Abstract
IBS is a common gastrointestinal condition characterized by chronic or recurrent abdominal pain associated with altered bowel habits. IBS is considered a functional bowel disorder (that is, not defined by structural or biochemical abnormalities) and is diagnosed using symptom-based criteria. Limited and judicious use of diagnostic testing is recommended, particularly in patients with typical symptoms of IBS without alarm signs and symptoms. Management of IBS is based on a multifactorial approach and includes establishment of an effective patient–provider relationship, education, reassurance, dietary alterations, pharmacotherapy, behavioral and psychological treatment. Patient-centered care is recommended, in which management is focused on the patient's most bothersome and impactful symptoms, their preferences and previous experiences with treatment, and addressing factors associated with the onset and exacerbation of symptoms. Pharmacotherapy is typically targeted against the predominant symptom. This Review discusses the current evidence-based recommendations for the diagnosis and management of IBS. An improved understanding of the recommended diagnostic and therapeutic approaches for IBS will lead to greater patient satisfaction, as well as reduced health-care costs.
Key Points
-
IBS can be confidently diagnosed with symptom-based criteria in the absence of alarm signs
-
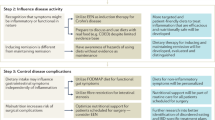
Management of IBS involves an integrative approach, including establishment of an effective patient–provider relationship, education, reassurance, dietary alterations, pharmacotherapy aimed at the most bothersome symptoms, behavioral and psychological treatment
-
Fiber, laxatives, a chloride channel activator and, rarely, 5-HT4 agonists are used to treat constipation-predominant symptoms
-
Antidiarrheal agents, antibiotics, tricyclic antidepressants and, in severe cases, a 5-HT3 antagonist are used to treat diarrhea-predominant symptoms
-
Dietary measures, probiotics and antibiotics may be efficacious for reducing bloating and gas; antidepressants and anticholinergics can help relieve abdominal pain
-
Effective psychological and behavioral treatment interventions for IBS include cognitive behavioral therapy, hypnosis, psychotherapy and stress management
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Longstreth, G. F. et al. Functional bowel disorders. Gastroenterology 130, 1480–1491 (2006).
Drossman, D. A., Camilleri, M., Mayer, E. A. & Whitehead, W. E. AGA technical review on irritable bowel syndrome. Gastroenterology 123, 2108–2131 (2002).
Gaburri, M. et al. Functional gut disorders and health care seeking behavior in an Italian non-patient population. Recenti Prog. Med. 80, 241–244 (1989).
Mearin, F. et al. Irritable bowel syndrome prevalence varies enormously depending on the employed diagnostic criteria: comparison of Rome II versus previous criteria in a general population. Scand. J. Gastroenterol. 36, 1155–1161 (2001).
Heaton, K. W. et al. Symptoms of irritable bowel syndrome in a British urban community: consulters and nonconsulters. Gastroenterology 102, 1962–1967 (1992).
Jones, R. & Lydeard, S. Irritable bowel syndrome in the general population. BMJ 304, 87–90 (1992).
Kennedy, T. M. & Jones, R. H. Epidemiology of cholecystectomy and irritable bowel syndrome in a UK population. Br. J. Surg. 87, 1658–1663 (2000).
Thompson, W. G., Heaton, K. W., Smyth, G. T. & Smyth, C. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut 46, 78–82 (2000).
Coffin, B., Dapoigny, M., Cloarec, D., Comet, D. & Dyard, F. Relationship between severity of symptoms and quality of life in 858 patients with irritable bowel syndrome. Gastroenterol. Clin. Biol. 28, 11–15 (2004).
Agreus, L., Svardsudd, K., Nyren, O. & Tibblin, G. Irritable bowel syndrome and dyspepsia in the general population: overlap and lack of stability over time. Gastroenterology 109, 671–680 (1995).
Kay, L., Jorgensen, T. & Jensen, K. H. The epidemiology of irritable bowel syndrome in a random population: prevalence, incidence, natural history and risk factors. J. Intern. Med. 236, 23–30 (1994).
