Key Points
-
Prion diseases are fatal, transmissible, neurodegenerative conditions of sporadic, infectious, iatrogenic or genetic origin. The infectious agent is termed a prion and consists of or coincides with scrapie prion protein (PrPSc), which is a misfolded conformer of cellular prion protein (PrPC).
-
Besides enabling prion replication and mediating prion-induced neurotoxicity, the ubiquitously expressed, membrane-anchored PrPC is involved in myelin maintenance under physiological conditions. Numerous other functions have been attributed to PrPC, including many within the immune system, but they have not been mechanistically elucidated and some are controversial.
-
In acquired prion diseases, prions are often first found in lymphoid tissues, mainly in association with follicular dendritic cells (FDCs). From lymphoid tissues, prions exploit nerves of the autonomic nervous system to reach the central nervous system (CNS), where they have their toxic effect.
-
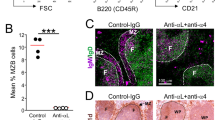
Lymphoid tissue inducer cells and B cells instruct perivascular stromal cells to form mature FDCs through tumour necrosis factor receptor 1 and lymphotoxin-β receptor signalling. Interference with these pathways can temporally deplete FDCs and retard neuroinvasion in experimental models of peripheral exposure to prions, so this can represent a post-exposure prophylaxis approach.
-
Prion infection does not induce an apparent peripheral immune response but activates microglia and astrocytes in the CNS. Microglia phagocytose prions, thereby playing a protective part in the disease development.
-
Immunotherapy, including both active and passive immunization, provides the potential to combat prion disease. However, great caution should be taken because of the striking toxicity of certain PrP-specific antibodies.
Abstract
Individuals infected with prions succumb to brain damage, and prion infections continue to be inexorably lethal. However, many crucial steps in prion pathogenesis occur in lymphatic organs and precede invasion of the central nervous system. In the past two decades, a great deal has been learnt concerning the cellular and molecular mechanisms of prion lymphoinvasion. These properties are diagnostically useful and have, for example, facilitated preclinical diagnosis of variant Creutzfeldt–Jakob disease in the tonsils. Moreover, the early colonization of lymphoid organs can be exploited for post-exposure prophylaxis of prion infections. As stromal cells of lymphoid organs are crucial for peripheral prion infection, the dedifferentiation of these cells offers a powerful means of hindering prion spread in infected individuals. In this Review, we discuss the current knowledge of the immunobiology of prions with an emphasis on how basic discoveries might enable translational strategies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Cuille, J. & Chelle, P. L. Experimental transmission of trembling to the goat. Comptes Rendus Séances Acad. Sci. 208, 1058–1160 (1939).
Gajdusek, D. C. & Zigas, V. Degenerative disease of the central nervous system in New Guinea; the endemic occurrence of kuru in the native population. N. Engl. J. Med. 257, 974–978 (1957).
Duffy, P. et al. Letter: possible person-to-person transmission of Creutzfeldt–Jakob disease. N. Engl. J. Med. 290, 692–693 (1974).
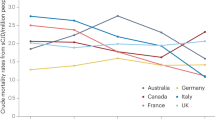
Will, R. G. et al. A new variant of Creutzfeldt–Jakob disease in the UK. Lancet 347, 921–925 (1996).
Llewelyn, C. A. et al. Possible transmission of variant Creutzfeldt–Jakob disease by blood transfusion. Lancet 363, 417–421 (2004).
Bishop, M. T. et al. Prion infectivity in the spleen of a PRNP heterozygous individual with subclinical variant Creutzfeldt–Jakob disease. Brain 136, 1139–1145 (2013).
Prusiner, S. B. Novel proteinaceous infectious particles cause scrapie. Science 216, 136–144 (1982).
Knowles, T. P. et al. An analytical solution to the kinetics of breakable filament assembly. Science 326, 1533–1537 (2009).
Brandner, S. et al. Normal host prion protein necessary for scrapie-induced neurotoxicity. Nature 379, 339–343 (1996).
Linden, R. et al. Physiology of the prion protein. Physiol. Rev. 88, 673–728 (2008).
Aguzzi, A., Barres, B. A. & Bennett, M. L. Microglia: scapegoat, saboteur, or something else? Science 339, 156–161 (2013).
Aguzzi, A. & Sigurdson, C. J. Antiprion immunotherapy: to suppress or to stimulate? Nature Rev. Immunol. 4, 725–736 (2004).
Bueler, H. et al. Normal development and behaviour of mice lacking the neuronal cell-surface PrP protein. Nature 356, 577–582 (1992).
Bremer, J. et al. Axonal prion protein is required for peripheral myelin maintenance. Nature Neurosci. 13, 310–318 (2010). This study shows that neuronal PrPC and its regulated proteolysis are required to maintain peripheral myelination.
Miranda, A., Pericuesta, E., Ramirez, M. A. & Gutierrez-Adan, A. Prion protein expression regulates embryonic stem cell pluripotency and differentiation. PLoS ONE 6, e18422 (2011).
Petit, C. S. et al. Requirement of cellular prion protein for intestinal barrier function and mislocalization in patients with inflammatory bowel disease. Gastroenterology 143, 122–132.e15 (2012).
