Key Points
-
Specific effector and regulatory players have a role in ineffective immunity and the dysregulation of inflammation in diseases that affect newborns and infants.
-
To better understand the infections and diseases that affect newborns, host–microorganism interactions should be investigated in the context of age-specific immune regulation.
-
Disruption of the delicate balance between hypo- and hyperinflammation in the context of infection can lead rapidly to life-threatening clinical situations, highlighting the need to better understand mechanisms of inflammation in early life.
-
Many regulatory cell types — including regulatory T cells, regulatory B cells and myeloid-derived suppressor cells — are implicated in the control of inflammation, but they limit immunity to infection in newborns to permit safe development of the fetus and to allow colonization of the commensal microbiota to be tolerated.
-
In the absence of any infection, transplacental antigen transfer occurs during pregnancy, and this can lead to in utero priming of fetal T cells in response to allergens or vaccines.
-
The perinatal environment supports type 2 immune responses to favour vital functions and tissue homeostasis and remodelling; however, this response can be reshaped in vivo (for example, by vaccination).
Abstract
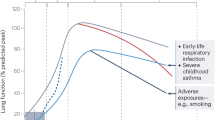
The early stages of life are associated with increased susceptibility to infection, which is in part due to an ineffective immune system. In the context of infection, the immune system must be stimulated to provide efficient protection while avoiding insufficient or excessive activation. Yet, in early life, age-dependent immune regulation at molecular and cellular levels contributes to a reduced immunological fitness in terms of pathogen clearance and response to vaccines. To enable microbial colonization to be tolerated at birth, epigenetic immune cell programming and early life-specific immune regulatory and effector mechanisms ensure that vital functions and organ development are supported and that tissue damage is avoided. Advancement in our understanding of age-related remodelling of immune networks and the consequent tuning of immune responsiveness will open up new possibilities for immune intervention and vaccine strategies that are designed specifically for early life.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
PrabhuDas, M. et al. Challenges in infant immunity: implications for responses to infection and vaccines. Nat. Immunol. 12, 189–194 (2011).
PrabhuDas, M. et al. Immune mechanisms at the maternal–fetal interface: perspectives and challenges. Nat. Immunol. 16, 328–334 (2015).
Marrack, P., McKee, A. S. & Munks, M. W. Towards an understanding of the adjuvant action of aluminium. Nat. Rev. Immunol. 9, 287–293 (2009).
Ivanovs, A. et al. Highly potent human hematopoietic stem cells first emerge in the intraembryonic aorta–gonad–mesonephros region. J. Exp. Med. 208, 2417–2427 (2011). This study identified HSC potency in the AGM region of human embryos by transfer into immunodeficient mice.
Charbord, P. et al. Early ontogeny of the human hematopoietic system [in French]. C. R. Seances Soc. Biol. Fil. 189, 601–609 (1995).
Christensen, R. D. Hematopoiesis in the fetus and neonate. Pediatr. Res. 26, 531–532 (1989).
Holt, P. G. & Jones, C. A. The development of the immune system during pregnancy and early life. Allergy 55, 688–697 (2000).
Migliaccio, G. et al. Human embryonic hemopoiesis. Kinetics of progenitors and precursors underlying the yolk sac–liver transition. J. Clin. Invest. 78, 51–60 (1986).
Mold, J. E. & McCune, J. M. Immunological tolerance during fetal development: from mouse to man. Adv. Immunol. 115, 73–111 (2012).
De Kleer, I., Willems, F., Lambrecht, B. & Goriely, S. Ontogeny of myeloid cells. Front. Immunol. 5, 423 (2014).
Ohls, R. K. et al. Neutrophil pool sizes and granulocyte colony-stimulating factor production in human mid-trimester fetuses. Pediatr. Res. 37, 806–811 (1995).
Haynes, B. F. & Heinly, C. S. Early human T cell development: analysis of the human thymus at the time of initial entry of hematopoietic stem cells into the fetal thymic microenvironment. J. Exp. Med. 181, 1445–1458 (1995).
Lobach, D. F., Hensley, L. L., Ho, W. & Haynes, B. F. Human T cell antigen expression during the early stages of fetal thymic maturation. J. Immunol. 135, 1752–1759 (1985).
Haynes, B. F. & Hale, L. P. The human thymus. A chimeric organ comprised of central and peripheral lymphoid components. Immunol. Res. 18, 175–192 (1998).
Millet, V. et al. Development of the newborn immune system. (in French) Arch. Pediatr. 6 (Suppl. 1), 14S–19S (1999).
Namikawa, R. et al. Ontogenic development of T and B cells and non-lymphoid cells in the white pulp of human spleen. Immunology 57, 61–69 (1986).
