Abstract
Hookworms are soil-transmitted nematode parasites that can reside for many years in the small intestine of their human hosts; Necator americanus is the predominant infecting species. Adult worms feed on the blood of a host and can cause iron deficiency anaemia, especially in high-risk populations (children and women of childbearing age). Almost 500 million people in developing tropical countries are infected, and simulation models estimate that hookworm infection is responsible for >4 million disability-adjusted life years lost annually. Humans mount an immune response to hookworms, but it is mostly unsuccessful at removing adult worms from the bowel. Accordingly, the host switches to an immune-tolerant state that enables hookworms to reside in the gut for many years. Although anthelmintic drugs are available and widely used, their efficacy varies and the drugs do not prevent reinfection. Thus, other control strategies aimed at improving water quality, sanitation and hygiene are needed. In addition, efforts are underway to develop a human hookworm vaccine through public–private partnerships. However, hookworms could also be a resource; as hookworms have the capability to regulate the host's inflammation, researchers are experimentally infecting patients to treat some inflammatory diseases as an approach to discover new anti-inflammatory molecules. This area of endeavour might well yield new biotherapeutics for autoimmune and allergic diseases.
Similar content being viewed by others
Introduction
Hookworms are soil-transmitted nematode parasites that can reside for many years in the small intestine of their human hosts, where they suck blood and can cause iron deficiency anaemia (IDA) in individuals who harbour moderate and high numbers of adult worms, which is known as hookworm disease. Hookworm infection affects almost 500 million people in the tropical regions of the world, accounting for 3.2 million disability-adjusted life years (DALYs) lost annually and ranking among the most important of the neglected tropical diseases in terms of causes of morbidity1. Alternative and newer estimates indicate that hookworm infection results in 4.1 million DALYs lost, as well as possibly over US$100 billion in global economic losses2. Indeed, hookworm infection, of which Necator americanus infection is the predominant human disease, has had a major influence on human history; in the early 1900s, hookworm infection was recognized as a major cause of anaemia and lost productivity in the southern United States. This understanding resulted in the formation of the Rockefeller-funded Human Hookworm Eradication Campaign3, which is the first example of modern-day public health philanthropy (the original 1920 silent film can be viewed online4). Although hookworm infection has mostly been eliminated through economic development (rather than mass treatment) in western European countries, the United States, South Korea and Japan, the disease burden remains unacceptably high in many low-income and middle-income countries, despite implementation of mass drug administration (MDA) programmes5. Safe drugs are available to combat human hookworm infection, but their efficacies are variable to the point that some MDA campaigns are rendered ineffective owing to outright drug failure6,7. Moreover, in the absence of a protective immune response, reinfection can rapidly occur, sometimes within 4–6 months in areas of high transmission8.
Although hookworms are clearly a major human pathogen, recent investigations into the immunobiology of hookworm infection have highlighted the ‘Jekyll and Hyde’ nature of this parasite. Indeed, the ability of hookworms and other helminths to modulate inflammation is so effective that some researchers are intentionally infecting human participants with low subclinical doses of larvae to treat a range of inflammatory diseases9–12, spurring discovery efforts to mine hookworm genomes and proteomes for new macromolecules to be used in the treatment of some autoimmune and allergic disorders that plague industrialized countries.
In this Primer, we review the current state of the field in hookworm research, focusing on the epidemiology; pathobiology and immunobiology; methods of diagnosis, screening and prevention; and management of hookworm infection and disease. We also provide a final outlook, in which we speculate on future directions for a hookworm research agenda, emphasizing the expanding efforts in improving control strategies and exploiting the therapeutic properties of hookworms for treating inflammatory diseases.
Epidemiology
Global burden of disease
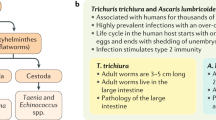
Prevalence. The most prevalent species of soil-transmitted helminths (STHs) are Ascaris lumbricoides, Trichuris trichiura and the three main hookworm species that infect humans (N. americanus, Ancylostoma duodenale and Ancylostoma ceylanicum). N. americanus is the predominant human hookworm that globally accounts for the majority of human hookworm cases; it is especially common in southern China, Southeast Asia, the Americas and most of Africa. A. duodenale is more focally endemic in the Mediterranean region, in northern regions of India and China and in North Africa. In some parts of Africa, China, India and elsewhere, it is not uncommon to find mixed human infections with N. americanus and A. duodenale. A third minor species, A. ceylanicum, which was thought to be primarily a canine parasite, has recently been identified as a highly prevalent species of hookworm in humans in a few focal regions in Southeast Asia, such as Malaysia and Indonesia, where it is also often co-endemic with N. americanus13,14.
Climate and soil structure are crucial determinants of hookworm prevalence, as the parasite thrives in tropical and subtropical zones, where moisture and temperature are ideal for larval development outside the host. The different distribution of the various hookworm species is not absolute, with mixed infections often occurring in individuals. An estimated 438.9 million people (95% credible interval: 406.3–480.2 million) were infected with hookworm in 2010 (Ref. 1), with the largest concentration of hookworm cases in Southeast Asia, followed by sub-Saharan Africa (Fig. 1). Hookworm infection tends to be more prevalent in rural areas, where the favourable tropical or subtropical ecologies converge with poverty and weak sanitary infrastructures. The decline in the prevalence of hookworm infection in the tropical regions of middle-income countries, such as China, was primarily achieved owing to newly urbanized economies, rapid economic development (especially in eastern China) and, in some areas, wide distribution of anthelmintic drugs. These advances were also the crucial factors in decreasing the prevalence of hookworm infection in the southern United States during the early twentieth century15.
The prevalence data are for overall hookworm infection, regardless of the parasite species. In 2010, 140 million individuals in South Asia were estimated to be infected with hookworms, 117 million in sub-Saharan Africa, 77 million in Southeast Asia, 64 million in East Asia, 30 million in Latin America and the Caribbean, 10 million in Oceania and 4.6 million in the Middle East and North Africa. Oceania had the highest prevalence (49%), followed by sub-Saharan Africa (13%), Southeast Asia (12.6%), South Asia (8.6%), East Asia (5%), and Latin America and the Caribbean (5%)1. The regions delimited by black borders (the Global Burden of Disease world regions) show the estimated prevalence rate of anaemia per 100,000 population due to hookworm infection. Prevalence data from Ref. 1, and based on geostatistical models for sub-Saharan Africa and available empirical information for all other regions. The anaemia data are courtesy of N. Kassebaum, University of Washington, Seattle, Washington, USA.
Morbidity and mortality. The prevalence of hookworm infection does not reflect its morbidity, which is directly correlated with the intensity of hookworm infection, generally expressed in eggs per gram of faeces (EPG)16. The WHO categorizes hookworm infections as light (≤1,999 EPG), moderate (2,000–3,999 EPG) and heavy (≥4,000 EPG)17. However, heavy infections are more likely to occur in areas that also exhibit high hookworm prevalence. Adult hookworms that feed in the host's gut cause blood loss, which can lead to IDA and hookworm disease. Hence, the greater the worm burden, the greater the blood loss. The extent of blood loss also depends on the species of infecting hookworm; A. duodenale is thought to be a wasteful feeder (not all the blood it ingests is digested) and is responsible for blood loss that is as much as 10-fold heavier than that caused by N. americanus18. Moreover, A. duodenale infection is associated with increased prevalence of IDA compared with N. americanus infection19. However, as N. americanus globally is the predominant hookworm on a population basis, it remains the leading cause of hookworm disease.
It is difficult to estimate the burden of disease from hookworm infection; the most common complications of this disease (IDA and poor birth outcomes, such as reduced birth weight and increased infant mortality) are often underreported and, when they are, they are not specifically associated with hookworm infection. Moreover, as hookworm infection often occurs in geographical areas where other conditions that are considered of greater public health importance, such as malaria and malnutrition20, are endemic, the morbidity from hookworm infection can be overlooked or even attributed to these conditions. The 2013 Global Burden of Disease Study indicated that IDA is a major cause of mortality, resulting in approximately 180,000 deaths worldwide21. However, this study does not ascribe any of this mortality to hookworm infection, although it does indicate that a substantial percentage of IDA in Africa and Oceania is due to hookworm infection22,23. More recently, hookworm disease was uncoupled from general IDA and shown to be second only to malaria as an underlying cause of global anaemia caused by parasitic infections23. Hookworm infection is a substantial cause of IDA in Oceania, tropical Latin America, southern sub-Saharan Africa and Southeast Asia in particular (Fig. 1).
