Abstract
Niacin, or water-soluble vitamin B3, when given at pharmacologic doses, is a powerful lipid-altering agent. This drug, which lowers the levels of atherogenic, apolipoprotein-B-containing lipoproteins, is one of few medications that can raise the levels of atheroprotective HDL cholesterol. Niacin also has beneficial effects on other cardiovascular risk factors, including lipoprotein(a), C-reactive protein, platelet-activating factor acetylhydrolase, plasminogen activator inhibitor 1 and fibrinogen. Many clinical trials have confirmed the lipid effects of niacin treatment; however, its effects on cardiovascular outcomes have been called into question owing to the AIM-HIGH trial, which showed no benefit of niacin therapy on cardiovascular endpoints. Furthermore, use of niacin has historically been limited by tolerability issues. In addition to flushing, worsened hyperglycaemia among patients with diabetes mellitus has also been a concern with niacin therapy. This article reviews the utility of niacin including its mechanism of action, clinical trial data regarding cardiovascular outcomes, adverse effect profile and strategies to address these effects and improve compliance.
Key Points
-
Niacin exerts several beneficial lipid-altering effects, including lowering the levels of all atherogenic particles that contain apolipoprotein B, such as LDL, VLDL, IDL and lipoprotein(a), and raising HDL cholesterol levels
-
Niacin should be used in the immediate-release or extended-release forms only, as the sustained-release preparations have been associated with hepatotoxicity
-
Compliance with niacin can be hindered by flushing, gastrointestinal and metabolic effects; of these, flushing is the most common reason for discontinuation of niacin therapy
-
Symptoms of flushing can be alleviated if the possibility of flushing is discussed in advance and advice is given to take a low-fat snack and a nonsteroidal anti-inflammatory drug and to avoid hot or spicy foods at the time of niacin ingestion
-
Use of niacin in patients with diabetes mellitus is often constrained by concern over provoking hyperglycaemia, but evidence would suggest that increases in plasma glucose levels are modest and transient
-
Despite the disappointing results of the AIM-HIGH trial, the relation between niacin therapy and cardiovascular disease endpoints remains yet to be fully defined by larger and more definitive clinical trials
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 285, 2486–2497 (2001).
Gordon, T., Castelli, W. P., Hjortland, M. C., Kannel, W. B. & Dawber, T. R. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am. J. Med. 62, 707–714 (1977).
Di Angelantonio, E. et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA 302, 1993–2000 (2009).
Sviridov, D. & Nestel, P. J. Genetic factors affecting HDL levels, structure, metabolism and function. Curr. Opin. Lipidol. 18, 157–163 (2007).
Yoshikawa, M., Sakuma, N., Hibino, T., Sato, T. & Fujinami, T. HDL3 exerts more powerful anti-oxidative, protective effects against copper-catalyzed LDL oxidation than HDL2. Clin. Biochem. 30, 221–225 (1997).
Asztalos, B. F. et al. High-density lipoprotein subpopulation profile and coronary heart disease prevalence in male participants of the Framingham Offspring Study. Arterioscler. Thromb. Vasc. Biol. 24, 2181–2187 (2004).
Asztalos, B. F. et al. Value of high-density lipoprotein (HDL) subpopulations in predicting recurrent cardiovascular events in the Veterans Affairs HDL Intervention Trial. Arterioscler. Thromb. Vasc. Biol. 25, 2185–2191 (2005).
Ballantyne, F. C., Clark, R. S., Simpson, H. S. & Ballantyne, D. High density and low density lipoprotein subfractions in survivors of myocardial infarction and in control subjects. Metabolism 31, 433–437 (1982).
Jacobs, M. J. et al. Prevalence and control of dyslipidemia among persons with diabetes in the United States. Diabetes Res. Clin. Pract. 70, 263–269 (2005).
Hoang, A. et al. Advanced glycation of apolipoprotein A-I impairs its anti-atherogenic properties. Diabetologia 50, 1770–1779 (2007).
Nobécourt, E. et al. Nonenzymatic glycation impairs the antiinflammatory properties of apolipoprotein A-I. Arterioscler. Thromb. Vasc. Biol. 30, 766–772 (2010).