Timens, W., Rozeboom, T. & Poppema, S. Fetal and neonatal development of human spleen: an immunohistological study. Immunology 60, 603–609 (1987).
Cupedo, T., Nagasawa, M., Weijer, K., Blom, B. & Spits, H. Development and activation of regulatory T cells in the human fetus. Eur. J. Immunol. 35, 383–390 (2005).
Jebbawi, F. et al. A microRNA profile of human CD8+ regulatory T cells and characterization of the effects of microRNAs on Treg cell-associated genes. J. Transl Med. 12, 218 (2014).
Mold, J. E. et al. Fetal and adult hematopoietic stem cells give rise to distinct T cell lineages in humans. Science 330, 1695–1699 (2010).
Mold, J. E. et al. Maternal alloantigens promote the development of tolerogenic fetal regulatory T cells in utero. Science 322, 1562–1565 (2008).
Michaelsson, J., Mold, J. E., McCune, J. M. & Nixon, D. F. Regulation of T cell responses in the developing human fetus. J. Immunol. 176, 5741–5748 (2006).
Byrne, J. A., Stankovic, A. K. & Cooper, M. D. A novel subpopulation of primed T cells in the human fetus. J. Immunol. 152, 3098–3106 (1994).
Bunders, M. J. et al. Memory CD4+CCR5+ T cells are abundantly present in the gut of newborn infants to facilitate mother-to-child transmission of HIV-1. Blood 120, 4383–4390 (2012).
Schuster, C. et al. Phenotypic characterization of leukocytes in prenatal human dermis. J. Invest. Dermatol. 132, 2581–2592 (2012).
Hazenberg, M. D. & Spits, H. Human innate lymphoid cells. Blood 124, 700–709 (2014).
Forsberg, A. et al. GATA binding protein 3+ group 2 innate lymphoid cells are present in cord blood and in higher proportions in male than in female neonates. J. Allergy Clin. Immunol. 134, 228–230 (2014).
Cohen, C. et al. Epidemiology of viral-associated acute lower respiratory tract infection among children <5 years of age in a high HIV prevalence setting, South Africa, 2009–2012. Pediatr. Infect. Dis. J. 34, 66–72 (2015).
Saravia, J. et al. Respiratory syncytial virus disease is mediated by age-variable IL-33. PLoS Pathog. 11, e1005217 (2015).
De Rosa, S. C. et al. Ontogeny of gamma delta T cells in humans. J. Immunol. 172, 1637–1645 (2004).
Vermijlen, D. & Prinz, I. Ontogeny of innate T lymphocytes — some innate lymphocytes are more innate than others. Front. Immunol. 5, 486 (2014).
Leeansyah, E., Loh, L., Nixon, D. F. & Sandberg, J. K. Acquisition of innate-like microbial reactivity in mucosal tissues during human fetal MAIT-cell development. Nat. Commun. 5, 3143 (2014).
Griffin, D. O., Holodick, N. E. & Rothstein, T. L. Human B1 cells in umbilical cord and adult peripheral blood express the novel phenotype CD20+ CD27+ CD43+ CD70-. J. Exp. Med. 208, 67–80 (2011).
Weill, J.-C., Weller, S. & Reynaud, C.-A. Human marginal zone B cells. Ann. Rev. Immunol. 27, 267–285 (2009).
Iwasaki, A. & Medzhitov, R. Control of adaptive immunity by the innate immune system. Nat. Immunol. 16, 343–353 (2015).
Kollmann, T. R., Levy, O., Montgomery, R. R. & Goriely, S. Innate immune function by Toll-like receptors: distinct responses in newborns and the elderly. Immunity 37, 771–783 (2012).
Upham, J. W. et al. Development of interleukin-12-producing capacity throughout childhood. Infect. Immun. 70, 6583–6588 (2002). This study was the first to describe age-dependent maturation of the IL-12 response following TLR4 stimulation of human blood.
Goriely, S. et al. A defect in nucleosome remodeling prevents IL-12(p35) gene transcription in neonatal dendritic cells. J. Exp. Med. 199, 1011–1016 (2004). This study showed epigenetic regulation of the IL12 locus in DCs derived from neonatal monocytes.
Aksoy, E. et al. Interferon regulatory factor 3-dependent responses to lipopolysaccharide are selectively blunted in cord blood cells. Blood 109, 2887–2893 (2007).
Kollmann, T. R. et al. Neonatal innate TLR-mediated responses are distinct from those of adults. J. Immunol. 183, 7150–7160 (2009).
Renneson, J. et al. IL-12 and type I IFN response of neonatal myeloid DC to human CMV infection. Eur. J. Immunol. 39, 2789–2799 (2009).