At-risk populations
In most protozoan and helminth parasitic infections, prevalence peaks in childhood. However, the age-specific epidemiology of hookworm infection is different: although prevalence is high among children, it increases until it plateaus in adulthood24. Studies from China and Brazil show an increase from approximately 15% at 10 years of age to approximately 60% at 70 years of age25.
Moderate or heavy infections can manifest as IDA (reviewed in Ref. 26) in populations with low underlying iron reserves, such as children and women of childbearing age. Evidence strongly links chronic IDA in children with hookworm infection27 and IDA can result in long-term poor health outcomes, including reduced cognitive, intellectual and physical development28, reduced fertility among women and even reduced future wage-earning29. Patients with heavy infections often present with a microcytic hypochromic anaemia, which, in children, can lead to stunted growth, which is especially noticeable around puberty when infected adolescents fail to achieve their expected growth spurt. Intellectual and cognitive delays are also possible, but these can be subtle and difficult to measure30,31. For example, hookworm infection in children 6–11 years of age in Brazil was associated with reduced concentration and information processing skills32.
Women of childbearing age are also at greater risk of hookworm disease, which can be worsened by a combination of low dietary iron intake in resource-poor settings and blood loss either from menstruation or pregnancy (owing to the iron demands of the fetus). Pregnant women with hookworm disease — notably, across Africa, where more than one-quarter of pregnant women are infected33 — are at risk of higher maternal and neonatal issues (including maternal anaemia, low birth weight and infant mortality34), particularly when hookworm and malaria co-infections occur. Overall, it is estimated that 44 million pregnancies globally are complicated by hookworm infection35. For these reasons, women of childbearing age and children have been identified by the WHO as being at special risk for STH infections, but especially hookworm infection36,37.
Mechanisms/pathophysiology
Host invasion
Of the stages of the hookworm life cycle (Figs 2,3), third-stage larvae (L3) can infect the human host through percutaneous invasion (N. americanus and A. duodenale) or oral ingestion (A. duodenale). L3 are approximately 0.5–0.6 mm in length, and although initial skin invasion might go unnoticed, it can result in a local pruritic, erythematous rash (Fig. 3a), referred to as ‘ground itch’. Ground itch typically appears on the hands and feet, which are the main sites of L3 percutaneous entry (via hair follicles, which are the path of least resistance).
Hookworm eggs hatch in soil and rhabditiform (early) larvae moult twice (first-stage larvae (L1) and L2) before becoming infective (L3). L3 accumulate in soil or on grass awaiting exposure to human skin (often the hands, feet or buttocks), which they can penetrate. L3 then make their way to the peripheral vasculature, where they are passively swept within the bloodstream, first to the right side of the heart and then to the pulmonary vasculature. In the lungs, L3 exit from the alveolar capillaries into the bronchial tree, which they ascend to reach the pharynx, from which they enter the gastrointestinal tract to finally complete their migration to the small bowel. Once in the duodenum, immature L5 hookworms use ‘teeth’ (Ancylostoma spp.) or cutting plates (Necator spp.) that line their buccal capsule to lacerate the mucosa and anchor themselves in position to facilitate feeding and avoid being ejected by gut peristalsis. As they begin to feed on blood, juvenile worms mature into sexually dioecious adult parasites. Mature adult male and female hookworms mate, and female hookworms produce as many as 10,000 eggs per day. Eggs are evacuated from the host via the faecal stream. The process from L3 invasion to patency (egg production) takes approximately 6–8 weeks for Necator americanus and possibly a similar period of time for Ancylostoma duodenale.
a | A few days after Necator americanus third-stage larvae (L3) infect the host, a rash known as ‘ground itch’ develops at the site of skin penetration. b | A longitudinal histological section of an adult Ancylostoma caninum attached to the duodenal wall of an infected dog. c | A scanning electron micrograph of A. caninum, with its ‘teeth’ clearly visible. d | An N. americanus female (arrow) and male in copula in the small bowel of a human volunteer9. e | Egg of N. americanus in human faeces.
Upon penetrating human tissues and in response to host signals, such as insulin signalling molecules38, the large secretory glands of infective L3 release macromolecules that facilitate parasite entry and invasion39, including copious amounts of hydrolytic enzymes, such as proteases and hyaluronidases40,41. Prominent among the larval secretions is a family of cysteine-rich proteins that belong to the CAP family (cysteine-rich secretory proteins, antigen 5, and pathogenesis-related 1 proteins), which are often referred to as Ancylostoma-secreted proteins (ASPs)42. ASPs are crucial in the developmental stages of the parasite and represent roughly one-third of all secreted proteins43; the N. americanus genome contains 137 different genes encoding distinct ASPs44.
At least one of these L3-secreted molecules, ASP-2, has been shown to be allergenic45 and might explain why repeated hookworm infections produce ground itch and other forms of dermatitis, as well as hookworm pneumonitis and Wakana disease26. Once the L3 reach the bloodstream through skin capillaries, they begin the journey that eventually leads them to the small bowel (Fig. 3b), where they use their cutting plates (or ‘teeth’, as is the case for Ancylostoma spp.; Fig. 3c) to attach to the mucosa and start feeding.
Pathophysiology
Blood loss. The mechanisms by which hookworms induce blood loss are multifactorial. Substantial blood loss occurs as a direct result of actively feeding adult worms. The host's erythrocytes are digested in the gastrointestinal tract of the hookworm by a suite of mechanistically distinct proteolytic enzymes46. Haemoglobin is cleaved by proteases, and the by-product of this process, haem, is detoxified by the glutathione S-transferase GST-1 (Ref. 47). However, most of the blood loss is a result of leakage around the attachment site of the hookworm in the gut of the host, rather than direct consumption by the parasite, and is caused by the secretion of parasite-derived anticoagulants, including factor Xa, factor XIa and factor VIIa–tissue factor inhibitors48. Adult hookworms are thought to ingest just 0.001 ml of blood per day49, but the amount of blood loss at the site of attachment is much greater, such that moderate or heavy N. americanus infections can produce losses of >1 ml daily28. Heavy hookworm infections can lead to hypoproteinaemia, which can cause anasarca (oedema of the face and lower limbs) and abdominal distension from ascites. The skin of infected individuals acquires a sickly yellowish colour, sometimes referred to as ‘chlorosis’ in the older literature, accounting for historical references to yellowish pallor, geophagy (the practice of eating soil) and a yellow disease of laziness dating back to the third century BC (reviewed in Ref. 50).
IDA. In the presence of moderate-to-heavy hookworm infections, when blood loss exceeds the host's intake and reserves of iron and proteins51, chronic IDA and the accompanying hypoalbuminaemia occur. Very heavy hookworm burden in nutritionally deprived adults is sufficient to induce IDA with haemoglobin levels of <11 g per dl. A study of 1,449 individuals in Uganda ≥50 years of age revealed that the greatest risk factors for IDA were heavy hookworm burden (odds ratio: 3.45) and malaria (odds ratio: 3.49)52. In children, IDA can occur with even lower hookworm burdens than those observed in adults53. The degree of IDA also depends on the species of the infecting hookworm: A. duodenale causes greater blood loss than N. americanus19. A study of almost 3,600 children from Pemba Island, Zanzibar, found that infection with N. americanus resulted in a lower incidence of IDA than did co-infection with both N. americanus and A. duodenale54. Systematic reviews have confirmed the association between moderate and heavy hookworm burdens and IDA in children and adults27,33. Along with iron losses, moderate and heavy hookworm infections result in substantial protein losses, which lead to hypoalbuminaemia and hypoproteinaemia. In severe cases, this can result in a clinical picture that resembles kwashiorkor (a severe form of malnutrition). The combination of anaemia and protein losses, together with chlorosis, is a reason why, in early twentieth century China, chronic hookworm infection was sometimes known as the ‘yellow puffy disease’ (Ref. 55).