Kontush, A. & Chapman, M. J. Functionally defective high-density lipoprotein: a new therapeutic target at the crossroads of dyslipidemia, inflammation, and atherosclerosis. Pharmacol. Rev. 58, 342–374 (2006).
Drew, B. G. et al. High-density lipoprotein modulates glucose metabolism in patients with type 2 diabetes mellitus. Circulation 119, 2103–2111 (2009).
Kruit, J. K., Brunham, L. R., Verchere, C. B. & Hayden, M. R. HDL and LDL cholesterol significantly influence β-cell function in type 2 diabetes mellitus. Curr. Opin. Lipidol. 21, 178–185 (2010).
Fryirs, M. A. et al. Effects of high-density lipoproteins on pancreatic β-cell insulin secretion. Arterioscler. Thromb. Vasc. Biol. 30, 1642–1648 (2010).
Farmer, J. A. Nicotinic acid: a new look at an old drug. Curr. Atheroscler. Rep. 11, 87–92 (2009).
[No authors listed] Clofibrate and niacin in coronary heart disease. JAMA 231, 360–381 (1975).
Brown, B. G. et al. Simvastatin and niacin, antioxidant vitamins, or the combination for the prevention of coronary disease. N. Engl. J. Med. 345, 1583–1592 (2001).
Carlson, L. A. & Rosenhamer, G. Reduction of mortality in the Stockholm Ischaemic Heart Disease Secondary Prevention Study by combined treatment with clofibrate and nicotinic acid. Acta Med. Scand. 223, 405–418 (1988).
Blankenhorn, D. H. et al. Beneficial effects of combined colestipol-niacin therapy on coronary atherosclerosis and coronary venous bypass grafts. JAMA 257, 3233–3240 (1987).
Brown, G. et al. Regression of coronary artery disease as a result of intensive lipid-lowering therapy in men with high levels of apolipoprotein B. N. Engl. J. Med. 323, 1289–1298 (1990).
Taylor, A. J., Sullenberger, L. E., Lee, H. J., Lee, J. K. & Grace, K. A. Arterial Biology for the Investigation of the Treatment Effects of Reducing Cholesterol (ARBITER) 2: a double-blind, placebo-controlled study of extended-release niacin on atherosclerosis progression in secondary prevention patients treated with statins. Circulation 110, 3512–3517 (2004).
Taylor, A. J., Lee, H. J. & Sullenberger, L. E. The effect of 24 months of combination statin and extended-release niacin on carotid intima-media thickness: ARBITER 3. Curr. Med. Res. Opin. 22, 2243–2250 (2006).
Rosenson, R. S. Measure for measure—sugar or fats? Reconciling cardiovascular and diabetes risk with niacin therapy. Nat. Clin. Pract. Endocrinol. Metab. 3, 72–73 (2007).
Ginsberg, H. N. Niacin in the metabolic syndrome: more risk than benefit? Nat. Clin. Pract. Endocrinol. Metab. 2, 300–301 (2006).
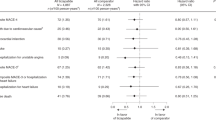
Boden, W. E. et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N. Engl. J. Med. 365, 2255–2267 (2011).
Altschul, R., Hoffer, A. & Stephen, J. D. Influence of nicotinic acid on serum cholesterol in man. Arch. Biochem. Biophys. 54, 558–559 (1955).
Piepho, R. W. The pharmacokinetics and pharmacodynamics of agents proven to raise high-density lipoprotein cholesterol. Am. J. Cardiol. 86, 35L–40L (2000).
Gille, A., Bodor, E. T., Ahmed, K. & Offermanns, S. Nicotinic acid: pharmacological effects and mechanisms of action. Annu. Rev. Pharmacol. Toxicol. 48, 79–106 (2008).
Dalton, T. A. & Berry, R. S. Hepatotoxicity associated with sustained-release niacin. Am. J. Med. 93, 102–104 (1992).
Etchason, J. A. et al. Niacin-induced hepatitis: a potential side effect with low-dose time-release niacin. Mayo Clin. Proc. 66, 23–28 (1991).