Belderbos, M. E. et al. Skewed pattern of Toll-like receptor 4-mediated cytokine production in human neonatal blood: low LPS-induced IL-12p70 and high IL-10 persist throughout the first month of life. Clin. Immunol. 133, 228–237 (2009).
Dirix, V. et al. Monocyte-derived interleukin-10 depresses the Bordetella pertussis-specific gamma interferon response in vaccinated infants. Clin. Vaccine Immunol. 16, 1816–1821 (2009).
Philbin, V. J. et al. Imidazoquinoline Toll-like receptor 8 agonists activate human newborn monocytes and dendritic cells through adenosine-refractory and caspase-1-dependent pathways. J. Allergy Clin. Immunol. 130, 195–204.e9 (2012).
Chassin, C. et al. miR-146a mediates protective innate immune tolerance in the neonate intestine. Cell Host Microbe 8, 358–368 (2010).
Lotz, M. et al. Postnatal acquisition of endotoxin tolerance in intestinal epithelial cells. J. Exp. Med. 203, 973–984 (2006). In references 45 and 46, the authors identified a mechanism of LPS tolerance that occurs in the intestine of neonatal mice during the first few hours after birth and allows commensal colonization.
Gill, M. A. et al. Mobilization of plasmacytoid and myeloid dendritic cells to mucosal sites in children with respiratory syncytial virus and other viral respiratory infections. J. Infect. Dis. 191, 1105–1115 (2005).
De Wit, D. et al. Blood plasmacytoid dendritic cell responses to CpG oligodeoxynucleotides are impaired in human newborns. Blood 103, 1030–1032 (2004).
Danis, B. et al. Interferon regulatory factor 7-mediated responses are defective in cord blood plasmacytoid dendritic cells. Eur. J. Immunol. 38, 507–517 (2008).
Marr, N. et al. Attenuation of respiratory syncytial virus-induced and RIG-I-dependent type I IFN responses in human neonates and very young children. J. Immunol. 192, 948–957 (2014).
Zhivaki, D. et al. Respiratory syncitial virus infects regulatory B cells in human neonates via chemokine receptor CX3CR1 and promotes lung disease severity. Immunity 46, 301–314 (2017). This study identified a B reg cell population that is specific to newborns and that is targeted by RSV to impair viral clearance. The presence of this population might be used as a biomarker to predict disease severity.
Zhang, X. et al. Neonatal plasmacytoid dendritic cells (pDCs) display subset variation but can elicit potent anti-viral innate responses. PLoS ONE 8, e52003 (2013).
Zhang, X. et al. Plasmacytoid dendritic cells engagement by influenza vaccine as a surrogate strategy for driving T-helper type 1 responses in human neonatal settings. J. Infect. Dis. 210, 424–434 (2014).
Remot, A. et al. Flt3 ligand improves the innate response to respiratory syncytial virus and limits lung disease upon RSV reexposure in neonate mice. Eur. J. Immunol. 46, 874–884 (2016).
Vollstedt, S. et al. Flt3 ligand-treated neonatal mice have increased innate immunity against intracellular pathogens and efficiently control virus infections. J. Exp. Med. 197, 575–584 (2003). These authors showed how boosting DC production in neonatal mice by administration of FLT3L can confer protection to a number of infections.
Vollstedt, S. et al. Treatment of neonatal mice with Flt3 ligand leads to changes in dendritic cell subpopulations associated with enhanced IL-12 and IFN-alpha production. Eur. J. Immunol. 34, 1849–1860 (2004).
Sun, C.-M., Fiette, L., Tanguy, M., Leclerc, C. & Lo-Man, R. Ontogeny and innate properties of neonatal dendritic cells. Blood 102, 585–591 (2003).
Dadaglio, G., Sun, C. M., Lo-Man, R., Siegrist, C. A. & Leclerc, C. Efficient in vivo priming of specific cytotoxic T cell responses by neonatal dendritic cells. J. Immunol. 168, 2219–2224 (2002).
Galindo-Albarran, A. O. et al. CD8+ T cells from human neonates are biased toward an innate immune response. Cell Rep. 17, 2151–2160 (2016).
Chen, S. F. et al. Antiviral CD8 T cells in the control of primary human cytomegalovirus infection in early childhood. J. Infect. Dis. 189, 1619–1627 (2004).
Marchant, A. et al. Mature CD8+ T lymphocyte response to viral infection during fetal life. J. Clin. Invest. 111, 1747–1755 (2003).
Miles, D. J. et al. CD4+ T cell responses to cytomegalovirus in early life: a prospective birth cohort study. J. Infect. Dis. 197, 658–662 (2008).
Vermijlen, D. et al. Human cytomegalovirus elicits fetal gammadelta T cell responses in utero. J. Exp. Med. 207, 807–821 (2010).