Gwee, K. A. Irritable bowel syndrome in developing countries—a disorder of civilization or colonization? Neurogastroenterol. Motil. 17, 317–324 (2005).
Saito, Y. A., Schoenfeld, P. & Locke, G. R. 3rd. The epidemiology of irritable bowel syndrome in North America: a systematic review. Am. J. Gastroenterol. 97, 1910–1915 (2002).
Andrews, E. B. et al. Prevalence and demographics of irritable bowel syndrome: results from a large web-based survey. Aliment. Pharmacol. Ther. 22, 935–942 (2005).
Hungin, A. P., Chang, L., Locke, G. R., Dennis, E. H. & Barghout, V. Irritable bowel syndrome in the United States: prevalence, symptom patterns and impact. Aliment. Pharmacol. Ther. 21, 1365–1375 (2005).
Chang, L. et al. Gender, age, society, culture, and the patient's perspective in the functional gastrointestinal disorders. Gastroenterology 130, 1435–1446 (2006).
Spiller, R. et al. Guidelines on the irritable bowel syndrome: mechanisms and practical management. Gut 56, 1770–1798 (2007).
Koloski, N. A., Talley, N. J. & Boyce, P. M. Predictors of health care seeking for irritable bowel syndrome and nonulcer dyspepsia: a critical review of the literature on symptom and psychosocial factors. Am. J. Gastroenterol. 96, 1340–1349 (2001).
Creed, F. The relationship between psychosocial parameters and outcome in irritable bowel syndrome. Am. J. Med. 107, 74S–80S (1999).
Creed, F. in Functional Disorders of the Gut: A Handbook for Clinicians (eds Phillips, S. F. & Wingate, D. L.) 71–97 (WB Saunders Co. Ltd, London, 1998).
Lydiard, R. B. Irritable bowel syndrome, anxiety, and depression: what are the links? J. Clin. Psychiatry 62 (Suppl. 8), 38–45 (2001).
Sperber, A. D. et al. Fibromyalgia in the irritable bowel syndrome: studies of prevalence and clinical implications. Am. J. Gastroenterol. 94, 3541–3546 (1999).
Whitehead, W. E., Palsson, O. & Jones, K. R. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology 122, 1140–1156 (2002).
Longstreth, G. F., Preskill, D. B. & Youkeles, L. Irritable bowel syndrome in women having diagnostic laparoscopy or hysterectomy. Relation to gynecologic features and outcome. Dig. Dis. Sci. 35, 1285–1290 (1990).
Chang, L. Irritable Bowel Syndrome and Related Functional Disorders (IASP Press, Seattle, Washington, 2009).
El-Serag, H. B., Olden, K. & Bjorkman, D. Health-related quality of life among persons with irritable bowel syndrome: a systematic review. Aliment. Pharmacol. Ther. 16, 1171–1185 (2002).
Gralnek, I. M., Hays, R. D., Kilbourne, A., Naliboff, B. & Mayer, E. A. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology 119, 654–660 (2000).
Patrick, D. L., Drossman, D. A., Frederick, I. O., DiCesare, J. & Puder, K. L. Quality of life in persons with irritable bowel syndrome: development and validation of a new measure. Dig. Dis. Sci. 43, 400–411 (1998).
Pare, P. et al. Health-related quality of life, work productivity, and health care resource utilization of subjects with irritable bowel syndrome: baseline results from LOGIC (Longitudinal Outcomes Study of Gastrointestinal Symptoms in Canada), a naturalistic study. Clin. Ther. 28, 1726–1735 (2006).
Spiegel, B. M. et al. Clinical determinants of health-related quality of life in patients with irritable bowel syndrome. Arch. Intern. Med. 164, 1773–1780 (2004).
Naliboff, B. D., Balice, G. & Mayer, E. A. Psychosocial moderators of quality of life in irritable bowel syndrome. Eur. J. Surg. Suppl. 57–59 (1998).