Nakato, G. et al. Cutting edge: Brucella abortus exploits a cellular prion protein on intestinal M cells as an invasive receptor. J. Immunol. 189, 1540–1544 (2012).
Nuvolone, M. et al. SIRPα polymorphisms, but not the prion protein, control phagocytosis of apoptotic cells. J. Exp. Med. http://dx.doi.org/10.1084/jem.20131274 (2013).
de Almeida, C. J. et al. The cellular prion protein modulates phagocytosis and inflammatory response. J. Leukoc. Biol. 77, 238–246 (2005).
Pan, K. M. et al. Conversion of α-helices into β-sheets features in the formation of the scrapie prion proteins. Proc. Natl Acad. Sci. USA 90, 10962–10966 (1993).
Wang, F., Wang, X., Yuan, C. G. & Ma, J. Generating a prion with bacterially expressed recombinant prion protein. Science 327, 1132–1135 (2010).
Kimberlin, R. H. & Walker, C. A. Pathogenesis of scrapie in mice after intragastric infection. Virus Res. 12, 213–220 (1989).
Prinz, M. et al. Oral prion infection requires normal numbers of Peyer's patches but not of enteric lymphocytes. Am. J. Pathol. 162, 1103–1111 (2003).
Sigurdson, C. J. et al. Bacterial colitis increases susceptibility to oral prion disease. J. Infect. Dis. 199, 243–252 (2009).
Heppner, F. L. et al. Transepithelial prion transport by M cells. Nature Med. 7, 976–977 (2001).
Donaldson, D. S. et al. M cell-depletion blocks oral prion disease pathogenesis. Mucosal Immunol. 5, 216–225 (2012).
Kujala, P. et al. Prion uptake in the gut: identification of the first uptake and replication sites. PLoS Pathog. 7, e1002449 (2011).
Carp, R. I. & Callahan, S. M. In vitro interaction of scrapie agent and mouse peritoneal macrophages. Intervirology 16, 8–13 (1981).
Beringue, V. et al. Role of spleen macrophages in the clearance of scrapie agent early in pathogenesis. J. Pathol. 190, 495–502 (2000).
Huang, F. P., Farquhar, C. F., Mabbott, N. A., Bruce, M. E. & MacPherson, G. G. Migrating intestinal dendritic cells transport PrPSc from the gut. J. Gen. Virol. 83, 267–271 (2002).
Raymond, C. R., Aucouturier, P. & Mabbott, N. A. In vivo depletion of CD11c+ cells impairs scrapie agent neuroinvasion from the intestine. J. Immunol. 179, 7758–7766 (2007).
Houston, F., Foster, J. D., Chong, A., Hunter, N. & Bostock, C. J. Transmission of BSE by blood transfusion in sheep. Lancet 356, 999–1000 (2000).
Mathiason, C. K. et al. Infectious prions in the saliva and blood of deer with chronic wasting disease. Science 314, 133–136 (2006).
Collins, S. et al. Surgical treatment and risk of sporadic Creutzfeldt–Jakob disease: a case-control study. Lancet 353, 693–697 (1999).
Carp, R. I. Transmission of scrapie by oral route: effect of gingival scarification. Lancet 1, 170–171 (1982).
Mohan, J., Brown, K. L., Farquhar, C. F., Bruce, M. E. & Mabbott, N. A. Scrapie transmission following exposure through the skin is dependent on follicular dendritic cells in lymphoid tissues. J. Dermatol. Sci. 35, 101–111 (2004).
Glaysher, B. R. & Mabbott, N. A. Role of the draining lymph node in scrapie agent transmission from the skin. Immunol. Lett. 109, 64–71 (2007).
Denkers, N. D. et al. Aerosol transmission of chronic wasting disease in white-tailed deer. J. Virol. 87, 1890–1892 (2013).
Haybaeck, J. et al. Aerosols transmit prions to immunocompetent and immunodeficient mice. PLoS Pathog. 7, e1001257 (2011).
Nichols, T. A. et al. Intranasal inoculation of white-tailed deer (Odocoileus virginianus) with lyophilized chronic wasting disease prion particulate complexed to montmorillonite clay. PLoS ONE 8, e62455 (2013).
Kincaid, A. E., Hudson, K. F., Richey, M. W. & Bartz, J. C. Rapid transepithelial transport of prions following inhalation. J. Virol. 86, 12731–12740 (2012).
Pattison, I. H. & Millson, G. C. Further observations on the experimental production of scrapie in goats and sheep. J. Comp. Pathol. 70, 182–193 (1960).
Sigurdson, C. J. et al. Oral transmission and early lymphoid tropism of chronic wasting disease PrPres in mule deer fawns (Odocoileus hemionus). J. Gen. Virol. 80, 2757–2764 (1999).
Hadlow, W. J., Race, R. E. & Kennedy, R. C. Temporal distribution of transmissible mink encephalopathy virus in mink inoculated subcutaneously. J. Virol. 61, 3235–3240 (1987).
Hilton, D. A., Fathers, E., Edwards, P., Ironside, J. W. & Zajicek, J. Prion immunoreactivity in appendix before clinical onset of variant Creutzfeldt–Jakob disease. Lancet 352, 703–704 (1998).