Gibson, L. et al. Reduced frequencies of polyfunctional CMV-specific T cell responses in infants with congenital CMV infection. J. Clin. Immunol. 35, 289–301 (2015).
Huygens, A. et al. Functional exhaustion limits CD4+ and CD8+ T-cell responses to congenital cytomegalovirus infection. J. Infect. Dis. 212, 484–494 (2015).
Hermann, E. et al. Human fetuses are able to mount an adultlike CD8 T-cell response. Blood 100, 2153–2158 (2002).
Dauby, N., Goetghebuer, T., Kollmann, T. R., Levy, J. & Marchant, A. Uninfected but not unaffected: chronic maternal infections during pregnancy, fetal immunity, and susceptibility to postnatal infections. Lancet Infect. Dis. 12, 330–340 (2012). This is an exhaustive Review describing how infections during pregnancy without vertical transmission of the pathogen can affect the perinatal immune system.
Zhang, X. et al. CD4 T cells with effector memory phenotype and function develop in the sterile environment of the fetus. Sci. Transl Med. 6, 238ra72 (2014).
Sathaliyawala, T. et al. Distribution and compartmentalization of human circulating and tissue-resident memory T cell subsets. Immunity 38, 187–197 (2013).
Naik, S. et al. Compartmentalized control of skin immunity by resident commensals. Science 337, 1115–1119 (2012).
Birnbaum, M. E. et al. Deconstructing the peptide-MHC specificity of T cell recognition. Cell 157, 1073–1087 (2014).
Thome, J. J. et al. Early-life compartmentalization of human T cell differentiation and regulatory function in mucosal and lymphoid tissues. Nat. Med. 22, 72–77 (2016). This study was the first to characterize in detail the T cell compartment, including effector memory T cells, tissue-resident memory T cells and T reg cells, in paediatric tissues such as the lungs and intestine.
Hebel, K. et al. CD4+ T cells from human neonates and infants are poised spontaneously to run a nonclassical IL-4 program. J. Immunol. 192, 5160–5170 (2014).
Webster, R. B., Rodriguez, Y., Klimecki, W. T. & Vercelli, D. The human IL-13 locus in neonatal CD4+ T cells is refractory to the acquisition of a repressive chromatin architecture. J. Biol. Chem. 282, 700–709 (2007).
Siegrist, C. A. Neonatal and early life vaccinology. Vaccine 19, 3331–3346 (2001).
Marchant, A. et al. Newborns develop a Th1-type immune response to Mycobacterium bovis bacillus Calmette–Guérin vaccination. J. Immunol. 163, 2249–2255 (1999). This study demonstrated the induction of T H 1 cell responses following BCG vaccination.
Ota, M. O. et al. Influence of Mycobacterium bovis bacillus Calmette–Guerin on antibody and cytokine responses to human neonatal vaccination. J. Immunol. 168, 919–925 (2002).
Odegaard, J. I. et al. Perinatal licensing of thermogenesis by IL-33 and ST2. Cell 166, 841–854 (2016). This study showed how neonatal IL-33, a T H 2 cell-response-driving cytokine, is crucial to maintain vital body temperature following birth.
de Kleer, I. M. et al. Perinatal activation of the interleukin-33 pathway promotes type 2 immunity in the developing lung. Immunity 45, 1285–1298 (2016). This study showed how the mouse neonatal lung shapes DC functions for allergen–T H 2 cell priming through IL-33.
Mor, G., Aldo, P. & Alvero, A. B. The unique immunological and microbial aspects of pregnancy. Nat. Rev. Immunol. http://dx.doi.org/10.1038/nri.2017.64 (2017).
Erlebacher, A., Vencato, D., Price, K. A., Zhang, D. & Glimcher, L. H. Constraints in antigen presentation severely restrict T cell recognition of the allogeneic fetus. J. Clin. Invest. 117, 1399–1411 (2007).
Rowe, J. H., Ertelt, J. M., Xin, L. & Way, S. S. Regulatory T cells and the immune pathogenesis of prenatal infection. Reproduction 146, R191–R203 (2013).
Aluvihare, V. R., Kallikourdis, M. & Betz, A. G. Regulatory T cells mediate maternal tolerance to the fetus. Nat. Immunol. 5, 266–271 (2004).
Somerset, D. A., Zheng, Y., Kilby, M. D., Sansom, D. M. & Drayson, M. T. Normal human pregnancy is associated with an elevation in the immune suppressive CD25+ CD4+ regulatory T-cell subset. Immunology 112, 38–43 (2004).
Allenspach, E. J. et al. Absence of functional fetal regulatory T cells in humans causes in utero organ-specific autoimmunity. J. Allergy Clin. Immunol. http://dx.doi.org/10.1016/j.jaci.2017.02.017 (2017).