Spiegel, B., Strickland, A., Naliboff, B. D., Mayer, E. A. & Chang, L. Predictors of patient-assessed illness severity in irritable bowel syndrome. Am. J. Gastroenterol. 103, 2536–2543 (2008).
Sandler, R. S. et al. The burden of selected digestive diseases in the United States. Gastroenterology 122, 1500–1511 (2002).
Maxion-Bergemann, S., Thielecke, F., Abel, F. & Bergemann, R. Costs of irritable bowel syndrome in the UK and US. Pharmacoeconomics 24, 21–37 (2006).
Dean, B. B. et al. Impairment in work productivity and health-related quality of life in patients with IBS. Am. J. Manag. Care 11, S17–S26 (2005).
Longstreth, G. F. et al. Irritable bowel syndrome, health care use, and costs: a US managed care perspective. Am. J. Gastroenterol. 98, 600–607 (2003).
Spiegel, B. M., Kanwal, F., Naliboff, B. & Mayer, E. The impact of somatization on the use of gastrointestinal health-care resources in patients with irritable bowel syndrome. Am. J. Gastroenterol. 100, 2262–2273 (2005).
Longstreth, G. F. & Yao, J. F. Irritable bowel syndrome and surgery: a multivariable analysis. Gastroenterology 126, 1665–1673 (2004).
Crowell, M. D., Harris, L., Jones, M. P. & Chang, L. New insights into the pathophysiology of irritable bowel syndrome: implications for future treatments. Curr. Gastroenterol. Rep. 7, 272–279 (2005).
Marshall, J. K. Post-infectious irritable bowel syndrome following water contamination. Kidney Int. Suppl. S42–S43 (2009).
Gwee, K. A. et al. Psychometric scores and persistence of irritable bowel after infectious diarrhoea. Lancet 347, 150–153 (1996).
Spiller, R. & Garsed, K. Postinfectious irritable bowel syndrome. Gastroenterology 136, 1979–1988 (2009).
Gwee, K. A. et al. The role of psychological and biological factors in postinfective gut dysfunction. Gut 44, 400–406 (1999).
Gwee, K. A. et al. Increased rectal mucosal expression of interleukin 1beta in recently acquired post-infectious irritable bowel syndrome. Gut 52, 523–526 (2003).
Brandt, L. J. et al. An evidence-based position statement on the management of irritable bowel syndrome. Am. J. Gastroenterol. 104 (Suppl. 1), S1–S35 (2009).
Spiegel, B. et al. Developing valid and reliable health utilities in irritable bowel syndrome: results from the IBS PROOF Cohort. Am. J. Gastroenterol. 104, 1984–1991 (2009).
Drossman, D. A. et al. Further validation of the IBS-QOL: a disease-specific quality-of-life questionnaire. Am. J. Gastroenterol. 95, 999–1007 (2000).
Park, M. I. & Camilleri, M. Is there a role of food allergy in irritable bowel syndrome and functional dyspepsia? A systematic review. Neurogastroenterol. Motil. 18, 595–607 (2006).
Simren, M. et al. Food-related gastrointestinal symptoms in the irritable bowel syndrome. Digestion 63, 108–115 (2001).
Clouse, R. E. et al. Functional abdominal pain syndrome. Gastroenterology 130, 1492–1497 (2006).
Heitkemper, M. M. et al. Symptoms across the menstrual cycle in women with irritable bowel syndrome. Am. J. Gastroenterol. 98, 420–430 (2003).
Manning, A. P., Thompson, W. G., Heaton, K. W. & Morris, A. F. Towards positive diagnosis of the irritable bowel. Br. Med. J. 2, 653–654 (1978).
Kruis, W. et al. A diagnostic score for the irritable bowel syndrome. Its value in the exclusion of organic disease. Gastroenterology 87, 1–7 (1984).
Ford, A. C. et al. Will the history and physical examination help establish that irritable bowel syndrome is causing this patient's lower gastrointestinal tract symptoms? JAMA 300, 1793–1805 (2008).