Other features. Controlled human challenge infections with N. americanus of healthy volunteers who reside in countries where hookworms are no longer endemic (for example, Australia and the United Kingdom) have provided insight into the kinetics and manifestations of primary hookworm infection in the absence of other tropical pathogens and comorbidities9,56,57. Besides IDA and hypoalbuminaemia, the most prominent feature of hookworm infection is systemic57 and mucosal58 eosinophilia. Systemic eosinophilia can be detected within 4 weeks of N. americanus infection (that is, before arrival in the gut) and peaks at 6–12 weeks as the young adult hookworms arrive in the small bowel. Individuals with a light hookworm burden (infected with 10–20 L3) are often asymptomatic, although flatulence is common for the first 12 weeks and gastrointestinal disturbance is sometimes reported within the first 3–15 weeks59. The severity of gastrointestinal pain seems to be associated with the challenge inoculum57,59.
Zoonotic hookworm infections
Zoonotic hookworms, particularly canine and feline parasites, can cause symptoms and pathological outcomes in humans that are not seen with anthropophilic hookworms. Perhaps the most frequently encountered zoonotic hookworm is Ancylostoma braziliense60. Percutaneous entry of A. braziliense L3 does not cause ground itch in humans but can cause cutaneous larva migrans (also known as ‘creeping eruption’), which is a self-limiting condition that is characterized by serpiginous, 1–5-cm-long tunnels generated by the larvae migrating through the epidermis. Like ground itch, cutaneous larva migrans usually occurs on the areas that are most likely to be in contact with contaminated soil. Cutaneous larva migrans is most frequently encountered in travellers who are returning from tropical locations and military personnel, and responds to treatment with oral anthelmintics (albendazole or ivermectin). In some cases, A. braziliense larvae may reach the lungs and cause pulmonary infiltrates61, although, in the majority of cases, the infection does not progress beyond cutaneous larva migrans.
The common canine hookworm A. caninum is not thought to induce cutaneous larva migrans, possibly because A. caninum L3 rapidly reach the subcutaneous tissues where they undergo developmental arrest. However, gastrointestinal symptoms from human A. caninum infection can be severe. A series of 93 cases of eosinophilic gastroenteritis in adults living in urban northern Australia showed that enteric infection was linked to A. caninum62. Inflammation in some patients was so severe that surgical intervention was required62,63. Whether these reports indicate that A. caninum generates an excessive gastrointestinal inflammatory response in humans is unclear. It is also possible that A. caninum reaches the human gut more often than appreciated but goes unnoticed because it is usually expelled soon after arrival. In fact, after the description of the cases of eosinophilic gastroenteritis in northern Australia, similar cases were reported in the southern United States64 and Egypt65, as clinicians became aware of the differential diagnosis. In no case was more than a single adult worm identified in the patient, which accounts for the absence of eggs in the faeces66.
Experimental models of hookworm infection
Animal models. Animal models for hookworm infection are available but have limitations, and each presents its own series of challenges, including cost, ethical and reproducibility issues67,68. The rodent strongyle nematode Nippostrongylus brasiliensis has a similar life cycle to N. americanus and induces a T helper 2 (TH2)-type immune response that exhibits all the features of a human hookworm infection, including CD4+ T cell-dependent IgE production, eosinophilia, mastocytosis and mucus production (see below, Immunopathology)69. N. brasiliensis reaches patency in the small bowel of mice, which has enabled researchers to conduct both mucosal and systemic immunological studies aimed at gaining mechanistic insight into human hookworm infection70. There is also some modest blood loss and drop in haemoglobin levels in N. brasiliensis-infected rats. However, N. brasiliensis is a phylogenetically distant nematode compared with human hookworms, belonging to the Trichostrongyloidea superfamily, as opposed to hookworms that belong to the Ancylostomatoidea superfamily. Moreover, rodents develop immunological resistance to A. ceylanicum71, N. americanus72 and N. brasiliensis (reviewed in Ref. 70), a phenomenon that is much less apparent in human hookworm infections.
An alternative and widely used model for human gastrointestinal nematode infections is mice infected with Heligmosomoides polygyrus. H. polygyrus has a different life cycle than hookworms and does not traverse the skin or lungs, relying on oral ingestion of infective larvae from the environment. Moreover, like N. brasiliensis, H. polygyrus is a member of the Trichostrongyloidea superfamly. However, like hookworm, H. polygyrus does induce chronic intestinal infections in some strains of mice that are not readily eliminated by a modified TH2 cell response, which sheds light on protective immune mechanisms at play in gastrointestinal nematode infections70,73.
Two other rodent models that have been developed are hamsters infected either with A. ceylanicum or N. americanus. Hamsters infected with A. ceylanicum develop patent infections and experience intestinal blood loss and anaemia74, as well intestinal mucosal inflammation75. Acquired immunity can be elicited, so the model is suitable for vaccine development71. Similarly, it is possible to achieve patent infections in hamsters following N. americanus infection, although the numbers of larvae that become adult hookworms are lower than for A. ceylanicum and the infections are often short lived, but the model is still potentially useful for vaccine development studies76.
Dogs develop both age-acquired and exposure-acquired immunity to canine hookworms77. However, even in the face of a robust immune response against many worm antigens44,78, it is often elderly individuals in hookworm-endemic areas who harbour the heaviest hookworm burdens, which makes experimental and natural infections of rodents and dogs of limited value in understanding the chronicity of and absence of protective immunity to hookworm in human populations79. A non-human primate model of N. americanus infection was established in marmosets using both field-adapted and laboratory-adapted strains of hookworms80. Infections became patent and animals developed disease and immune responses that were similar to those seen in human infections, including anaemia, eosinophilia and parasite-specific IgE and IgG antibody responses. Despite the apparent usefulness of this model, we could not identify additional publications since the original description in 2008, which perhaps reflects the expense and ethical concerns around the use of non-human primates. Nonetheless, consideration of more-widespread use of this model might be warranted, particularly when testing new drugs and vaccines before conducting expensive human clinical trials.
Controlled human challenge models. The human challenge model presents distinct advantages over studying hookworm infection in an endemic transmission setting, where co-infections are the norm, exposure history is sketchy at best and compliance is a challenge. However, some of these same advantages can be viewed as problematic, as the controlled setting may not reflect real-world hookworm infection, which usually occurs in developing countries and impoverished settings with poor hygiene. Thus, studying hookworm infection in isolation in developed countries with low incidence of infectious diseases might have reduced generalizability. Nonetheless, the increasing adoption of the human challenge model in various laboratories around the world will probably accelerate testing of new interventions to control hookworm disease, as well as provide proof of concept that the hookworm proteome is a veritable pharmacopoeia for inflammatory disease therapeutics81. Moreover, the ability to study human hookworm infections in a controlled setting offers substantial advantages over mouse model studies, particularly owing to the development of chronic infection and the immune markers that define it (some of which are not detected in mice), such as IgG4.