Elahi, S. et al. Immunosuppressive CD71+ erythroid cells compromise neonatal host defence against infection. Nature 504, 158–162 (2013). This study characterized the immunosuppressive properties of immature erythroid cells.
Wynn, J. L. et al. Neonatal CD71+ erythroid cells do not modify murine sepsis mortality. J. Immunol. 195, 1064–1070 (2015).
Pillay, J., Tak, T., Kamp, V. M. & Koenderman, L. Immune suppression by neutrophils and granulocytic myeloid-derived suppressor cells: similarities and differences. Cell. Mol. Life Sci. 70, 3813–3827 (2013).
Gervassi, A. et al. Myeloid derived suppressor cells are present at high frequency in neonates and suppress in vitro T cell responses. PLoS ONE 9, e107816 (2014).
Rieber, N. et al. Neutrophilic myeloid-derived suppressor cells in cord blood modulate innate and adaptive immune responses. Clin. Exp. Immunol. 174, 45–52 (2013).
Zhang, X., Majlessi, L., Deriaud, E., Leclerc, C. & Lo-Man, R. Coactivation of Syk kinase and MyD88 adaptor protein pathways by bacteria promotes regulatory properties of neutrophils. Immunity 31, 761–771 (2009). This study identified how regulatory neutrophils that produce IL-10 are mobilized in the context of mycobacterial infection in the lungs.
Sun, C. M., Deriaud, E., Leclerc, C. & Lo-Man, R. Upon TLR9 signaling CD5+ B cells control the IL-12-dependent Th1-priming capacity of neonatal DCs. Immunity 22, 467–477 (2005).
Zhang, X. et al. Type I interferons protect neonates from acute inflammation through interleukin 10- producing B cells. J. Exp. Med. 204, 1107–1118 (2007).
Mauri, C. & Bosma, A. Immune regulatory function of B cells. Ann. Rev. Immunol. 30, 221–241 (2012).
Pan, X., Ji, Z. & Xue, J. Percentage of peripheral CD19+CD24hiCD38hi regulatory B cells in neonatal sepsis patients and its functional implication. Med. Sci. Monit. 22, 2374–2378 (2016).
Sarvaria, A. et al. IL-10+ regulatory B cells are enriched in cord blood and may protect against cGVHD after cord blood transplantation. Blood 128, 1346–1361 (2016).
Shah, B. A. & Padbury, J. F. Neonatal sepsis: an old problem with new insights. Virulence 5, 170–178 (2014).
Davies, N. P. et al. Fetal leukocyte count in rhesus disease. Arch. Dis. Child. 67, 404–406 (1992).
Melvan, J. N., Bagby, G. J., Welsh, D. A., Nelson, S. & Zhang, P. Neonatal sepsis and neutrophil insufficiencies. Int. Rev. Immunol. 29, 315–348 (2010).
Bektas, S., Goetze, B. & Speer, C. Decreased adherence, chemotaxis and phagocytic activities of neutrophils from preterm neonates. Acta Paediatr. 79, 1031–1038 (1990).
Celik, I. H., Demirel, G., Erdeve, O. & Dilmen, U. Neutrophil volume, conductivity and scatter in neonatal sepsis. Pediatr. Infect. Dis. J. 32, 301 (2013).
Yost, C. C. et al. Impaired neutrophil extracellular trap (NET) formation: a novel innate immune deficiency of human neonates. Blood 113, 6419–6427 (2009).
Yost, C. C. et al. Neonatal NET-inhibitory factor and related peptides inhibit neutrophil extracellular trap formation. J. Clin. Invest. 126, 3783–3798 (2016). This study showed that cord blood NET formation is negatively regulated by NET-inhibitory factor and related peptides from neonatal plasma.
Deshmukh, H. S. et al. The microbiota regulates neutrophil homeostasis and host resistance to Escherichia coli K1 sepsis in neonatal mice. Nat. Med. 20, 528–534 (2014). This study showed that normal neonatal neutrophil development and function require the colonization of gut microbiota and IL-17 production by ILC3s.
Andrade, E. B. et al. TLR2-induced IL-10 production impairs neutrophil recruitment to infected tissues during neonatal bacterial sepsis. J. Immunol. 191, 4759–4768 (2013).
Sharma, A. A. et al. Impaired NLRP3 inflammasome activity during fetal development regulates IL-1 β production in human monocytes. Eur. J. Immunol. 45, 238–249 (2015).
Marchant, E. A. et al. Attenuated innate immune defenses in very premature neonates during the neonatal period. Pediatr. Res. 78, 492–497 (2015).
Krow-Lucal, E. R., Kim, C. C., Burt, T. D. & McCune, J. M. Distinct functional programming of human fetal and adult monocytes. Blood 123, 1897–1904 (2014).