Jellema, P., van der Windt, D. A., Schellevis, F. G. & van der Horst, H. E. Systematic review: accuracy of symptom-based criteria for diagnosis of irritable bowel syndrome in primary care. Aliment. Pharmacol. Ther. 30, 695–706 (2009).
Tibble, J. A., Sigthorsson, G., Foster, R., Forgacs, I. & Bjarnason, I. Use of surrogate markers of inflammation and Rome criteria to distinguish organic from nonorganic intestinal disease. Gastroenterology 123, 450–460 (2002).
Vanner, S. J. et al. Predictive value of the Rome criteria for diagnosing the irritable bowel syndrome. Am. J. Gastroenterol. 94, 2912–2917 (1999).
Hammer, J., Eslick, G. D., Howell, S. C., Altiparmak, E. & Talley, N. J. Diagnostic yield of alarm features in irritable bowel syndrome and functional dyspepsia. Gut 53, 666–672 (2004).
Ford, A. C. et al. Diagnostic utility of alarm features for colorectal cancer: systematic review and meta-analysis. Gut 57, 1545–1553 (2008).
Fasano, A. et al. Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch. Intern. Med. 163, 286–292 (2003).
Podolsky, D. K. Inflammatory bowel disease. N. Engl. J. Med. 347, 417–429 (2002).
Winawer, S. et al. Colorectal cancer screening and surveillance: clinical guidelines and rationale—Update based on new evidence. Gastroenterology 124, 544–560 (2003).
Spiegel, B. M., Farid, M., Esrailian, E., Talley, J. & Chang, L. Is irritable bowel syndrome a diagnosis of exclusion?: a survey of primary care providers, gastroenterologists, and IBS experts. Am. J. Gastroenterol. 105, 848–858 (2010).
Ford, A. C. et al. Yield of diagnostic tests for celiac disease in individuals with symptoms suggestive of irritable bowel syndrome: systematic review and meta-analysis. Arch. Intern. Med. 169, 651–658 (2009).
Spiegel, B. M., DeRosa, V. P., Gralnek, I. M., Wang, V. & Dulai, G. S. Testing for celiac sprue in irritable bowel syndrome with predominant diarrhea: a cost-effectiveness analysis. Gastroenterology 126, 1721–1732 (2004).
Wahnschaffe, U., Schulzke, J. D., Zeitz, M. & Ullrich, R. Predictors of clinical response to gluten-free diet in patients diagnosed with diarrhea-predominant irritable bowel syndrome. Clin. Gastroenterol. Hepatol. 5, 844–850 (2007).
Chey, W. D. et al. The yield of colonoscopy in patients with non-constipated irritable bowel syndrome: results from a prospective, controlled US trial. Am. J. Gastroenterol. 105, 859–865 (2010).
Pimentel, M. Evaluating a bacterial hypothesis in IBS using a modification of Koch's postulates: part 1. Am. J. Gastroenterol. 105, 718–721 (2010).
Saad, R. J. & Chey, W. D. Breath tests for gastrointestinal disease: the real deal or just a lot of hot air? Gastroenterology 133, 1763–1766 (2007).
Posserud, I., Stotzer, P. O., Bjornsson, E. S., Abrahamsson, H. & Simren, M. Small intestinal bacterial overgrowth in patients with irritable bowel syndrome. Gut 56, 802–808 (2007).
Shah, E. D., Basseri, R. J., Chong, K. & Pimentel, M. Abnormal breath testing in IBS: a meta-analysis. Dig. Dis. Sci. 55, 2441–2449 (2010).
Lembo, A. J. et al. Use of serum biomarkers in a diagnostic test for irritable bowel syndrome. Aliment. Pharmacol. Ther. 29, 834–842 (2009).
Drossman, D. A. & Thompson, W. G. The irritable bowel syndrome: review and a graduated multicomponent treatment approach. Ann. Intern. Med. 116, 1009–1016 (1992).
Stewart, M., Meredith, L., Brown, J. B. & Galajda, J. The influence of older patient–physician communication on health and health-related outcomes. Clin. Geriatr. Med. 16, 25–36, vii–viii (2000).
Drossman, D. A. et al. A focus group assessment of patient perspectives on irritable bowel syndrome and illness severity. Dig. Dis. Sci. 54, 1532–1541 (2009).
Halpert, A. et al. Irritable bowel syndrome patients' ideal expectations and recent experiences with healthcare providers: a national survey. Dig. Dis. Sci. 55, 375–383 (2010).
Halpert, A. et al. What patients know about irritable bowel syndrome (IBS) and what they would like to know. National Survey on Patient Educational Needs in IBS and development and validation of the Patient Educational Needs Questionnaire (PEQ). Am. J. Gastroenterol. 102, 1972–1982 (2007).
Locke, G. R. 3rd, Zinsmeister, A. R., Talley, N. J., Fett, S. L. & Melton, L. J. Risk factors for irritable bowel syndrome: role of analgesics and food sensitivities. Am. J. Gastroenterol. 95, 157–165 (2000).
Stefanini, G. F. et al. Oral disodium cromoglycate treatment on irritable bowel syndrome: an open study on 101 subjects with diarrheic type. Am. J. Gastroenterol. 87, 55–57 (1992).
Stefanini, G. F., Bazzocchi, G., Prati, E., Lanfranchi, G. A. & Gasbarrini, G. Efficacy of oral disodium cromoglycate in patients with irritable bowel syndrome and positive skin prick tests to foods. Lancet 1, 207–208 (1986).
Roussos, A., Koursarakos, P., Patsopoulos, D., Gerogianni, I. & Philippou, N. Increased prevalence of irritable bowel syndrome in patients with bronchial asthma. Respir. Med. 97, 75–79 (2003).
White, A. M., Stevens, W. H., Upton, A. R., O'Byrne, P. M. & Collins, S. M. Airway responsiveness to inhaled methacholine in patients with irritable bowel syndrome. Gastroenterology 100, 68–74 (1991).
Bischoff, S. C., Mayer, J. H. & Manns, M. P. Allergy and the gut. Int. Arch. Allergy Immunol. 121, 270–283 (2000).
Carroccio, A. et al. A cytologic assay for diagnosis of food hypersensitivity in patients with irritable bowel syndrome. Clin. Gastroenterol. Hepatol. 8, 254–260 (2010).
Shepherd, S. J. & Gibson, P. R. Fructose malabsorption and symptoms of irritable bowel syndrome: guidelines for effective dietary management. J. Am. Diet. Assoc. 106, 1631–1639 (2006).
Oku, T. & Nakamura, S. Comparison of digestibility and breath hydrogen gas excretion of fructo-oligosaccharide, galactosyl-sucrose, and isomalto-oligosaccharide in healthy human subjects. Eur. J. Clin. Nutr. 57, 1150–1156 (2003).
Gibson, P. R. & Shepherd, S. J. Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. J. Gastroenterol. Hepatol. 25, 252–258 (2010).
Ford, A. C. et al. Effect of fibre, antispasmodics, and peppermint oil in the treatment of irritable bowel syndrome: systematic review and meta-analysis. BMJ 337, a2313 (2008).
Bijkerk, C. J. et al. Soluble or insoluble fibre in irritable bowel syndrome in primary care? Randomised placebo controlled trial. BMJ 339, b3154 (2009).
Khoshoo, V., Armstead, C. & Landry, L. Effect of a laxative with and without tegaserod in adolescents with constipation predominant irritable bowel syndrome. Aliment. Pharmacol. Ther. 23, 191–196 (2006).
Awad, R. A. & Camacho, S. A randomized, double-blind, placebo-controlled trial of polyethylene glycol effects on fasting and postprandial rectal sensitivity and symptoms in hypersensitive constipation-predominant irritable bowel syndrome. Colorectal Dis. doi:10.1111/j.146301318.2009.01990.x.
Johanson, J. F., Drossman, D. A., Panas, R., Wahle, A. & Ueno, R. Clinical trial: phase 2 study of lubiprostone for irritable bowel syndrome with constipation. Aliment. Pharmacol. Ther. 27, 685–696 (2008).
Drossman, D. A. et al. Clinical trial: lubiprostone in patients with constipation-associated irritable bowel syndrome—results of two randomized, placebo-controlled studies. Aliment. Pharmacol. Ther. 29, 329–341 (2009).
Lin, S. R. et al. A randomized, double-blind, placebo-controlled trial assessing the efficacy and safety of tegaserod in patients from China with chronic constipation. World J. Gastroenterol. 13, 732–739 (2007).
Chey, W. D., Pare, P., Viegas, A., Ligozio, G. & Shetzline, M. A. Tegaserod for female patients suffering from IBS with mixed bowel habits or constipation: a randomized controlled trial. Am. J. Gastroenterol. 103, 1217–1225 (2008).
Ford, A. C. et al. Efficacy of 5-HT3 antagonists and 5-HT4 agonists in irritable bowel syndrome: systematic review and meta-analysis. Am. J. Gastroenterol. 104, 1831–1843 (2009).
Thompson, C. A. Novartis suspends tegaserod sales at FDA's request. Am. J. Health Syst. Pharm. 64, 1020 (2007).
Hovdenak, N. Loperamide treatment of the irritable bowel syndrome. Scand. J. Gastroenterol. Suppl. 130, 81–84 (1987).
Lavo, B., Stenstam, M. & Nielsen, A. L. Loperamide in treatment of irritable bowel syndrome—a double-blind placebo controlled study. Scand. J. Gastroenterol. Suppl. 130, 77–80 (1987).
Efskind, P. S., Bernklev, T. & Vatn, M. H. A double-blind placebo-controlled trial with loperamide in irritable bowel syndrome. Scand. J. Gastroenterol. 31, 463–468 (1996).
Grundmann, O. & Yoon, S. L. Irritable bowel syndrome: epidemiology, diagnosis and treatment: an update for health-care practitioners. J. Gastroenterol. Hepatol. 25, 691–699 (2010).
Chang, L. et al. Incidence of ischemic colitis and serious complications of constipation among patients using alosetron: systematic review of clinical trials and post-marketing surveillance data. Am. J. Gastroenterol. 101, 1069–1079 (2006).
Chang, L. et al. A dose-ranging, phase II study of the efficacy and safety of alosetron in men with diarrhea-predominant IBS. Am. J. Gastroenterol. 100, 115–123 (2005).
Chey, W. D. et al. Long-term safety and efficacy of alosetron in women with severe diarrhea-predominant irritable bowel syndrome. Am. J. Gastroenterol. 99, 2195–2203 (2004).
Chang, L., Tong, K. & Ameen, V. Ischemic colitis and complications of constipation associated with the use of alosetron under a risk management plan: clinical characteristics, outcomes, and incidences. Am. J. Gastroenterol. 105, 866–875 (2010).
Lembo, A. et al. Rifaximin for the treatment of diarrhea-associated irritable bowel syndrome: short term treatment leading to long term sustained response. Gastroenterology 134 (Suppl. 1), A-545 (2008).
Pimentel, M. et al. Rifaximin treatment for 2 weeks provides acute and sustained relief over 12 weeks of IBS symptoms in non-constipated irritable bowel syndrome: results from 2 North American phase 3 trials (Target 1 and Target 2). Gastroenterology 138 (Suppl. 1), S-64–S-65 (2010).
Sharara, A. I. et al. A randomized double-blind placebo-controlled trial of rifaximin in patients with abdominal bloating and flatulence. Am. J. Gastroenterol. 101, 326–333 (2006).
Peralta, S., Cottone, C., Doveri, T., Almasio, P. L. & Craxi, A. Small intestine bacterial overgrowth and irritable bowel syndrome-related symptoms: experience with rifaximin. World J. Gastroenterol. 15, 2628–2631 (2009).
Tursi, A., Brandimarte, G., Giorgetti, G. M. & Elisei, W. Assessment of small intestinal bacterial overgrowth in uncomplicated acute diverticulitis of the colon. World J. Gastroenterol. 11, 2773–2776 (2005).
Darvish-Damavandi, M., Nikfar, S. & Abdollahi, M. A systematic review of efficacy and tolerability of mebeverine in irritable bowel syndrome. World J. Gastroenterol. 16, 547–553 (2010).
Grover, M. & Drossman, D. A. Psychotropic agents in functional gastrointestinal disorders. Curr. Opin. Pharmacol. 8, 715–723 (2008).
Su, X. & Gebhart, G. F. Effects of tricyclic antidepressants on mechanosensitive pelvic nerve afferent fibers innervating the rat colon. Pain 76, 105–114 (1998).
Morgan, V., Pickens, D., Gautam, S., Kessler, R. & Mertz, H. Amitriptyline reduces rectal pain related activation of the anterior cingulate cortex in patients with irritable bowel syndrome. Gut 54, 601–607 (2005).
Ford, A. C., Talley, N. J., Schoenfeld, P. S., Quigley, E. M. & Moayyedi, P. Efficacy of antidepressants and psychological therapies in irritable bowel syndrome: systematic review and meta-analysis. Gut 58, 367–378 (2009).
Drossman, D. A. et al. Cognitive-behavioral therapy versus education and desipramine versus placebo for moderate to severe functional bowel disorders. Gastroenterology 125, 19–31 (2003).
Lackner, J. M. et al. Self-administered cognitive behavior therapy for moderate to severe irritable bowel syndrome: clinical efficacy, tolerability, feasibility. Clin. Gastroenterol. Hepatol. 6, 899–906 (2008).
Lackner, J. M. et al. Rapid response to cognitive behavior therapy predicts treatment outcome in patients with irritable bowel syndrome. Clin. Gastroenterol. Hepatol. 8, 426–432 (2010).
Reme, S. E., Kennedy, T., Jones, R., Darnley, S. & Chalder, T. Predictors of treatment outcome after cognitive behavior therapy and antispasmodic treatment for patients with irritable bowel syndrome in primary care. J. Psychosom. Res. 68, 385–388 (2010).
Drossman, D. A. et al. Alterations of brain activity associated with resolution of emotional distress and pain in a case of severe irritable bowel syndrome. Gastroenterology 124, 754–761 (2003).
Blanchard, E. B. et al. Prediction of outcome from cognitive-behavioral treatment of irritable bowel syndrome. Behav. Res. Ther. 30, 647–650 (1992).
Blanchard, E. B. et al. Prediction of treatment outcome among patients with irritable bowel syndrome treated with group cognitive therapy. Behav. Res. Ther. 44, 317–337 (2006).
Webb, A. N., Kukuruzovic, R. H., Catto-Smith, A. G. & Sawyer, S. M. Hypnotherapy for treatment of irritable bowel syndrome. Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD005110. doi:10.1002/14651858.CD005110.pub2. (2007).
Whorwell, P. J., Prior, A. & Faragher, E. B. Controlled trial of hypnotherapy in the treatment of severe refractory irritable-bowel syndrome. Lancet 2, 1232–1234 (1984).
Gonsalkorale, W. M., Houghton, L. A. & Whorwell, P. J. Hypnotherapy in irritable bowel syndrome: a large-scale audit of a clinical service with examination of factors influencing responsiveness. Am. J. Gastroenterol. 97, 954–961 (2002).
Spiller, R. Review article: probiotics and prebiotics in irritable bowel syndrome. Aliment. Pharmacol. Ther. 28, 385–396 (2008).
Brenner, D. M., Moeller, M. J., Chey, W. D. & Schoenfeld, P. S. The utility of probiotics in the treatment of irritable bowel syndrome: a systematic review. Am. J. Gastroenterol. 104, 1033–1049 (2009).
O'Mahony, L. et al. Lactobacillus and bifidobacterium in irritable bowel syndrome: symptom responses and relationship to cytokine profiles. Gastroenterology 128, 541–551 (2005).
Whorwell, P. J. et al. Efficacy of an encapsulated probiotic Bifidobacterium infantis 35624 in women with irritable bowel syndrome. Am. J. Gastroenterol. 101, 1581–1590 (2006).
Lim, B. et al. Acupuncture for treatment of irritable bowel syndrome. Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD005111. doi:10.1002/14651858.CD005111.pub2 (2006).
Schneider, A. et al. Acupuncture treatment in irritable bowel syndrome. Gut 55, 649–654 (2006).
Lembo, A. J. et al. A treatment trial of acupuncture in IBS patients. Am. J. Gastroenterol. 104, 1489–1497 (2009).
Kaptchuk, T. J. et al. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ 336, 999–1003 (2008).
Liu, J. P., Yang, M., Liu, Y. X., Wei, M. L. & Grimsgaard, S. Herbal medicines for treatment of irritable bowel syndrome. Cochrane Database of Systematic Reviews, Issue 1. Art. No.: CD004116. doi:10.1002/14651858.CD004116.pub2 (2006).
Adeyemo, M. A. & Chang, L. New treatments for irritable bowel syndrome in women. Womens Health (Lond. Engl.) 4, 605–622 (2008).
Camilleri, M. & Chang, L. Challenges to the therapeutic pipeline for irritable bowel syndrome: end points and regulatory hurdles. Gastroenterology 135, 1877–1891 (2008).
Simren, M., Abrahamsson, H., Bajor, A. & Graffner, H. The IBAT inhibitor A3309—a promising treatment option for patients with chronic idiopathic constipation (Cic). Gastroenterology 138 (Suppl. 1), S223 (2010).
Rao, A. et al. Dose-related effects of chenodeoxycholate on gastrointestinal and colonic transit and bowel function in female patients with constipation-predominant irritable bowel syndrome. Gastroenterology 138 (Suppl. 1), S224 (2010).
Tack, J. et al. AST-120 (spherical carbon adsorbent) improves pain and bloating in a randomized, double-blind, placebo-controlled trial in patients with non-constipating irritable bowel syndrome (IBS). Gastroenterology 138, (Suppl. 1), S223 (2010).
Brown, P. et al. LX1031, a novel locally-acting inhibitor of serotonin (5-HT) synthesis significantly improves symptoms in patients with IBS. Gastroenterology 138 (Suppl. 1), S129 (2010).
Hellstrom, P. M. GLP-1 playing the role of a gut regulatory compound. Acta Physiol. (Oxf.) doi:10.1111/j.1748-1716.2010.02150.x.
Acknowledgements
Charles P. Vega, University of California, Irvine, CA, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the MedscapeCME-accredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Contributions
Both authors contributed equally to the research, discussion, writing and reviewing of the article.
Corresponding author
Ethics declarations
Competing interests
S. Khan declares no competing interests. L. Chang has served as a consultant for Albireo, Forest, GlaxoSmithKline, Ironwood, McNeil, Movetis, Ocera, Prometheus Laboratories, Rose Pharma, Salix and Takeda. She has received research funding from Takeda, Rose and Prometheus.
Rights and permissions
About this article
Cite this article
Khan, S., Chang, L. Diagnosis and management of IBS. Nat Rev Gastroenterol Hepatol 7, 565–581 (2010). https://doi.org/10.1038/nrgastro.2010.137
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2010.137
This article is cited by
-
A neuropsychosocial signature predicts longitudinal symptom changes in women with irritable bowel syndrome
Molecular Psychiatry (2022)
-
Evidence-based clinical practice guidelines for irritable bowel syndrome 2020
Journal of Gastroenterology (2021)
-
Adherence to the pro-inflammatory diet in relation to prevalence of irritable bowel syndrome
Nutrition Journal (2019)
-
Health education program improves QOL in students with irritable bowel syndrome after the Wenchuan earthquake: a five-year multi-center study
BMC Gastroenterology (2018)
-
Comparison of Symptoms, Healthcare Utilization, and Treatment in Diagnosed and Undiagnosed Individuals With Diarrhea-Predominant Irritable Bowel Syndrome
American Journal of Gastroenterology (2017)