Immunopathology
Despite the high global prevalence of N. americanus, the immunopathology of human hookworm infection has not received as much attention as that of other human helminth infections, such as schistosomiasis and filariasis. This lack of information can be attributed to the difficulty and expense of maintaining the hookworm life cycle in a suitable animal model and the inability of any of the main species of hookworms to reach full maturity in mice in substantial numbers82. Nonetheless, mouse studies with hookworm-like gastrointestinal nematodes of rodents have revealed the predominant cellular mechanisms that drive the immunopathological responses to these parasites. Early host responses in a primary hookworm infection are aimed at eliminating the invading parasites. Migrating L3 and adult hookworms are the target of inflammatory responses that are characterized by systemic and localized eosinophilia and mastocytosis58,78. Experimental human hookworm infection is not associated with significant pulmonary inflammation or compromised airway responsiveness11, but resulted in increased mucosal expression of TH1 cytokines, such as interferon-γ (IFNγ), IL-2 and IL-15, and TH2 cytokines, including IL-4, IL-5 and IL-13 (Ref. 58), and infection intensity is negatively associated with parasite-specific IL-5 levels83. Despite the predominance of TH2 cells, type 2 cytokines and parasite-killing antibody isotypes (such as IgE), attempts to dislodge adult hookworms from the gut are mostly unsuccessful. Moreover, despite the robust and enduring TH2 cell response that is induced by hookworms, infected individuals show no signs of overt allergy to worms, and indeed are even protected from developing allergies to bystander antigens84. Thus, to limit the immunopathology caused by a primary hookworm infection, the phenotype of the immune response switches over time to become regulatory in nature (see section on Host tolerance), allowing the host and the parasite to reach a status quo, in which the parasite burden is regulated and tolerated by many infected individuals.
Immune clearance. In the N. brasiliensis experimental mouse model of human hookworm infection, acquired immunity manifests in the early stages of secondary infection. IgE-armed basophils are responsible for trapping larvae in the skin, thereby limiting their migration through the lungs and associated injury83. There is also evidence for clearance of parasites in the lungs, where long-lived M2 macrophages directly mediate rapid nematode damage and clearance85. In the gut, N. brasiliensis triggers TH2 cell responses, including the secretion of type 2 cytokines, such as IL-4 and IL-13, and the induction of goblet cell hyperplasia and mucus production, all of which culminate in worm expulsion (Fig. 4). Moreover, the production of IL-25 by intestinal tuft cells was recently shown to be a key early event in triggering protective TH2 cell responses in this model86.
Feeding worms bury their anterior ends in the wall of the small bowel, where they physically rupture cells within the mucosa and actively release excretory–secretory (ES) products. Damaged cells release alarmins, which, along with ES products, act directly on dendritic cells (DCs) and type 2 innate lymphoid cells (ILC2s), which in turn induce the development of T helper 2 (TH2) cells. TH2 cells, through secretion of IL-4 and IL-13, promote B cells to secrete IgE antibodies, which crosslink antigens on basophils and mast cells to trigger histamine release through degranulation. TH2 cells also secrete IL-5, which activates eosinophils and promotes degranulation. ILC2, activated DCs and T cells release IL-22, which triggers epithelial cell turnover and mucus production by goblet cells. Disruption of the intestinal barrier can result in changes to the composition of the resident microbiota, and translocation of microbial products can exacerbate pathology.
Unlike in the mouse model of N. brasiliensis infection, immunological clearance of hookworm infection in humans is less apparent, and, despite robust immune responses, substantial parasite numbers persist in the human host into old age. The kinetics of the antibody response has been addressed in controlled human challenge infections57,59,87. IgA, IgD, IgE, IgG1, IgG4 and IgM antibodies from individuals who live in hookworm-endemic settings have all been shown to bind to hookworm antigens88,89. IgE has a protective, anti-parasite role in many helminth infections90 and has, therefore, been of particular interest in efforts to combat hookworm disease. In Papua New Guinea, it was shown that IgE, either parasite-specific or polyclonal, afforded partial protection against hookworm infection91,92. As with other helminth infections, IgE responses seem to develop over multiple exposures56,93. Despite the robust IgE response that is induced by hookworm infection, isotypes that counterbalance the protective nature of IgE, such as IgG4, are dominant in chronic human infections. In other human helminthiases, for example, filariasis and schistosomiasis, parasite-specific IgG4 correlates with a modified TH2 immune response, which can be differentiated from the parasite-killing (and often more pathogenic) IgG1 and IgE isotypes94. A similar situation probably exists in hookworm infection, as a parasite-specific IgG4 response is a good predictor of hookworm infection95,96. Thus, if the immune response to hookworm is diverted from a modified TH2–IgG4 response towards a potentially protective TH2–IgE response, anti-parasite immunity might indeed be possible97.
Host tolerance. Co-evolution of helminths and humans has resulted in a status quo: on the one hand, anthelmintic, protective TH2 immune responses limit hookworm numbers to manageable levels, whereas, on the other hand, over time, regulatory responses develop, which protect the host from excessive immunopathology but also prevent resident hookworms from being ejected by immune effector mechanisms. This phenomenon is exquisitely exemplified in the hookworm–human host relationship. The association between helminths and humans is so intimate that helminths have been credited with influencing entire arms of the human immune system. For example, the TH2 cell response is thought to have evolved to fight helminths and mop up (or contain) the damage they induce during their migration and feeding98. Hookworms can regulate inflammation in a complex and multifactorial way. Like many other helminths, hookworms are potent inducers of regulatory immune responses that are aimed at promoting their own survival and reproductive capacity. In humans, the expansion of regulatory T cells (Treg cells) has been reported in many helminth infections in endemic settings, including hookworm infection (reviewed in Ref. 99). Peripheral blood mononuclear cells from individuals infected with hookworm that are pulsed with hookworm antigens had an impaired proliferative capacity, which was partially augmented by the depletion of Treg cells100. Moreover, studies with low-dose experimental N. americanus infection in human volunteers showed a remarkable absence of inflammation surrounding feeding worms (Fig. 3d), an expansion of Treg cell numbers in the gut9,58 and upregulation of microRNAs that encode the regulatory cytokines IL-10 and transforming growth factor-β (TGFβ) and the intestinal wound-repair cytokine IL-22. In addition, intestinal tissue from humans who are experimentally infected with hookworms shows an increased expression of genes in the retinoic acid pathway, indicating the presence of tolerogenic dendritic cells, which might imprint gut homing on resident T cells58 (Fig. 5).
The secretion of excretory–secretory (ES) products from hookworms and the release of alarmins from damaged cells trigger the activation of type 2 innate lymphoid cells (ILC2s) and tolerogenic dendritic cells (DCs). As adult hookworms establish a chronic infection in the gut, tolerogenic pathways are triggered. DCs express reduced levels of activation and co-stimulatory markers and increased levels of molecules associated with tolerance, such as enzymes of the retinoic acid production pathway and transforming growth factor-β (TGFβ), which in turn generate anergic T helper 2 (TH2) cells and regulatory T cells (Treg cells) that express mucosal homing markers, such as CC-chemokine receptor 9 (CCR9) and the downregulatory checkpoint receptor cytotoxic T lymphocyte protein 4 (CTLA4) to prevent TH1 cell-mediated and TH17 cell-mediated damage. ILC2s and anergic TH2 cells produce type 2 cytokines (IL-4 and IL-13) that promote alternative activation of M2 macrophages, which adopt a wound-healing phenotype and prevent TH1-mediated damage. Increased mucus production triggered by IL-22, among other unknown factors, supports the maintenance of a species-rich microbiota, including bacteria that release short-chain fatty acids that promote Treg cell function.
Products from the resident gut microbiota, such as DNA and lipopolysaccharide (LPS), have been shown to cross the disrupted gastrointestinal endothelial barrier in diseases such as inflammatory bowel disease or upon treatment for HIV infection (reviewed in Ref. 101). This translocation has immunological consequences: inflammation in the short term, but possibly the establishment of an anti-inflammatory state if there is chronic exposure to microbial products. In India, an area that is endemic for hookworm infection, the levels of LPS and other markers of microbial translocation were increased in individuals infected with hookworm compared with uninfected controls102. However, this increased microbial transfer was not associated with any acute-phase response, and indeed C-reactive protein levels were significantly decreased in these individuals. The lack of systemic inflammation was confirmed by unaltered levels of pro-inflammatory cytokines in the circulation, whereas the levels of anti-inflammatory cytokines, such as IL-10, were substantially increased and strongly correlated with the levels of LPS in circulation. Anthelmintic treatment lowered LPS levels, which indicates that hookworm infection was the cause of the increased microbial transfer. Dissecting the complex series of interactions between hookworms, microbiota and immunoregulation is now a priority, particularly in light of the current enthusiasm generated by the potential use of hookworms and their secreted products as the next generation of biologics to treat inflammation. The importance of the three-way relationship between microbiota, macrobiota (macroscopic residents of the gut, such as hookworms) and inflammation is only now being recognized (Box 1).
