Abstract
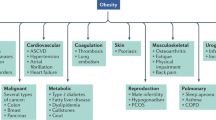
For obese individuals, successful weight loss and maintenance are notoriously difficult. Traditional drug development fails to exploit knowledge of the psychological factors that crucially influence appetite, concentrating instead on restrictive criteria of intake and weight reduction, allied to a mechanistic view of energy regulation. Drugs are under development that may produce beneficial changes in appetite expression in the obese. These currently include glucagon-like peptide-1 analogs such as liraglutide, an amylin analog davalintide, the 5-HT2C receptor agonist lorcaserin, the monoamine re-uptake inhibitor tesofensine, and a number of combination therapies such as pramlintide and metreleptin, bupropion and naltrexone, phentermine and topiramate, and bupropion and zonisamide. However, the effects of these treatments on eating behavior remain poorly characterized. Obesity is typically a consequence of overconsumption driven by an individual's natural sensitivity to food stimuli and the pleasure derived from eating. Intuitively, these processes should be effective targets for pharmacotherapy, and behavioral analysis can identify drugs that selectively affect desire to eat, enjoyment of eating, satiation or postmeal satiety. Rational interventions designed specifically to modulate these processes could limit the normally aversive consequences of caloric restriction and maximize an individual's capacity to successfully gain control over their appetite.
Key Points
-
Traditional antiobesity drug development focuses on weight and obesity-related disease end points, without adequate consideration of behavioral and psychological changes that initiate weight gain or that impede weight management
-
Classical energy homeostasis models emphasize energy regulation systems, but fail to acknowledge key motivational, emotional and behavioral factors that contribute to energy intake and the propensity to gain weight
-
Drug efficacy has been limited, as key behavioral features of appetite have been ignored—namely, hedonic aspects of consumption and the powerful influence of the environment in triggering overeating
-
Pharmaceutical companies are beginning to focus on treatments that combine existing compounds to exploit additive, or supra-additive, actions of separate agents
-
This approach could be advanced by exploiting the specific actions of drugs on distinct components of eating motivation rather than merely emphasizing simple effects on energy intake and body weight
-
Behavioral analysis can isolate drugs that reduce the desire to eat by acting on the processes that initiate, sustain and terminate meals or inhibit consumption
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Brown, W. J., Williams, L., Ford, J. H., Ball, K. & Dobson, A. J. Identifying the energy gap: magnitude and determinants of 5-year weight gain in mid-age women. Obes. Res. 13, 1431–1441 (2005).
National Institute for Clinical Excellence. Obesity: the prevention, identification, assessment and management of overweight and obesity in adults and children [online], (2006).
Pasman, W. J., Saris, W. H. & Westerterp-Plantenga, M. S. Predictors of weight maintenance. Obes. Res. 7, 43–50 (2006).
Keys, A., Brozek, J., Henschel, A., Mickelsen, O. & Taylor, H. L. The Biology of Human Starvation (2 volumes) (University of Minnesota Press, Minneapolis, 1950).
Warren, C. & Cooper, P. J. Psychological effects of dieting. Br. J. Clin. Psychol. 27, 269–270 (1988).
Ogden, J. & Evans, C. The problem with weighing: Effects of mood, self-esteem and body image. Int. J. Obes. Relat. Metab. Disord. 20, 272–277 (1996).
Laessle, R. G., Platte, P., Schweiger, U. & Pirke, K. M. Biological and psychological correlates of intermittent dieting behavior in young women. A model for bulimia nervosa. Physiol. Behav. 60, 1–5 (1996).
Halford, J. C. Clinical pharmacotherapy for obesity: current drugs and those in advanced development. Curr. Drug Targets 5, 637–646 (2004).
O'Donovan, D., Feinle-Bisset, C., Wishart, J. & Horowitz, M. Lipase inhibition attenuates the acute inhibitory effects of oral fat on food intake in healthy subjects. Br. J. Nutr. 90, 849–852 (2003).
Swhwizer, A. et al. Role of lipase in the regulation of upper gastrointestinal function in humans. Am. J. Physiol. 273, G612–G620 (1997).
Rosenbaum, M. et al. Low-dose leptin reverses sketetal muscle, autonomic, and neuroendocrine adaptation to maintenance of reduced body weight. J. Clin. Invest. 115, 3579–3586 (2005).
Mars, M., de Graaf, C., de Groot, C. P., van Rossum, C. T. & Kok, F. J. Fasting leptin and appetite responses induced by a 4-day 65%-energy-restricted diet. Int. J. Obes. 30, 122–128 (2006).
Blundell, J. E. & Halford, J. C. Regulation of nutrient supply: the brain and appetite control. Proc. Nutr. Soc. 53, 407–418 (1994).
Halford, J. C. & Blundell, J. E. Separate systems for serotonin and leptin in appetite control. Ann. Med. 32, 222–232 (2000).
Mela, D. J. Eating for pleasure or just wanting to eat? Reconsidering sensory hedonic responses as a driver of obesity. Appetite 47, 10–17 (2006).
Finlayson, G., King, N. & Blundell, J. E. Liking vs wanting food: importance for human appetite control and weight regulation. Neurosci. Biobehav. Rev. 31, 987–1002 (2007).