Mohri, S., Handa, S. & Tateishi, J. Lack of effect of thymus and spleen on the incubation period of Creutzfeldt–Jakob disease in mice. J. Gen. Virol. 68, 1187–1189 (1987).
Beringue, V. et al. Facilitated cross-species transmission of prions in extraneural tissue. Science 335, 472–475 (2012).
Hill, A. F., Zeidler, M., Ironside, J. & Collinge, J. Diagnosis of new variant Creutzfeldt–Jakob disease by tonsil biopsy. Lancet 349, 99–100 (1997).
Fraser, H. & Dickinson, A. G. Pathogenesis of scrapie in the mouse: the role of the spleen. Nature 226, 462–463 (1970). This study shows prion accumulation in lymphoid tissues of scrapie-infected mice.
Clarke, M. C. & Haig, D. A. Multiplication of scrapie agent in mouse spleen. Res. Vet. Sci. 12, 195–197 (1971).
Kimberlin, R. H. & Walker, C. A. The role of the spleen in the neuroinvasion of scrapie in mice. Virus Res. 12, 201–211 (1989).
Kitamoto, T., Muramoto, T., Mohri, S., Doh-Ura, K. & Tateishi, J. Abnormal isoform of prion protein accumulates in follicular dendritic cells in mice with Creutzfeldt–Jakob disease. J. Virol. 65, 6292–6295 (1991).
Lasmezas, C. I. et al. Immune system-dependent and -independent replication of the scrapie agent. J. Virol. 70, 1292–1295 (1996).
Brown, K. L., Stewart, K., Bruce, M. E. & Fraser, H. Severely combined immunodeficient (SCID) mice resist infection with bovine spongiform encephalopathy. J. Gen. Virol. 78, 2707–2710 (1997).
Lavelle, G. C., Sturman, L. & Hadlow, W. J. Isolation from mouse spleen of cell populations with high specific infectivity for scrapie virus. Infect. Immun. 5, 319–323 (1972).
Clarke, M. C. & Kimberlin, R. H. Pathogenesis of mouse scrapie: distribution of agent in the pulp and stroma of infected spleens. Vet. Microbiol. 9, 215–225 (1984).
Fraser, H. & Farquhar, C. F. Ionising radiation has no influence on scrapie incubation period in mice. Vet. Microbiol. 13, 211–223 (1987).
Klein, M. A. et al. A crucial role for B cells in neuroinvasive scrapie. Nature 390, 687–690 (1997). This study shows that PrP in lymphocytes is not necessary for neuroinvasion of prions, which suggests that cells dependent on B cells or their products, such as FDCs, are involved in this process.
Bueler, H. et al. Mice devoid of PrP are resistant to scrapie. Cell 73, 1339–1347 (1993).
Klein, M. A. et al. PrP expression in B lymphocytes is not required for prion neuroinvasion. Nature Med. 4, 1429–1433 (1998).
Montrasio, F. et al. B lymphocyte-restricted expression of prion protein does not enable prion replication in prion protein knockout mice. Proc. Natl Acad. Sci. USA 98, 4034–4037 (2001).
Blattler, T. et al. PrP-expressing tissue required for transfer of scrapie infectivity from spleen to brain. Nature 389, 69–73 (1997).
Kaeser, P. S., Klein, M. A., Schwarz, P. & Aguzzi, A. Efficient lymphoreticular prion propagation requires PrPc in stromal and hematopoietic cells. J. Virol. 75, 7097–7106 (2001).
Brown, K. L. et al. Scrapie replication in lymphoid tissues depends on prion protein-expressing follicular dendritic cells. Nature Med. 5, 1308–1312 (1999).
Loeuillet, C. et al. Prion replication in the hematopoietic compartment is not required for neuroinvasion in scrapie mouse model. PLoS ONE 5, e13166 (2010).
Krautler, N. J. et al. Follicular dendritic cells emerge from ubiquitous perivascular precursors. Cell 150, 194–206 (2012). These authors show the origin and the ontology of FDCs.
Montrasio, F. et al. Impaired prion replication in spleens of mice lacking functional follicular dendritic cells. Science 288, 1257–1259 (2000).
Mabbott, N. A., Mackay, F., Minns, F. & Bruce, M. E. Temporary inactivation of follicular dendritic cells delays neuroinvasion of scrapie. Nature Med. 6, 719–720 (2000). References 67 and 68 show the role of FDCs in peripheral prion pathogenesis.
Mabbott, N. A., McGovern, G., Jeffrey, M. & Bruce, M. E. Temporary blockade of the tumor necrosis factor receptor signaling pathway impedes the spread of scrapie to the brain. J. Virol. 76, 5131–5139 (2002).
Mabbott, N. A., Young, J., McConnell, I. & Bruce, M. E. Follicular dendritic cell dedifferentiation by treatment with an inhibitor of the lymphotoxin pathway dramatically reduces scrapie susceptibility. J. Virol. 77, 6845–6854 (2003).
Prinz, M. et al. Lymph nodal prion replication and neuroinvasion in mice devoid of follicular dendritic cells. Proc. Natl Acad. Sci. USA 99, 919–924 (2002).
Klein, M. A. et al. Complement facilitates early prion pathogenesis. Nature Med. 7, 488–492 (2001).