Diagnosis, screening and prevention
Diagnostics
Hookworm diagnostics are used to confirm infection in clinical settings, map hookworm infections to identify ‘hotspots’ of transmission for targeted intervention and evaluate MDA campaigns. Examination (microscopic or molecular) of faecal samples is essential to diagnose hookworm infection103 (Box 2; Table 1).
As the prevalence of hookworm infection declines dramatically in locally defined settings, highly sensitive diagnostic methods are required to determine whether transmission has in fact been reduced after intensive MDA, particularly if other preventive measures have not been implemented104. In this regard, the detection of hookworm eggs in the faeces becomes imperative. The conventional egg-counting techniques (Box 3) are inadequate in efforts to detect the extremely low egg counts that would be expected after intensive MDA has been implemented and transmission is ‘rebounding’ (Ref. 104). As such, recent efforts have been devoted to the development of PCR-based methods (Table 1), which are still being validated for their ability to determine quantitative eggs counts. However, some of these tests have already proven to be more effective for the detection of hookworm infection than conventional diagnostics, which cannot identify extremely low numbers of hookworm eggs that are shed in faeces105. Indeed, one such multiplex quantitative PCR faecal assay can potentially differentiate hookworm species and obtain direct information on quantitative intestinal helminthic and protozoan infections105.
In addition, when diagnostics are used to quantify EPG, the objective is to assess (by this proxy) the worm burden of an individual to determine if that individual is at risk of morbidity from hookworm infection. That is, measurements of EPG can identify individuals, especially children and women of childbearing age, who are likely to develop IDA and associated outcomes.
Prevention
The focus of most current control strategies is preventive chemotherapy through MDA (discussed below). However, complete elimination or at least long-term control and reduction in the prevalence of hookworm and other STH infections will probably require, besides MDA, general sanitary improvements, as shown in the Water, Sanitation and Hygiene (WASH) programme. This programme has been most promising as an integrated approach to the prevention of diarrhoeal diseases106,107. WASH interventions are diverse and include a range of improvements in water conditions (such as quality, quantity and access), sanitation (such as improved latrines and sewer maintenance) and hygiene (for example, adopting good personal hygiene habits, such as hand washing before eating and after defaecation, wearing shoes and safely storing water)108–110. Another key feature of WASH programmes is community engagement and awareness, with a particular focus on improving the general population's understanding of what constitutes unhygienic behaviour, such as open defaecation.
WASH programmes hold periodic community-based health education activities, such as the convening of community boards or community events, to discuss the sanitation and hygiene problems in the locale. WASH interventions also use innovative pedagogical methods, especially educational devices (for example, flashcards, games, songs and videogames), to teach children in endemic areas sanitation and hygiene111. Promoting the use of footwear has been a successful component of community engagement WASH programmes for the control of hookworm infection107. However, some studies suggest that the use of footwear to prevent hookworm infection is not supported by robust evidence112. Hookworm larvae can penetrate human skin anywhere in the body and exposure to hookworm larvae is not limited to the hands and feet; for example, during agricultural activities, such as dry rice cultivation, the naked chest and arms are also exposed.
There are few studies to date that look directly at the role of WASH programmes in controlling STH infections and even fewer that look solely at the effect of WASH programmes on hookworm infection. In the context of STH infections, WASH interventions have been associated with reduced odds of STH infection107. Individuals who had access to and used sanitation facilities were at lower risk of STH infections than individuals without sanitation113. Nevertheless, additional evidence of the benefits of WASH programmes in the reduction of STH infections is needed to improve the coordination between MDA and WASH interventions114.
In the United States, South Korea, Australia and Japan115,116, improvements in habitat and lifestyle similar to those advocated and implemented by WASH programmes led to the elimination of hookworm and other STH infections. These achievements demonstrate the potential effectiveness of WASH programmes. However, hygiene improvements in these countries were accompanied by improved economic conditions, and it is likely that general economic development and its accompanying forces of urbanization represent more-powerful forces for reducing hookworm prevalence and intensity than WASH programmes as an isolated measure. To date, MDA and WASH interventions in low-resource countries have not resulted in remarkable long-term declines in hookworm prevalence and intensity in the absence of simultaneous substantial economic development. Thus, WASH-related improvements might be more challenging to achieve in rural communities that are located in resource-limited settings, many of which still rely on subsistence economy. The construction of latrines in rural and remote schools and the use of household waste to produce biogas, a process that helps to reduce the pathogen load in night soil117, are two modest but relevant changes that can contribute to the disruption of the life cycle of hookworms. Finally, all these considerations have stimulated interest in developing a hookworm vaccine (discussed below).
Management
Benzimidazole-based therapies
Currently, the two most commonly used drugs for the treatment of N. americanus and A. duodenale infections worldwide are mebendazole and albendazole, both of which are benzimidazole anthelmintic drugs (Table 2). These drugs act by inhibiting microtubule polymerization in invertebrates, therefore killing adult worms. Both N. americanus and A. duodenale have similar susceptibility to benzimidazoles; nevertheless, there are important differences in therapeutic efficacy between mebendazole and albendazole118. A single 400 mg dose of albendazole is more effective than a single 500 mg dose of mebendazole; a systematic review and meta-analysis of published randomized controlled trials of treatment for hookworm infection found an overall cure rate of 72% for a single dose of albendazole and 15% for a single dose of mebendazole118. Similarly, another study conducted in 1,845 schoolchildren at seven sites worldwide reported an overall cure rate of 87.8% for a single dose of albendazole, although this rate varied considerably across countries, age groups and different pretreatment intensity of infection119. Thus, despite their promise, the efficacies of these benzimidazole drugs in treating human hookworm infection can be highly variable, with surprisingly high rates of single-dose drug failure noted for both mebendazole and albendazole6,7. Three consecutive daily doses of either drug improve both cure and egg reduction rates, but this option is less convenient for MDA programmes, in which single-dose treatment is preferred120. Interestingly, the formulation of these drugs probably affects their bioavailability in the intestine, as different formulations of the same drug, which are produced by different manufacturers, result in different efficacies121.
The reasons for the observed failures of mebendazole or albendazole to treat human hookworm infections are unclear. Repeated use of mebendazole in the same communities has been associated with diminishing efficacy over time, which suggests the emergence of drug resistance, although this hypothesis remains controversial122. However, resistance to benzimidazoles that are used in animal husbandry has been observed in intestinal nematodes infecting livestock and it has been linked to point mutations in the β-tubulin gene in the parasite genome123. Thus, research is ongoing to determine whether albendazole and mebendazole failure to treat hookworm and other STH infections are caused by similar resistance mechanisms124.
Both albendazole and mebendazole have excellent safety profiles in the doses used to treat hookworm infection125, although transient abdominal pain, diarrhoea, nausea, dizziness and headache might occur. As benzimidazoles are embryotoxic and teratogenic in pregnant rats and rabbits, there have been concerns about the use of these drugs in children <1 year of age and in pregnant women. To date, teratogenicity in humans has not been observed, and a study of >800 women who were treated with albendazole during the second and third trimesters demonstrated no adverse effects126. However, albendazole use in the first trimester is not recommended. Similarly, despite the lack of formal safety studies of albendazole or mebendazole in children <2 years of age, both drugs have been widely used to treat entire communities irrespective of the age of the individuals as part of MDA programmes127, with no reports of adverse effects in children. As a result, the WHO recommends that both drugs can be used safely in children ≥1 year of age128 (Table 2).
Alternative treatment approaches
Despite concerns about the sustainability of MDA with benzimidazoles and the potential emergence of resistance, few effective alternatives for the treatment of hookworm infection are available or being developed. Pyrantel pamoate and levamisole are alternative drugs, although neither is as effective as albendazole. Both drugs interfere with the function of nicotinic acetylcholine receptors on the body muscle of hookworms, which leads to muscle cell depolarization and spastic paralysis that result in expulsion of the worm from the gastrointestinal tract129. Tribendimidine, which is a synthetic derivative of amidantel that acts as a nicotinic acetylcholine receptor agonist, is also emerging as a treatment, and was highly active against hookworm infection in both animal models and human studies130. This drug was originally developed in the 1980s in China, where it was registered for human use in 2004, although no other country has approved it yet131.