Rankinen, T. et al. The human obesity gene map: The 2005 update. Obesity 14, 529–644 (2006).
O'Rahilly, S. & Farooqi, I. S. Genetics of obesity. Philos. Trans. R. Soc. Lond. B Biol. Sci. 361, 1095–1105 (2006).
Blundell, J. E. et al. Resistance and susceptibility to weight gain: individual variability in response to a high fat diet. Physiol. Behav. 86, 614–622 (2005).
Wardle, J. et al. Obesity associated genetic variation in FTO is associated with diminished satiety. J. Clin. Endocrinol. Metab. 93, 3640–3643 (2008).
Cecil, J. E., Tavendale, R., Watt, P., Hetherington, M. M. & Palmer, C. N. An obesity-associated FTO gene variant and increased energy intake in children. N. Engl. J. Med. 359, 2558–2566 (2008).
Wardle, J., Llewellyn, C., Sanderson, S. & Plomin, R. The FTO gene and measured food intake in children. Int. J. Obes. 33, 42–45 (2009).
Haupt, A. et al. Variation in the FTO gene influences food intake but not energy expenditure. Exp. Clin. Endocrinol. Diabetes 117, 194–197 (2009).
Spiegel, T. A., Wadden, T. A. & Foster, G. D. Objective measurement of eating rate during behavioral treatment of obesity. Behav. Ther. 22, 61–67 (1991).
Barkeling, B., Ekman, S. & Rössner, S. Eating behaviour in obese and normal weight 11-year-old children. Int. J. Obes. Relat. Metab. Disord. 16, 335–360 (1992).
Laessle, R. G., Lehrke, S. & Dückers, S. Laboratory eating behavior in obesity. Appetite 49, 399–404 (2007).
Meyer, J. E. & Pudel, V. Experimental studies on food-intake in obese and normal weight subjects. J. Psychosom. Res. 16, 305–308 (1972).
Stunkard, A. & Kaplan, D. Eating in public places: a review of reports of the direct observation of eating behavior. Int. J. Obes. 1, 89–101 (1977).
Näslund, E., Gutniak, M., Skogar, S., Rössner, S. & Hellström, P. M. Glucagon-like peptide 1 increases the period of postprandial satiety and slows gastric emptying in obese men. Am. J. Clin. Nutr. 68, 525–530 (1998).
Lindgren, A. C. et al. Eating behaviour in Prader–Willi syndrome, normal weight and obese control groups. J. Pediatr. 137, 50–55 (2000).
Williamson, D. A. et al. Microanalysis of eating behavior of three leptin deficient adults treated with leptin therapy. Appetite 45, 75–80 (2005).
Otsuka, R. et al. Eating fast leads to obesity: Findings based on self-administered questionnaires among middle-aged Japanese men and women. J. Epidemiol. 16, 117–124 (2006).
Maruyama, K. et al. The joint impact on being overweight of self reported behaviours of eating quickly and eating until full: cross sectional survey. BMJ 337, a2002 (2008).
Llewellyn, C. H., van Jaarsveld, C. H., Boniface, D., Carnell, S. & Wardle, J. Eating rate is a heritable phenotype related to weight in children. Am. J. Clin. Nutr. 88, 1560–1566 (2008).
Pearcey, S. M. & de Castro, J. M. Food intake and meal patterns of weight-stable and weight-gaining persons. Am. J. Clin. Nutr. 76, 107–112 (2002).
Rissanen, A. et al. Acquired preference especially for dietary fat and obesity: a study of weight-discordant monozygotic twin pairs. Int. J. Obes. Relat. Metab. Disord. 26, 973–977 (2002).
Bray, G. A., Paeratakul, S. & Popkin, B. M. Dietary fat and obesity: a review of animal, clinical and epidemiological studies. Physiol. Behav. 83, 549–555 (2004).
Kral, T. V., Roe, L. S. & Rolls, B. J. Combined effects of energy density and portion size on energy intake in women. Am. J. Clin. Nutr. 79, 962–968 (2004).
Geliebter, A. & Hashim, S. A. Gastric capacity in normal obese, and bulimic women. Physiol. Behav. 74, 743–746 (2001).
Geliebter, A., Yahav, E. K., Gluck, M. E. & Hashim, S. A. Gastric capacity, test meal intake, and appetitive hormones in binge eating disorder. Physiol. Behav. 81, 735–740 (2004).
Ranganath, L. R. et al. Attenuated GLP-1 secretion in obesity: cause or consequence? Gut 38, 916–919 (1996).
De Graaf, C., Blom, W. A., Smeets, P. A., Staflue, A. & Hendricks, H. F. Biomarkers of satiation and satiety. Am. J. Clin. Nutr. 17, 949–961 (2004).
Adam, T. C. & Westerterp-Plantenga, M. S. Glucagon-like peptide-1 release and satiety after a nutrient challenge in normal-weight and obese. Br. J. Nutr. 93, 845–851 (2005).
le Roux, C. W. et al. Attenuated peptide YY release in obese subjects is associated with reduced satiety. Endocrinology 147, 3–8 (2006).
Blundell, J. E. et al. Over-consumption and obesity: peptides and susceptibility to weight gain. Regul. Pept. 149, 32–38 (2008).
Matsuda, M. et al. Altered hypothalamic function in response to glucose ingestion in obese humans. Diabetes 48, 1801–1806 (1999).
Gautier, J. F. et al. Differential brain responses to satiation in obese and lean men. Diabetes 49, 838–846 (2000).
Carnell, S. & Wardle, J. Appetite and adiposity in children: evidence for a behavioral susceptibility theory of obesity. Am. J. Clin. Nutr. 88, 22–29 (2008).
Halford, J. C. et al. Beyond-brand effect of television food advertisements on food choice in children: the effects of weight status. Public Health Nutr. 11, 897–904 (2008).
Rothemund, Y. et al. Differential activation of the dorsal striatum by high-calorie visual food stimuli in obese individuals. Neuroimage 37, 410–421 (2007).
Stoeckel, L. E. et al. Widespread reward-system activation in obese women in response to pictures of high-calorie foods. Neuroimage 41, 636–647 (2008).
Drewnowski, A., Brunzell, J. D., Sande, K., Iverise, K. & Greenwood, M. R. Sweet tooth reconsidered: taste responsiveness in human obesity. Physiol. Behav. 35, 617–622 (1985).
Mela, D. J. & Sacchetti, D. A. Sensory preference for fats: relationships with diet and body composition. Am. J. Clin. Nutr. 53, 908–915 (1991).
Blundell, J. E. & Finlayson, G. Is susceptibility to weight gain characterized by homeostatic or hedonic risk factors for over-consumption? Physiol. Behav. 82, 21–25 (2004).
Hill, A. J., Rogers, P. J. & Blundell, J. E. Techniques for the experimental measurement of human eating behaviour and food intake: a practical guide. Int. J. Obes. Relat. Metab. Disord. 19, 361–375 (1995).
Blundell, J. E. et al. in Handbook of Assessment Methods for Eating Behaviors and Weight-Related Problems: Measures, Theory, and Research (eds Allison, D. B. & Baskin, M. L.) 283–326 (Sage Publications Inc., Thousand Oaks, 2009).
Halford, J. C., Harrold, J. A., Boyland, E. J., Lawton, C. L. & Blundell, J. E. Serotonergic drugs: effects on appetite expression and use for the treatment of obesity. Drugs 67, 27–55 (2007).
Flint, A., Raben, A., Blundell, J. E. & Astrup, A. Reproducibility, power and validity of visual analogue scales in assessment of appetite sensations in a single test meal studies. Int. J. Obes. Relat. Metab. Disord. 24, 38–48 (2000).
Stubbs, R. J. et al. The use of visual analogue scales to assess motivation to eat in human subjects: A review of their reliability and validity with an evaluation of new hand-held computerized systems for temporal tracking of appetite ratings. Br. J. Nutr. 84, 405–415 (2000).
Drapeau, V. et al. Appetite sensations as a marker of overall intake. Br. J. Nutr. 93, 273–280 (2005).
Drapeau, V. et al. Appetite sensations and satiety quotient: predictors of energy intake and weight loss. Appetite 48, 159–166 (2007).
Rogers, P. J. & Blundell, J. E. Effect of anorexic drugs on food intake and the micro-structure of eating in human subjects. Psychopharmacology 66, 159–165 (1979).
Yeomans, M. R. & Gray, R. W. Effects of naltrexone on food intake and changes in subjective appetite during eating: Evidence for opioid involvement in the appetizer effect. Physiol. Behav. 62, 15–21 (1997).
Halford, J. C. et al. The effects of sibutramine on the microstructure of feeding behaviour as measured by the Universal Eating Monitor (UEM). J. Psychopharmacol. 24, 99–109 (2010).
Erondu, N. et al. Neuropeptide Y5 receptor antagonism does not induce clinically meaningful weight loss in overweight and obese adults. Cell Metab. 4, 275–282 (2006).
King, N. A., Lawton, C. L., Delargy, H. J., Smith, F. C. & Blundell, J. E. in Ingestive Behavior Protocols (eds Wellmann, P. J. & Hoebel, B. G.) 71–76 (Society for the Study of Ingestive Behavior, New York, 1997).
Stubbs, R. J. et al. Description and evaluation of a Newton-based electronic appetite rating system for temporal tracking of appetite in human subjects. Physiol. Behav. 72, 615–619 (2001).
Bolger, N., Davis, A. & Rafaeli, E. Diary methods: capturing life as it is lived. Annu. Rev. Psychol. 54, 579–616 (2003).
Burton, C., Weller, D. & Sharpe, M. Are electronic diaries useful for symptoms research? A systematic review. J. Psychosom. Res. 62, 553–561 (2007).
Shiffman, S., Stone, A. A. & Hufford, M. R. Ecological momentary assessment. Annu. Rev. Clin. Psychol. 4, 1–32 (2008).
Ebner-Priemer, U. W. & Trull, T. J. Ambulatory assessment: An innovative and promising approach for clinical psychology. European Psychol. 14, 109–119 (2009).
Cappelleri, J. C. et al. Evaluating the Power of Food Scale in obese subjects and a general sample of individuals: development and measurement properties. Int. J. Obes. 33, 913–922 (2009).
Cappelleri, J. C. et al. Psychometric analysis of the Three-Factor Eating Questionnaire-R21: results from a large diverse sample of obese and non-obese participants. Int. J. Obes. 33, 611–620 (2009).
Karlsson, J., Persson, L. O., Sjöström, L. & Sullivan, M. Psychometric properties and factor structure of the three-factor eating questionnaire (TFEQ) in obese men and women, results from the Swedish obese subjects (SOS) study. Int. J. Obes. 24, 1715–1725 (2000).
Barkeling, B., King, N. A., Näslund, E. & Blundell, J. E. Characterization of obese individuals who claim to detect no relationship between their eating pattern and sensations of hunger or fullness. Int. J. Obes. 31, 435–439 (2007).
Provencher, V., Drapeau, V., Tremblay, A., Després, J. P. & Lemieux, S. Eating behaviors and indexes of body composition in men and women from the Quebéc family study. Obes. Res. 11, 783–792 (2003).
Dykes, J., Brunner, E. J., Martikeainene, P. T. & Wardle, J. Socioeconomic gradient in body size and oboist among women: The role of dietary restraint, disinhibition and hunger in the Whitehall II study. Int. J. Obes. Relat. Metab. Disord. 28, 262–268 (2004).
Lawson, O. J. et al. The association of body weight, dietary intake, and energy expenditure with dietary restraint and disinhibition. Obes. Res. 3, 153–161 (1995).
Williamson, D. A. et al. Association of body mass with dietary restraint and disinhibition. Appetite 25, 31–41 (1995).
Hays, N. P. et al. Eating behaviour correlates of adult weight gain and obesity in healthy women aged 55–65 y. Am. J. Clin. Nutr. 75, 476–483 (2002).
Bellisle, F. et al. The eating inventory and body adiposity from leanness to massive obesity: A study of 2509 adults. Obes. Res. 12, 2023–2030 (2004).
Borg, P., Fogelholm, M. & Kukkonen-Harjula, K. Food selection and eating behaviour during weight maintenance intervention and 2-y follow-up in obese men. Int. J. Obes. Relat. Metab. Disord. 28, 1548–1554 (2004).
Provencher, V. et al. Familial resemblance in eating behaviors in men and women from the Quebéc family study. Obes. Res. 13, 1624–1629 (2005).
Bouchard, L. et al. Neuromedin β: a strong candidate gene linking eating behaviors and susceptibility to obesity. Am. J. Clin. Nutr. 80, 1478–1486 (2004).
Stunkard, A. J. Eating patterns in obesity. Psychiatr. Q. 33, 284–292 (1959).
Hsu, L. K. et al. Binge eating disorder in extreme obesity. Int. J. Obes. Relat. Metab. Disord. 26, 1398–1403 (2002).
Grucza, R. A., Przybeck, T. R. & Cloninger, C. R. Prevalence and correlates of binge eating disorder in a community sample. Compr. Psychiatr. 48, 124–131 (2007).
Elfhag, K. & Rössner, S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes. Rev. 6, 67–85 (2005).
Bryant, E. J., King, N. A. & Blundell, J. E. Disinhibition: its effects on appetite and weight regulation. Obes. Rev. 9, 409–419 (2008).
Elfhag, K., Rössner, S., Barkeling, B. & Rooth, P. Sibutramine treatment in obesity: initial eating behaviour in relation to weight loss results and changes in mood. Pharmacol. Res. 51, 159–163 (2005).
Elfhag, K., Finer, N. & Rössner, S. Who will lose weight on sibutramine and orlistat? Psychological correlates for treatment success. Diabetes Obes. Metab. 10, 498–505 (2008).
Wren, A. M. et al. Ghrelin enhances appetite and increases food intake in humans. J. Clin. Endocrinol. Metab. 86, 5992–5995 (2001).
Ballinger, A., McLoughlin, L., Medbak, S. & Clark, M. Cholecystokinin is a satiety hormone in humans at physiological postprandial plasma concentrations. Clin. Sci. 89, 375–381 (1995).
Batterham, R. L. et al. Gut hormone PYY(3–36) physiologically inhibits food intake. Nature 418, 650–654 (2002).
English, P. J., Ghatei, M. A., Malik, I. A., Bloom, S. R. & Wilding, J. P. Food fails to suppress ghrelin levels in obese humans. J. Clin. Endocrinol. Metab. 87, 2984–2987 (2002).
Jordan, J. et al. Stimulation of cholecystokinin-A receptors with GI181771X does not cause weight loss in overweight or obese patients. Clin. Pharmacol. Ther. 83, 281–287 (2008).
Bojanowska, E. Physiology and pathophysiology of glucagon-like peptide 1 (GLP-1): the role of GLP-1 in the pathogenesis of diabetes mellitus, obesity, and stress. Med. Sci. Monit. 11, RA271–RA278 (2005).
Nauck, M. A. et al. Glucagon-like peptide-1 inhibition of gastric emptying outweighs its insulinotropic effects in healthy humans. Am. J. Physiol. Endocrinol. Metab. 273, E981–E988 (1997).
Little, T. J. et al. Effects of intravenous glucagon-like peptide-1 on gastric emptying and intragastric distribution in healthy subjects: relationships with postprandial glycemic and insulinemic responses. J. Clin. Endocrinol. Metab. 91, 1916–1923 (2006).
Flint, A., Raben, A., Astrup, A. & Holst, J. J. Glucagon-like peptide 1 promotes satiety and suppresses energy intake in humans. J. Clin. Invest. 101, 515–520 (1998).
Gutzwiller, J. P. et al. Glucagon-like peptide-1: a potent regulator of food intake in humans. Gut 44, 81–86 (1999).
Degen, L. et al. Effects of a preload on reduction of food intake by GLP-1 in healthy subjects. Digestion 74, 78–84 (2006).
Gutzwiller, J. P., Degen, L., Matzinger, D., Prestin, S. & Beglinger, C. Interaction between GLP-1 and CCK-33 in inhibiting food intake and appetite in men. Am. J. Physiol. Regul. Comp. Physiol. 287, R562–R567 (2004).
Näslund, E., Gutniak, M., Skogar, S., Rössner, S. & Hellström, P. M. Glucagon-like peptide 1 increase the period of postprandial satiety and slows gastric emptying in obese men. Am. J. Clin. Nutr. 68, 525–530 (1998).
Näslund, E. et al. Energy intake and appetite are suppressed by glucagon-like peptide-1 (GLP-1) in obese men. Int. J. Obes. Relat. Metab. Disord. 23, 304–311 (1999).
Näslund, E. et al. Prandial subcutaneous injections of glucagon like peptide 1 cause weight loss in obese human subjects. Br. J. Nutr. 91, 439–446 (2004).
Gutzwiller, J. P. et al. Glucagon-like peptide-1 promotes satiety and reduced food intake in patients with diabetes mellitus. Am. J. Physiol. 276, R1541–R1545 (1999).
Flint, A., Raben, A., Ersbøll, A. K., Holst, J. J. & Astrup, A. The effect of physiological levels of glucagon-like peptide-1 on appetite, gastric emptying, energy and substrate metabolism in obesity. Int. J. Obes. Relat. Metab. Disord. 25, 781–792 (2001).
Edwards, C. M. et al. Exendin-4 reduces fasting and postprandial glucose and decreases energy intake in healthy volunteers. Am. J. Physiol. Endocrinol. Metab. 291, E155–E161 (2001).
Madsbad, S. Exenatide and liraglutide: different approaches to develop GLP-1 receptor agonists (incretin mimetics)—preclinical and clinical results. Best Pract. Res. Clin. Endocrinol. Metab. 23, 463–477 (2009).
Hanssen, K. B., Knop, F. K., Holst, J. J. & Vilsbøll, T. Treatment of type 2 diabetes with glucagon-like peptide-1 receptor agonists. Int. J. Clin. Pract. 63, 1154–1160 (2009).
Cohen, M. A. et al. Oxyntomodulin suppresses appetite and reduced food intake in humans. J. Clin. Endocrinol. Metab. 88, 4696–4701 (2003).
Wynne, K. et al. Oxyntomodulin increases energy expenditure in addition to decreasing energy intake in overweight and obese humans: a randomised controlled trial. Int. J. Obes. 30, 1729–1736 (2006).
Wynne, K. et al. Subcutaneous oxyntomodulin reduces body weight in overweight and obese subjects: a double-blind, randomized, controlled trial. Diabetes 54, 2390–2395 (2005).
Onga, T., Zabielski, R. & Kato, S. Multiple regulation of peptide YY secretion in the digestive tract. Peptides 23, 279–290 (2002).
Renshaw, D. & Batterham, R. L. Peptide YY: a potential therapy for obesity. Curr. Drug Targets 6, 171–179 (2005).
Baggiano, M. M. et al. PYY3–36 as an anti-obesity drug target. Obes. Rev. 6, 307–322 (2005).
Batterham, R. L. et al. Inhibition of food intake in obese subjects by peptide YY3–36 . N. Engl. J. Med. 349, 914–918 (2003).
Batterham, R. L. et al. PYY modulation of cortical and hypothalamic brain areas predicts feeding behaviour in humans. Nature 450, 106–109 (2007).
le Roux, C. W. et al. Supraphysiological doses of intravenous PYY3–36 cause nausea, but no additional reduction in food intake. Ann. Clin. Biochem. 45, 93–95 (2008).
Degen, L. et al. Effect of peptide PYY3–36 on food intake in humans. Gastroenterology 129, 1430–1436 (2005).
Sloth, B., Davidson, L., Holst, J. J., Flint, A. & Astrup, A. Effect of subcutaneous injections of PYY1–36 and PYY3–36 on appetite, ad libitum energy intake, and plasma free fatty acid concentration in obese males. Am. J. Physiol. Endocrinol. Metab. 293, E604–E609 (2007).
Sloth, B., Holst, J. J., Flint, A., Gregersen, N. T. & Astrup, A. Effects of PYY1–36 and PYY3–36 on appetite, energy intake, energy expenditure, glucose and fat metabolism in obese and lean subjects. Am. J. Physiol. Endocrinol. Metab. 292, E1062–E1068 (2007).
Chapman, I. et al. Low-dose pramlintide reduced food intake and meal duration in healthy, normal-weight subjects. Obesity 15, 1179–1186 (2007).
Reda, T. K., Geliebter, A. & Pi-Sunyer, F. X. Amylin, food intake and obesity. Obes. Res. 10, 1087–1091 (2002).
Lutz, T. A. Pancreatic amylin as a centrally acting satiating hormone. Curr. Drug Targets 6, 181–189 (2005).
Chapman, I. et al. Effect of pramlintide on satiety and food intake in obese subjects and subjects with type 2 diabetes. Diabetologia 48, 838–848 (2005).
Smith, S. R. et al. Pramlintide treatment reduces 24-h caloric intake and meal sizes and improves control of eating in obese subjects: a 6-wk translational research study. Am. J. Physiol. Endocrinol. Metab. 293, E620–E627 (2007).
Hollander, P. et al. Addition of pramlintide to insulin therapy lowers HbA1c in conjunction with weight loss in patients with type 2 diabetes approaching glycaemic targets. Diabetes Obes. Metab. 5, 408–414 (2003).
Hollander P. et al. Effect of pramlintide on weight in overweight and obese insulin treated type 2 diabetes patients. Obes. Res. 12, 661–668 (2004).
Farooqi, I. S. et al. Effects of recombinant leptin therapy in a child with congenital leptin deficiency. N. Engl. J. Med. 341, 879–884 (1999).
Williamson, D. A. et al. Microanalysis of eating behavior of three leptin deficient adults treated with leptin therapy. Appetite 45, 75–80 (2005).
Ravussin, E. et al. Enhanced weight loss with pramlintide/metreleptin: an integrated neurohormonal approach to obesity pharmacotherapy. Obesity 17, 1736–1743 (2009).
Abenhaim, L. et al. Appetite suppressant drugs and the risk of primary pulmonary hypertension. International Primary Pulmonary Hypertension Study Group. N. Engl. J. Med. 335, 609–616 (1996).
Rothman, R. B. & Baumann, M. H. Serotonergic drugs and valvular heart disease. Expert Opin. Drug Saf. 8, 317–329 (2009).
Rolls, B. J., Shide, D. J., Thorwart, M. L. & Ulbrecht, J. S. Sibutramine reduces food intake in non-dieting women with obesity. Obes. Res. 6, 1–11 (1998).
Barkeling, B., Elfhag, K., Rooth, P. & Rössner, S. Short-term effects of sibutramine (Reductil™) on appetite and eating behaviour and the long-term therapeutic outcomes. Int. J. Obes. Relat. Metab. Disord. 27, 693–700 (2003).
Appolinario, J. C. et al. A randomized, double-blind, placebo-controlled study of sibutramine in the treatment of binge-eating disorder. Arch. Gen. Psychiatry 60, 1109–1116 (2003).
Appolinario, J. C. et al. An open-label trial of sibutramine in obese patients with binge-eating disorder. J. Clin. Psychiatry 63, 28–30 (2002).
Milano, W. et al. Use of sibutramine, an inhibitor of the reuptake of serotonin and noradrenaline, in the treatment of binge eating disorder: A placebo-controlled study. Adv. Ther. 22, 25–31 (2005).
Taflinski, T. & Chojnacka, J. Sibutramine-associated psychotic episode. Am. J. Psychiatry 157, 2057–2058 (2000).
Binkley, K. & Knowles, S. R. Sibutramine and panic attacks. Am. J. Psychiatry 159, 1793–1794 (2002).
Sharma, S. M. et al. Blood pressure changes associated with sibutramine and weight management – an analysis from the 6-week lead-in period of the sibutramine cardiovascular outcomes trial (SCOUT). Diabetes Obes. Metab. 11, 239–250 (2009).
Heisler, L. K. et al. Activation of central melanocortin pathways by fenfluramine. Science 297, 609–611 (2002).
Heisler, L. K. et al. Serotonin reciprocally regulates melanocortin neurons to modulate food intake. Neuron 51, 239–249 (2006).
Walsh, A. E. et al. m-Chlorophenylpiperazine decreases food intake in a test meal. Psychopharmacology 116, 120–122 (1994).
Cowen, P. J., Sargent, P. A., Williams, C., Goodall, E. M. & Orlikov, A. B. Hypophagic, endocrine and subjective responses to m-chlorophenylpiperazine in healthy-men and women. Hum. Psychopharmacol. 10, 385–391 (1995).
Sargent, P. A., Sharpley, A. L., Williams, C., Goodall, E. M. & Cowen, P. J. 5-HT2C activation decreases appetite and body weight in obese subjects. Psychopharmacology 133, 309–312 (1997).
Ghaziuddin, N., Welch, K. & Greden, J. Central serotonergic effects of m-chlorophenylpiperazine (mCPP) among normal control adolescents. Neuropsychopharmacology 28, 133–139 (2003).
Smith, B. M. et al. Discovery and SAR of new benzazepines as potent and selective 5-HT(2C) receptor agonists for the treatment of obesity. Bioorg. Med. Chem. Lett. 15, 1467–1470 (2005).
Smith, S. R. et al. Lorcaserin (APD356), a selective 5-HT(2C) agonist, reduces body weight in obese men and women. Obesity 17, 494–503 (2009).
Doggrell, S. A. Tesofensine—a novel potent weight loss medication. Expert Opinion Invest. Drugs 18, 1043–1046 (2009).
Bello, N. T. & Zahner, M. R. Tesofensine, a monoanime reuptake inhibitor for the treatment of obesity. Curr. Opinion Investig. Drugs 10, 1105–1116 (2009).
Hauser, R. A., Saline, L., Judel, N., Konyago, V. L. & The NS 2330 Monotherepy PC Study Group. Randomized trial of the triple monoamine reuptake inhibitor NS 2330 (tesofensine) in early Parkinson's disease. Mov. Disord. 22, 359–365 (2007).
Astrup, A. et al. Effect of tesofensine on bodyweight loss, body composition, and quality of life in obese patients: a randomised, double-blind, placebo-controlled trial. Lancet 372, 1906–1913 (2008).
Gasteyger, C., Sjödin, A., Meier, D. H. & Astrup, A. Effects of tesofensine on appetite in obese subjects. Obesity 16 (Suppl. 1), S138–S139 (2008).
Sommet, A., Pathak, A. & Montastruc, J. L. Tesofensine and weight loss. Lancet 373, 719 (2009).
Astrup, A., Madsbad, S. & Larsen, T. M. Tesofensine and weight loss—Authors' reply. Lancet 373, 720 (2009).
Kalra, S. P. et al. Interacting appetite-regulating pathways in the hypothalamic regulation of body weight. Endocr. Rev. 20, 68–100 (1999).
Berthoud, H. R. & Morrison, C. The brain, appetite and obesity. Annu. Rev. Psychol. 59, 55–92 (2008).
Kamiji, M. M. & Inui, A. Neuropeptide Y receptor selective ligands in the treatment of obesity. Endocr. Rev. 28, 664–684 (2007).
Jeon, M. K. & Cheon, H. G. Promising strategies for obesity pharmacotherapy: melanocortin-4 (MC-4) receptor agonists and melanin concentrating hormone (MCH) receptor-1 antagonists. Curr. Top. Med. Chem. 9, 504–538 (2009).
ClinicalTrials.gov. Phase IIb one year efficacy and safety study of S-2367 (Velneperit) in obese subjects with initial 6-week low calorie diet (LDC) [online], (2009).
Shionogi & Co., Ltd. Shionogi announces positive top-line efficacy results from year-long studies of velneperit, a novel NPY Y5 receptor antagonist being investigated for the treatment of obesity [online], (2009).
Drewnowski, A., Krahn, D. D., Demitrack, M. A., Nairn, K. & Gosnell, B. A. Naloxone, an opiate blocker, reduces the consumption of sweet high-fat foods in obese and lean female binge eaters. Am. J. Clin. Nutr. 61, 1206–1212 (1995).
Yeomans, M. R. & Gray, R. W. Selective effects of naltrexone on food pleasantness and intake. Physiol. Behav. 60, 439–446 (1996).
Yeomans, M. R. & Gray, R. W. Effects of naltrexone on food intake and changes in subjective appetite during eating: Evidence for opioid involvement in the appetizer effect. Physiol. Behav. 62, 15–21 (1997).
Yeomans, M. R., Wright, P., Macleod, H. A. & Critchley, J. A. Effects of nalmefene on feeding in humans—dissociation of hunger and palatability. Psychopharmacology 100, 426–432 (1990).
Yeomans, M. R. & Wright, P. Lower pleasantness of palatable foods in nalmefene-treated human volunteers. Appetite 16, 249–259 (1991).
Speigal, T. A. et al. Effect of naltrexone on food intake, hunger, and satiety in obese men. Physiol. Behav. 40, 135–141 (1987).
Alger, S. A., Schwalberg, M. D., Bigaouette, J. M., Michalek, A. V. & Howard, L. J. Effect of a tricyclic antidepressant and opiate antagonist on binge-eating behavior in normoweight bulimic and obese, binge-eating subjects. Am. J. Clin. Nutr. 53, 865–871 (1991).
Lee, M. W. & Fujioka, K. Naltrexone for the treatment of obesity: review and update. Expert Opin. Pharmacother. 10, 1841–1845 (2009).
Kirkham, T. C. Endocannabinoids in the regulation of appetite and body weight. Behav. Pharmacol. 16, 297–313 (2005).
Haney, M., Ward, A. S., Comer, S. D., Foltin, R. W. & Fischman, M. W. Abstinence symptoms following oral THC administration to humans. Psychopharmacol. 141, 385–394 (1999).
Kirkham, T. C., Townson, A. L. & Halford, J. C. Oromucosal application of a cannabis extract accentuates pre-prandial hunger and increases caloric intake in healthy volunteers. Int. J. Obes. 31 (Suppl. 1), T2:PO.86, S99 (2007).
Van Gaal, L. F., Rissanen, A. M., Scheen, A. J., Ziegler, O. & Rossner, S. Effects of the cannabinoid-1 receptor blocker rimonabant on weight reduction and cardiovascular risk factors in overweight patients: 1-year experience from the RIO-Europe study. Lancet 365, 1389–1397 (2005).
Pi-Sunyer, X., Despres, J. P., Scheen, A. & Van Gaal, L. Improvement of metabolic parameters with rimonabant beyond the effect attributable to weight loss alone: Pooled 1-year data from the RIO (rimonabant in obesity and related metabolic disorders) program. J. Am. Coll. Cardiol. 47 (Suppl. A), 362A (2006).
Pi-Sunyer, F. X. et al. Effect of rimonabant, a cannabinoid-1 receptor blocker, on weight and cardiometabolic risk factors in overweight or obese patients: RIO-North America: A randomized controlled trial. JAMA. 295, 761–775 (2006).
Scheen, A. J., Finer, N., Hollander, P., Jensen, M. D. & Van Gaal, L. F. Efficacy and tolerability of rimonabant in overweight or obese patients with type 2 diabetes: a randomised controlled study. Lancet 368, 1660–1672 (2006).
Blundell, J. E. et al. Effect of rimonabant on energy intake, motivation to eat and body weight with or without hypocaloric diet: the REBA study. Obes. Rev. 7 (Suppl. 2), PP0021, 104 (2006).
Addy, C. et al. Multiple-dose pharmacokinetics, pharmacodynamics, and safety of taranabant, a novel selective cannabinoid-1 receptor inverse agonist, in healthy male volunteers. J. Clin. Pharmacol. 48, 734–744 (2008).
Plodowski, R. A. et al. Bupropion and naltrexone: a review of their use individually and in combination for the treatment of obesity. Expert Opin. Pharmacother. 10, 1069–1081 (2009).
Hausenloy, D. J. Contrave™: a novel treatment for obesity. Clin. Lipidol. 4, 279–285 (2009).
Jain, A. K. et al. Buproprion SR vs placebo for weight loss in obese patients with depressive symptoms. Obes. Res. 10, 1049–1056 (2002).
Anderson, J. W. et al. Buproprion SR enhances weight loss: A 48-week double blind, placebo-controlled trial. Obes. Res. 10, 633–641 (2002).
Li, Z. et al. Meta-analysis: pharmacologic treatments of obesity. Ann. Intern. Med. 142, 532–546 (2005).
Silverstone, T. Anorectic effect of a long-acting preparation of phentermine (duromine). Psychopharmacologica 25, 315–320 (1972).
Van Ameringen, M., Mancini, C., Pipe, B., Campbell, M. & Oakman, J. Topiramate treatment for SSRI-incuded weight gain in anxiety disorders. J. Clin. Psychiatry 63, 981–984 (2002).
Ben-Menachem, A., Axelsen, M., Johanson, E. H., Stagge, A. & Smith, U. Predictors of weight loss in adults with topiramate-treated epilepsy. Obes. Res. 11, 556–562 (2003).
Gadde, K. M., Francisey, D. M., Wagner, H. R. & Krishnan, K. R. Zonisamide for weight loss in obese adults: a randomized controlled trial. JAMA 289, 1820–1825 (2003).
Appolinario, J. C. & McElroy, S. L. Pharmacological approaches in the treatment of binge eating disorder. Curr. Drug Targets 5, 301–307 (2004).
Bray, G. A. et al. A 6-month randomized, placebo-controlled, dose-ranging trial of topiramate for weight loss in obesity. Obes. Res. 11, 722–733 (2003).
Wilding, J. et al. A randomised double-blind placebo controlled study of the long-term efficacy and safety of topiramate in the treatment of obese subjects. Int. J. Obes. Relat. Metab. Disord. 28, 1399–1410 (2004).
McElroy, S. L. et al. Role of antiepileptic drugs in the management of eating disorders. CNS Drugs 23, 139–156 (2009).
Neary, N. M. et al. Peptide YY3–36 and glucagon-like peptide-1(7–36) inhibit food intake additively. Endocrinology 146, 5120–5127 (2005).
Rosenbaum, M., Sy, M., Pavlovich, K., Leibel, R. L. & Hirsch, J. Leptin reverses weight loss-induced changes in regional neural activity responses to visual food stimuli. J. Clin. Invest. 118, 2583–2591 (2008).Ut nos adiatinit,
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
J. C. G. Halford declares associations with the following companies/organizations: GlaxoSmithKline (Speakers Bureau), Novo Nordisk (Speakers Bureau), Prosidion OSI Pharmaceuticals (Consultant). J. E. Blundell is an expert consultant to the NDA Panel of the European Food Safety Authority (EFSA), a Scientific Governor of the British Nutrition Foundation, and Treasurer and Trustee of the European Association for the Study of Obesity. He is also an advisor/consultant to industrial companies in the food and pharmaceutical sectors (Consultant: Merck, Amylin, Covance, Barilla, Danone; Speakers bureau: Kellogg's, Fonterra; Grant/research support: National Starch, Coca-Cola, Sanofi-aventis, Unilever). Lastly, he has grant/research support from the Biotechnology and Biological Sciences Research Council. The other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Halford, J., Boyland, E., Blundell, J. et al. Pharmacological management of appetite expression in obesity. Nat Rev Endocrinol 6, 255–269 (2010). https://doi.org/10.1038/nrendo.2010.19
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrendo.2010.19
This article is cited by
-
Anti-obesity activity of human gut microbiota Bacteroides stercoris KGMB02265
Archives of Microbiology (2024)
-
How does lorcaserin facilitate weight loss and who will benefit?
Nature Reviews Endocrinology (2018)
-
Sympathetic inputs regulate adaptive thermogenesis in brown adipose tissue through cAMP-Salt inducible kinase axis
Scientific Reports (2018)
-
Pharmacological Interventions for Obesity: Current and Future Targets
Current Addiction Reports (2018)
-
Serotonin-dependent kinetics of feeding bursts underlie a graded response to food availability in C. elegans
Nature Communications (2017)