Pedraza-Sanchez, S., Hise, A. G., Ramachandra, L., Arechavaleta-Velasco, F. & King, C. L. Reduced Frequency of a CD14+ CD16+ monocyte subset with high Toll-like receptor 4 expression in cord blood compared to adult blood contributes to lipopolysaccharide hyporesponsiveness in newborns. Clin. Vaccine Immunol. 20, 962–971 (2013).
Lissner, M. M. et al. Age-related gene expression differences in monocytes from human neonates, young adults, and older adults. PLoS ONE 10, e0132061 (2015).
Levy, O. et al. The adenosine system selectively inhibits TLR-mediated TNF-α production in the human newborn. J. Immunol. 177, 1956–1966 (2006).
Ulas, T. et al. S100-alarmin-induced innate immune programming protects newborn infants from sepsis. Nat. Immunol. http://dx.doi.org/10.1038/ni.3745 (2017).
Roger, T. et al. High expression levels of macrophage migration inhibitory factor sustain the innate immune responses of neonates. Proc. Natl Acad. Sci. USA 113, E997–E1005 (2016). This study showed that neonates have ten-fold higher levels of circulating pro-inflammatory MIF.
Azizia, M., Lloyd, J., Allen, M., Klein, N. & Peebles, D. Immune status in very preterm neonates. Pediatrics 129, E967–E974 (2012).
Genel, F., Atlihan, F., Ozsu, E. & Ozbek, E. Monocyte HLA-DR expression as predictor of poor outcome in neonates with late onset neonatal sepsis. J. Infect. 60, 224–228 (2010).
Lavoie, P. M. et al. Profound lack of interleukin (IL)-12/IL-23p40 in neonates born early in gestation is associated with an increased risk of sepsis. J. Infect. Dis. 202, 1754–1763 (2010).
Gibbons, D. et al. Interleukin-8 (CXCL8) production is a signatory T cell effector function of human newborn infants. Nat. Med. 20, 1206–1210 (2014). This study characterized inflammatory T cells that produce IL-8 as a major biological event in clinical cases of newborns suffering from necrotizing enterocolitis.
Hodge, G., Hodge, S., Han, P. & Haslam, R. Multiple leucocyte activation markers to detect neonatal infection. Clin. Exp. Immunol. 135, 125–129 (2004).
Pagel, J. et al. Regulatory T cell frequencies are increased in preterm infants with clinical early-onset sepsis. Clin. Exp. Immunol. 185, 219–227 (2016).
Reynolds, L. A. & Finlay, B. B. Early life factors that affect allergy development. Nat. Rev. Immunol. http://dx.doi.org/10.1038/nri.2017.39 (2017).
Holloway, J. A. et al. Detection of house-dust-mite allergen in amniotic fluid and umbilical-cord blood. Lancet 356, 1900–1902 (2000).
Edelbauer, M. et al. Maternally delivered nutritive allergens in cord blood and in placental tissue of term and preterm neonates. Clin. Exp. Allergy 34, 189–193 (2004).
Prescott, S. L. et al. Transplacental priming of the human immune system to environmental allergens: universal skewing of initial T cell responses toward the Th2 cytokine profile. J. Immunol. 160, 4730–4737 (1998).
Prescott, S. L. et al. Development of allergen-specific T-cell memory in atopic and normal children. Lancet 353, 196–200 (1999). This cohort study characterized in utero priming of allergen-specific T cells responsible for atopy in children.
Chen, J. C. et al. Fetal phagocytes take up allergens to initiate T-helper cell type 2 immunity and facilitate allergic airway responses. Am. J. Respir. Crit. Care Med. 194, 934–947 (2016).
Tulic, M. K. et al. Differences in innate immune function between allergic and nonallergic children: new insights into immune ontogeny. J. Allergy Clin. Immunol. 127, 470–478 (2011).
Zhang, Y. et al. Cord blood monocyte-derived inflammatory cytokines suppress IL-2 and induce nonclassic “TH2-type” immunity associated with development of food allergy. Sci. Transl Med. 8, 321ra8 (2016). This study showed that hyperinflammation can lead to a non-classical T H 2 cell response at birth.
Legg, J. P., Hussain, I. R., Warner, J. A., Johnston, S. L. & Warner, J. O. Type 1 and type 2 cytokine imbalance in acute respiratory syncytial virus bronchiolitis. Am. J. Respir. Crit. Care 168, 633–639 (2003).
Kristjansson, S. et al. Respiratory syncytial virus and other respiratory viruses during the first 3 months of life promote a local TH2-like response. J. Allergy Clin. Immun. 116, 805–811 (2005).
Thornburg, N. J., Shepherd, B. & Crowe, J. E. Transforming growth factor beta is a major regulator of human neonatal immune responses following respiratory syncytial virus infection. J. Virol. 84, 12895–12902 (2010).
Smith, M. et al. Children with egg allergy have evidence of reduced neonatal CD4+CD25+CD127lo/- regulatory T cell function. J. Allergy Clin. Immunol. 121, 1460–1466 (2008).
Schaub, B. et al. Impairment of T-regulatory cells in cord blood of atopic mothers. J. Allergy Clin. Immunol. 121, 1491–1499 (2008).
von Mutius, E. & Vercelli, D. Farm living: effects on childhood asthma and allergy. Nat. Rev. Immunol. 10, 861–868 (2010).
Schaub, B. et al. Maternal farm exposure modulates neonatal immune mechanisms through regulatory T cells. J. Allergy Clin. Immunol. 123, 774–782.e5 (2009).
MacPherson, A. J., Gomez de Aguero, M. & Ganal-Vonarburg, S. C. How nutrition and the maternal microbiota shape the neonatal immune system. Nat. Rev. Immunol. http://dx.doi.org/10.1038/nri.2017.58 (2017).
Logan, A. C., Jacka, F. N. & Prescott, S. L. Immune–microbiota interactions: dysbiosis as a global health issue. Curr. Allergy Asthma Rep. 16, 13 (2016).
Cahenzli, J., Koller, Y., Wyss, M., Geuking, M. B. & McCoy, K. D. Intestinal microbial diversity during early-life colonization shapes long-term IgE levels. Cell Host Microbe 14, 559–570 (2013).
Arrieta, M. C. et al. Early infancy microbial and metabolic alterations affect risk of childhood asthma. Sci. Transl Med. 7, 307ra152 (2015).
Fujimura, K. E. et al. Neonatal gut microbiota associates with childhood multisensitized atopy and T cell differentiation. Nat. Med. 22, 1187–1191 (2016). References 137–139 showed that gut microbial dysbiosis and an enrichment of pro-inflammatory metabolites are associated with T H 2-driven allergic responses.
Smith, P. M. et al. The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science 341, 569–573 (2013).
Furusawa, Y. et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature 504, 446–450 (2013).
Arpaia, N. et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature 504, 451–455 (2013).
Gollwitzer, E. S. et al. Lung microbiota promotes tolerance to allergens in neonates via PD-L1. Nat. Med. 20, 642–647 (2014).
Olotu, A. et al. Four-year efficacy of RTS,S/AS01E and its interaction with malaria exposure. N. Engl. J. Med. 368, 1111–1120 (2013).
Sancho, D. & Reis e Sousa, C. Signaling by myeloid C-type lectin receptors in immunity and homeostasis. Ann. Rev. Immunol. 30, 491–529 (2012).
Kamath, A. T. et al. A liposome-based mycobacterial vaccine induces potent adult and neonatal multifunctional T cells through the exquisite targeting of dendritic cells. PLoS ONE 4, e5771 (2009).
Lemoine, S. et al. Dectin-1 activation unlocks IL12A expression and reveals the TH1 potency of neonatal dendritic cells. J. Allergy Clin. Immunol. 136, 1355–1368.e15 (2015).
Torres, D. et al. IL-12p40/IL-10 producing preCD8alpha/Clec9A+ dendritic cells are induced in neonates upon Listeria monocytogenes infection. PLoS Pathog. 12, e1005561 (2016).
Nakaya, H. I. et al. Systems biology of immunity to MF59-adjuvanted versus nonadjuvanted trivalent seasonal influenza vaccines in early childhood. Proc. Natl Acad. Sci. USA 113, 1853–1858 (2016).
Graham, B. S. Biological challenges and technological opportunities for respiratory syncytial virus vaccine development. Immunol. Rev. 239, 149–166 (2011).
Rastogi, D. et al. Antigen-specific immune responses to influenza vaccine in utero. J. Clin. Invest. 117, 1637–1646 (2007).
Kapikian, A. Z., Mitchell, R. H., Chanock, R. M., Shvedoff, R. A. & Stewart, C. E. An epidemiologic study of altered clinical reactivity to respiratory syncytial (RS) virus infection in children previously vaccinated with an inactivated RS virus vaccine. Am. J. Epidemiol. 89, 405–421 (1969).
Acknowledgements
R.L.-M. and D.Z. are supported by an ANR grant (ANR 13-BSV3-0016) and by the Fondation pour la Recherche Médicale (grant number DEQ20120323719). R.L.-M. received funding from the French Government's Investissement d'Avenir program, Laboratoire d'Excellence 'Integrative Biology of Emerging Infectious Diseases' (grant number ANR-10-LABX-62-IBEID). X.Z. is supported by the National Basic Research Program of China (grant number 2014CB541904); National Natural Science Foundation of China (grant numbers 31270961 and 31470879); Interdisciplinary Innovation Team, External Cooperation Program (grant number GJHZ201312) and Key Project QYZDB-SSW-SMC036, and the Strategic Priority Research Program (grant number XDPB0303), Chinese Academy of Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
- Group B streptococcus
-
(GBS; also known as Streptocococcus agalactiae). The major cause of neonatal sepsis, a severe infection that affects preterm neonates, leading to severe inflammation and organ failure. The bacterium is transmitted from the mother upon delivery and the immune system has a crucial role in the outcome and the pathophysiological consequences of this infection.
- Feto–maternal tolerance
-
Tolerance mechanisms that allow safe development of the fetus during pregnancy. They avoid fetal tissue rejection by the immune system of the mother and immune reactivity against non-inherited maternal antigens by the immune system of the fetus.
- Innate lymphoid cells
-
(ILCs). Lymphoid cells derived from the common lymphoid progenitor that lack expression of an antigen receptor. ILCs have important roles in lymphoid tissue formation and homeostasis and also in linking innate and adaptive immune responses through effects on T helper cell polarization.
- γδ T cells
-
T cells that express a T cell receptor consisting of a γ-chain and a δ-chain. These T cells are present in the intestinal epithelium as intraepithelial lymphocytes. γδ T cells are also present in the lungs, skin, liver and other tissue sites during inflammation. γδ T cells are thought to have an important role in innate immune responses.
- Mucosa-associated invariant T cells
-
(MAIT cells). A population of innate-like lymphocytes that express an evolutionarily conserved invariant T cell receptor and are selected by the MHC class I-related molecule MR1. They are abundant in human blood, in the intestinal mucosa and in mesenteric lymph nodes, and can produce interferon-γ in response to various bacterial infections.
- Pre-B cell receptor
-
A receptor that is formed at the surface of pre-B cells by the pairing of rearranged immunoglobulin heavy chains with surrogate light chains and the heterodimer of Igα and Igβ. Signalling by the pre-B cell receptor occurs in the absence of known ligands and is a crucial event in B cell development.
- Pattern-recognition receptors
-
(PRRs). Host receptors that can sense pathogen-associated molecular patterns and initiate signalling cascades that lead to an innate immune response. PRRs can be membrane bound (such as Toll-like receptors) or soluble cytoplasmic receptors (such as NOD-like receptors).
- Type I IFN
-
A family of cytokines that bind to the IFNα receptor (IFNAR) complex, which consists of IFNAR1 and IFNAR2 chains. The type I IFNs in humans are mainly IFNα, IFNβ and IFNλ and these IFNs mediate the inhibition of viral replication, activate natural killer cells and macrophages and increase antigen presentation to T cells during infections and during an immune response to tumour cells.
- Tissue-resident memory T cells
-
Non-recirculating memory T cells that persist long-term in epithelial barrier tissues, including the gastrointestinal tract, lungs, skin and reproductive tract. They provide rapid on-site immune protection against known pathogens in peripheral tissues.
- Immunodysregulation, polyendocrinopathy, enteropathy, X-linked syndrome
-
(IPEX syndrome). A disease caused by mutations in FOXP3 and characterized by refractory enteritis, autoimmune endocrinopathies (including type 1 diabetes), thyroiditis and allergy.
- C-type lectin receptor
-
(CLR). A large family of receptors that bind glycosylated ligands and have multiple functions, such as cell adhesion, endocytosis, target recognition by natural killer cells and dendritic cell activation, as well as antigen capture and presentation.
- Regulatory B cells
-
(Breg cells). Populations of B cells with immunosuppressive responses that control inflammation. These cells are most often associated with production of the immunosuppressive cytokine IL-10.
Rights and permissions
About this article
Cite this article
Zhang, X., Zhivaki, D. & Lo-Man, R. Unique aspects of the perinatal immune system. Nat Rev Immunol 17, 495–507 (2017). https://doi.org/10.1038/nri.2017.54
Published:
Issue Date:
DOI: https://doi.org/10.1038/nri.2017.54
This article is cited by
-
Epidemiology, risk factors, clinical presentation and complications of late-onset neonatal sepsis among preterm neonates in Cyprus: a prospective case-control study
BMC Pediatrics (2024)
-
Factors affecting the immunogenicity of influenza vaccines in human
BMC Infectious Diseases (2023)
-
Neonatal intensive care admission for term neonates and subsequent childhood mortality: a retrospective linkage study
BMC Medicine (2023)
-
IL6 suppresses vaccine responses in neonates by enhancing IL2 activity on T follicular helper cells
npj Vaccines (2023)
-
Gut microbiome immaturity and childhood acute lymphoblastic leukaemia
Nature Reviews Cancer (2023)