Mabbott, N. A., Bruce, M. E., Botto, M., Walport, M. J. & Pepys, M. B. Temporary depletion of complement component C3 or genetic deficiency of C1q significantly delays onset of scrapie. Nature Med. 7, 485–487 (2001). References 72 and 73 show the role of the complement system in peripheral prion pathogenesis.
Zabel, M. D. et al. Stromal complement receptor CD21/35 facilitates lymphoid prion colonization and pathogenesis. J. Immunol. 179, 6144–6152 (2007).
McCulloch, L. et al. Follicular dendritic cell-specific prion protein (PrP) expression alone is sufficient to sustain prion infection in the spleen. PLoS Pathog. 7, e1002402 (2011).
Heikenwalder, M. et al. Chronic lymphocytic inflammation specifies the organ tropism of prions. Science 307, 1107–1110 (2005). This study shows that lymphocytic follicles can be sites of prion replication in organs that are usually prion-free.
Seeger, H. et al. Coincident scrapie infection and nephritis lead to urinary prion excretion. Science 310, 324–326 (2005).
Hamir, A. N., Kunkle, R. A., Miller, J. M. & Hall, S. M. Abnormal prion protein in ectopic lymphoid tissue in a kidney of an asymptomatic white-tailed deer experimentally inoculated with the agent of chronic wasting disease. Vet. Pathol. 43, 367–369 (2006).
Ligios, C. et al. PrPSc in mammary glands of sheep affected by scrapie and mastitis. Nature Med. 11, 1137–1138 (2005).
Lacroux, C. et al. Prions in milk from ewes incubating natural scrapie. PLoS Pathog. 4, e1000238 (2008).
Konold, T. et al. Evidence of effective scrapie transmission via colostrum and milk in sheep. BMC Vet. Res. 9, 99 (2013).
Ligios, C. et al. Sheep with scrapie and mastitis transmit infectious prions through the milk. J. Virol. 85, 1136–1139 (2011).
O'Connor, T. et al. Lymphotoxin, but not TNF, is required for prion invasion of lymph nodes. PLoS Pathog. 8, e1002867 (2012).
Heikenwalder, M. et al. Lymphotoxin-dependent prion replication in inflammatory stromal cells of granulomas. Immunity 29, 998–1008 (2008).
Cole, S. & Kimberlin, R. H. Pathogenesis of mouse scrapie: dynamics of vacuolation in brain and spinal cord after intraperitoneal infection. Neuropathol. Appl. Neurobiol. 11, 213–227 (1985).
McBride, P. A. & Beekes, M. Pathological PrP is abundant in sympathetic and sensory ganglia of hamsters fed with scrapie. Neurosci. Lett. 265, 135–138 (1999).
Heggebo, R. et al. Disease-associated PrP in the enteric nervous system of scrapie-affected Suffolk sheep. J. Gen. Virol. 84, 1327–1338 (2003).
Glatzel, M., Heppner, F. L., Albers, K. M. & Aguzzi, A. Sympathetic innervation of lymphoreticular organs is rate limiting for prion neuroinvasion. Neuron 31, 25–34 (2001). This paper shows that the sympathetic innervation of lymphoid organs is one of the rate-limiting steps for prion neuroinvasion.
van Keulen, L. J., Schreuder, B. E., Vromans, M. E., Langeveld, J. P. & Smits, M. A. Pathogenesis of natural scrapie in sheep. Arch. Virol. Suppl. 16, 57–71 (2000).
Sigurdson, C. J., Spraker, T. R., Miller, M. W., Oesch, B. & Hoover, E. A. PrP(CWD) in the myenteric plexus, vagosympathetic trunk and endocrine glands of deer with chronic wasting disease. J. Gen. Virol. 82, 2327–2334 (2001).
Haik, S. et al. The sympathetic nervous system is involved in variant Creutzfeldt–Jakob disease. Nature Med. 9, 1121–1123 (2003).
Prinz, M. et al. Positioning of follicular dendritic cells within the spleen controls prion neuroinvasion. Nature 425, 957–962 (2003). This study shows that the neuroinvasion velocity of prions depends on the distance between FDCs and splenic nerves, and that the neuroimmune transition of prions occurs between FDCs and sympathetic nerves.
Fevrier, B. et al. Cells release prions in association with exosomes. Proc. Natl Acad. Sci. USA 101, 9683–9688 (2004).
Gousset, K. et al. Prions hijack tunnelling nanotubes for intercellular spread. Nature Cell Biol. 11, 328–336 (2009).
Silveira, J. R. et al. The most infectious prion protein particles. Nature 437, 257–261 (2005).
Bartz, J. C., Kincaid, A. E. & Bessen, R. A. Retrograde transport of transmissible mink encephalopathy within descending motor tracts. J. Virol. 76, 5759–5768 (2002).
Spinner, D. S. et al. Accelerated prion disease pathogenesis in Toll-like receptor 4 signaling-mutant mice. J. Virol. 82, 10701–10708 (2008).
Ishibashi, D. et al. Protective role of interferon regulatory factor 3-mediated signaling against prion infection. J. Virol. 86, 4947–4955 (2012).
Prinz, M. et al. Prion pathogenesis in the absence of Toll-like receptor signalling. EMBO Rep. 4, 195–199 (2003).
