Key Points
-
Patient optimization of modifiable risk factors before abdominal surgery for Crohn's disease reduces perioperative complications including postoperative intra-abdominal septic complications
-
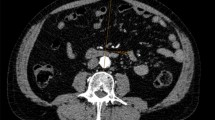
Cross-sectional imaging is required to define extent, severity and complications arising from penetrating Crohn's disease
-
Optimizing nutritional status before surgery reduces postoperative intra-abdominal septic complications and the need for a temporary diverting stoma
-
Preoperative treatment of abdominal abscesses or phlegmons substantially reduces all postoperative complications, the need for a temporary diverting stoma and increases the likelihood of a laparoscopic approach
-
Correction of preoperative anaemia reduces postoperative complications including intra-abdominal abscess, anastomosis leak and postoperative perforation
Abstract
The majority of patients with Crohn's disease require abdominal surgery during their lifetime, some of whom will require multiple operations. Postoperative complications are seen more frequently in patients requiring abdominal surgery for Crohn's disease than in patients requiring abdominal surgery for other conditions. In this article, we review the evidence supporting preoperative optimization, discussing strategies that potentially improve surgical outcomes and reduce perioperative morbidity and mortality. We discuss the roles of adequate cross-sectional imaging, nutritional optimization, appropriate adjustments of medical therapy, management of preoperative abscesses and phlegmons, smoking cessation and thromboembolic prophylaxis. We also review operation-related factors, and discuss their potential implications with respect to postoperative complications. Overall, the literature suggests that preoperative management has a major effect on postoperative outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Frolkis, A. D. et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology 145, 996–1006 (2013).
Bouguen, G. & Peyrin-Biroulet, L. Surgery for adult Crohn's disease: what is the actual risk? Gut 60, 1178–1181 (2011).
Caprilli, R. et al. European evidence based consensus on the diagnosis and management of Crohn's disease: special situations. Gut 55 (Suppl. 1), i36–i58 (2006).
Binder, V., Hendriksen, C. & Kreiner, S. Prognosis in Crohn's disease—based on results from a regional patient group from the county of Copenhagen. Gut 26, 146–150 (1985).
Goldberg, P. A., Wright, J. P., Gerber, M. & Claassen, R. Incidence of surgical resection for Crohn's disease. Dis. Colon Rectum 36, 736–739 (1993).
Masoomi, H. et al. Predictive factors of early bowel obstruction in colon and rectal surgery: data from the Nationwide Inpatient Sample, 2006–2008. J. Am. Coll. Surg. 214, 831–837 (2012).
Kirchhoff, P., Clavien, P. A. & Hahnloser, D. Complications in colorectal surgery: risk factors and preventive strategies. Patient Saf. Surg. 4, 5 (2010).
Bellolio, F. et al. Outcomes following surgery for perforating Crohn's disease. Br. J. Surg. 100, 1344–1348 (2013).
Bernstein, C. N., Nugent, Z., Targownik, L. E., Singh, H. & Lix, L. M. Predictors and risks for death in a population-based study of persons with IBD in Manitoba. Gut 64, 1403–1411 (2015).
Khoury, W., Strong, S. A., Fazio, V. W. & Kiran, R. P. Factors associated with operative recurrence early after resection for Crohn's disease. J. Gastrointest. Surg. 15, 1354–1360 (2011).
Yang, S. S. et al. Risk factors for complications after bowel surgery in Korean patients with Crohn's disease. J. Korean Surg. Soc. 83, 141–148 (2012).
Zerbib, P. et al. Pre-operative management is associated with low rate of post-operative morbidity in penetrating Crohn's disease. Aliment. Pharmacol. Ther. 32, 459–465 (2010).
Jacobson, S. Early postoperative complications in patients with Crohn's disease given and not given preoperative total parenteral nutrition. Scand. J. Gastroenterol. 47, 170–177 (2012).
Calabrese, E. et al. Bowel ultrasonography in the management of Crohn's disease. A review with recommendations of an international panel of experts. Inflamm. Bowel Dis. 22, 1168–1183 (2016).
Chatu, S., Subramanian, V. & Pollok, R. C. Meta-analysis: diagnostic medical radiation exposure in inflammatory bowel disease. Aliment. Pharmacol. Ther. 35, 529–539 (2012).