Fischer, D. J., Knight, L. L. & Vestal, R. E. Fulminant hepatic failure following low-dose sustained-release niacin therapy in hospital. West J. Med. 155, 410–412 (1991).
Alsheikh-Ali, A. A. & Karas, R. H. The safety of niacin in the US Food and Drug Administration adverse event reporting database. Am. J. Cardiol. 101, 9B–13B (2008).
Knopp, R. H. et al. Equivalent efficacy of a time-release form of niacin (Niaspan) given once-a-night versus plain niacin in the management of hyperlipidemia. Metabolism 47, 1097–1104 (1998).
Cefali, E. A., Simmons, P. D., Stanek, E. J. & Shamp, T. R. Improved control of niacin-induced flushing using an optimized once-daily, extended-release niacin formulation. Int. J. Clin. Pharmacol. Ther. 44, 633–640 (2006).
Goldberg, A. et al. Multiple-dose efficacy and safety of an extended-release form of niacin in the management of hyperlipidemia. Am. J. Cardiol. 85, 1100–1105 (2000).
Meyers, C. D., Carr, M. C., Park, S. & Brunzell, J. D. Varying cost and free nicotinic acid content in over-the-counter niacin preparations for dyslipidemia. Ann. Intern. Med. 139, 996–1002 (2003).
Kruse, W. et al. Nocturnal inhibition of lipolysis in man by nicotinic acid and derivatives. Eur. J. Clin. Pharmacol. 16, 11–15 (1979).
Ziliotto, G. R., Lamberti, G., Wagner, A., Cima, L. & Genco, G. Comparative studies of the response of normolipemic and dyslipemic aged subjects to 2 forms of delayed-action nicotinic acid polyesters. Pentaerythrotol tetranicotinate and inositol hexanicotinate. Results of a controlled cross-over trial [Italian]. Arch. Sci. Med. (Torino) 134, 359–394 (1977).
Soga, T. et al. Molecular identification of nicotinic acid receptor. Biochem. Biophys. Res. Commun. 303, 364–369 (2003).
Tunaru, S. et al. PUMA-G and HM74 are receptors for nicotinic acid and mediate its anti-lipolytic effect. Nat. Med. 9, 352–355 (2003).
Wise, A. et al. Molecular identification of high and low affinity receptors for nicotinic acid. J. Biol. Chem. 278, 9869–9874 (2003).
Digby, J. E., Lee, J. M. & Choudhury, R. P. Nicotinic acid and the prevention of coronary artery disease. Curr. Opin. Lipidol. 20, 321–326 (2009).
Havel, R. J. Conversion of plasma free fatty acids into triglycerides of plasma lipoprotein fractions in man. Metabolism 10, 1031–1034 (1961).
Ganji, S. H. et al. Niacin noncompetitively inhibits DGAT2 but not DGAT1 activity in HepG2 cells. J. Lipid Res. 45, 1835–1845 (2004).
Jin, F. Y., Kamanna, V. S. & Kashyap, M. L. Niacin accelerates intracellular ApoB degradation by inhibiting triacylglycerol synthesis in human hepatoblastoma (HepG2) cells. Arterioscler. Thromb. Vasc. Biol. 19, 1051–1059 (1999).
Zhang, L. H., Kamanna, V. S., Zhang, M. C. & Kashyap, M. L. Niacin inhibits surface expression of ATP synthase b chain in HepG2 cells: implications for raising HDL. J. Lipid Res. 49, 1195–1201 (2008).
Kamanna, V. S., Vo, A. & Kashyap, M. L. Nicotinic acid: recent developments. Curr. Opin. Cardiol. 23, 393–398 (2008).
Airan-Javia, S. L. et al. Atheroprotective lipoprotein effects of a niacin-simvastatin combination compared to low- and high-dose simvastatin monotherapy. Am. Heart J. 157, 687.e1–687.e8 (2009).
Blum, C. B. et al. High density lipoprotein metabolism in man. J. Clin. Invest. 60, 795–807 (1977).