Porter, D. D., Porter, H. G. & Cox, N. A. Failure to demonstrate a humoral immune response to scrapie infection in mice. J. Immunol. 111, 1407–1410 (1973).
McGovern, G., Brown, K. L., Bruce, M. E. & Jeffrey, M. Murine scrapie infection causes an abnormal germinal centre reaction in the spleen. J. Comp. Pathol. 130, 181–194 (2004).
Kingsbury, D. T., Smeltzer, D. A., Gibbs, C. J. Jr & Gajdusek, D. C. Evidence for normal cell-mediated immunity in scrapie-infected mice. Infect. Immun. 32, 1176–1180 (1981).
Mabbott, N. A. et al. Tumor necrosis factor alpha-deficient, but not interleukin-6-deficient, mice resist peripheral infection with scrapie. J. Virol. 74, 3338–3344 (2000).
Heikenwalder, M. et al. Germinal center B cells are dispensable in prion transport and neuroinvasion. J. Neuroimmunol. 192, 113–123 (2007).
Sasaki, A., Hirato, J. & Nakazato, Y. Immunohistochemical study of microglia in the Creutzfeldt–Jakob diseased brain. Acta Neuropathol. 86, 337–344 (1993).
Williams, A. E., Lawson, L. J., Perry, V. H. & Fraser, H. Characterization of the microglial response in murine scrapie. Neuropathol. Appl. Neurobiol. 20, 47–55 (1994).
Falsig, J. et al. Prion pathogenesis is faithfully reproduced in cerebellar organotypic slice cultures. PLoS Pathog. 8, e1002985 (2012).
Falsig, J. et al. A versatile prion replication assay in organotypic brain slices. Nature Neurosci. 11, 109–117 (2008).
Kranich, J. et al. Engulfment of cerebral apoptotic bodies controls the course of prion disease in a mouse strain-dependent manner. J. Exp. Med. 207, 2271–2281 (2010).
Hughes, M. M., Field, R. H., Perry, V. H., Murray, C. L. & Cunningham, C. Microglia in the degenerating brain are capable of phagocytosis of beads and of apoptotic cells, but do not efficiently remove PrPSc, even upon LPS stimulation. Glia 58, 2017–2030 (2010).
Sharief, M. K., Green, A., Dick, J. P., Gawler, J. & Thompson, E. J. Heightened intrathecal release of proinflammatory cytokines in Creutzfeldt–Jakob disease. Neurology 52, 1289–1291 (1999).
Campbell, I. L., Eddleston, M., Kemper, P., Oldstone, M. B. & Hobbs, M. V. Activation of cerebral cytokine gene expression and its correlation with onset of reactive astrocyte and acute-phase response gene expression in scrapie. J. Virol. 68, 2383–2387 (1994).
Kordek, R. et al. Heightened expression of tumor necrosis factor-α, interleukin-α, and glial fibrillary acidic protein in experimental Creutzfeldt–Jakob disease in mice. Proc. Natl Acad. Sci. USA 93, 9754–9758 (1996).
Walsh, D. T., Betmouni, S. & Perry, V. H. Absence of detectable IL-1β production in murine prion disease: a model of chronic neurodegeneration. J. Neuropathol. Exp. Neurol. 60, 173–182 (2001).
Baker, C. A., Lu, Z. Y., Zaitsev, I. & Manuelidis, L. Microglial activation varies in different models of Creutzfeldt–Jakob disease. J. Virol. 73, 5089–5097 (1999).
Stoeck, K. et al. Interleukin 4 and interleukin 10 levels are elevated in the cerebrospinal fluid of patients with Creutzfeldt–Jakob disease. Arch. Neurol. 62, 1591–1594 (2005).
Schultz, J. et al. Role of interleukin-1 in prion disease-associated astrocyte activation. Am. J. Pathol. 165, 671–678 (2004).
Tamguney, G. et al. Genes contributing to prion pathogenesis. J. Gen. Virol. 89, 1777–1788 (2008).
Akhtar, S. et al. Sod1 deficiency reduces incubation time in mouse models of prion disease. PLoS ONE 8, e54454 (2013).
Thackray, A. M., McKenzie, A. N., Klein, M. A., Lauder, A. & Bujdoso, R. Accelerated prion disease in the absence of interleukin-10. J. Virol. 78, 13697–13707 (2004).
Felton, L. M. et al. MCP-1 and murine prion disease: separation of early behavioural dysfunction from overt clinical disease. Neurobiol. Dis. 20, 283–295 (2005).
O'Shea, M. et al. Investigation of mcp1 as a quantitative trait gene for prion disease incubation time in mouse. Genetics 180, 559–566 (2008).
LaCasse, R. A., Striebel, J. F., Favara, C., Kercher, L. & Chesebro, B. Role of Erk1/2 activation in prion disease pathogenesis: absence of CCR1 leads to increased Erk1/2 activation and accelerated disease progression. J. Neuroimmunol. 196, 16–26 (2008).
Riemer, C., Queck, I., Simon, D., Kurth, R. & Baier, M. Identification of upregulated genes in scrapie-infected brain tissue. J. Virol. 74, 10245–10248 (2000).