Pore-forming crystal (Cry) proteins, which are derived from Bacillus thuringiensis132, show in vivo activity against A. ceylanicum133. In particular, Cry5B in combination with a nicotinic acetylcholine receptor agonist has synergistic activity against intestinal nematodes132.
Finally, combination therapy using drugs with different mechanisms of action could improve treatment efficacy and stall the emergence of resistance, although it has not become common practice, as there is little data from well-designed clinical trials134. One trial combined single-dose albendazole with single-dose oxantel pamoate (an orthologue of pyrantel pamoate that is used in veterinary medicine) or ivermectin, but cure rates were only approximately 40–50% compared with 24% for single-dose mebendazole135. Most combination therapies would be expected to improve efficacy of trichuriasis treatments, but similar results might not be true for hookworm infection, as ivermectin or oxantel pamoate do not show substantial drug activity against it.
In industrialized countries, iron deficiency occurs only with chronic infections of moderate or heavy intensity. Thus, iron supplementation treatment is not routinely practiced in areas with access to benzimidazole anthelmintics. In resource-poor settings (where iron deficiency is most prevalent), no strong evidence supports that iron supplementation provides added benefits, except possibly in pregnant women with severe anaemia due to hookworm infection136,137. Options for iron replacement include ferrous sulfate, ferrous gluconate or ferrous fumarate. To replete iron stores, treatment must continue for 3–6 months after haemoglobin concentration has been restored to physiological levels. The most common adverse effect of oral iron supplementation is gastrointestinal intolerance, including epigastric pain, nausea, vomiting, constipation and diarrhoea. Formulations with lower levels of elemental iron, liquid formulations or taking the formulation with food (although this option might reduce absorption) might reduce symptoms.
MDA
Goals. Chronic infection with hookworm or other STHs leads to undernutrition and impairs physical and cognitive development in children. Thus, control programmes based on frequent and periodic MDA to children in endemic areas have been implemented, with the goal of large-scale reduction in the burden of these diseases. In 2001, a WHO resolution urged member states to regularly treat high-risk groups and ≥75% of at-risk preschool and school-aged children by 2020. Unfortunately, it does not seem likely that this goal will be achieved despite substantial expansion of MDA programmes over the past decade138,139.
Good-quality, non-proprietary, inexpensive benzimidazoles are widely available. Treating children with benzimidazoles regularly diminishes hookworm burdens, maintaining them below the disease-causing threshold140,141. Studies in preschool children have shown that anthelmintic treatment improved nutritional indicators, including stunted growth and muscle wasting142,143. MDA treatment also decreases the number of hookworm eggs that are shed into the environment, therefore contributing to reduced transmission. However, elimination in endemic countries by MDA alone is unlikely, as large numbers of infected adults are not currently targeted by MDA programmes5,139.
Limitations. The principal drawback of MDA programmes is that re-infection often occurs rapidly once treatment stops8,144. Hookworm re-infection can reach 25% of pretreatment levels as early as 18 weeks after albendazole treatment135. Annual treatment rounds of albendazole MDA in eastern Indonesia reduced the prevalence of hookworm infection from 28% to 4% after 5 years, but prevalence rebounded to near the initial rate within 3 years after cessation of MDA, although infection intensities were lower145.
Another concern regarding MDA interventions is the findings of unusually high rates of outright drug failure with either mebendazole or albendazole6,7 as well as the potential emergence of drug resistance, which is already widespread in livestock nematodes because of ubiquitous benzimidazole use146. In fact, several reports of reduced cure rates of human hookworm infection have been published7,147,148. In addition, the efficacy of single-dose albendazole and mebendazole can be highly variable, with frequent episodes of drug failure149,150.
Despite MDA successfully lowering the prevalence of ascariasis, re-infection and variable drug efficacies might have contributed to MDA failure of reducing global hookworm prevalence over the past 23 years. For instance, the 2013 Global Burden of Disease Study found that hookworm prevalence has decreased by only 5% compared with a 25% decrease for ascariasis21. Thus, eliminating the public health problem that endemic hookworm infection causes will probably also require simultaneous and substantial economic development and sanitation improvements in affected areas.
Quality of life
Compared with other neglected tropical diseases151, there is a dearth of qualitative or social science studies on hookworm infection. The main consequence of parasite feeding and intestinal blood loss is iron deficiency, which eventually leads to IDA. Hookworm disease especially affects populations with low underlying iron reserves (for example, children and women of childbearing age) with moderate or heavy infections.
Women and children
Moderate and heavy hookworm infections can cause anaemia in pregnant33 and non-pregnant women27. IDA in pregnancy can lead to poor outcomes for both the mother and the baby in resource-limited countries33,152, including reduced fertility29, maternal morbidity and even mortality and reduced child survival34,152.
Systematic evidence also links anaemia to moderate and heavy hookworm infections in children27. The paediatric physical consequences of hookworm disease include reduced pubertal and post-pubertal growth and fitness153 and were first described in the 1920s154. Similarly, by the 1920s, moderate and heavy hookworm infections were linked to reduced intelligence (‘mental sluggishness’)155, and more-recent studies have supported an association between hookworm infection and cognitive delays in children31. However, direct measurement of health-related quality of life among school-aged children using generic instruments was shown not to be sufficiently sensitive to measure the effect of parasitic infections (including hookworm infection) in Cote d'Ivoire156 and Yunnan Province, China157. Thus, more-precise and tailored instruments to assess quality of life are needed.
Productivity and poverty
As highlighted above, the most recent estimates indicate that hookworm infection globally is linked to 4.1 million DALYs lost, ranking it among the most serious of the neglected tropical diseases along with schistosomiasis and leishmaniasis2. Chronic hookworm infection also reinforces poverty in low-income and middle-income countries through its long-term debilitating effects15. For instance, an analysis of paediatric hookworm infection in the southern United States in the early twentieth century showed that it resulted in a substantial drop in future wage-earnings158. Additional (mostly anecdotal) evidence shows the long-term damage of hookworm infection to worker productivity, especially in agricultural activities159. Anaemia associated with helminth infections (presumably mostly hookworm infection) among female tea pluckers in Bangladesh decreased labour productivity and increased sick days160, although among anaemic Sri Lankan tea pluckers, low dietary iron intake was a more important determinant than hookworm disease161. It is difficult to attribute these adverse effects on productivity specifically to hookworm infection rather than to other STH infections or alternative causes of undernutrition. Recently, the Public Health Computational and Operational Research (PHICOR) group at Johns Hopkins University provided new economic impact assessments of hookworm infection, finding that total productivity losses were as high as US$139 billion annually2.
Effects of treatment
In a systematic analysis, single-dose mebendazole in MDA programmes had no effect on improving hookworm disease27, which is consistent with the low efficacy and occasional failure of this drug6. Conversely, albendazole improved anaemia in doses that are commonly used during MDA programmes27. However, other studies have indicated that albendazole often fails to adequately treat hookworm infection in MDA programmes in low-income settings7,150, findings that might partly explain why a 2015 Cochrane analysis could not always find strong evidence for the therapeutic effect of deworming interventions149. In terms of quality of life, there are minimal studies available, but in at least one case, anthelmintic treatment does not show a direct effect on worker productivity160. Interestingly, treatment of cutaneous larva migrans resulted in substantial improvements in quality of life162.