Shepherd, J., Packard, C. J., Patsch, J. R., Gotto, A. M. Jr & Taunton, O. D. Effects of nicotinic acid therapy on plasma high density lipoprotein subfraction distribution and composition and on apolipoprotein A metabolism. J. Clin. Invest. 63, 858–867 (1979).
Jin, F. Y., Kamanna, V. S. & Kashyap, M. L. Niacin decreases removal of high-density lipoprotein apolipoprotein A-I but not cholesterol ester by Hep G2 cells. Implication for reverse cholesterol transport. Arterioscler. Thromb. Vasc. Biol. 17, 2020–2028 (1997).
Lamon-Fava, S. et al. Extended-release niacin alters the metabolism of plasma apolipoprotein (Apo) A-I and ApoB-containing lipoproteins. Arterioscler. Thromb. Vasc. Biol. 28, 1672–1678 (2008).
van der Hoorn, J. W. et al. Niacin increases HDL by reducing hepatic expression and plasma levels of cholesteryl ester transfer protein in APOE*3Leiden.CETP mice. Arterioscler. Thromb. Vasc. Biol. 28, 2016–2022 (2008).
Rubic, T., Trottmann, M. & Lorenz, R. L. Stimulation of CD36 and the key effector of reverse cholesterol transport ATP-binding cassette A1 in monocytoid cells by niacin. Biochem. Pharmacol. 67, 411–419 (2004).
Thoenes, M. et al. The effects of extended-release niacin on carotid intimal media thickness, endothelial function and inflammatory markers in patients with the metabolic syndrome. Int. J. Clin. Pract. 61, 1942–1948 (2007).
Carlson, L. A., Hamsten, A. & Asplund, A. Pronounced lowering of serum levels of lipoprotein Lp(a) in hyperlipidaemic subjects treated with nicotinic acid. J. Intern. Med. 226, 271–276 (1989).
Rosengren, A., Wilhelmsen, L., Eriksson, E., Risberg, B. & Wedel, H. Lipoprotein (a) and coronary heart disease: a prospective case–control study in a general population sample of middle aged men. BMJ 301, 1248–1251 (1990).
Schaefer, E. J. et al. Lipoprotein(a) levels and risk of coronary heart disease in men. The Lipid Research Clinics Coronary Primary Prevention Trial. JAMA 271, 999–1003 (1994).
Rosenson, R. S. Future role for selective phospholipase A2 inhibitors in the prevention of atherosclerotic cardiovascular disease. Cardiovasc. Drugs Ther. 23, 93–101 (2009).
Kuvin, J. T. et al. Effects of extended-release niacin on lipoprotein particle size, distribution, and inflammatory markers in patients with coronary artery disease. Am. J. Cardiol. 98, 743–745 (2006).
Heinrich, J., Balleisen, L., Schulte, H., Assmann, G. & van de Loo, J. Fibrinogen and factor VII in the prediction of coronary risk. Results from the PROCAM study in healthy men. Arterioscler. Thromb. 14, 54–59 (1994).
Meade, T. W. et al. Haemostatic function and cardiovascular death: early results of a prospective study. Lancet 1, 1050–1054 (1980).
Ernst, E. & Resch, K. L. Fibrinogen as a cardiovascular risk factor: a meta-analysis and review of the literature. Ann. Intern. Med. 118, 956–963 (1993).
Johansson, J. O., Egberg, N., Asplund-Carlson, A. & Carlson, L. A. Nicotinic acid treatment shifts the fibrinolytic balance favourably and decreases plasma fibrinogen in hypertriglyceridaemic men. J. Cardiovasc. Risk 4, 165–171 (1997).
Tavintharan, S., Sivakumar, M., Lim, S. C. & Sum, C. F. Niacin affects cell adhesion molecules and plasminogen activator inhibitor-1 in HepG2 cells. Clin. Chim. Acta 376, 41–44 (2007).
Rosenson, R. S. Antiatherothrombotic effects of nicotinic acid. Atherosclerosis 171, 87–96 (2003).
Westphal, S., Borucki, K., Taneva, E., Makarova, R. & Luley, C. Extended-release niacin raises adiponectin and leptin. Atherosclerosis 193, 361–365 (2007).