Riemer, C. et al. Accelerated prion replication in, but prolonged survival times of, prion-infected CXCR3−/− mice. J. Virol. 82, 12464–12471 (2008).
Baker, C. A., Martin, D. & Manuelidis, L. Microglia from Creutzfeldt–Jakob disease-infected brains are infectious and show specific mRNA activation profiles. J. Virol. 76, 10905–10913 (2002).
Fuhrmann, M. et al. Microglial Cx3cr1 knockout prevents neuron loss in a mouse model of Alzheimer's disease. Nature Neurosci. 13, 411–413 (2010).
Hughes, P. M., Botham, M. S., Frentzel, S., Mir, A. & Perry, V. H. Expression of fractalkine (CX3CL1) and its receptor, CX3CR1, during acute and chronic inflammation in the rodent CNS. Glia 37, 314–327 (2002).
Xie, W. L. et al. Abnormal activation of microglia accompanied with disrupted CX3CR1/CX3CL1 pathway in the brains of the hamsters infected with scrapie agent 263K. J. Mol. Neurosci. 51, 919–932 (2013).
Kim, J. I. et al. Expression of cytokine genes and increased nuclear factor-κB activity in the brains of scrapie-infected mice. Brain Res. Mol. Brain Res. 73, 17–27 (1999).
Bourteele, S. et al. Alteration of NF-κB activity leads to mitochondrial apoptosis after infection with pathological prion protein. Cell. Microbiol. 9, 2202–2217 (2007).
Julius, C. et al. Prion propagation in mice lacking central nervous system NF-κB signalling. J. Gen. Virol. 89, 1545–1550 (2008).
Bremer, J. et al. Repetitive immunization enhances the susceptibility of mice to peripherally administered prions. PLoS ONE 4, e7160 (2009).
Michel, B. et al. Genetic depletion of complement receptors CD21/35 prevents terminal prion disease in a mouse model of chronic wasting disease. J. Immunol. 189, 4520–4527 (2012).
Sethi, S., Lipford, G., Wagner, H. & Kretzschmar, H. Postexposure prophylaxis against prion disease with a stimulator of innate immunity. Lancet 360, 229–230 (2002).
Heikenwalder, M. et al. Lymphoid follicle destruction and immunosuppression after repeated CpG oligodeoxynucleotide administration. Nature Med. 10, 187–192 (2004).
Gabizon, R., McKinley, M. P., Groth, D. & Prusiner, S. B. Immunoaffinity purification and neutralization of scrapie prion infectivity. Proc. Natl Acad. Sci. USA 85, 6617–6621 (1988).
Enari, M., Flechsig, E. & Weissmann, C. Scrapie prion protein accumulation by scrapie-infected neuroblastoma cells abrogated by exposure to a prion protein antibody. Proc. Natl Acad. Sci. USA 98, 9295–9299 (2001).
Peretz, D. et al. Antibodies inhibit prion propagation and clear cell cultures of prion infectivity. Nature 412, 739–743 (2001).
Schenk, D. et al. Immunization with amyloid-β attenuates Alzheimer-disease-like pathology in the PDAPP mouse. Nature 400, 173–177 (1999).
Heppner, F. L. et al. Prevention of scrapie pathogenesis by transgenic expression of anti-prion protein antibodies. Science 294, 178–182 (2001). This study shows for the first time PrP-specific antibody-mediated immunotherapy for prion disease in vivo.
Souan, L. et al. Modulation of proteinase-K resistant prion protein by prion peptide immunization. Eur. J. Immunol. 31, 2338–2346 (2001).
Sigurdsson, E. M. et al. Immunization delays the onset of prion disease in mice. Am. J. Pathol. 161, 13–17 (2002).
Polymenidou, M. et al. Humoral immune response to native eukaryotic prion protein correlates with anti-prion protection. Proc. Natl Acad. Sci. USA 101 (Suppl. 2), 14670–14676 (2004).
Xanthopoulos, K. et al. Immunization with recombinant prion protein leads to partial protection in a murine model of TSEs through a novel mechanism. PLoS ONE 8, e59143 (2013).
Fernandez-Borges, N. et al. DNA vaccination can break immunological tolerance to PrP in wild-type mice and attenuates prion disease after intracerebral challenge. J. Virol. 80, 9970–9976 (2006).
White, A. R. et al. Monoclonal antibodies inhibit prion replication and delay the development of prion disease. Nature 422, 80–83 (2003). This study describes the immunotherapy of prion disease by passive administration of PrP-specific antibodies.
Sigurdsson, E. M. et al. Anti-prion antibodies for prophylaxis following prion exposure in mice. Neurosci. Lett. 336, 185–187 (2003).
Sadowski, M. J. et al. Anti-PrP Mab 6D11 suppresses PrPSc replication in prion infected myeloid precursor line FDC-P1/22L and in the lymphoreticular system in vivo. Neurobiol. Dis. 34, 267–278 (2009).
Petsch, B. et al. Biological effects and use of PrPSc- and PrP-specific antibodies generated by immunization with purified full-length native mouse prions. J. Virol. 85, 4538–4546 (2011).
Lefebvre-Roque, M. et al. Toxic effects of intracerebral PrP antibody administration during the course of BSE infection in mice. Prion 1, 198–206 (2007).
