescents with refractory or recurrent non-testicular malignant germ-cell tumours: an open-label, non-randomised, single-institution, phase 2 study. Lancet Oncol. 14, 843–852 (2013).
Jones, E. L. et al. Randomized trial of hyperthermia and radiation for superficial tumors. J. Clin. Oncol. 23, 3079–3085 (2005). References 209–211 demonstrate that thermal therapy has a clinical benefit when used in an adjuvant setting in combination with chemotherapy or radiotherapy.
Kong, G., Braun, R. D. & Dewhirst, M. W. Characterization of the effect of hyperthermia on nanoparticle extravasation from tumor vasculature. Cancer Res. 61, 3027–3032 (2001).
Sen, A. et al. Mild elevation of body temperature reduces tumor interstitial fluid pressure and hypoxia and enhances efficacy of radiotherapy in murine tumor models. Cancer Res. 71, 3872–3880 (2011).
Xu, Y. et al. Fever-range whole body hyperthermia increases the number of perfused tumor blood vessels and therapeutic efficacy of liposomally encapsulated doxorubicin. Int. J. Hyperthermia 23, 513–527 (2007).
Song, C. W., Park, H. J., Lee, C. K. & Griffin, R. Implications of increased tumor blood flow and oxygenation caused by mild temperature hyperthermia in tumor treatment. Int. J. Hyperthermia 21, 761–767 (2005).
Dewhirst, M. W., Landon, C. D., Hofmann, C. L. & Stauffer, P. R. Novel approaches to treatment of hepatocellular carcinoma and hepatic metastases using thermal ablation and thermosensitive liposomes. Surg. Oncol. Clin. N. Am. 22, 545–561 (2013).
Page, D. B., Postow, M. A., Callahan, M. K., Allison, J. P. & Wolchok, J. D. Immune modulation in cancer with antibodies. Annu. Rev. Med. 65, 185–202 (2014).
Restifo, N. P., Dudley, M. E. & Rosenberg, S. A. Adoptive immunotherapy for cancer: harnessing the T cell response. Nature Rev. Immunol. 12, 269–281 (2012).
Palucka, K. & Banchereau, J. Cancer immunotherapy via dendritic cells. Nature Rev. Cancer 12, 265–277 (2012).
Wolchok, J. D. & Chan, T. A. Cancer: antitumour immunity gets a boost. Nature 515, 496–498 (2014).
Guo, J. et al. Intratumoral injection of dendritic cells in combination with local hyperthermia induces systemic antitumor effect in patients with advanced melanoma. Int. J. Cancer 120, 2418–2425 (2007).
Mukhopadhaya, A. et al. Localized hyperthermia combined with intratumoral dendritic cells induces systemic antitumor immunity. Cancer Res. 67, 7798–7806 (2007).
Grivennikov, S. I., Greten, F. R. & Karin, M. Immunity, inflammation, and cancer. Cell 140, 883–899 (2010).
Acknowledgements
The authors thank M. Appenheimer, J. Black and M. Messmer for helpful comments on the manuscript, and E. Smith and UC Berkeley Natural Resources Library for assistance with archived citations. This work was supported by the US National Institutes of Health (CA79765, CA085183 and AI082039) and the Jennifer Linscott Tietgen Family Foundation. The authors also acknowledge the significant contributions of colleagues in the field that could not always be cited owing to space limitations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Evans, S., Repasky, E. & Fisher, D. Fever and the thermal regulation of immunity: the immune system feels the heat. Nat Rev Immunol 15, 335–349 (2015). https://doi.org/10.1038/nri3843
Published:
Issue Date:
DOI: https://doi.org/10.1038/nri3843
This article is cited by
-
Therapeutic bacteria and viruses to combat cancer: double-edged sword in cancer therapy: new insights for future
Cell Communication and Signaling (2024)
-
Temperature impacts the bovine ex vivo immune response towards Mycoplasmopsis bovis
Veterinary Research (2024)
-
Fever-like temperature impacts on Staphylococcus aureus and Pseudomonas aeruginosa interaction, physiology, and virulence both in vitro and in vivo
BMC Biology (2024)
-
Immune response enhancement by dietary supplementation with Caesalpinia sappan extract in weaned pigs challenged with porcine reproductive and respiratory syndrome virus
BMC Veterinary Research (2024)
-
Elevated body temperature is associated with depressive symptoms: results from the TemPredict Study
Scientific Reports (2024)