Ouchi, N. et al. Adipocyte-derived plasma protein, adiponectin, suppresses lipid accumulation and class A scavenger receptor expression in human monocyte-derived macrophages. Circulation 103, 1057–1063 (2001).
Bodary, P. F. & Eitzman, D. T. Adiponectin: vascular protection from the fat? Arterioscler. Thromb. Vasc. Biol. 26, 235–236 (2006).
Ganji, S. H., Qin, S., Zhang, L., Kamanna, V. S. & Kashyap, M. L. Niacin inhibits vascular oxidative stress, redox-sensitive genes, and monocyte adhesion to human aortic endothelial cells. Atherosclerosis 202, 68–75 (2009).
Canner, P. L. et al. Fifteen year mortality in Coronary Drug Project patients: long-term benefit with niacin. J. Am. Coll. Cardiol. 8, 1245–1255 (1986).
Cashin-Hemphill, L. et al. Beneficial effects of colestipol-niacin on coronary atherosclerosis. A 4-year follow-up. JAMA 264, 3013–3017 (1990).
Kane, J. P. et al. Regression of coronary atherosclerosis during treatment of familial hypercholesterolemia with combined drug regimens. JAMA 264, 3007–3012 (1990).
Whitney, E. J. et al. A randomized trial of a strategy for increasing high-density lipoprotein cholesterol levels: effects on progression of coronary heart disease and clinical events. Ann. Intern. Med. 142, 95–104 (2005).
Taylor, A. J. et al. Extended-release niacin or ezetimibe and carotid intima-media thickness. N. Engl. J. Med. 361, 2113–2122 (2009).
Bruckert, E., Labreuche, J. & Amarenco, P. Meta-analysis of the effect of nicotinic acid alone or in combination on cardiovascular events and atherosclerosis. Atherosclerosis 210, 353–361 (2010).
[No authors listed] NIH stops clinical trial on combination cholesterol treatment. National Institutes of Health [online], (2011).
Ridker, P. M. et al. HDL cholesterol and residual risk of first cardiovascular events after treatment with potent statin therapy: an analysis from the JUPITER trial. Lancet 376, 333–339 (2010).
Datar, R., Kaesemeyer, W. H., Chandra, S., Fulton, D. J. & Caldwell, R. W. Acute activation of eNOS by statins involves scavenger receptor-B1, G protein subunit Gi, phospholipase C and calcium influx. Br. J. Pharmacol. 160, 1765–1772 (2010).
US National Library of Medicine. ClinicalTrials.gov [online], (2010).
Bruckert, E., Hayem, G., Dejager, S., Yau, C. & Bégaud, B. Mild to moderate muscular symptoms with high-dosage statin therapy in hyperlipidemic patients—the PRIMO study. Cardiovasc. Drugs Ther. 19, 403–414 (2005).
Nichols, G. A. & Koro, C. E. Does statin therapy initiation increase the risk for myopathy? An observational study of 32,225 diabetic and nondiabetic patients. Clin. Ther. 29, 1761–1770 (2007).
Reiner, Z. et al. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur. Heart J. 32, 1769–1818 (2011).
Bodor, E. T. & Offermanns, S. Nicotinic acid: an old drug with a promising future. Br. J. Pharmacol. 153 (Suppl. 1), S68–S75 (2008).
Chapman, M. J. et al. Triglyceride-rich lipoproteins and high-density lipoprotein cholesterol in patients at high risk of cardiovascular disease: evidence and guidance for management. Eur. Heart J. 32, 1345–1361 (2011).
Miller, M. et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation 123, 2292–2333 (2011).
Erqou, S. et al. Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA 302, 412–423 (2009).
Greenland, P. et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 56, e50–e103 (2010).
Genest, J. et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult—2009 recommendations. Can. J. Cardiol. 25, 567–579 (2009).
Nordestgaard, B. G. et al. Lipoprotein(a) as a cardiovascular risk factor: current status. Eur. Heart J. 31, 2844–2853 (2010).
Birjmohun, R. S. et al. Safety and tolerability of prolonged-release nicotinic acid in statin-treated patients. Curr. Med. Res. Opin. 23, 1707–1713 (2007).