Wuertzer, C. A., Sullivan, M. A., Qiu, X. & Federoff, H. J. CNS delivery of vectored prion-specific single-chain antibodies delays disease onset. Mol. Ther. 16, 481–486 (2008).
Solforosi, L. et al. Cross-linking cellular prion protein triggers neuronal apoptosis in vivo. Science 303, 1514–1516 (2004).
Sonati, T. et al. The toxicity of antiprion antibodies is mediated by the flexible tail of the prion protein. Nature 501, 102–106 (2013). References 153 and 154 report the neurotoxicity of certain PrP-specific antibodies and investigate the mechanisms that cause this neurotoxicity.
Mackay, F. & Browning, J. L. Turning off follicular dendritic cells. Nature 395, 26–27 (1998).
Meier, P. et al. Soluble dimeric prion protein binds PrPScin vivo and antagonizes prion disease. Cell 113, 49–60 (2003).
Moore, R. C. et al. Mice with gene targetted prion protein alterations show that Prnp, Sinc and Prni are congruent. Nature Genet. 18, 118–125 (1998).
Bueler, H. et al. High prion and PrPSc levels but delayed onset of disease in scrapie-inoculated mice heterozygous for a disrupted PrP gene. Mol. Med. 1, 19–30 (1994).
Sakaguchi, S. et al. Loss of cerebellar Purkinje cells in aged mice homozygous for a disrupted PrP gene. Nature 380, 528–531 (1996).
Moore, R. C. et al. Ataxia in prion protein (PrP)-deficient mice is associated with upregulation of the novel PrP-like protein doppel. J. Mol. Biol. 292, 797–817 (1999).
Mallucci, G. et al. Depleting neuronal PrP in prion infection prevents disease and reverses spongiosis. Science 302, 871–874 (2003).
Prusiner, S. B. et al. Transgenetic studies implicate interactions between homologous PrP isoforms in scrapie prion replication. Cell 63, 673–686 (1990).
Fischer, M. et al. Prion protein (PrP) with amino-proximal deletions restoring susceptibility of PrP knockout mice to scrapie. EMBO J. 15, 1255–1264 (1996).
Scott, M. et al. Transgenic mice expressing hamster prion protein produce species-specific scrapie infectivity and amyloid plaques. Cell 59, 847–857 (1989).
Telling, G. C. et al. Prion propagation in mice expressing human and chimeric PrP transgenes implicates the interaction of cellular PrP with another protein. Cell 83, 79–90 (1995).
Shmerling, D. et al. Expression of amino-terminally truncated PrP in the mouse leading to ataxia and specific cerebellar lesions. Cell 93, 203–214 (1998).
Sigurdson, C. J. et al. De novo generation of a transmissible spongiform encephalopathy by mouse transgenesis. Proc. Natl Acad. Sci. USA 106, 304–309 (2009).
Lauren, J., Gimbel, D. A., Nygaard, H. B., Gilbert, J. W. & Strittmatter, S. M. Cellular prion protein mediates impairment of synaptic plasticity by amyloid-β oligomers. Nature 457, 1128–1132 (2009). This paper claims that PrPC is a high-affinity receptor of amyloid-β oligomers and mediates their toxic effects. This finding is highly controversial.
Larson, M. et al. The complex PrPC-Fyn couples human oligomeric Aβ with pathological tau changes in Alzheimer's disease. J. Neurosci. 32, 16857–16871 (2012).
Gimbel, D. A. et al. Memory impairment in transgenic Alzheimer mice requires cellular prion protein. J. Neurosci. 30, 6367–6374 (2010).
Um, J. W. et al. Alzheimer amyloid-β oligomer bound to postsynaptic prion protein activates Fyn to impair neurons. Nature Neurosci. 15, 1227–1235 (2012).
Balducci, C. et al. Synthetic amyloid-β oligomers impair long-term memory independently of cellular prion protein. Proc. Natl Acad. Sci. USA 107, 2295–2300 (2010).
Calella, A. M. et al. Prion protein and Aβ-related synaptic toxicity impairment. EMBO Mol. Med. 2, 306–314 (2010).
Kessels, H. W., Nguyen, L. N., Nabavi, S. & Malinow, R. The prion protein as a receptor for amyloid-β. Nature 466, E3–E4 (2010).
Alzualde, A. et al. Somatic mosaicism in a case of apparently sporadic Creutzfeldt–Jakob disease carrying a de novo D178N mutation in the PRNP gene. Am. J. Med. Genet. B Neuropsychiatr. Genet. 153B, 1283–1291 (2010).
Schwarz, A. et al. Immunisation with a synthetic prion protein-derived peptide prolongs survival times of mice orally exposed to the scrapie agent. Neurosci. Lett. 350, 187–189 (2003).
Goni, F. et al. High titers of mucosal and systemic anti-PrP antibodies abrogate oral prion infection in mucosal-vaccinated mice. Neuroscience 153, 679–686 (2008).
Bade, S., Baier, M., Boetel, T. & Frey, A. Intranasal immunization of Balb/c mice against prion protein attenuates orally acquired transmissible spongiform encephalopathy. Vaccine 24, 1242–1253 (2006).