Comorbidities
In Africa, hookworm and malaria co-infections are widespread and can lead to severe anaemia20,163. Indeed, regions of predicted hookworm prevalence (based on both the observed prevalence among school-aged children and the satellite-derived environmental data) mirror the areas that have climatic suitability for Plasmodium falciparum malaria transmission163. Systematic reviews confirm that school-aged children and pregnant women in particular are at risk for malaria and hookworm co-infections20,163. However, whereas hookworm disease is due to intestinal blood loss, malaria-induced anaemia results from haemolysis, splenic sequestration and dyserythropoiesis. Thus, the two infections can produce comorbidities that lead to anaemia, but arrive at this clinical sequela through different mechanisms. Similarly, co-infections with hookworms and schistosomes (especially Schistosoma mansoni) are also common in Africa164. Schistosomiasis anaemia is a result of chronic inflammation and some blood loss. Triple infection with hookworms, schistosomes and P. falciparum are not uncommon on the African continent and might combine (along with high rates of haemoglobinopathies and inadequate diet) to produce additive haematological effects — a ‘perfect storm’ of anaemia, which is a major issue, especially in rural Africa165.
Such findings have generated an interest in simultaneously preventing all three infections by linking intermittent preventive therapy for malaria with anthelminthic MDA165 or by co-formulating hookworm, schistosome and P. falciparum antigens in a multivalent vaccine166. As the malaria vaccine RTS,S advances towards licensure, it would be interesting to explore how it could be combined with one or more hookworm or schistosome antigens that are currently under development.
Outlook
Prospects for a hookworm vaccine
Hookworm infection, like most other neglected tropical diseases, is a disease of impoverished people. The WHO has proposed annual albendazole or mebendazole MDA of entire populations or age strata within an endemic area as the most cost-effective means of reducing morbidity caused by chronic intestinal helminth infections167. However, annual deworming might be less effective for hookworm infection than for other STH infections139,168, possibly owing to benzimidazole drug failures and post-treatment reinfections. Indeed, the 2013 Global Burden of Disease Study found that the global prevalence of hookworm infection is nearly unchanged despite more than two decades of deworming21,169. Such concerns about the sustainability of MDA programmes prompted the establishment of the Human Hookworm Vaccine Initiative (HHVI)170–172, an initiative of the non-profit product development partnership of the Sabin Vaccine Institute. The goal of the HHVI is to develop a subunit vaccine that prevents moderate and heavy hookworm infections, therefore minimizing intestinal blood loss caused by feeding adult worms (Box 4).
The development of vaccines for neglected tropical diseases is being led by non-profit product development partnerships in collaboration with academic and industrial partners, including vaccine manufacturers based in resource-limited countries. Thus, issues that are often taken for granted in vaccine development (such as manufacturing cost and cold chain logistics) combined with insufficient financial investment are major hurdles in the development of neglected tropical disease vaccines — and a pressing issue for public health in general.
Hookworm infection to treat inflammatory diseases
Hookworm infection has been viewed in an entirely different light since the publication of the first clinical trial on the therapeutic use of experimental human hookworm infection to treat inflammatory diseases10. The epidemiological association between helminth infection and reduced susceptibility to inflammatory diseases has been proposed173,174, with compelling examples of hookworm infection protecting against the onset of allergies. Indeed, negative associations have been reported between hookworm infection and the risk of wheeze84, dust mite allergy175 and even metabolic diseases as determined by insulin sensitivity176. Furthermore, studies in populations from poor-hygiene areas migrating to high-sanitation regions have shown that these individuals have an increased risk of inflammatory diseases177, although there might be other contributing factors (such as changes in the host microbiota). The lack of exposure to pathogens, such as hookworms, often combined with genetic predisposition, can uncover underlying inflammatory diseases178. However, it has also been pointed out that elements of the helminth-associated ‘hygiene hypothesis’ are often not so clear-cut. For example, helminth infections that lead to inflammatory diseases are surprisingly prevalent in high-income countries, whereas some helminth species can actually promote inflammatory states179.
Nevertheless, some of the observations highlighted above have led to clinical trials using iatrogenic helminth infections to treat inflammatory diseases, which have had mixed results180. Experimental human hookworm infection exhibited no effect on asthma or allergic rhinitis11,181. However, experimental hookworm infection restored gluten tolerance in individuals affected by coeliac disease when coupled with increasing dietary gluten. Infection with 20 worms enabled patients to tolerate gluten doses corresponding to a medium-sized bowl of pasta every day for 2 weeks, with no clinical, histological or immunological evidence of inflammation9 (Fig. 6).
Individuals affected by coeliac disease who are on a regular diet that contains gluten develop inflammation in the gut, which leads to blunting of the villi and hyperplasia of the crypts (inset, left). In healthy individuals and in diet-treated patients with coeliac disease, the villus-height-to-crypt-depth ratio exceeds 3:1. After commencing a strict gluten-free diet, it takes approximately 1 year for the morphology of the duodenal epithelium to be restored to a healthy state (inset, middle), but much less time for its appearance to deteriorate when gluten is re-introduced in the diet. Individuals affected by coeliac disease and on a strict long-term gluten-free diet were infected with 20 Necator americanus third-stage larvae and were fed increasing amounts of pasta (oral gluten) over a 52-week period9. Controlled hookworm infection resulted in protection against villous blunting and other inflammatory changes that characterize coeliac disease (inset, right).
Although the mechanisms behind the therapeutic benefits of hookworm infection are unclear, both infected healthy individuals and patients with coeliac disease had reduced levels of inflammatory cytokines and increased levels of regulatory cytokines and Treg cells in the gut9,58. Moreover, infection of patients with coeliac disease with hookworms resulted in an increased richness of commensal microbial species in the gut182 and increased concentrations of anti-inflammatory short-chain fatty acids derived from the microbiota183.
The notion of live helminth therapy is unpalatable to many people, so the development of the worm itself as a marketable drug product would face substantial regulatory hurdles. However, the immunoregulatory prowess of hookworms seems to reside within their secretomes. Adult-stage hookworms that are recovered from definitive hosts after euthanasia can be cultured in vitro whereupon they secrete various molecules, including proteins, peptides, glycans and small molecules, which are collectively referred to as excretory–secretory (ES) products. ES products of A. caninum have been shown to protect mice against chemically induced colitis184–186. Defined synthetic ES peptides have been shown to suppress T cell proliferation187, and a recombinant hookworm protein with sequence identity to mammalian tissue inhibitor of metalloproteinase protected mice against asthma by inducing tolerogenic dendritic cells and expanding Treg cell numbers that homed to mucosal sites of inflammation188. Moreover, a recombinant ES protein that binds to the CD11b integrin prevents neutrophil accumulation and is neuroprotective after focal ischaemia in rats189, and even underwent phase IIa clinical trials for stroke190. The unique specificity and potency of hookworm antithrombotics have also generated substantial interest in their use for treating a range of vascular pathologies, including heart disease, stroke and even cancer191. The ES proteome of A. caninum has been characterized using tandem mass spectrometry43, and the recent publication of the N. americanus genome and immunome44 will facilitate the discovery of new proteins with potential as novel biologics, as well as vaccine and diagnostic antigens to control and ultimately eradicate hookworm disease.
Final words
Hookworm infection has plagued humans for millennia and there are descriptions of helminths in the earliest medical texts from 1500 BC192. Hookworms are one of the most exquisitely adapted human parasites and are capable of overcoming the barrage of physical and physiological challenges they encounter along their migratory route within the host. They can survive for decades in the gastrointestinal tract despite an immune onslaught targeting hundreds of antigens44 (A.L., unpublished observation). Indeed, the ability of this ancient parasite to avoid the immune system might well hold the key to the control of modern-day immune and metabolic diseases. Despite huge international efforts to control hookworm and other STH infections, little progress has been made. Now more than ever, new strategies are needed. The continuous use of currently available drugs and the development of new ones are fundamental, and so are substantial investments towards economic development and improved sanitation in endemic, resource-limited regions. However, drugs alone are not likely to eliminate hookworm infection, especially given the variability of mebendazole and albendazole efficacies. Thus, a human hookworm vaccine would represent a leap towards global elimination. Much work lies ahead for public health workers, clinicians and biomedical scientists to eradicate hookworm infection from endemic countries while harnessing its untapped therapeutic properties.