Guyton, J. R. & Bays, H. E. Safety considerations with niacin therapy. Am. J. Cardiol. 99, 22C–31C (2007).
Carlson, L. A. Nicotinic acid: the broad-spectrum lipid drug. A 50th anniversary review. J. Intern. Med. 258, 94–114 (2005).
Stern, R. H., Spence, J. D., Freeman, D. J. & Parbtani, A. Tolerance to nicotinic acid flushing. Clin. Pharmacol. Ther. 50, 66–70 (1991).
McKenney, J. New perspectives on the use of niacin in the treatment of lipid disorders. Arch. Intern. Med. 164, 697–705 (2004).
Birjmohun, R. S., Hutten, B. A., Kastelein, J. J. & Stroes, E. S. Efficacy and safety of high-density lipoprotein cholesterol-increasing compounds: a meta-analysis of randomized controlled trials. J. Am. Coll. Cardiol. 45, 185–197 (2005).
Elam, M. B. et al. Effect of niacin on lipid and lipoprotein levels and glycemic control in patients with diabetes and peripheral arterial disease: the ADMIT study: A randomized trial. Arterial Disease Multiple Intervention Trial. JAMA 284, 1263–1270 (2000).
Benyó, Z., Gille, A., Bennett, C. L., Clausen, B. E. & Offermanns, S. Nicotinic acid-induced flushing is mediated by activation of epidermal Langerhans cells. Mol. Pharmacol. 70, 1844–1849 (2006).
Guyton, J. R. Niacin in cardiovascular prevention: mechanisms, efficacy, and safety. Curr. Opin. Lipidol. 18, 415–420 (2007).
Cheng, K. et al. Antagonism of the prostaglandin D2 receptor 1 suppresses nicotinic acid-induced vasodilation in mice and humans. Proc. Natl Acad. Sci. USA 103, 6682–6687 (2006).
Dunn, R. T., Ford, M. A., Rindone, J. P. & Kwiecinski, F. A. Low-dose Aspirin and ibuprofen reduce the cutaneous reactions following niacin administration. Am. J. Ther. 2, 478–480 (1995).
Thakkar, R. B. et al. Acetylsalicylic acid reduces niacin extended-release-induced flushing in patients with dyslipidemia. Am. J. Cardiovasc. Drugs 9, 69–79 (2009).
Cefali, E. A., Simmons, P. D., Stanek, E. J., McGovern, M. E. & Kissling, C. J. Aspirin reduces cutaneous flushing after administration of an optimized extended-release niacin formulation. Int. J. Clin. Pharmacol. Ther. 45, 78–88 (2007).
Whelan, A. M., Price, S. O., Fowler, S. F. & Hainer, B. L. The effect of aspirin on niacin-induced cutaneous reactions. J. Fam. Pract. 34, 165–168 (1992).
Wilkin, J. K. et al. Aspirin blocks nicotinic acid-induced flushing. Clin. Pharmacol. Ther. 31, 478–482 (1982).
Jungnickel, P. W., Maloley, P. A., Vander Tuin, E. L., Peddicord, T. E. & Campbell, J. R. Effect of two aspirin pretreatment regimens on niacin-induced cutaneous reactions. J. Gen. Intern. Med. 12, 591–596 (1997).
Oberwittler, H. & Baccara-Dinet, M. Clinical evidence for use of acetyl salicylic acid in control of flushing related to nicotinic acid treatment. Int. J. Clin. Pract. 60, 707–715 (2006).
Maccubbin, D. et al. Flushing profile of extended-release niacin/laropiprant versus gradually titrated niacin extended-release in patients with dyslipidemia with and without ischemic cardiovascular disease. Am. J. Cardiol. 104, 74–81 (2009).
Andersson, S., Carlson, L. A., Orö, L. & Richards, E. A. Effect of nicotinic acid on gastric secretion of acid in human subjects and in dogs. Scand. J. Gastroenterol. 6, 693–698 (1971).
Garg, A. & Grundy, S. M. Nicotinic acid as therapy for dyslipidemia in non-insulin-dependent diabetes mellitus. JAMA 264, 723–726 (1990).
Zhao, X. Q. et al. Safety and tolerability of simvastatin plus niacin in patients with coronary artery disease and low high-density lipoprotein cholesterol (The HDL Atherosclerosis Treatment Study). Am. J. Cardiol. 93, 307–312 (2004).
Grundy, S. M. et al. Efficacy, safety, and tolerability of once-daily niacin for the treatment of dyslipidemia associated with type 2 diabetes: results of the assessment of diabetes control and evaluation of the efficacy of niaspan trial. Arch. Intern. Med. 162, 1568–1576 (2002).
Ambegaonkar, B. M., Wentworth, C., Allen, C. & Sazonov, V. Association between extended-release niacin treatment and glycemic control in patients with type 2 diabetes mellitus: analysis of an administrative-claims database. Metabolism 60, 1038–1044 (2011).
Goldberg, R. B. & Jacobson, T. A. Effects of niacin on glucose control in patients with dyslipidemia. Mayo Clin. Proc. 83, 470–478 (2008).
Gershon, S. L. & Fox, I. H. Pharmacologic effects of nicotinic acid on human purine metabolism. J. Lab. Clin. Med. 84, 179–186 (1974).
Cooper, K. J. et al. Lack of effect of ketoconazole on the pharmacokinetics of rosuvastatin in healthy subjects. Br. J. Clin. Pharmacol. 55, 94–99 (2003).
Rätz Bravo, A. E. et al. Prevalence of potentially severe drug-drug interactions in ambulatory patients with dyslipidaemia receiving HMG-CoA reductase inhibitor therapy. Drug Saf. 28, 263–275 (2005).
Gaudineau, C. & Auclair, K. Inhibition of human P450 enzymes by nicotinic acid and nicotinamide. Biochem. Biophys. Res. Commun. 317, 950–956 (2004).
Lee, J. M. et al. Effects of high-dose modified-release nicotinic acid on atherosclerosis and vascular function: a randomized, placebo-controlled, magnetic resonance imaging study. J. Am. Coll. Cardiol. 54, 1787–1794 (2009).
Author information
Authors and Affiliations
Contributions
J. C. Creider and T. R. Joy researched the data for the article. All authors provided a substantial contribution to discussions of the content, contributed equally to writing the article and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
J. C. Creider declares no competing interests. R. A. Hegele declares associations with the following companies: Abbott (consultant; speakers bureau [honoraria]), AstraZeneca (consultant; speakers bureau [honoraria]; grant/research support), Merck (consultant; speakers bureau [honoraria]; grant/research support), Pfizer (grant/research support), Sepracor (consultant; speakers bureau [honoraria]). T. R. Joy declares associations with the following companies: Eli Lilly (speakers bureau [honoraria]), GlaxoSmithKline (speakers bureau [honoraria]), Merck (consultant; speakers bureau [honoraria]), Novo Nordisk (consultant; speakers bureau [honoraria]), Sanofi (consultant), Sepracor (consultant; speakers bureau [honoraria]).
Rights and permissions
About this article
Cite this article
Creider, J., Hegele, R. & Joy, T. Niacin: another look at an underutilized lipid-lowering medication. Nat Rev Endocrinol 8, 517–528 (2012). https://doi.org/10.1038/nrendo.2012.22
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrendo.2012.22
This article is cited by
-
Niacin-mediated rejuvenation of macrophage/microglia enhances remyelination of the aging central nervous system
Acta Neuropathologica (2020)
-
Current drugs, targets, and drug delivery systems for the treatment of dyslipidemia
Journal of Pharmaceutical Investigation (2018)
-
Progress in the care of common inherited atherogenic disorders of apolipoprotein B metabolism
Nature Reviews Endocrinology (2016)
-
Sildenafil Therapy Normalizes the Aberrant Metabolomic Profile in the Comt−/− Mouse Model of Preeclampsia/Fetal Growth Restriction
Scientific Reports (2015)
-
Targeting Lipoprotein (a): an Evolving Therapeutic Landscape
Current Atherosclerosis Reports (2015)