Pilon, J. et al. Anti-prion activity generated by a novel vaccine formulation. Neurosci. Lett. 429, 161–164 (2007).
Ishibashi, D. et al. Immunization with recombinant bovine but not mouse prion protein delays the onset of disease in mice inoculated with a mouse-adapted prion. Vaccine 25, 985–992 (2007).
Nitschke, C. et al. Immunisation strategies against prion diseases: prime-boost immunisation with a PrP DNA vaccine containing foreign helper T-cell epitopes does not prevent mouse scrapie. Vet. Microbiol. 123, 367–376 (2007).
Sacquin, A., Bergot, A. S., Aucouturier, P. & Bruley-Rosset, M. Contribution of antibody and T cell-specific responses to the progression of 139A-scrapie in C57BL/6 mice immunized with prion protein peptides. J. Immunol. 181, 768–775 (2008).
Tayebi, M., Collinge, J. & Hawke, S. Unswitched immunoglobulin M response prolongs mouse survival in prion disease. J. Gen. Virol. 90, 777–782 (2009).
Rosset, M. B. et al. Dendritic cell-mediated-immunization with xenogenic PrP and adenoviral vectors breaks tolerance and prolongs mice survival against experimental scrapie. PLoS ONE 4, e4917 (2009).
Bachy, V. et al. Mouse vaccination with dendritic cells loaded with prion protein peptides overcomes tolerance and delays scrapie. J. Gen. Virol. 91, 809–820 (2010).
Ishibashi, D. et al. Antigenic mimicry-mediated anti-prion effects induced by bacterial enzyme succinylarginine dihydrolase in mice. Vaccine 29, 9321–9328 (2011).
Roettger, Y. et al. Immunotherapy in prion disease. Nature Rev. Neurol. 9, 98–105 (2013).
Acknowledgements
We apologize to all those colleagues whose work was discussed without proper quotation owing to space constraints. We thank T. P. Johnson for critically reading our manuscript. A.A. is the recipient of an Advanced Grant of the European Research Council and is supported by grants from the European Union (PRIORITY and NEURINOX), the Swiss National Foundation, the Foundation Alliance BioSecure, the Novartis Research Foundation and the Clinical Research Priority Program (KFSP) of the University of Zurich, Switzerland. M.N. received grants from Collegio Ghislieri (Pavia, Italy) and the Foundation for Research at the Medical Faculty of the University of Zurich.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
FURTHER INFORMATION
Glossary
- Protein-only hypothesis
-
Introduced by Griffith and formally enunciated by Prusiner, it states that prions are unconventional infectious agents that are devoid of informational nucleic acids and that uniquely consist of an infectious, pathogenic protein.
- Prion
-
The aetiological agent of prion disease; prion is short for proteinaceous infectious particle.
- Scrapie prion protein
-
(PrPSc). The pathological version of prion protein that is present in the central nervous system and other tissues of patients with transmissible spongiform encephalopathies. It is believed to differ from cellular PrP only in terms of post-translational modifications.
- Cellular prion protein
-
(PrPC). The physiological version of prion protein, which is present in the central nervous system and other tissues under normal circumstances.
- Prion diseases
-
Also known as transmissible spongiform encephalopathies (TSEs). These are a group of transmissible neurodegenerative diseases that affect humans and various mammals.
- Prion strains
-
Natural sources or isolates of prions that, when inoculated into genetically homogeneous hosts, induce a prion disease with peculiar clinical, histological and biochemical features.
- Propagons
-
Proteinaceous aggregates that are capable of seeding a self-perpetuating reaction of templated nucleation within a biological system. Propagons are not necessarily identical to scrapie prion proteins but might represent a subset of prion protein conformations, some of which might not be resistant to proteolysis. Propagons could, in principle, have specific post-translational modifications.
- Prionoids
-
Self-aggregating proteins that are capable of transmitting between cells within one organism, but not from one organism to another. Amyloid-β, tau, huntingtin and amyloid A protein are examples of prionoids. Synuclein was thought to be a prionoid, but recent evidence suggests that it might behave like a bona fide prion.
- Follicular dendritic cells
-
(FDCs). Stromal cells derived from platelet-derived growth factor receptor-β (PDGFR)+ perivascular precursors and localized in lymphoid follicles. FDCs trap and retain immune complexes to stimulate an immune response. FDCs also express milk fat globule epidermal growth factor 8 (MFGE8) to facilitate the removal of apoptotic cells in secondary lymphoid organs.
- Mastitis
-
Inflammation occurring in the mammary gland. It can be caused by infection or by blockage of milk ducts.
- M2 phenotype
-
Activated macrophages or microglia that show phagocytic behaviour and express factors such as interleukin-4 (IL-4), IL-10 and arginase 1.
- M1 phenotype
-
Activated macrophages or microglia that show pro-inflammatory features and express factors such as interleukin-1β, tumour necrosis factor and inducible nitric oxide synthase.
Rights and permissions
About this article
Cite this article
Aguzzi, A., Nuvolone, M. & Zhu, C. The immunobiology of prion diseases. Nat Rev Immunol 13, 888–902 (2013). https://doi.org/10.1038/nri3553
Published:
Issue Date:
DOI: https://doi.org/10.1038/nri3553