References
Pullan, R. L., Smith, J. L., Jasrasaria, R. & Brooker, S. J. Global numbers of infection and disease burden of soil transmitted helminth infections in 2010. Parasit. Vectors 7, 37 (2014).
Bartsch, S. M. et al. The global economic and health burden of human hookworm infection. PLoS Negl. Trop. Dis. 10, e0004922 (2016). This computational simulation model estimates the economic and health burden of hookworm infection, highlighting that countries transitioning to higher income, such as Brazil and China, still face considerable hookworm burden.
Brown, E. R. Public health in imperialism: early Rockefeller programs at home and abroad. Am. J. Public Health 66, 897–903 (1976).
International Health Division of the Rockefeller Foundation. Unhooking the hookworm. YouTubehttps://www.youtube.com/watch?v=OD-sDlSDrKk (1920).
Bartsch, S. M. et al. Modeling the economic and epidemiologic impact of hookworm vaccine and mass drug administration (MDA) in Brazil, a high transmission setting. Vaccine 34, 2197–2206 (2016).
De Clercq, D. et al. Failure of mebendazole in treatment of human hookworm infections in the southern region of Mali. Am. J. Trop. Med. Hyg. 57, 25–30 (1997).
Soukhathammavong, P. A. et al. Low efficacy of single-dose albendazole and mebendazole against hookworm and effect on concomitant helminth infection in Lao PDR. PLoS Negl. Trop. Dis. 6, e1417 (2012).
Albonico, M. et al. Rate of reinfection with intestinal nematodes after treatment of children with mebendazole or albendazole in a highly endemic area. Trans. R. Soc. Trop. Med. Hyg. 89, 538–541 (1995).
Croese, J. et al. Experimental hookworm infection and gluten microchallenge promote tolerance in celiac disease. J. Allergy Clin. Immunol. 135, 508–516 (2015).
Croese, J. et al. A proof of concept study establishing Necator americanus in Crohn's patients and reservoir donors. Gut 55, 136–137 (2006).
Feary, J. et al. Safety of hookworm infection in individuals with measurable airway responsiveness: a randomized placebo-controlled feasibility study. Clin. Exp. Allergy 39, 1060–1068 (2009).
Summers, R. W. et al. Trichuris suis therapy for active ulcerative colitis: a randomized controlled trial. Gastroenterology 128, 825–832 (2005).
Inpankaew, T. et al. High prevalence of Ancylostoma ceylanicum hookworm infections in humans, Cambodia, 2012. Emerg. Infect. Dis. 20, 976–982 (2014). This study shows that A. ceylanicum — usually thought of as a parasite of dogs and only a minor human species — was responsible for more than half of human hookworm infections in a rural Cambodian village and attributes infection to preventative chemotherapy in the absence of concurrent hygiene and animal health programmes.
Traub, R. J. Ancylostoma ceylanicum, a re-emerging but neglected parasitic zoonosis. Int. J. Parasitol. 43, 1009–1015 (2013).
Hotez, P. Hookworm and poverty. Ann. NY Acad. Sci. 1136, 38–44 (2008).
Haswell-Elkins, M. R., Elkins, D. B., Manjula, K., Michael, E. & Anderson, R. M. An investigation of hookworm infection and reinfection following mass anthelmintic treatment in the south Indian fishing community of Vairavankuppam. Parasitology 96, 565–577 (1988).
Montresor, A., Compton, D. W. T., Hall, A., Bundy, D. A. P. & Savioli, L. Guidelines for the Evaluation of Soil-Transmitted Helminthiasis and Schistosomiasis at Community Level (WHO, 1998).
Roche, M. & Layrisse, M. The nature and causes of “hookworm anemia”. Am. J. Trop. Med. Hyg. 15, 1029–1102 (1966).
Albonico, M. et al. Epidemiological evidence for a differential effect of hookworm species. Ancylostoma duodenale or Necator americanus, on iron status of children. Int. J. Epidemiol. 27, 530–537 (1998).
Brooker, S. et al. Epidemiology of plasmodium-helminth co-infection in Africa: populations at risk, potential impact on anemia, and prospects for combining control. Am. J. Trop. Med. Hyg. 77, 88–98 (2007).
GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 385, 117–171 (2015).
Hotez, P. J., Bottazzi, M. E. & Strych, U. New vaccines for the world's poorest people. Annu. Rev. Med. 67, 405–417 (2016).
Kassebaum, N. J. & GBD 2013 Anemia Collaborators. The global burden of anemia. Hematol. Oncol. Clin. North Am. 30, 247–308 (2016). This study reports on the estimated levels and trends of non-fatal anaemia burden in 188 countries from 1990 to 2013, highlighting that hookworm disease was second only to malaria as an underlying cause of global anaemia caused by parasitic infections.
Anderson, R. M., Truscott, J. E., Pullan, R. L., Brooker, S. J. & Hollingsworth, T. D. How effective is school-based deworming for the community-wide control of soil-transmitted helminths? PLoS Negl. Trop. Dis. 7, e2027 (2013).
Bethony, J. et al. Emerging patterns of hookworm infection: influence of aging on the intensity of Necator infection in Hainan Province, People's Republic of China. Clin. Infect. Dis. 35, 1336–1344 (2002).
Hotez, P. J. et al. Hookworm infection. N. Engl. J. Med. 351, 799–807 (2004).
Smith, J. L. & Brooker, S. Impact of hookworm infection and deworming on anaemia in non-pregnant populations: a systematic review. Trop. Med. Int. Health 15, 776–795 (2010).
Crompton, D. W. The public health importance of hookworm disease. Parasitology 121, S39–S50 (2000).
Blackwell, A. D. et al. Helminth infection, fecundity, and age of first pregnancy in women. Science 350, 970–972 (2015).
Dickson, R., Awasthi, S., Williamson, P., Demellweek, C. & Garner, P. Effects of treatment for intestinal helminth infection on growth and cognitive performance in children: systematic review of randomised trials. BMJ 320, 1697–1701 (2000).
Sakti, H. et al. Evidence for an association between hookworm infection and cognitive function in Indonesian school children. Trop. Med. Int. Health 4, 322–334 (1999).
Jardim-Botelho, A. et al. Hookworm, Ascaris lumbricoides infection and polyparasitism associated with poor cognitive performance in Brazilian schoolchildren. Trop. Med. Int. Health 13, 994–1004 (2008).
Brooker, S., Hotez, P. J. & Bundy, D. A. Hookworm-related anaemia among pregnant women: a systematic review. PLoS Negl. Trop. Dis. 2, e291 (2008).
Christian, P., Khatry, S. K. & West, K. P. Jr. Antenatal anthelmintic treatment, birthweight, and infant survival in rural Nepal. Lancet 364, 981–983 (2004).
Bundy, D. A., Chan, M. S. & Savioli, L. Hookworm infection in pregnancy. Trans. R. Soc. Trop. Med. Hyg. 89, 521–522 (1995).
Menzies, S. K. et al. Risk factors for soil-transmitted helminth infections during the first 3 years of life in the tropics; findings from a birth cohort. PLoS Negl. Trop. Dis. 8, e2718 (2014).
World Health Organization. Report of the WHO Informal Consultation on Hookworm Infection and Anaemia in Girls and Women (WHO, 1994).
Brand, A. & Hawdon, J. M. Phosphoinositide-3-OH-kinase inhibitor LY294002 prevents activation of Ancylostoma caninum and Ancylostoma ceylanicum third-stage infective larvae. Int. J. Parasitol. 34, 909–914 (2004).
Yoshida, Y., Matsuo, K., Kondo, K., Arizono, N. & Ogino, K. Scanning electron microscopy of hookworms. 1. Adults and infective-stage larvae of Necator americanus (Stiles, 1902). Southeast Asian J. Trop. Med. Public Health 5, 510–514 (1974).
Brown, A., Girod, N., Billett, E. E. & Pritchard, D. I. Necator americanus (human hookworm) aspartyl proteinases and digestion of skin macromolecules during skin penetration. Am. J. Trop. Med. Hyg. 60, 840–847 (1999).
Hotez, P. J. et al. