Abstract
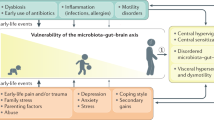
In this Review, after a brief historical introduction, we first provide an overview of epidemiological studies that demonstrate an association between functional dyspepsia and psychological traits, states or psychiatric disorders. These studies suggest an important intrinsic role for psychosocial factors and psychiatric disorders, especially anxiety and depression, in the aetiopathogenesis of functional dyspepsia, in addition to their putative influence on health-care-seeking behaviour. Second, we describe pathophysiological evidence on how psychosocial factors and psychiatric disorders might exert their role in functional dyspepsia. Novel insights from functional brain imaging studies regarding the integration of gut–brain signals, processed in homeostatic–interoceptive brain regions, with input from the exteroceptive system, the reward system and affective and cognitive circuits, help to clarify the important role of psychological processes and psychiatric morbidity. We therefore propose an integrated model of functional dyspepsia as a disorder of gut–brain signalling, supporting a biopsychosocial approach to the diagnosis and management of this disorder.
Key Points
-
Epidemiological studies demonstrate a higher prevalence of anxiety and depression in patients with functional dyspepsia than in healthy individuals, suggesting an intrinsic role for these psychiatric disorders in the aetiopathogenesis of functional dyspepsia
-
Epidemiological evidence also suggests a role for personality traits, stressful life events in general (and sexual and physical abuse in particular) and other psychosocial factors in functional dyspepsia
-
Pathophysiological studies show that psychosocial factors and psychiatric disorders might exert their role in functional dyspepsia by modulating the processing of visceral signals in the brain and through descending pathways
-
The autonomic nervous system and stress hormone system are important brain–gut interfaces through which psychosocial factors and psychiatric comorbidity might influence gastric motor function, including accommodation and emptying
-
A biopsychosocial approach to the diagnosis and management of functional dyspepsia is warranted and empirically supported by an integrated model of functional dyspepsia as a disorder of brain–gut signalling
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Cannon, W. B. The influence of emotional states on the functions of the alimentary canal. Am. J. Med. Sci. 137, 480–486 (1909).
Leube . Ueber Nervöse Dyspepsie. Dtsch. Arch. Klin. Med. 28 (1879).
Flanders Dunbar, H. Emotions and bodily changes 2nd edn (Columbia University Press, New York, 1938).
Einhorn, M. Diseases of the stomach: a textbook for practitioners and students (William Wood and Company, New York, 1896).
Burkhart, R. Zur pathologie der Neurasthenia gastrica [Dyspepsia nervosa] [German] (Bonn, 1882).
Ewald, C. A. Die nervöse dyspepsie [German]. Verhandlungen den Dritten Congres für innere Medizin (1884).
Stiller, B. Die nervösen Magenkrankheiten [German] (Ferdinand Enke, Stuttgart, 1884).
Dreyfus, G. L. Über Nervöse Dyspepsie: Psychiatrische Untersuchungen aus der Medizinischen Klinik zu Heidelberg [German] (Fischer, Jena, 1908).
Gustavsson, S., Bates, S., Adami, H. O., Lööf, L. & Nyren, O. Dyspepsia. Definition and discussion of nomenclature. Scand. J. Gastroenterol. Suppl. 109, 11–13 (1985).
Thompson, W. G. Nonulcer dyspepsia. Can. Med. Assoc. J. 130, 565–569 (1984).
Alexander, F. Psychosomatic Medicine: Its Principles and Applications (W. W. Norton & Company, Inc., New York, 1950).
Drossman, D. A., Talley, N. & Richter, J. E. The Functional Gastrointestinal Disorders: Diagnosis, pathophysiology, and treatment—a multinational consensus (Little, Brown, Boston, 1994).
De Gucht, V. & Fischler, B. Somatization: a critical review of conceptual and methodological issues. Psychosomatics 43, 1–9 (2002).
Henningsen, P., Zimmermann, T. & Sattel, H. Medically unexplained physical symptoms, anxiety, and depression: a meta-analytic review. Psychosom. Med. 65, 528–533 (2003).
