Abstract
Caretakers are often intimidated or alienated by patients with borderline personality disorder (BPD), compounding the clinical challenges posed by the severe morbidity, high social costs and substantial prevalence of this disorder in many health-care settings. BPD is found in ∼1.7% of the general population but in 15–28% of patients in psychiatric clinics or hospitals and in a large proportion of individuals seeking help for psychological problems in general health facilities. BPD is characterized by extreme sensitivity to perceived interpersonal slights, an unstable sense of self, intense and volatile emotionality and impulsive behaviours that are often self-destructive. Most patients gradually enter symptomatic remission, and their rate of remission can be accelerated by evidence-based psychosocial treatments. Although self-harming behaviours and proneness to crisis can decrease over time, the natural course and otherwise effective treatments of BPD usually leave many patients with persistent and severe social disabilities related to depression or self-harming behaviours. Thus, clinicians need to actively enquire about the central issues of interpersonal relations and unstable identity. Failure to correctly diagnose patients with BPD leads to misleading pharmacological interventions that rarely succeed. Whether the definition of BPD should change is under debate that is linked to not fully knowing the nature of this disorder.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Black, D. W. et al. Attitudes toward borderline personality disorder: a survey of 706 mental health clinicians. CNS Spectr. 16, 67–74 (2011).
Linehan, M. Cognitive-Behavioral Treatment of Borderline Personality Disorder. (Guilford Press, 1993).
Bateman, A. & Fonagy, P. Effectiveness of partial hospitalization in the treatment of borderline personality disorder: a randomized controlled trial. Am. J. Psychiatry 156, 1563–1569 (1999).
Clarkin, J. F., Levy, K. N., Lenzenweger, M. F. & Kernberg, O. F. Evaluating three treatments for borderline personality disorder: a multiwave study. Am. J. Psychiatry 164, 922–928 (2007). This study compares a psychoanalytically based therapy (TFP) to a behavioural therapy (DBT) and a non-intensive supportive generalist therapy, finding that they had comparable outcomes and thereby legitimizing both the psychoanalytic and supportive models.
Zanarini, M. C., Frankenburg, F. R., Reich, D. B. & Fitzmaurice, G. Attainment and stability of sustained symptomatic remission and recovery among patients with borderline personality disorder and Axis II comparison subjects: a 16-year prospective follow-up study. Am. J. Psychiatry 169, 476–483 (2012).
Gunderson, J. G. et al. Ten-year course of borderline personality disorder: psychopathology and function from the Collaborative Longitudinal Personality Disorders study. Arch. Gen. Psychiatry 68, 827–837 (2011). This paper highlights how patients with BPD frequently can have enduring symptom remissions while still having severe functional impairments.
Torgersen, S. et al. A twin study of personality disorders. Compr. Psychiatry 41, 416–425 (2000). This article presents the first methodologically robust twin study of BPD; it established the heritability of BPD at a time when the aetiology of this disorder was considered to be exclusively environmental.
Torgersen, S., Kringlen, E. & Cramer, V. The prevalence of personality disorders in a community sample. Arch. Gen. Psychiatry 58, 590–596 (2001). The article presents the prevalence and associations of sociodemographic variables to personality disorders, applying multivariate analyses in a large representative sample from the common population.
Johnson, J. G., Cohen, P., Kasen, S., Skodol, A. E. & Oldham, J. M. Cumulative prevalence of personality disorders between adolescence and adulthood. Acta Psychiatr. Scand. 118, 410–413 (2008). The article presents a longitudinal study of personality disorders at four ages over almost 20 years.
Torgersen, S. in American Psychiatric Publishing Textbook of Personality Disorders 2nd edn (ed. Oldham, J. M., Skodol, A. E., Bender, D. S. ) 109–129 (American Psychiatric Publishing, Washington, DC, 2014).
Grant, B. F. et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J. Clin. Psychiatry 69, 533–545 (2008).
Kaess, M., Brunner, R. & Chanen, A. Borderline personality disorder in adolescence. Pediatrics 134, 782–793 (2014).
Tomko, R. L., Trull, T. J., Wood, P. K. & Sher, K. J. Characteristics of borderline personality disorder in a community sample: comorbidity, treatment utilization, and general functioning. J. Pers. Disord. 28, 734–750 (2014).
Bender, D. S. et al. Treatment utilization by patients with personality disorders. Am. J. Psychiatry 158, 295–302 (2001).
Zanarini, M. C., Frankenburg, F. R., Hennen, J. & Silk, K. R. Mental health service utilization by borderline personality disorder patients and Axis II comparison subjects followed prospectively for 6 years. J. Clin. Psychiatry 65, 28–36 (2004).
Chanen, A. M. et al. Screening for borderline personality disorder in outpatient youth. J. Pers. Disord. 22, 353–364 (2008).
Zimmerman, M., Chelminski, I. & Young, D. The frequency of personality disorders in psychiatric patients. Psychiatr. Clin. North Am. 31, 405–420 (2008).
Korzekwa, M. I., Dell, P. F., Links, P. S., Thabane, L. & Webb, S. P. Estimating the prevalence of borderline personality disorder in psychiatric outpatients using a two-phase procedure. Compr. Psychiatry 49, 380–386 (2008).
Gross, R. et al. Borderline personality disorder in primary care. Arch. Intern. Med. 162, 53 (2002).
Chaput, Y. J. A. & Lebel, M.-J. Demographic and clinical profiles of patients who make multiple visits to psychiatric emergency services. Psychiatr. Serv. 58, 335–341 (2007).
Torgersen, S. in The Oxford Handbook of Personality Disorders (ed. Widiger, T. A. ) 186–205 (Oxford Univ. Press, New York, 2012).
Cramer, V., Torgersen, S. & Kringlen, E. Personality disorders and quality of life. A population study. Compr. Psychiatry 47, 178–184 (2006).
Cramer, V., Torgersen, S. & Kringlen, E. Socio-demographic conditions, subjective somatic health, Axis I disorders and personality disorders in the common population: the relationship to quality of life. J. Pers. Disord. 21, 552–567 (2007). The article presents a study of the influence of personality disorders on different aspects of quality of life, compared to, and controlled for, different sociodemographic variables and Axis I disorders.
Ullrich, S. & Coid, J. The age distribution of self-reported personality disorder traits in a household population. J. Pers. Disord. 23, 187–200 (2009).
Cattane, N., Rossi, R., Lanfredi, M. & Cattaneo, A. Borderline personality disorder and childhood trauma: exploring the affected biological systems and mechanisms. BMC Psychiatry 17, 221 (2017).
Feldker, K. et al. Transdiagnostic brain responses to disorder-related threat across four psychiatric disorders. Psychol. Med. 47, 730–743 (2017).
Dannlowski, U. et al. Limbic scars: long-term consequences of childhood maltreatment revealed by functional and structural magnetic resonance imaging. Biol. Psychiatry 71, 286–293 (2012).
Distel, M. A. et al. Life events and borderline personality features: the influence of gene–environment interaction and gene–environment correlation. Psychol. Med. 41, 849–860 (2010).
Zanarini, M. C. et al. Reported pathological childhood experiences associated with the development of borderline personality disorder. Am. J. Psychiatry 154, 1101–1106 (1997).
Afifi, T. O. et al. Childhood adversity and personality disorders: results from a nationally representative population-based study. J. Psychiatr. Res. 45, 814–822 (2011).
Hengartner, M. P., Ajdacic-Gross, V., Rodgers, S., Müller, M. & Rössler, W. Childhood adversity in association with personality disorder dimensions: new findings in an old debate. Eur. Psychiatry 28, 476–482 (2013).
Johnson, J. G., Cohen, P., Brown, J., Smailes, E. M. & Bernstein, D. P. Childhood maltreatment increases risk for personality disorders during early adulthood. Arch. Gen. Psychiatry 56, 600 (1999).
Johnson, J. G., Cohen, P., Chen, H., Kasen, S. & Brook, J. S. Parenting behaviors associated with risk for offspring personality disorder during adulthood. Arch. Gen. Psychiatry 63, 579 (2006).
Crawford, T. N., Cohen, P. R., Chen, H., Anglin, D. M. & Ehrensaft, M. Early maternal separation and the trajectory of borderline personality disorder symptoms. Dev. Psychopathol. 21, 1013 (2009).
Rogosch, F. A. & Cicchetti, D. Child maltreatment and emergent personality organization: perspectives from the five-factor model. J. Abnorm. Child Psychol. 32, 123–145 (2004).
Fonagy, P. & Bateman, A. The development of borderline personality disorder — a mentalizing model. J. Pers. Disord. 22, 4–21 (2008).
Stepp, S. D. & Lazarus, S. A. Identifying a borderline personality disorder prodrome: implications for community screening. Personal. Ment. Health 11, 195–205 (2017).
Helgeland, M. I., Kjelsberg, E. & Torgersen, S. Continuities between emotional and disruptive behavior disorders in adolescence and personality disorders in adulthood. Am. J. Psychiatry 162, 1941–1947 (2005).
Stepp, S. D., Burke, J. D., Hipwell, A. E. & Loeber, R. Trajectories of attention deficit hyperactivity disorder and oppositional defiant disorder symptoms as precursors of borderline personality disorder symptoms in adolescent girls. J. Abnorm. Child Psychol. 40, 7–20 (2011).
Chanen, A. M. & Kaess, M. Developmental pathways to borderline personality disorder. Curr. Psychiatry Rep. 14, 45–53 (2011).
Gunderson, J. G. Family study of borderline personality disorder and its sectors of psychopathology. Arch. Gen. Psychiatry 68, 753 (2011).
Torgersen, S. et al. The heritability of cluster B personality disorders assessed both by personal interview and questionnaire. J. Pers. Disord. 26, 848–866 (2012).
Reichborn-Kjennerud, T. et al. A longitudinal twin study of borderline and antisocial personality disorder traits in early to middle adulthood. Psychol. Med. 45, 3121–3131 (2015).
Grilo, C. M. et al. Longitudinal diagnostic efficiency of DSM-IV criteria for borderline personality disorder: a 2-year prospective study. Can. J. Psychiatry 52, 357–362 (2007).
Torgersen, S. et al. Dimensional representations of DSM-IV cluster B personality disorders in a population-based sample of Norwegian twins: a multivariate study. Psychol. Med. 38, 1617 (2008).
Kendler, K. S. et al. The structure of genetic and environmental risk factors for DSM-IV personality disorders. Arch. Gen. Psychiatry 65, 1438 (2008).
Bornovalova, M. A., Hicks, B. M., Iacono, W. G. & McGue, M. Stability, change, and heritability of borderline personality disorder traits from adolescence to adulthood: a longitudinal twin study. Dev. Psychopathol. 21, 1335 (2009).
Amad, A., Ramoz, N., Thomas, P., Jardri, R. & Gorwood, P. Genetics of borderline personality disorder: systematic review and proposal of an integrative model. Neurosci. Biobehav. Rev. 40, 6–19 (2014).
Witt, S. H. et al. Genome-wide association study of borderline personality disorder reveals genetic overlap with bipolar disorder, major depression and schizophrenia. Transl Psychiatry 7, e1155 (2017).
Prados, J. et al. Borderline personality disorder and childhood maltreatment: a genome-wide methylation analysis. Genes Brain Behav. 14, 177–188 (2015).
Perroud, N. et al. Response to psychotherapy in borderline personality disorder and methylation status of the BDNF gene. Transl Psychiatry 3, e207–e207 (2013).
Martín-Blanco, A. et al. The role of hypothalamus–pituitary–adrenal genes and childhood trauma in borderline personality disorder. Eur. Arch. Psychiatry Clin. Neurosci. 266, 307–316 (2015).
de Kloet, E. R., Joëls, M. & Holsboer, F. Stress and the brain: from adaptation to disease. Nat. Rev. Neurosci. 6, 463–475 (2005).
Carrion, V. G. & Wong, S. S. Can Traumatic Stress Alter the Brain? Understanding the implications of early trauma on brain development and learning. J. Adolesc. Health 51, S23–S28 (2012).
Di Iorio, C. R. et al. Hypothalamic-pituitary-adrenal axis genetic variation and early stress moderates amygdala function. Psychoneuroendocrinology 80, 170–178 (2017).
Veer, I. M. et al. Endogenous cortisol is associated with functional connectivity between the amygdala and medial prefrontal cortex. Psychoneuroendocrinology 37, 1039–1047 (2012).
Pratt, M. et al. Mother-child adrenocortical synchrony; moderation by dyadic relational behavior. Horm. Behav. 89, 167–175 (2017).
Feldman, R., Gordon, I., Schneiderman, I., Weisman, O. & Zagoory-Sharon, O. Natural variations in maternal and paternal care are associated with systematic changes in oxytocin following parent–infant contact. Psychoneuroendocrinology 35, 1133–1141 (2010).
Fonagy, P., Luyten, P. & Allison, E. Epistemic petrification and the restoration of epistemic trust: a new conceptualization of borderline personality disorder and its psychosocial treatment. J. Pers. Disord. 29, 575–609 (2015).
Sharp, C. et al. Theory of mind and emotion regulation difficulties in adolescents with borderline traits. J. Am. Acad. Child Adolesc. Psychiatry 50, 563–573.e1 (2011).
Krause-Utz, A. et al. Amygdala and dorsal anterior cingulate connectivity during an emotional working memory task in borderline personality disorder patients with interpersonal trauma history. Front. Hum. Neurosci. 8, 848 (2014).
Beeney, J. E., Hallquist, M. N., Ellison, W. D. & Levy, K. N. Self-other disturbance in borderline personality disorder: neural, self-report, and performance-based evidence. Personal. Disord. 7, 28–39 (2016).
New, A. S. et al. Empathy and alexithymia in borderline personality disorder: clinical and laboratory measures. J. Pers. Disord. 26, 660–675 (2012).
Domes, G., Grabe, H. J., Czieschnek, D., Heinrichs, M. & Herpertz, S. C. Alexithymic Traits and Facial Emotion Recognition in Borderline Personality Disorder. Psychother. Psychosom. 80, 383–385 (2011).
Meaney, R., Hasking, P. & Reupert, A. Borderline personality disorder symptoms in college students: the complex interplay between alexithymia, emotional dysregulation and rumination. PLoS ONE 11, e0157294 (2016).
Mier, D. et al. Neuronal correlates of social cognition in borderline personality disorder. Soc. Cogn. Affect. Neurosci. 8, 531–537 (2013).
Dziobek, I. et al. Neuronal correlates of altered empathy and social cognition in borderline personality disorder. Neuroimage 57, 539–548 (2011).
Bilek, E. et al. State-dependent cross-brain information flow in borderline personality disorder. JAMA Psychiatry 74, 949–957 (2017).
O’Neill, A. et al. Dysregulation between emotion and theory of mind networks in borderline personality disorder. Psychiatry Res. 231, 25–32 (2015).
Herpertz, S. C., Bertsch, K. & Jeung, H. Neurobiology of Criterion A: self and interpersonal personality functioning. Curr. Opin. Psychol. 21, 23–27 (2017). This review provides the first thorough and systematic evaluation of the neurobiology of personality disorders within the framework of the DSM-5 AMPD, following the innovative approach of functional impairments instead of symptoms in personality disorders.
Eisenberger, N. I. & Lieberman, M. D. Why rejection hurts: a common neural alarm system for physical and social pain. Trends Cogn. Sci. 8, 294–300 (2004).
Domsalla, M. et al. Cerebral processing of social rejection in patients with borderline personality disorder. Soc. Cogn. Affect. Neurosci. 9, 1789–1797 (2014).
Carpenter, R. W. & Trull, T. J. Components of emotion dysregulation in borderline personality disorder: a review. Curr. Psychiatry Rep. 15, 335 (2013).
Bertsch, K. et al. Oxytocin and reduction of social threat hypersensitivity in women with borderline personality disorder. Am. J. Psychiatry 170, 1169–1177 (2013).
Izurieta Hidalgo, N. A. et al. Time course of facial emotion processing in women with borderline personality disorder: an ERP study. J. Psychiatry Neurosci. 41, 16–26 (2016).
Schneider, I. et al. Remnants and changes in facial emotion processing in women with remitted borderline personality disorder: an EEG study. Eur. Arch. Psychiatry Clin. Neurosci. https://doi.org/10.1007/s00406-017-0841-7 (2017).
Schulze, L., Schmahl, C. & Niedtfeld, I. Neural correlates of disturbed emotion processing in borderline personality disorder: a multimodal meta-analysis. Biol. Psychiatry 79, 97–106 (2016). This meta-analysis provides a large body of evidence that a dysfunctional amygdala and dorsolateral PFC are characteristic features of individuals with BPD.
Kamphausen, S. et al. Medial prefrontal dysfunction and prolonged amygdala response during instructed fear processing in borderline personality disorder. World J. Biol. Psychiatry 14, 307–318 (2013).
Hazlett, E. A. et al. Potentiated amygdala response to repeated emotional pictures in borderline personality disorder. Biol. Psychiatry 72, 448–456 (2012).
Koenigsberg, H. W. et al. The neural correlates of anomalous habituation to negative emotional pictures in borderline and avoidant personality disorder patients. Am. J. Psychiatry 171, 82–90 (2014).
Dyck, M. et al. Cognitive versus automatic mechanisms of mood induction differentially activate left and right amygdala. Neuroimage 54, 2503–2513 (2011).
Hoerst, M. et al. Metabolic alterations in the amygdala in borderline personality disorder: a proton magnetic resonance spectroscopy study. Biol. Psychiatry 67, 399–405 (2010).
Schienle, A., Leutgeb, V. & Wabnegger, A. Symptom severity and disgust-related traits in borderline personality disorder: the role of amygdala subdivisions. Psychiatry Res. 232, 203–207 (2015).
Kuhlmann, A., Bertsch, K., Schmidinger, I., Thomann, P. A. & Herpertz, S. C. Morphometric differences in central stress-regulating structures between women with and without borderline personality disorder. J. Psychiatry Neurosci. 38, 129–137 (2013).
Kreisel, S. H. et al. Volume of hippocampal substructures in borderline personality disorder. Psychiatry Res. 231, 218–226 (2015).
Niedtfeld, I. et al. Voxel-based morphometry in women with borderline personality disorder with and without comorbid posttraumatic stress disorder. PLoS ONE 8, e65824 (2013).
Kimmel, C. L. et al. Age-related parieto-occipital and other gray matter changes in borderline personality disorder: a meta-analysis of cortical and subcortical structures. Psychiatry Res. 251, 15–25 (2016).
Mancke, F. et al. Assessing the marks of change: how psychotherapy alters the brain structure in women with borderline personality disorder. J. Psychiatry Neurosci. 43, 170132 (2017).
Silvers, J. A. et al. Affective lability and difficulties with regulation are differentially associated with amygdala and prefrontal response in women with Borderline Personality Disorder. Psychiatry Res. 254, 74–82 (2016).
Koenigsberg, H. W. et al. Neural correlates of the use of psychological distancing to regulate responses to negative social cues: a study of patients with borderline personality disorder. Biol. Psychiatry 66, 854–863 (2009).
Schulze, L. et al. Neuronal correlates of cognitive reappraisal in borderline patients with affective instability. Biol. Psychiatry 69, 564–573 (2011).
Cullen, K. R. et al. Brain activation in response to overt and covert fear and happy faces in women with borderline personality disorder. Brain Imag. Behav. 10, 319–331 (2016).
Herpertz, S. C. et al. Brain mechanisms underlying reactive aggression in borderline personality disorder-sex matters. Biol. Psychiatry 82, 257–266 (2017).
Sato, J. R. et al. Can neuroimaging be used as a support to diagnosis of borderline personality disorder? An approach based on computational neuroanatomy and machine learning. J. Psychiatr. Res. 46, 1126–1132 (2012).
Carrasco, J. L. et al. Microstructural white matter damage at orbitofrontal areas in borderline personality disorder. J. Affect. Disord. 139, 149–153 (2012).
Schmitt, R., Winter, D., Niedtfeld, I., Herpertz, S. C. & Schmahl, C. Effects of psychotherapy on neuronal correlates of reappraisal in female patients with borderline personality disorder. Biol. Psychiatry Cogn. Neurosci. Neuroimag. 1, 548–557 (2016).
Scherpiet, S. et al. Reduced neural differentiation between self-referential cognitive and emotional processes in women with borderline personality disorder. Psychiatry Res. 233, 314–323 (2015).
Müller, L. E. et al. Cortical representation of afferent bodily signals in borderline personality disorder: neural correlates and relationship to emotional dysregulation. JAMA Psychiatry 72, 1077–1086 (2015).
Gentili, C. et al. Not in one metric: Neuroticism modulates different resting state metrics within distinctive brain regions. Behav. Brain Res. 327, 34–43 (2017).
Turner, D., Sebastian, A. & Tüscher, O. Impulsivity and cluster B personality disorders. Curr. Psychiatry Rep. 19, 15 (2017).
McHugh, C. & Balaratnasingam, S. Impulsivity in personality disorders: current views and future directions. Curr. Opin. Psychiatry 31, 63–68 (2018).
Herbort, M. C. et al. A negative relationship between ventral striatal loss anticipation response and impulsivity in borderline personality disorder. NeuroImage Clin. 12, 724–736 (2016).
Soloff, P. H., White, R., Omari, A., Ramaseshan, K. & Diwadkar, V. A. Affective context interferes with brain responses during cognitive processing in borderline personality disorder: fMRI evidence. Psychiatry Res. 233, 23–35 (2015).
Silbersweig, D. et al. Failure of frontolimbic inhibitory function in the context of negative emotion in borderline personality disorder. Am. J. Psychiatry 164, 1832–1841 (2007).
Jacob, G. A. et al. Emotional modulation of motor response inhibition in women with borderline personality disorder: an fMRI study. J. Psychiatry Neurosci. 38, 164–172 (2013).
Schmahl, C. & Baumgärtner, U. Pain in borderline personality disorder. Mod. Trends Pharmacopsychiatry 30, 166–175 (2015).
Reitz, S. et al. Incision and stress regulation in borderline personality disorder: neurobiological mechanisms of self-injurious behaviour. Br. J. Psychiatry 207, 165–172 (2015).
Niedtfeld, I. et al. Functional connectivity of pain-mediated affect regulation in Borderline Personality Disorder. PLoS ONE 7, e33293 (2012).
Willis, F. et al. The role of nociceptive input and tissue injury on stress regulation in borderline personality disorder. Pain 158, 479–487 (2017).
Niedtfeld, I. et al. Pain-mediated affect regulation is reduced after dialectical behavior therapy in borderline personality disorder: a longitudinal fMRI study. Soc. Cogn. Affect. Neurosci. 12, 739–747 (2017).
Glenn, J. J., Michel, B. D., Franklin, J. C., Hooley, J. M. & Nock, M. K. Pain analgesia among adolescent self-injurers. Psychiatry Res. 220, 921–926 (2014).
Carvalho Fernando, S. et al. Associations of childhood trauma with hypothalamic-pituitary-adrenal function in borderline personality disorder and major depression. Psychoneuroendocrinology 37, 1659–1668 (2012).
Rausch, J. et al. Increased testosterone levels and cortisol awakening responses in patients with borderline personality disorder: gender and trait aggressiveness matter. Psychoneuroendocrinology 55, 116–127 (2015).
Wingenfeld, K. & Wolf, O. T. Effects of cortisol on cognition in major depressive disorder, posttraumatic stress disorder and borderline personality disorder — 2014 Curt Richter Award Winner. Psychoneuroendocrinology 51, 282–295 (2015).
Lyons-Ruth, K., Choi-Kain, L., Pechtel, P., Bertha, E. & Gunderson, J. Perceived parental protection and cortisol responses among young females with borderline personality disorder and controls. Psychiatry Res. 189, 426–432 (2011).
Bertsch, K., Schmidinger, I., Neumann, I. D. & Herpertz, S. C. Reduced plasma oxytocin levels in female patients with borderline personality disorder. Horm. Behav. 63, 424–429 (2013).
Jobst, A. et al. Lower oxytocin plasma levels in borderline patients with unresolved attachment representations. Front. Hum. Neurosci. 10, 125 (2016).
Smith, A. S. & Wang, Z. Hypothalamic oxytocin mediates social buffering of the stress response. Biol. Psychiatry 76, 281–288 (2014).
Simeon, D. et al. Oxytocin administration attenuates stress reactivity in borderline personality disorder: a pilot study. Psychoneuroendocrinology 36, 1418–1421 (2011).
Lischke, A., Herpertz, S. C., Berger, C., Domes, G. & Gamer, M. Divergent effects of oxytocin on (para-)limbic reactivity to emotional and neutral scenes in females with and without borderline personality disorder. Soc. Cogn. Affect. Neurosci. 12, 1783–1792 (2017).
Cataldo, I., Azhari, A., Lepri, B. & Esposito, G. Oxytocin receptors (OXTR) and early parental care: an interaction that modulates psychiatric disorders. Res. Dev. Disabil.https://doi.org/10.1016/j.ridd.2017.10.007 (2017).
Hammen, C., Bower, J. E. & Cole, S. W. Oxytocin receptor gene variation and differential susceptibility to family environment in predicting youth borderline symptoms. J. Pers. Disord. 29, 177–192 (2015).
Cicchetti, D., Rogosch, F. A., Hecht, K. F., Crick, N. R. & Hetzel, S. Moderation of maltreatment effects on childhood borderline personality symptoms by gender and oxytocin receptor and FK506 binding protein 5 genes. Dev. Psychopathol. 26, 831–849 (2014).
Dettenborn, L. et al. Increased hair testosterone but unaltered hair cortisol in female patients with borderline personality disorder. Psychoneuroendocrinology 71, 176–179 (2016).
Volman, I., Toni, I., Verhagen, L. & Roelofs, K. Endogenous testosterone modulates prefrontal-amygdala connectivity during social emotional behavior. Cereb. Cortex 21, 2282–2290 (2011).
Eisenlohr-Moul, T. A., DeWall, C. N., Girdler, S. S. & Segerstrom, S. C. Ovarian hormones and borderline personality disorder features: preliminary evidence for interactive effects of estradiol and progesterone. Biol. Psychol. 109, 37–52 (2015).
Association, A. P. Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
Zimmerman, M., Chelminski, I., Young, D., Dalrymple, K. & Martinez, J. Is dimensional scoring of borderline personality disorder important only for subthreshold levels of severity? J. Pers. Disord. 27, 244–251 (2013).
Zimmerman, M., Chelminski, I., Young, D., Dalrymple, K. & Martinez, J. Does the presence of one feature of borderline personality disorder have clinical significance? J. Clin. Psychiatry 73, 8–12 (2011).
Ellison, W. D., Rosenstein, L., Chelminski, I., Dalrymple, K. & Zimmerman, M. The clinical significance of single features of borderline personality disorder: anger, affective instability, impulsivity, and chronic emptiness in psychiatric outpatients. J. Pers. Disord. 30, 261–270 (2016).
World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders (WHO, Geneva, 1992).
Zimmerman, M. & Mattia, J. I. Differences between clinical and research practices in diagnosing borderline personality disorder. Am. J. Psychiatry 156, 1570–1574 (1999).
Morey, L. C. & Benson, K. T. An investigation of adherence to diagnostic criteria, revisited: clinical diagnosis of the DSM-IV/DSM-5 Section II Personality Disorders. J. Pers. Disord. 30, 130–144 (2016).
Zanarini, M. C. et al. The collaborative longitudinal personality disorders study: reliability of Axis I and II diagnoses. J. Pers. Disord. 14, 291–299 (2000).
Samuel, D. B. et al. Convergent and incremental predictive validity of clinician, self-report, and structured interview diagnoses for personality disorders over 5 years. J. Consult. Clin. Psychol. 81, 650–659 (2013).
Hopwood, C. J. et al. A comparison of interview and self-report methods for the assessment of borderline personality disorder criteria. Psychol. Assess. 20, 81–85 (2008).
Zimmerman, M., Multach, M. D., Dalrymple, K. & Chelminski, I. Clinically useful screen for borderline personality disorder in psychiatric out-patients. Br. J. Psychiatry 210, 165–166 (2016).
Eaton, N. R. et al. Borderline personality disorder co-morbidity: relationship to the internalizing–externalizing structure of common mental disorders. Psychol. Med. 41, 1041–1050 (2010).
Kotov, R. et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. J. Abnorm. Psychol. 126, 454–477 (2017). This article places BPD in a hierarchical structure spanning internalizing and externalizing spectra of psychopathology, helping to explain commonly observed comorbidities and suggesting the possibilities of shared risk factors, aetiology, pathophysiology, illness course and treatment response.
McGlashan, T. H. et al. The Collaborative Longitudinal Personality Disorders Study: baseline Axis I/II and II/II diagnostic co-occurrence. Acta Psychiatr. Scand. 102, 256–264 (2000).
Zanarini, M. C. et al. Axis I comorbidity of borderline personality disorder. Am. J. Psychiatry 155, 1733–1739 (1998).
Zimmerman, M. & Mattia, J. I. Axis I diagnostic comorbidity and borderline personality disorder. Compr. Psychiatry 40, 245–252 (1999).
Asherson, P. et al. Differential diagnosis, comorbidity, and treatment of attention-deficit/hyperactivity disorder in relation to bipolar disorder or borderline personality disorder in adults. Curr. Med. Res. Opin. 30, 1657–1672 (2014).
Feinstein, A. R. The pre-therapeutic classification of co-morbidity in chronic disease. J. Chron. Dis. 23, 455–468 (1970).
Gunderson, J. G. et al. Major depressive disorder and borderline personality disorder revisited. J. Clin. Psychiatry 65, 1049–1056 (2004).
Boritz, T., Barnhart, R. & McMain, S. F. The influence of posttraumatic stress disorder on treatment outcomes of patients with borderline personality disorder. J. Pers. Disord. 30, 395–407 (2016).
Keuroghlian, A. S. et al. Interactions of borderline personality disorder and anxiety disorders over 10 years. J. Clin. Psychiatry 76, 1529–1534 (2015).
Skodol, A. E. et al. Relationship of personality disorders to the course of major depressive disorder in a nationally representative sample. Am. J. Psychiatry 168, 257–264 (2011).
Hasin, D. Personality disorders and the 3-year course of alcohol, drug, and nicotine use disorders. Arch. Gen. Psychiatry 68, 1158 (2011).
Gunderson, J. G. et al. Interactions of borderline personality disorder and mood disorders over 10 years. J. Clin. Psychiatry 75, 829–834 (2014).
Quirk, S. E. et al. Personality disorders and physical comorbidities in adults from the United States: data from the National Epidemiologic Survey on Alcohol and Related Conditions. Soc. Psychiatry Psychiatr. Epidemiol. 50, 807–820 (2015).
Chanen, A. M. et al. The HYPE Clinic: an early intervention service for borderline personality disorder. J. Psychiatr. Pract. 15, 163–172 (2009).
Marieke Schuppert, H. et al. Emotion regulation training for adolescents with borderline personality disorder traits: a randomized controlled trial. J. Am. Acad. Child Adolesc. Psychiatry 51, 1314–1323.e2 (2012).
Chanen, A. M. et al. Early intervention for adolescents with borderline personality disorder using cognitive analytic therapy: randomised controlled trial. Br. J. Psychiatry 193, 477–484 (2008).
Zanarini, M. C. & Frankenburg, F. R. A. Preliminary, randomized trial of psychoeducation for women with borderline personality disorder. J. Pers. Disord. 22, 284–290 (2008).
Zimmerman, M., Ruggero, C. J., Chelminski, I. & Young, D. Psychiatric diagnoses in patients previously overdiagnozed with bipolar disorder. J. Clin. Psychiatry 71, 26–31 (2009).
Paris, J. Why psychiatrists are reluctant to diagnose: borderline personality disorder. Psychiatry 4, 35–39 (2007).
Zanarini, M. C., Frankenburg, F. R., Reich, D. B., Harned, A. L. & Fitzmaurice, G. M. Rates of psychotropic medication use reported by borderline patients and Axis II comparison subjects over 16 years of prospective follow-up. J. Clin. Psychopharmacol. 35, 63–67 (2015).
Kendall, T., Burbeck, R. & Bateman, A. Pharmacotherapy for borderline personality disorder: NICE guideline. Br. J. Psychiatry 196, 158–159 (2010).
Gabbard, G. O. Do all roads lead to Rome? New Findings Borderline Personal. Disorder. Am. J. Psychiatry 164, 853–855 (2007).
Gunderson, J. G. Borderline personality disorder. N. Engl. J. Med. 364, 2037–2042 (2011).
Linehan, M. M. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch. Gen. Psychiatry 48, 1060 (1991). This article presents the first randomized control trial to demonstrate that BPD can be successfully treated. This report irrevocably changed this disorder's reputation for untreatability.
Linehan, M. M. et al. Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder. JAMA Psychiatry 72, 475 (2015).
Bateman, A. & Fonagy, P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am. J. Psychiatry 166, 1355–1364 (2009).
McMain, S. F. et al. A randomized trial of dialectical behavior therapy versus general psychiatric management for borderline personality disorder. Am. J. Psychiatry 166, 1365–1374 (2009).
Yeomans, F. E., Clarkin, J. F. & Kernberg, O. F. A Primer on Transference-Focused Psychotherapy for the Borderline Patient. (J. Aronson, 2002).
Choi-Kain, L. W., Finch, E. F., Masland, S. R., Jenkins, J. A. & Unruh, B. T. What works in the treatment of borderline personality disorder. Curr. Behav. Neurosci. Rep. 4, 21–30 (2017).
Gunderson, J. G. The emergence of a generalist model to meet public health needs for patients with borderline personality disorder. Am. J. Psychiatry 173, 452–458 (2016). This article serves notice that less intensive, easier-to-learn models of treatment can be effective for most patients with BPD.
Gunderson, J. G. & Links, P. S. Handbook of Good Psychiatric Management for Borderline Personality Disorder. (American Psychiatric Publishing, 2014).
Choi-Kain, L. W., Albert, E. B. & Gunderson, J. G. Evidence-based treatments for borderline personality disorder. Harv. Rev. Psychiatry 24, 342–356 (2016).
Chanen, A. M. & McCutcheon, L. Prevention and early intervention for borderline personality disorder: current status and recent evidence. Br. J. Psychiatry 202, s24–s29 (2013).
Zanarini, M. C. et al. The pain of being borderline: dysphoric states specific to borderline personality disorder. Harv. Rev. Psychiatry 6, 201–207 (1998).
Lieb, K., Vollm, B., Rucker, G., Timmer, A. & Stoffers, J. M. Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials. Br. J. Psychiatry 196, 4–12 (2009).
Pennay, A. et al. A systematic review of interventions for co-occurring substance use disorder and borderline personality disorder. J. Subst. Abuse Treat. 41, 363–373 (2011).
Lee, N. K., Cameron, J. & Jenner, L. A systematic review of interventions for co-occurring substance use and borderline personality disorders. Drug Alcohol Rev. 34, 663–672 (2015).
Bohus, M. et al. Dialectical behaviour therapy for post-traumatic stress disorder after childhood sexual abuse in patients with and without borderline personality disorder: a randomised controlled trial. Psychother. Psychosom. 82, 221–233 (2013).
Harned, M. S., Korslund, K. E. & Linehan, M. M. A pilot randomized controlled trial of Dialectical Behavior Therapy with and without the Dialectical Behavior Therapy Prolonged Exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behav. Res. Ther. 55, 7–17 (2014).
Ingenhoven, T. Pharmacotherapy for borderline patients: business as usual or by default? J. Clin. Psychiatry 76, e522–e523 (2015).
NICE. Borderline Personality Disorder: Treatment and Management. (British Psychological Society, Great Britain, 2009). This scholarly and critical review of psychoactive medication use concludes that BPD symptoms are not responsive and that medications should be prescribed sparingly.
Crawford, M. J. et al. The clinical effectiveness and cost-effectiveness of lamotrigine in borderline personality disorder: a randomized placebo-controlled trial. Am. J. Psychiatryhttps://doi.org/10.1176/appi.ajp.2018.17091006 (2018).
Hoffman, P. D. et al. Family Connections: a program for relatives of persons with borderline personality disorder. Fam. Process 44, 217–225 (2005).
Gunderson, J. G., Berkowitz, C. & Ruiz-Sancho, A. Families of borderline patients: a psychoeducational approach. Bull. Menninger Clin. 61, 446–457 (1997).
Jørgensen, C. R. et al. Outcome of mentalization-based and supportive psychotherapy in patients with borderline personality disorder: a randomized trial. Acta Psychiatr. Scand. 127, 305–317 (2012).
Gunderson, J. Predictors of 2-year outcome for patients with borderline personality disorder. Am. J. Psychiatry 163, 822 (2006).
Zanarini, M. C., Frankenburg, F. R., Hennen, J., Reich, D. B. & Silk, K. R. Prediction of the 10-year course of borderline personality disorder. Am. J. Psychiatry 163, 827–832 (2006).
Zanarini, M. The subsyndromal phenomenology of borderline personality disorder: a 10-year follow-up study. Am. J. Psychiatry 164, 929 (2007).
Zanarini, M. C., Frankenburg, F. R., Reich, D. B. & Fitzmaurice, G. M. Fluidity of the subsyndromal phenomenology of borderline personality disorder over 16 years of prospective follow-up. Am. J. Psychiatry 173, 688–694 (2016).
McGlashan, T. H. et al. Two-year prevalence and stability of individual DSM-IV criteria for schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders: toward a hybrid model of Axis II disorders. Am. J. Psychiatry 162, 883–889 (2005).
Lenzenweger, M. F., Lane, M. C., Loranger, A. W. & Kessler, R. C. DSM-IV personality disorders in the National Comorbidity Survey Replication. Biol. Psychiatry 62, 553–564 (2007).
Skodol, A. E. et al. Stability of functional impairment in patients with schizotypal, borderline, avoidant, or obsessive–compulsive personality disorder over two years. Psychol. Med. 35, 443–451 (2005).
Zanarini, M. C., Frankenburg, F. R., Hennen, J., Reich, D. B. & Silk, K. R. Psychosocial functioning of borderline patients and Axis II comparison subjects followed prospectively for six years. J. Pers. Disord. 19, 19–29 (2005).
Zanarini, M. C., Frankenburg, F. R., Reich, D. B. & Fitzmaurice, G. The 10-year course of psychosocial functioning among patients with borderline personality disorder and axis II comparison subjects. Acta Psychiatr. Scand. 122, 103–109 (2010). This paper demonstrates that unexpectedly high rates of both symptomatic and functional recovery are achievable over 16 years by patients with BPD.
Zanarini, M. C., Frankenburg, F. R., Reich, D. B. & Fitzmaurice, G. Time to attainment of recovery from borderline personality disorder and stability of recovery: a 10-year prospective follow-up study. Am. J. Psychiatry 167, 663–667 (2010).
Zanarini, M. C. et al. The course of marriage/sustained cohabitation and parenthood among borderline patients followed prospectively for 16 years. J. Pers. Disord. 29, 62–70 (2015).
Frankenburg, F. R. & Zanarini, M. C. The association between borderline personality disorder and chronic medical illnesses, poor health-related lifestyle choices, and costly forms of health care utilization. J. Clin. Psychiatry 65, 1660–1665 (2004).
Keuroghlian, A. S., Frankenburg, F. R. & Zanarini, M. C. The relationship of chronic medical illnesses, poor health-related lifestyle choices, and health care utilization to recovery status in borderline patients over a decade of prospective follow-up. J. Psychiatr. Res. 47, 1499–1506 (2013).
El-Gabalawy, R., Katz, L. Y. & Sareen, J. Comorbidity and associated severity of borderline personality disorder and physical health conditions in a nationally representative sample. Psychosom. Med. 72, 641–647 (2010).
Kochanek, K. D., Murphy, S. L., Xu, J. & Tejada-Vera, B. Deaths: Final Data for 2014. Natl Vital Stat. Rep. 65, 1–122 (2016).
Sharp, C. et al. The structure of personality pathology: both general (‘g’) and specific (‘s’) factors? J. Abnorm. Psychol. 124, 387–398 (2015).
Wright, A. G. C., Hopwood, C. J., Skodol, A. E. & Morey, L. C. Longitudinal validation of general and specific structural features of personality pathology. J. Abnorm. Psychol. 125, 1120–1134 (2016). This study confirms that BPD represents general impairments shared across other personality disorders, which showed lower absolute stability but stronger relationships to concurrent and prospective psychosocial functioning than specific features that were more stable in a 10-year longitudinal study.
Sanislow, C. A. et al. Developing constructs for psychopathology research: Research domain criteria. J. Abnorm. Psychol. 119, 631–639 (2010).
American Psychiatric Association. DSM-III. Diagnostic and Statistical Manual of Mental Disorders 3rd edn (American Psychiatric Press, 1980).
Saulsman, L. M. & Page, A. C. The five-factor model and personality disorder empirical literature: a meta-analytic review. Clin. Psychol. Rev. 23, 1055–1085 (2004).
Samuel, D. B & Widiger, T. A. A meta-analytic review of the relationships between the five-factor model and DSM-IV-TR personality disorders: a facet level analysis. Clin. Psychol. Rev. 28, 1326–1342 (2008).
Morey, L. C., Benson, K. T. & Skodol, A. E. Relating DSM-5 section III personality traits to section II personality disorder diagnoses. Psychol. Med. 46, 647–655 (2015).
Herpertz, S. C. et al. The challenge of transforming the diagnostic system of personality disorders. J. Pers. Disord. 31, 577–589 (2017). This report summarizes the controversy about classifying personality disorders from within the dimensional trait-based perspective versus retaining the categorical model that has been in use, concluding that change should proceed incrementally.
Winsper, C. et al. Clinical and psychosocial outcomes of borderline personality disorder in childhood and adolescence: a systematic review. Psychol. Med. 45, 2237–2251 (2015). This comprehensive review shows that borderline pathology prior to the age of 19 years is predictive of subsequent symptoms and deficits in functioning up to 20 years later, suggesting the clinical utility of the BPD phenotype in younger populations and warranting early intervention.
Crawford, T. N. et al. Comorbid Axis I and Axis II disorders in early adolescence. Arch. Gen. Psychiatry 65, 641 (2008).
Ha, C., Balderas, J. C., Zanarini, M. C., Oldham, J. & Sharp, C. Psychiatric comorbidity in hospitalized adolescents with borderline personality disorder. J. Clin. Psychiatry 75, e457–e464 (2014).
Wright, A. G. C., Zalewski, M., Hallquist, M. N., Hipwell, A. E. & Stepp, S. D. Developmental trajectories of borderline personality disorder symptoms and psychosocial functioning in adolescence. J. Pers. Disord. 30, 351–372 (2016).
Chanen, A. M. Borderline personality disorder in young people: are we there yet? J. Clin. Psychol. 71, 778–791 (2015).
Sharp, C. & Fonagy, P. Practitioner Review: Borderline personality disorder in adolescence — recent conceptualization, intervention, and implications for clinical practice. J. Child Psychol. Psychiatry 56, 1266–1288 (2015).
Morey, L. C. et al. State effects of major depression on the assessment of personality and personality disorder. Am. J. Psychiatry 167, 528–535 (2010).
Zimmerman, M. & Morgan, T. A. Problematic boundaries in the diagnosis of bipolar disorder: the interface with borderline personality disorder. Curr. Psychiatry Rep. 15, 422 (2013).
Ruggero, C. J., Zimmerman, M., Chelminski, I. & Young, D. Borderline personality disorder and the misdiagnosis of bipolar disorder. J. Psychiatr. Res. 44, 405–408 (2010).
Zimmerman, M. et al. Distinguishing bipolar II depression from major depressive disorder with comorbid borderline personality disorder. J. Clin. Psychiatry 74, 880–886 (2013).
Soeteman, D. I., Hakkaart-van Roijen, L., Verheul, R. & Busschbach, J. J. V. The economic burden of personality disorders in mental health care. J. Clin. Psychiatry 69, 259–265 (2008).
Meuldijk, D., McCarthy, A., Bourke, M. E. & Grenyer, B. F. S. The value of psychological treatment for borderline personality disorder: systematic review and cost offset analysis of economic evaluations. PLoS ONE 12, e0171592 (2017). This thoughtful analysis of the direct costs of BPD and how evidence-based care can more than offset this establishes a basis for good reimbursement standard.
van Asselt, A. D. I., Dirksen, C. D., Arntz, A. & Severens, J. L. The cost of borderline personality disorder: societal cost of illness in BPD-patients. Eur. Psychiatry 22, 354–361 (2007).
Bailey, R. C., G. B. Burden and support needs of carers of persons with borderline personality disorder: a systematic review. Harv. Rev. Psychiatry 21, 248–258 (2013).
Page, A., Hooke, G., O’Brien, N. & de Felice, N. Assessment of distress and burden in Australian private psychiatric inpatients. Australas. Psychiatry 14, 285–290 (2006).
Ekdahl, S., Idvall, E., Samuelsson, M. & Perseius, K.-I. A. Life tiptoeing: being a significant other to persons with borderline personality disorder. Arch. Psychiatr. Nurs. 25, e69–e76 (2011).
Goodman, M. et al. Parental burden associated with borderline personality disorder in female offspring. J. Pers. Disord. 25, 59–74 (2011).
Stern, A. Psychoanalytic investigation of and therapy in the borderline group of neuroses. Psychoanal Q. 7, 467–489 (1938).
Knight, R. P. Borderline states. Bull. Menninger Clin. 17, 1–12 (1953).
Kernberg, O. Borderline personality organization. J. Am. Psychoanal. Assoc. 15, 641–685 (1967). This psychoanalytic conception of borderline patients ignited hopes that these patients could be distinguishable and that they were treatable.
Kety, S. S., Rosenthal, D., Wender, P. H. & Schulsinger, F. The types and prevalence of mental illness in the biological and adoptive families of adopted schizophrenics. J. Psychiatr. Res. 6, 345–362 (1968).
Grinker, R. R., Werble, B. & Drye, R. C. Borderline Syndrome: A Behavioral Study of Ego-Functions. (Basic Books, 1968).
Gunderson, J. G. & Kolb, J. E. Discriminating features of borderline patients. Am. J. Psychiatry 135, 792–796 (1978). This article identifies a reliably assessed and discriminating set of criteria that became the official definition of BPD in the DSM-III.
Spitzer, R. L., Endicott, J. & Gibbon, M. Crossing the border into borderline personality and borderline schizophrenia. The development of criteria. Arch. Gen. Psychiatry 36, 17–24 (1979).
Haas, B. W. & Miller, J. D. Borderline personality traits and brain activity during emotional perspective taking. Personal. Disord. 6, 315–320 (2015).
First, M. et al. Structured Clinical Interview for DSM-IV Axis II Personality Disorders, (SCID-II) (American Psychiatric Press, Inc., 1997).
Zanarini, M. C., Frankenburg, F. R., Chauncey, D. L. & Gunderson, J. G. The diagnostic interview for personality disorders: Interrater and test-retest reliability. Compr. Psychiatry 28, 467–480 (1987).
Loranger, A. W. International Personality Disorder Examination Manual (1999).
Pfohl, B., Blum, N. S. & Zimmerman, M. Structured interview for DSM-IV personality: SIDP-IV. (American Psychiatric Press, 1997).
First, M. B., Skodol, A. E., Bender, D. S. & Oldham, J. M. User's Guide for the Structured Clinical Interview for the DSM-5 Alternative Model for Personality Disorders (SCID-5-AMPD) (American Psychiatric Association, 2018).
Zanarini, M. C., Gunderson, J. G., Frankenburg, F. R. & Chauncey, D. L. The revised diagnostic interview for borderlines: discriminating BPD from other Axis II disorders. J. Pers. Disord. 3, 10–18 (1989).
Zanarini, M. C., Gunderson, J. G., Frankenburg, F. R.,& Chauncey, D. L. Discriminating borderline personality disorder from other Axis II disorders. Am. J. Psychiatry 147, 161–167 (1990).
Sharp, C., Ha, C., Michonski, J., Venta, A. & Carbone, C. Borderline personality disorder in adolescents: evidence in support of the Childhood Interview for DSM-IV Borderline Personality Disorder in a sample of adolescent inpatients. Compr. Psychiatry 53, 765–774 (2012).
Arntz, A. et al. Reliability and validity of the Borderline Personality Disorder Severity Index. J. Pers. Disord. 17, 45–59 (2003).
Zanarini, M. C. Zanarini Rating Scale For Borderline Personality Disorder (ZAN-BPD): a continuous measure of DSM-IV borderline psychopathology. J. Pers. Disord. 17, 233–242 (2003).
Zanarini, M. C., Weingeroff, J. L., Frankenburg, F. R. & Fitzmaurice, G. M. Development of the self-report version of the Zanarini Rating Scale for Borderline Personality Disorder. Personal. Ment. Health 9, 243–249 (2015).
Grant, B. F. et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): reliability of substance use and psychiatric disorder modules in a general population sample. Drug Alcohol Depend. 148, 27–33 (2015).
Hyler, S. E. Personality Diagnostic Questionnaire-4. (New York State Psychiatric Institute, 1994).
Morey, L. C. Personality Assessment Inventory Professional Manual. (Psychological Assessment Resources, 1991).
Bohus, M. et al. Psychometric properties of the Borderline Symptom List (BSL). Psychopathology 40, 126–132 (2007).
Mullins-Sweatt, S. N. et al. Five-factor measure of borderline personality traits. J. Pers. Assess. 94, 475–487 (2012).
Clark, L. A., Simms, L. J., Wu, K. D. & Casillas, A. Manual for the Schedule for Nonadaptive and Adaptive Personality (SNAP-2). (Univ. of Minnesota Press, 2008).
John Livesley, W. & Douglas Jackson, N. Dimensional Assessment of Personality Pathology. SIGMA Assessment Systemshttp://www.sigmaassessmentsystems.com/assessments/dimensional-assessment-of-personality-pathology-basic-questionnaire/ (2009).
Sellbom, M. & Smith, A. Assessment of DSM-5 section II personality disorders with the MMPI-2-RF in a nonclinical sample. J. Pers. Assess. 99, 384–397 (2016).
Krueger, R. F., Derringer, J., Markon, K. E., Watson, D. & Skodol, A. E. Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychol. Med. 42, 1879–1890 (2011).
Zanarini, M. C. et al. A screening measure for BPD: the McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD). J. Pers. Disord. 17, 568–573 (2003).
Chang, B., Sharp, C. & Ha, C. The criterion validity of the borderline personality features scale for children in an adolescent inpatient setting. J. Pers. Disord. 25, 492–503 (2011).
Poreh, A. M. et al. The BPQ: a scale for the assessment of borderline personality based on DSM-IV criteria. J. Pers. Disord. 20, 247–260 (2006).
Verheul, R. et al. Severity Indices of Personality Problems (SIPP-118): development, factor structure, reliability, and validity. Psychol. Assess. 20, 23–34 (2008).
Hentschel, A. G. & Livesley, W. J. The General Assessment of Personality Disorder (GAPD): factor structure, incremental validity of self-pathology, and relations to DSM–IV personality disorders. J. Pers. Assess. 95, 479–485 (2013).
Morey, L. C. Development and initial evaluation of a self-report form of the DSM-5 Level of Personality Functioning Scale. Psychol. Assess. 29, 1302–1308 (2017).
Author information
Authors and Affiliations
Contributions
Introduction (J.G.G.); Epidemiology (S.T.); Mechanisms/pathophysiology (S.C.H.); Diagnosis, screening and prevention (A.E.S.); Management (J.G.G.); Quality of life (M.C.Z.); Outlook (J.G.G.); Overview of Primer (J.G.G.).
Corresponding author
Ethics declarations
Competing interests
S.C.H. was the past president of the International Society for the Study of Personality Disorders. A.E.S. receives author and editor royalties from American Psychiatric Association Publishing and from UpToDate. All other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Gunderson, J., Herpertz, S., Skodol, A. et al. Borderline personality disorder. Nat Rev Dis Primers 4, 18029 (2018). https://doi.org/10.1038/nrdp.2018.29
Published:
DOI: https://doi.org/10.1038/nrdp.2018.29
This article is cited by
-
Evidence of deviant parasympathetic response to social exclusion in women with borderline personality disorder
European Archives of Psychiatry and Clinical Neuroscience (2024)
-
Theta burst stimulation add on to dialectical behavioral therapy in borderline-personality-disorder: methods and design of a randomized, single-blind, placebo-controlled pilot trial
European Archives of Psychiatry and Clinical Neuroscience (2024)
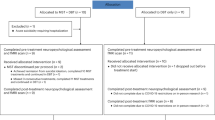
-
Differential outcomes of outpatient only versus combined inpatient/outpatient treatment in early intervention for adolescent borderline personality disorder
European Child & Adolescent Psychiatry (2024)
-
Resting-State EEG Microstates and Power Spectrum in Borderline Personality Disorder: A High-Density EEG Study
Brain Topography (2024)
-
Stress and reward in the maternal brain of mothers with borderline personality disorder: a script-based fMRI study
European Archives of Psychiatry and Clinical Neuroscience (2024)