Chiorean, M. V. et al. Correlation of CT enteroclysis with surgical pathology in Crohn's disease. Am. J. Gastroenterol. 102, 2541–2550 (2007).
Punwani, S. et al. Mural inflammation in Crohn disease: location-matched histologic validation of MR imaging features. Radiology 252, 712–720 (2009).
Gourtsoyiannis, N. C., Papanikolaou, N. & Karantanas, A. Magnetic resonance imaging evaluation of small intestinal Crohn's disease. Best Pract. Res. Clin. Gastroenterol. 20, 137–156 (2006).
Menys, A. et al. Quantified terminal ileal motility during MR enterography as a potential biomarker of Crohn's disease activity: a preliminary study. Eur. Radiol. 22, 2494–2501 (2012).
Qi, F. et al. Utility of the diffusion-weighted imaging for activity evaluation in Crohn's disease patients underwent magnetic resonance enterography. BMC Gastroenterol. 15, 12 (2015).
Griffin, N., Grant, L. A., Anderson, S., Irving, P. & Sanderson, J. Small bowel MR enterography: problem solving in Crohn's disease. Insights Imaging 3, 251–263 (2012).
Bouhnik, Y. et al. 287 efficacy of adalimumab in patients with Crohn's disease and symptomatic small bowel stricture: a multicentre, prospective, observational cohort study (CREOLE). Gastroenterology 148 (Suppl. 1), S-62 (2015).
Rimola, J. et al. Characterization of inflammation and fibrosis in Crohn's disease lesions by magnetic resonance imaging. Am. J. Gastroenterol. 110, 432–440 (2015).
Horsthuis, K., Bipat, S., Bennink, R. J. & Stoker, J. Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: meta-analysis of prospective studies. Radiology 247, 64–79 (2008).
Qiu, Y. et al. Systematic review with meta-analysis: magnetic resonance enterography versus computed tomography enterography for evaluating disease activity in small bowel Crohn's disease. Aliment. Pharmacol. Ther. 40, 134–146 (2014).
Seastedt, K. P. et al. Accuracy of CT enterography and magnetic resonance enterography imaging to detect lesions preoperatively in patients undergoing surgery for Crohn's disease. Dis. Colon Rectum 57, 1364–1370 (2014).
Studley, H. O. Percentage of weight loss. A basic indicator of surgical risk in patients with chronic peptic ulcer. JAMA 106, 458–460 (1936).
White, J. V. et al. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). JPEN J. Parenter. Enteral Nutr. 36, 275–283 (2012).
Lindor, K. D., Fleming, C. R. & Ilstrup, D. M. Preoperative nutritional status and other factors that influence surgical outcome in patients with Crohn's disease. Mayo Clin. Proc. 60, 393–396 (1985).
Lochs, H. et al. ESPEN guidelines on enteral nutrition: gastroenterology. Clin. Nutr. 25, 260–274 (2006).
Donnellan, C. F., Yann, L. H. & Lal, S. Nutritional management of Crohn's disease. Therap. Adv. Gastroenterol. 6, 231–242 (2013).
Skowronska-Piekarska, U., Matysiak, K. & Sowinska, A. The impact of the nutritional state of patients on the results of the surgical treatment of Crohn's disease. Pol. Przegl. Chir. 85, 361–370 (2013).
Bozzetti, F., Gianotti, L., Braga, M., Di Carlo, V. & Mariani, L. Postoperative complications in gastrointestinal cancer patients: the joint role of the nutritional status and the nutritional support. Clin. Nutr. 26, 698–709 (2007).
Li, G. et al. Preoperative exclusive enteral nutrition reduces the postoperative septic complications of fistulizing Crohn's disease. Eur. J. Clin. Nutr. 68, 441–446 (2014).
Lashner, B. A., Evans, A. A. & Hanauer, S. B. Preoperative total parenteral nutrition for bowel resection in Crohn's disease. Dig. Dis. Sci. 34, 741–746 (1989).
Gibbs, J. et al. Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the National VA Surgical Risk Study. Arch. Surg. 134, 36–42 (1999).
Haupt, W., Holzheimer, R. G., Riese, J., Klein, P. & Hohenberger, W. Association of low preoperative serum albumin concentrations and the acute phase response. Eur. J. Surg. 165, 307–313 (1999).
Huang, W., Tang, Y., Nong, L. & Sun, Y. Risk factors for postoperative intra-abdominal septic complications after surgery in Crohn's disease: a meta-analysis of observational studies. J. Crohns Colitis 9, 293–301 (2015).
Morar, P. S. et al. Determining predictors for intra-abdominal septic complications following ileocolonic resection for Crohn's disease-considerations in pre-operative and peri-operative optimisation techniques to improve outcome. J. Crohns Colitis 9, 483–491 (2015).
Musallam, K. M. et al. Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet 378, 1396–1407 (2011).
Baron, D. M. et al. Preoperative anaemia is associated with poor clinical outcome in non-cardiac surgery patients. Br. J. Anaesth. 113, 416–423 (2014).
Marik, P. E. & Corwin, H. L. Efficacy of red blood cell transfusion in the critically ill: a systematic review of the literature. Crit. Care Med. 36, 2667–2674 (2008).
Li, Y. et al. Perioperative blood transfusion and postoperative outcome in patients with Crohn's disease undergoing primary ileocolonic resection in the “biological era”. J. Gastrointest. Surg. 19, 1842–1851 (2015).
Fraser, C. G., Preuss, F. S. & Bigford, W. D. Adrenal atrophy and irreversible shock associated with cortisone therapy. J. Am. Med. Assoc. 149, 1542–1543 (1952).
Axelrod, L. Perioperative management of patients treated with glucocorticoids. Endocrinol. Metab. Clin. North Am. 32, 367–383 (2003).
Subramanian, V., Saxena, S., Kang, J. Y. & Pollok, R. C. Preoperative steroid use and risk of postoperative complications in patients with inflammatory bowel disease undergoing abdominal surgery. Am. J. Gastroenterol. 103, 2373–2381 (2008).
Ziv, Y., Church, J. M., Fazio, V. W., King, T. M. & Lavery, I. C. Effect of systemic steroids on ileal pouch-anal anastomosis in patients with ulcerative colitis. Dis. Colon Rectum 39, 504–508 (1996).
Aberra, F. N. et al. Corticosteroids and immunomodulators: postoperative infectious complication risk in inflammatory bowel disease patients. Gastroenterology 125, 320–327 (2003).
Zaghiyan, K., Melmed, G., Murrell, Z. & Fleshner, P. Safety and feasibility of using low-dose perioperative intravenous steroids in inflammatory bowel disease patients undergoing major colorectal surgery: a pilot study. Surgery 152, 158–163 (2012).
Zaghiyan, K., Melmed, G., Murrell, Z. & Fleshner, P. Are high-dose perioperative steroids necessary in patients undergoing colorectal surgery treated with steroid therapy within the past 12 months? Am. Surg. 77, 1295–1299 (2011).
Zaghiyan, K. N., Murrell, Z., Melmed, G. Y. & Fleshner, P. R. High-dose perioperative corticosteroids in steroid-treated patients undergoing major colorectal surgery: necessary or overkill? Am. J. Surg. 204, 481–486 (2012).
Zaghiyan, K. et al. A prospective, randomized, noninferiority trial of steroid dosing after major colorectal surgery. Ann. Surg. 259, 32–37 (2014).
Colombel, J. F. et al. Early postoperative complications are not increased in patients with Crohn's disease treated perioperatively with infliximab or immunosuppressive therapy. Am. J. Gastroenterol. 99, 878–883 (2004).
Myrelid, P. et al. Thiopurine therapy is associated with postoperative intra-abdominal septic complications in abdominal surgery for Crohn's disease. Dis. Colon Rectum 52, 1387–1394 (2009).
Schaeffer, D. F. et al. Distinctive histopathologic phenotype in resection specimens from patients with Crohn's disease receiving anti-TNF-α therapy. Hum. Pathol. 45, 1928–1935 (2014).
Billioud, V. et al. Preoperative use of anti-TNF therapy and postoperative complications in inflammatory bowel diseases: a meta-analysis. J. Crohns Colitis 7, 853–867 (2013).
Rosenfeld, G., Qian, H. & Bressler, B. The risks of post-operative complications following pre-operative infliximab therapy for Crohn's disease in patients undergoing abdominal surgery: a systematic review and meta-analysis. J. Crohns Colitis 7, 868–877 (2013).
Yang, Z. P., Hong, L., Wu, Q., Wu, K. C. & Fan, D. M. Preoperative infliximab use and postoperative complications in Crohn's disease: a systematic review and meta-analysis. Int. J. Surg. 12, 224–230 (2014).
Appau, K. A. et al. Use of infliximab within 3 months of ileocolonic resection is associated with adverse postoperative outcomes in Crohn's patients. J. Gastrointest. Surg. 12, 1738–1744 (2008).
Van Assche, G. et al. The second European evidence-based Consensus on the diagnosis and management of Crohn's disease: definitions and diagnosis. J. Crohns Colitis 4, 7–27 (2010).
Alves, A. et al. Risk factors for intra-abdominal septic complications after a first ileocecal resection for Crohn's disease: a multivariate analysis in 161 consecutive patients. Dis. Colon Rectum 50, 331–336 (2007).
Tzivanakis, A. et al. Influence of risk factors on the safety of ileocolic anastomosis in Crohn's disease surgery. Dis. Colon Rectum 55, 558–562 (2012).
Gutierrez, A., Lee, H. & Sands, B. E. Outcome of surgical versus percutaneous drainage of abdominal and pelvic abscesses in Crohn's disease. Am. J. Gastroenterol. 101, 2283–2289 (2006).
Cullen, G. et al. Abdominal phlegmons in Crohn's disease: outcomes following antitumor necrosis factor therapy. Inflamm. Bowel Dis. 18, 691–696 (2012).
Feagins, L. A., Holubar, S. D., Kane, S. V. & Spechler, S. J. Current strategies in the management of intra-abdominal abscesses in Crohn's disease. Clin. Gastroenterol. Hepatol. 9, 842–850 (2011).
Lobaton, T. et al. Comparison of the long-term outcome of two therapeutic strategies for the management of abdominal abscess complicating Crohn's disease: percutaneous drainage or immediate surgical treatment. Colorectal Dis. 15, 1267–1272 (2013).
Nguyen, D. L. et al. Similar outcomes of surgical and medical treatment of intra-abdominal abscesses in patients with Crohn's disease. Clin. Gastroenterol. Hepatol. 10, 400–404 (2012).
Nguyen, D. L., Nguyen, E. T. & Bechtold, M. L. Outcomes of initial medical compared with surgical strategies in the management of intra-abdominal abscesses in patients with Crohn's disease: a meta-analysis. Eur. J. Gastroenterol. Hepatol. 27, 235–241 (2015).
da Luz Moreira, A., Stocchi, L., Tan, E., Tekkis, P. P. & Fazio, V. W. Outcomes of Crohn's disease presenting with abdominopelvic abscess. Dis. Colon Rectum 52, 906–912 (2009).
Rypens, F., Dubois, J., Garel, L., Deslandres, C. & Saint-Vil, D. Percutaneous drainage of abdominal abscesses in pediatric Crohn's disease. AJR Am. J. Roentgenol. 188, 579–585 (2007).
Xie, Y., Zhu, W., Li, N. & Li, J. The outcome of initial percutaneous drainage versus surgical drainage for intra-abdominal abscesses in Crohn's disease. Int. J. Colorectal Dis. 27, 199–206 (2012).
Bermejo, F. et al. Efficacy of different therapeutic options for spontaneous abdominal abscesses in Crohn's disease: are antibiotics enough? Inflamm. Bowel Dis. 18, 1509–1514 (2012).
Reese, G. E. et al. The effect of smoking after surgery for Crohn's disease: a meta-analysis of observational studies. Int. J. Colorectal Dis. 23, 1213–1221 (2008).
Warner, M. A., Divertie, M. B. & Tinker, J. H. Preoperative cessation of smoking and pulmonary complications in coronary artery bypass patients. Anesthesiology 60, 380–383 (1984).
Moller, A. & Tonnesen, H. Risk reduction: perioperative smoking intervention. Best Pract. Res. Clin. Anaesthesiol. 20, 237–248 (2006).
Moller, A. M., Villebro, N., Pedersen, T. & Tonnesen, H. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet 359, 114–117 (2002).
Irving, P. M., Pasi, K. J. & Rampton, D. S. Thrombosis and inflammatory bowel disease. Clin. Gastroenterol. Hepatol. 3, 617–628 (2005).
Bryant, R. V., Jairath, V., Curry, N. & Travis, S. P. Thrombosis in inflammatory bowel disease: are we tailoring prophylaxis to those most at risk? J. Crohns Colitis 8, 166–171 (2014).
Merrill, A. & Millham, F. Increased risk of postoperative deep vein thrombosis and pulmonary embolism in patients with inflammatory bowel disease: a study of National Surgical Quality Improvement Program patients. Arch. Surg. 147, 120–124 (2012).
Wallaert, J. B. et al. Venous thromboembolism after surgery for inflammatory bowel disease: are there modifiable risk factors? Data from ACS NSQIP. Dis. Colon Rectum 55, 1138–1144 (2012).
Nguyen, G. C. & Sam, J. Rising prevalence of venous thromboembolism and its impact on mortality among hospitalized inflammatory bowel disease patients. Am. J. Gastroenterol. 103, 2272–2280 (2008).
Bergqvist, D. et al. Duration of prophylaxis against venous thromboembolism with enoxaparin after surgery for cancer. N. Engl. J. Med. 346, 975–980 (2002).
Gross, M. E., Vogler, S. A., Mone, M. C., Sheng, X. & Sklow, B. The importance of extended postoperative venous thromboembolism prophylaxis in IBD: a National Surgical Quality Improvement Program analysis. Dis. Colon Rectum 57, 482–489 (2014).
Copeland, G. P., Jones, D. & Walters, M. POSSUM: a scoring system for surgical audit. Br. J. Surg. 78, 355–360 (1991).
Egberts, J. H. et al. Preoperative risk evaluation of postoperative morbidity in IBD patients—impact of the POSSUM score. Int. J. Colorectal Dis. 26, 783–792 (2011).
Ugolini, G. et al. Can POSSUM accurately predict post-operative complications risk in patients with abdominal Crohn's disease? ANZ J. Surg. 84, 78–84 (2014).
Older, P., Smith, R., Courtney, P. & Hone, R. Preoperative evaluation of cardiac failure and ischemia in elderly patients by cardiopulmonary exercise testing. Chest 104, 701–704 (1993).
Older, P., Hall, A. & Hader, R. Cardiopulmonary exercise testing as a screening test for perioperative management of major surgery in the elderly. Chest 116, 355–362 (1999).
Snowden, C. P. et al. Submaximal cardiopulmonary exercise testing predicts complications and hospital length of stay in patients undergoing major elective surgery. Ann. Surg. 251, 535–541 (2010).
Whipp, B. J., Ward, S. A. & Wasserman, K. Respiratory markers of the anaerobic threshold. Adv. Cardiol. 35, 47–64 (1986).
Otto, J. M. et al. Preoperative exercise capacity in adult inflammatory bowel disease sufferers, determined by cardiopulmonary exercise testing. Int. J. Colorectal Dis. 27, 1485–1491 (2012).
Nordenvall, C., Ekbom, A., Bottai, M., Smedby, K. E. & Nilsson, P. J. Mortality after total colectomy in 3084 atients with inflammatory bowel disease: a population-based cohort study. Aliment. Pharmacol. Ther. 40, 280–287 (2014).
Kaplan, G. G. et al. Impact of hospital volume on postoperative morbidity and mortality following a colectomy for ulcerative colitis. Gastroenterology 134, 680–687 (2008).
Ananthakrishnan, A. N., McGinley, E. L. & Binion, D. G. Does it matter where you are hospitalized for inflammatory bowel disease? A nationwide analysis of hospital volume. Am. J. Gastroenterol. 103, 2789–2798 (2008).
Tottrup, A., Erichsen, R., Svaerke, C., Laurberg, S. & Srensen, H. T. Thirty-day mortality after elective and emergency total colectomy in Danish patients with inflammatory bowel disease: a population-based nationwide cohort study. BMJ Open 2, e000823 (2012).
Masoomi, H. et al. Predictive factors of in-hospital mortality in colon and rectal surgery. J. Am. Coll. Surg. 215, 255–261 (2012).
Tan, J. J. & Tjandra, J. J. Laparoscopic surgery for Crohn's disease: a meta-analysis. Dis. Colon Rectum 50, 576–585 (2007).
Bergamaschi, R., Pessaux, P. & Arnaud, J. P. Comparison of conventional and laparoscopic ileocolic resection for Crohn's disease. Dis. Colon Rectum 46, 1129–1133 (2003).
Dignass, A. et al. The second European evidence-based Consensus on the diagnosis and management of Crohn's disease: current management. J. Crohns Colitis 4, 28–62 (2010).
Tilney, H. S. et al. Comparison of laparoscopic and open ileocecal resection for Crohn's disease: a metaanalysis. Surg. Endosc. 20, 1036–1044 (2006).
Lee, Y. et al. A laparoscopic approach reduces short-term complications and length of stay following ileocolic resection in Crohn's disease: an analysis of outcomes from the NSQIP database. Colorectal Dis. 14, 572–577 (2012).
Eshuis, E. J. et al. Long-term outcomes following laparoscopically assisted versus open ileocolic resection for Crohn's disease. Br. J. Surg. 97, 563–568 (2010).
Umanskiy, K. et al. Laparoscopic colectomy for Crohn's colitis. A large prospective comparative study. J. Gastrointest. Surg. 14, 658–663 (2010).
Holubar, S. D. et al. Minimally invasive colectomy for Crohn's colitis: a single institution experience. Inflamm. Bowel Dis. 16, 1940–1946 (2010).
da Luz Moreira, A. et al. Laparoscopic surgery for patients with Crohn's colitis: a case-matched study. J. Gastrointest. Surg. 11, 1529–1533 (2007).
Brouquet, A. et al. A laparoscopic approach to iterative ileocolonic resection for the recurrence of Crohn's disease. Surg. Endosc. 24, 879–887 (2010).
Chaudhary, B., Glancy, D. & Dixon, A. R. Laparoscopic surgery for recurrent ileocolic Crohn's disease is as safe and effective as primary resection. Colorectal Dis. 13, 1413–1416 (2011).
Alves, A. et al. Factors that predict conversion in 69 consecutive patients undergoing laparoscopic ileocecal resection for Crohn's disease: a prospective study. Dis. Colon Rectum 48, 2302–2308 (2005).
Goyer, P. et al. Impact of complex Crohn's disease on the outcome of laparoscopic ileocecal resection: a comparative clinical study in 124 patients. Dis. Colon Rectum 52, 205–210 (2009).
Gardenbroek, T. J. et al. Single-port versus multiport laparoscopic ileocecal resection for Crohn's disease. J. Crohns Colitis 7, e443–e448 (2013).
Lesperance, K., Martin, M. J., Lehmann, R., Brounts, L. & Steele, S. R. National trends and outcomes for the surgical therapy of ileocolonic Crohn's disease: a population-based analysis of laparoscopic versus open approaches. J. Gastrointest. Surg. 13, 1251–1259 (2009).
Simillis, C. et al. A meta-analysis comparing conventional end-to-end anastomosis versus other anastomotic configurations after resection in Crohn's disease. Dis. Colon Rectum 50, 1674–1687 (2007).
Guo, Z. et al. Comparing outcomes between side-to-side anastomosis and other anastomotic configurations after intestinal resection for patients with Crohn's disease: a meta-analysis. World J. Surg. 37, 893–901 (2013).
He, X. et al. Stapled side-to-side anastomosis might be better than handsewn end-to-end anastomosis in ileocolic resection for Crohn's disease: a meta-analysis. Dig. Dis. Sci. 59, 1544–1551 (2014).
McLeod, R. S. et al. Recurrence of Crohn's disease after ileocolic resection is not affected by anastomotic type: results of a multicenter, randomized, controlled trial. Dis. Colon Rectum 52, 919–927 (2009).
Ikeuchi, H., Kusunoki, M. & Yamamura, T. Long-term results of stapled and hand-sewn anastomoses in patients with Crohn's disease. Dig. Surg. 17, 493–496 (2000).
Zurbuchen, U. et al. Complications after end-to-end versus side-to-side anastomosis in ileocecal Crohn's disease—early postoperative results from a randomized controlled multi-center trial (ISRCTN-45665492). Langenbecks Arch. Surg. 398, 467–474 (2013).
Kono, T. et al. A new antimesenteric functional end-to-end handsewn anastomosis: surgical prevention of anastomotic recurrence in Crohn's disease. Dis. Colon Rectum 54, 586–592 (2011).
Choy, P. Y. et al. Stapled versus handsewn methods for ileocolic anastomoses. Cochrane Database Syst. Rev. 9, CD004320 (2011).
Fazio, V. W. et al. Effect of resection margins on the recurrence of Crohn's disease in the small bowel. A randomized controlled trial. Ann. Surg. 224, 563–571; discussion 571–563 (1996).
Shental, O., Tulchinsky, H., Greenberg, R., Klausner, J. M. & Avital, S. Positive histological inflammatory margins are associated with increased risk for intra-abdominal septic complications in patients undergoing ileocolic resection for Crohn's disease. Dis. Colon Rectum 55, 1125–1130 (2012).
Simi, M. et al. Early complications after surgery for Crohn's disease. Neth. J. Surg. 42, 105–109 (1990).
Tonelli, P. et al. Preliminary results of the influence of the in vivo use of a lymphatic dye (patent blue v) in the surgical treatment of Crohn's disease. Surg. Innov. 21, 381–388 (2014).
Kuiper, T. et al. New classification for probe-based confocal laser endomicroscopy in the colon. Endoscopy 43, 1076–1081 (2011).
Abbaci, M. et al. Patent blue V and indocyanine green for fluorescence microimaging of human peritoneal carcinomatosis using probe-based confocal laser endomicroscopy. Surg. Endosc. http://dx.doi.org/10.1007/s00464-016-4873-2 (2016).
de Silva, A. D., Mylonaki, M. & Rampton, D. S. Oral iron therapy in inflammatory bowel disease: usage, tolerance, and efficacy. Inflamm. Bowel Dis. 9, 316–320 (2003).
Lee, T. W., Kolber, M. R., Fedorak, R. N. & van Zanten, S. V. Iron replacement therapy in inflammatory bowel disease patients with iron deficiency anemia: a systematic review and meta-analysis. J. Crohns Colitis 6, 267–275 (2012).
Van Assche, G. et al. The second European evidence-based Consensus on the diagnosis and management of Crohn's disease: special situations. J. Crohns Colitis 4, 63–101 (2010).
Gustafsson, U. O. et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Clin. Nutr. 31, 783–800 (2012).
Nygren, J. et al. Guidelines for perioperative care in elective rectal/pelvic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Clin. Nutr. 31, 801–816 (2012).
Nygren, J. et al. Guidelines for perioperative care in elective rectal/pelvic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. World J. Surg. 37, 285–305 (2013).
Geerts, W. H. et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 133, 381S–453S (2008).
Warner, D. O. Helping surgical patients quit smoking: why, when, and how. Anesth. Analg. 101, 481–487 (2005).
Windsor, A. C. Ileal Crohn's disease is best treated by surgery. Gut 51, 11–12 (2002).
Patel, K. V. et al. DOP014 nutritional optimisation of presurgical Crohn's disease patients with enteral nutrition significantly decreases length of stay and need for a stoma [abstract]. ECCO Congress 10, S33 (2016).
Author information
Authors and Affiliations
Contributions
P.M.I. researched data for the article, contributed to discussion of content and reviewed/edited the manuscript before submission. K.V.P. researched data for the article, contributed to discussion of content and wrote the article. A.A.D. contributed to discussion of content and reviewed/edited the manuscript before submission. N.G. wrote the article. A.B.W and J.D.S. reviewed/edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Patel, K., Darakhshan, A., Griffin, N. et al. Patient optimization for surgery relating to Crohn's disease. Nat Rev Gastroenterol Hepatol 13, 707–719 (2016). https://doi.org/10.1038/nrgastro.2016.158
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2016.158
This article is cited by
-
Role of visceral fat on postoperative complications and relapse in patients with Crohn's disease after ileocecal resection: Is it overrated?
International Journal of Colorectal Disease (2024)
-
The Sasaki-W anastomosis for recurrent Crohn’s disease stenosis after the Kono-S anastomosis
Surgical Case Reports (2023)
-
Prognostic factors for the efficacy of infliximab in patients with luminal fistulizing Crohn’s disease
BMC Gastroenterology (2023)
-
Quantitative analysis of adipose tissue for predicting Crohn's disease postoperative endoscopic recurrence and anastomotic ulcer
International Journal of Colorectal Disease (2023)
-
Ileocecal valve that cannot be intubated in Crohn’s disease: is this a sign of poor prognosis?
International Journal of Colorectal Disease (2023)