Aro, P. et al. Associations with uninvestigated and functional dyspepsia (Rome III) in a random adult population: The Kalixanda study. Gastroenterology 137, 94–100 (2009).
Ochi, M. et al. Perfectionism underlying psychological background correlated with the symptoms of functional dyspepsia. J. Gastroenterol. 43, 699–704 (2008).
Jones, M. P., Schettler, A., Olden, K. & Crowell, M. D. Alexithymia and somatosensory amplification in functional dyspepsia. Psychosomatics 45, 508–516 (2004).
Herschbach, P., Henrich, G. & von Rad, M. Psychological factors in functional gastrointestinal disorders: characteristics of the disorder or of the illness behavior? Psychosom. Med. 61, 148–153 (1999).
Haug, T. T., Wilhelmsen, I., Berstad, A. & Ursin, H. Life events and stress in patients with functional dyspepsia compared with patients with duodenal ulcer and healthy controls. Scand. J. Gastroenterol. 30, 524–530 (1995).
Jain, A. K., Gupta, J. P., Gupta, S., Rao, K. P. & Bahre, P. B. Neuroticism and stressful life events in patients with non-ulcer dyspepsia. J. Assoc. Physicians India 43, 90–91 (1995).
Jonsson, B. H., Theorell, T. & Gotthard, R. Symptoms and personality in patients with chronic functional dyspepsia. J. Psychosom. Res. 39, 93–102 (1995).
Haug, T. T., Svebak, S., Wilhelmsen, I., Berstad, A. & Ursin, H. Psychological factors and somatic symptoms in functional dyspepsia. A comparison with duodenal ulcer and healthy controls. J. Psychosom. Res. 38, 281–291 (1994).
Bennett, E., Beaurepaire, J., Langeluddecke, P., Kellow, J. & Tennant, C. Life stress and non-ulcer dyspepsia: a case–control study. J. Psychosom. Res. 35, 579–590 (1991).
Kok, L. P., Yap, I. L. & Guan, R. Y. Psychosocial aspects of non-ulcer dyspepsia. Singapore M. J. 30, 346–349 (1989).
Talley, N. J. et al. Relation among personality and symptoms in nonulcer dyspepsia and the irritable bowel syndrome. Gastroenterology 99, 327–333 (1990).
Talley, N. J., Fung, L. H., Gilligan, I. J., McNeil, D. & Piper, D. W. Association of anxiety, neuroticism, and depression with dyspepsia of unknown cause. A case–control study. Gastroenterology 90, 886–892 (1986).
Lee, S.-Y. et al. Stress, coping, and depression in non-ulcer dyspepsia patients. J. Psychosom. Res. 49, 93–99 (2000).
Cheng, C., Hui, W. M. & Lam, S. K. Coping style of individuals with functional dyspepsia. Psychosom. Med. 61, 789–795 (1999).
Koloski, N. A., Talley, N. J. & Boyce, P. M. A history of abuse in community subjects with irritable bowel syndrome and functional dyspepsia: the role of other psychosocial variables. Digestion 72, 86–96 (2005).
Hui, W. M., Shiu, L. P. & Lam, S. K. The perception of life events and daily stress in nonulcer dyspepsia. Am. J. Gastroenterol. 86, 292–296 (1991).
Talley, N. J. & Piper, D. W. Major life event stress and dyspepsia of unknown cause: a case control study. Gut 27, 127–134 (1986).
Lydiard, R. B. Increased prevalence of functional gastrointestinal disorders in panic disorder: clinical and theoretical implications. CNS Spectr. 10, 899–908 (2005).
Perona, M. N. et al. Prevalence of functional gastrointestinal disorders in women who report domestic violence to the police. Clin. Gastroenterol. Hepatol. 3, 436–441 (2005).
Li, Y., Nie, Y., Sha, W. & Su, H. The link between psychosocial factors and functional dyspepsia: an epidemiological study. Chin. Med. J. (Engl.) 115, 1082–1084 (2002).
Tominaga, K. et al. Comparison of gastrointestinal symptoms and psychological factors of functional dyspepsia to peptic ulcer or panic disorder patients. Inflammopharmacology 15, 84–89 (2007).
Nakao, H. et al. Comparison of clinical features and patient background in functional dyspepsia and peptic ulcer. Dig. Dis. Sci. 52, 2152–2158 (2007).
Wilhelmsen, I., Haug, T. T., Ursin, H. & Berstad, A. Discriminant analysis of factors distinguishing patients with functional dyspepsia from patients with duodenal ulcer. Significance of somatization. Dig. Dis. Sci. 40, 1105–1111 (1995).
Pajala, M., Heikkinen, M. & Hintikka, J. Mental distress in patients with functional or organic dyspepsia: a comparative study with a sample of the general population. Aliment. Pharmacol. Ther. 21, 277–281 (2005).
Mahadeva, S. & Goh, K. L. Anxiety, depression and quality of life differences between functional and organic dyspepsia. J. Gastroenterol. Hepatol. 26, 49–52 (2011).
Alexander, P. J. & Tantry, B. V. Role of anxiety and personality in non-ulcer dyspepsia: a comparative study with duodenal ulcer. Indian J. Gastroenterol. 12, 86–88 (1993).
Koloski, N. A., Talley, N. J. & Boyce, P. M. Predictors of health care seeking for irritable bowel syndrome and nonulcer dyspepsia: a critical review of the literature on symptom and psychosocial factors. Am. J. Gastroenterol. 96, 1340–1349 (2001).
Locke, G. R. 3rd, Weaver, A. L., Melton, L. J. 3rd & Talley, N. J. Psychosocial factors are linked to functional gastrointestinal disorders: a population based nested case–control study. Am. J. Gastroenterol. 99, 350–357 (2004).
Gathaiya, N. et al. Novel associations with dyspepsia: a community-based study of familial aggregation, sleep dysfunction and somatization. Neurogastroenterol. Motil. 21, 922–e69 (2009).
Castillo, E. J. et al. A community-based, controlled study of the epidemiology and pathophysiology of dyspepsia. Clin. Gastroenterol. Hepatol. 2, 985–996 (2004).
Pajala, M., Heikkinen, M. & Hintikka, J. Association between mental distress, gastrointestinal symptoms, and health-care utilization in functional dyspepsia: a prospective 7-year follow-up study. Scand. J. Gastroenterol. 47, 407–413 (2012).
Koloski, N., Boyce, P. & Talley, N. Is health care seeking for irritable bowel syndrome and functional dyspepsia a socially learned response to illness? Dig. Dis. Sci. 50, 153–162 (2005).
Koloski, N. A., Talley, N. J., Huskic, S. S. & Boyce, P. M. Predictors of conventional and alternative health care seeking for irritable bowel syndrome and functional dyspepsia. Aliment. Pharmacol. Ther. 17, 841–851 (2003).
Koloski, N. A., Talley, N. J. & Boyce, P. M. Epidemiology and health care seeking in the functional GI disorders: a population-based study. Am. J. Gastroenterol. 97, 2290–2299 (2002).
Cheng, C. Seeking medical consultation: perceptual and behavioral characteristics distinguishing consulters and nonconsulters with functional dyspepsia. Psychosom. Med. 62, 844–852 (2000).
Koloski, N. A. et al. The brain–gut pathway in functional gastrointestinal disorders is bidirectional: a 12-year prospective population-based study. Gut 61, 1284–1290 (2012).
Jones, M. P., Van Oudenhove, L. & Talley, N. J. Functional gastrointestinal disorders (FGIDs) and psychological disorders: strong evidence that the link is bidirectional, but psychological distress is more likely to precede a new diagnosis of an FGID [abstract]. Gastroenterology 142 (Suppl. 1), S570 (2012).
Sykes, M. A., Blanchard, E. B., Lackner, J., Keefer, L. & Krasner, S. Psychopathology in irritable bowel syndrome: support for a psychophysiological model. J. Behav. Med. 26, 361–372 (2003).
Van Oudenhove, L., Talley, N. J., Jones, M. P. & Koloski, N. A. Psychological factors and somatization at baseline predict gastrointestinal symptom severity and consulting behaviour at 18 months follow-up [abstract]. Gastroenterology 142 (Suppl. 1), S9 (2012).
Holtmann, G. et al. Clinical presentation and personality factors are predictors of the response to treatment in patients with functional dyspepsia: a randomized, double-blind placebo-controlled crossover study. Dig. Dis. Sci. 49, 672–679 (2004).
Bates, S., Sjoden, P.-O. & Nyren, O. Behavioral treatment of non-ulcer dyspepsia. Scand. J. Behav. Ther. 17, 155–165 (1988).
Calvert, E. L., Houghton, L. A., Cooper, P., Morris, J. & Whorwell, P. J. Long-term improvement in functional dyspepsia using hypnotherapy. Gastroenterology 123, 1778–1785 (2002).
Haug, T. T., Wilhelmsen, I., Svebak, S., Berstad, A. & Ursin, H. Psychotherapy in functional dyspepsia. J. Psychosom. Res. 38, 735–744 (1994).
Hamilton, J. et al. A randomized controlled trial of psychotherapy in patients with chronic functional dyspepsia. Gastroenterology 119, 661–669 (2000).
Soo, S. et al. Psychological interventions for non-ulcer dyspepsia. Cochrane Database of Systematic Reviews, Issue 2. Art. No.: CD002301 http://dx.doi.org/10.1002/14651858.CD002301.pub4.
Haag, S. et al. Is there a benefit from intensified medical and psychological interventions in patients with functional dyspepsia not responding to conventional therapy? Aliment. Pharmacol. Ther. 25, 973–986 (2007).
Cheng, C., Yang, F. C., Jun, S. & Hutton, J. M. Flexible coping psychotherapy for functional dyspeptic patients: a randomized, controlled trial. Psychosom. Med. 69, 81–88 (2007).
Cheng, C., Hui, W. M. & Lam, S. K. Psychosocial factors and perceived severity of functional dyspeptic symptoms: a psychosocial interactionist model. Psychosom. Med. 66, 85–91 (2004).
Jones, M. P., Sharp, L. K. & Crowell, M. D. Psychosocial correlates of symptoms in functional dyspepsia. Clin. Gastroenterol. Hepatol. 3, 521–528 (2005).
Jones, M. P. & Maganti, K. Symptoms, gastric function, and psychosocial factors in functional dyspepsia. J. Clin. Gastroenterol. 38, 866–872 (2004).
Van Oudenhove, L. et al. Determinants of symptoms in functional dyspepsia: gastric sensorimotor function, psychosocial factors or somatization? Gut 57, 1666–1673 (2008).
Handa, M. et al. Esophageal motility and psychiatric factors in functional dyspepsia patients with or without pain. Dig. Dis. Sci. 44, 2094–2098 (1999).
Fischler, B. et al. Heterogeneity of symptom pattern, psychosocial factors, and pathophysiological mechanisms in severe functional dyspepsia. Gastroenterology 124, 903–910 (2003).
Hsu, Y. C. et al. Psychopathology and personality trait in subgroups of functional dyspepsia based on Rome III criteria. Am. J. Gastroenterol. 104, 2534–2542 (2009).
Clauwaert, N. et al. Associations between gastric sensorimotor function, depression, somatization, and symptom-based subgroups in functional gastroduodenal disorders: are all symptoms equal? Neurogastroenterol. Motil. 24, 1088–e565 (2012).
Van Oudenhove, L. et al. Risk factors for impaired health-related quality of life in functional dyspepsia. Aliment. Pharmacol. Ther. 33, 261–274 (2010).
Haag, S. et al. Impairment of health-related quality of life in functional dyspepsia and chronic liver disease: the influence of depression and anxiety. Aliment. Pharmacol. Ther. 27, 561–571 (2008).
Biggs, A. M., Aziz, Q., Tomenson, B. & Creed, F. Effect of childhood adversity on health related quality of life in patients with upper abdominal or chest pain. Gut 53, 180–186 (2004).
Gutierrez, A. A. et al. Quality of life in patients with functional dyspepsia: a prospective 1-year follow-up study in Spanish patients. Eur. J. Gastroenterol. Hepatol. 15, 1175–1181 (2003).
Tack, J., Bisschops, R. & Sarnelli, G. Pathophysiology and treatment of functional dyspepsia. Gastroenterology 127, 1239–1255 (2004).
Tack, J. et al. Functional gastroduodenal disorders. Gastroenterology 130, 1466–1479 (2006).
Hausken, T. et al. Low vagal tone and antral dysmotility in patients with functional dyspepsia. Psychosom. Med. 55, 12–22 (1993).
Hveem, K., Hausken, T., Svebak, S. & Berstad, A. Gastric antral motility in functional dyspepsia. Effect of mental stress and cisapride. Scand. J. Gastroenterol. 31, 452–457 (1996).
Haug, T. T. et al. Low vagal activity as mediating mechanism for the relationship between personality factors and gastric symptoms in functional dyspepsia. Psychosom. Med. 56, 181–186 (1994).
Kawakami, H. et al. Personality deviation and gastric motility in patients with functional dyspepsia. J. Clin. Gastroenterol. 21 (Suppl. 1), S179–S184 (1995).
Chou, L. T. et al. The correlation of depression and gastric dysrhythmia in functional dyspepsia. J. Clin. Gastroenterol. 33, 127–131 (2001).
Chen, T. S., Lee, Y. C., Chang, F. Y., Wu, H. C. & Lee, S. D. Psychosocial distress is associated with abnormal gastric myoelectrical activity in patients with functional dyspepsia. Scand. J. Gastroenterol. 41, 791–796 (2006).
Chiarioni, G., Vantini, I., De Iorio, F. & Benini, L. Prokinetic effect of gut-oriented hypnosis on gastric emptying. Aliment. Pharmacol. Ther. 23, 1241–1249 (2006).
Van Oudenhove, L. et al. Relationship between anxiety and gastric sensorimotor function in functional dyspepsia. Psychosom. Med. 69, 455–463 (2007).
Geeraerts, B. et al. Influence of abuse history on gastric sensorimotor function in functional dyspepsia. Neurogastroenterol. Motil. 21, 33–41 (2009).
Van Oudenhove, L. et al. Abuse history, depression, and somatization are associated with gastric sensitivity and gastric emptying in functional dyspepsia. Psychosom. Med. 73, 648–655 (2011).
Geeraerts, B. et al. Influence of experimentally induced anxiety on gastric sensorimotor function in man. Gastroenterology 129, 1437–1444 (2005).
Aziz, Q. & Thompson, D. Brain-gut axis in health and disease. Gastroenterology 114, 559–578 (1998).
Van Oudenhove, L., Demyttenaere, K., Tack, J. & Aziz, Q. Central nervous system involvement in functional gastrointestinal disorders. Best Pract. Res. Clin. Gastroenterol. 18, 663–680 (2004).
Van Oudenhove, L., Coen, S. & Aziz, Q. Functional brain imaging of gastrointestinal sensation in health and disease. World J. Gastroenterol. 13, 3438–3445 (2007).
Jones, M. P., Dilley, J. B., Drossman, D. & Crowell, M. D. Brain-gut connections in functional GI disorders: anatomic and physiologic relationships. Neurogastroenterol. Motil. 18, 91–103 (2006).
Mayer, E. A. Gut feelings: the emerging biology of gut-brain communication. Nat. Rev. Neurosci. 12, 453–466 (2011).
Mayer, E. A., Naliboff, B. D. & Craig, A. D. B. Neuroimaging of the brain-gut axis: from basic understanding to treatment of functional GI disorders. Gastroenterology 131, 1925–1942 (2006).
Craig, A. D. How do you feel? Interoception: the sense of the physiological condition of the body. Nat. Rev. Neurosci. 3, 655–666 (2002).
Craig, A. D. How do you feel—now? The anterior insula and human awareness. Nat. Rev. Neurosci. 10, 59–70 (2009).
Van Oudenhove, L. Understanding gut–brain interactions in gastrointestinal pain by neuroimaging: lessons from somatic pain studies. Neurogastroenterol. Motil. 23, 292–302 (2011).
Berthoud, H. R. & Morrison, C. The brain, appetite, and obesity. Ann. Rev. Psychol. 59, 55–92 (2008).
Grundy, D. Signalling the state of the digestive tract. Auton. Neurosci. 125, 76–80 (2006).
Kaye, W. H., Fudge, J. L. & Paulus, M. New insights into symptoms and neurocircuit function of anorexia nervosa. Nat. Rev. Neurosci. 10, 573–584 (2009).
Wiech, K., Ploner, M. & Tracey, I. Neurocognitive aspects of pain perception. Trends Cogn. Sci. 12, 306–313 (2008).
Wiech, K. & Tracey, I. The influence of negative emotions on pain: behavioral effects and neural mechanisms. Neuroimage 47, 987–994 (2009).
Fields, H. State-dependent opioid control of pain. Nat. Rev. Neurosci. 5, 565–575 (2004).
Wilder-Smith, C. H. The balancing act: endogenous modulation of pain in functional gastrointestinal disorders. Gut 60, 1589–1599 (2011).
Coen, S. J. et al. Effects of attention on visceral stimulus intensity encoding in the male human brain. Gastroenterology 135, 2065–2074 (2008).
Coen, S. J. et al. Negative mood affects brain processing of visceral sensation. Gastroenterology 137, 253–261 (2009).
Coen, S. J. et al. Neuroticism influences brain activity during the experience of visceral pain. Gastroenterology 141, 909–917e1 (2011).
Vandenberghe, J. et al. Regional cerebral blood flow during gastric balloon distention in functional dyspepsia. Gastroenterology 132, 1684–1693 (2007).
Van Oudenhove, L. et al. The role of somatosensory cortical regions in the processing of painful gastric fundic distension: an update of brain imaging findings. Neurogastroenterol. Motil. 20, 479–487 (2008).
Van Oudenhove, L. et al. Abnormal regional brain activity during rest and (anticipated) gastric distension in functional dyspepsia and the role of anxiety: a H215O-PET study. Am. J. Gastroenterol. 105, 913–924 (2010).
Van Oudenhove, L. et al. Altered brain network connectivity associated with increased perceptual response to aversive gastric distension and its expectation in functional dyspepsia [abstract 67]. Neurogastroenterol. Motil. 22 (Suppl. s1), 20–21 (2010).
Van Oudenhove, L. et al. Regional brain activity in functional dyspepsia: a H215O-PET study on the role of gastric sensitivity & abuse history. Gastroenterology 139, 236–247 (2010).
Van Oudenhove, L. et al. Altered brain connectivity underlies visceral perceptual hypersensitivity in abused functional dyspepsia patients. Gastroenterology 142, S-69–S-70 (2012).
Zeng, F. et al. Abnormal resting brain activity in patients with functional dyspepsia is related to symptom severity. Gastroenterology 141, 499–506 (2011).
Liu, M. L. et al. Cortical-limbic regions modulate depression and anxiety factors in functional dyspepsia: a PET-CT study. Ann. Nucl. Med. 26, 35–40 (2012).
Zeng, F. et al. Influence of acupuncture treatment on cerebral activity in functional dyspepsia patients and its relationship with efficacy. Am. J. Gastroenterol. 107, 1236–1247 (2012).
Camilleri, M., Malagelada, J. R., Kao, P. C. & Zinsmeister, A. R. Gastric and autonomic responses to stress in functional dyspepsia. Dig. Dis. Sci. 31, 1169–1177 (1986).
Mearin, F., Cucala, M., Azpiroz, F. & Malagelada, J. R. The origin of symptoms on the brain-gut axis in functional dyspepsia. Gastroenterology 101, 999–1006 (1991).
Hveem, K., Svebak, S., Hausken, T. & Berstad, A. Effect of mental stress and cisapride on autonomic nerve functions in functional dyspepsia. Scand. J. Gastroenterol. 33, 123–127 (1998).
Hjelland, I. E., Svebak, S., Berstad, A., Flatabø, G. & Hausken, T. Breathing exercises with vagal biofeedback may benefit patients with functional dyspepsia. Scand. J. Gastroenterol. 42, 1054–1062 (2007).
Lunding, J. et al. Vagal activation by sham feeding improves gastric motility in functional dyspepsia. Neurogastroenterol. Motil. 20, 618–624 (2008).
Muth, E. R., Koch, K. L. & Stern, R. M. Significance of autonomic nervous system activity in functional dyspepsia. Dig. Dis. Sci. 45, 854–863 (2000).
Lorena, S. L., Figueiredo, M. J., Almeida, J. R. & Mesquita, M. A. Autonomic function in patients with functional dyspepsia assessed by 24-hour heart rate variability. Dig. Dis. Sci. 47, 27–32 (2002).
Park, D. I. et al. Role of autonomic dysfunction in patients with functional dyspepsia. Dig. Liver Dis. 33, 464–471 (2001).
Friesen, C. A., Lin, Z., Schurman, J. V., Andre, L. & McCallum, R. W. The effect of a meal and water loading on heart rate variability in children with functional dyspepsia. Dig. Dis. Sci. 55, 2283–2287 (2010).
Jonsson, B. H. & Theorell, T. Low plasma prolactin levels in patients with functional dyspepsia. Psychother. Psychosom. 68, 151–156 (1999).
Bohmelt, A. H., Nater, U. M., Franke, S., Hellhammer, D. H. & Ehlert, U. Basal and stimulated hypothalamic–pituitary–adrenal axis activity in patients with functional gastrointestinal disorders and healthy controls. Psychosom. Med. 67, 288–294 (2005).
Ehlert, U., Nater, U. M. & Bohmelt, A. High and low unstimulated salivary cortisol levels correspond to different symptoms of functional gastrointestinal disorders. J. Psychosom. Res. 59, 7–10 (2005).
Heim, C. et al. Pituitary–adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA 284, 592–597 (2000).
Videlock, E. J. et al. Childhood trauma is associated with hypothalamic–pituitary–adrenal axis responsiveness in irritable bowel syndrome. Gastroenterology 137, 1954–1962 (2009).
Vanheel, H. & Farré, R. Changes in gastrointestinal tract function and structure in functional dyspepsia. Nat. Rev. Gastroenterol. Hepatol. http://dx.doi.org/10.1038/nrgastro.2012.255.
Author information
Authors and Affiliations
Contributions
L. Van Oudenhove contributed to all aspects of this manuscript. Q. Aziz contributed to discussion of content and reviewing/editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Table 1
Studies comparing levels of psychopathology between functional dyspepsia patients and healthy controls (DOC 138 kb)
Supplementary Table 2
Studies comparing levels of psychopathology between patients with functional dyspepsia and patients with other organic disease (controls) (DOC 76 kb)
Rights and permissions
About this article
Cite this article
Van Oudenhove, L., Aziz, Q. The role of psychosocial factors and psychiatric disorders in functional dyspepsia. Nat Rev Gastroenterol Hepatol 10, 158–167 (2013). https://doi.org/10.1038/nrgastro.2013.10
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2013.10
This article is cited by
-
Patients with postprandial distress syndrome experience problems with their interoceptive perceptual function to the gastric region, but their heartbeat perception is normal: a case control study
BioPsychoSocial Medicine (2023)
-
Exercise is inversely associated with functional dyspepsia among a sample of Chinese male armed police recruits
BMC Gastroenterology (2023)
-
Tuina treatment for children and adults with functional dyspepsia: a meta-analysis and systematic review of randomized controlled trials
Journal of Acupuncture and Tuina Science (2023)
-
Clinical Efficacy of Tandospirone on Functional Dyspepsia Patients with Anxiety: A Randomized, Placebo-Controlled Study
Digestive Diseases and Sciences (2023)
-
Brain activity in response to food images in patients with irritable bowel syndrome and functional dyspepsia
Journal of Gastroenterology (2023)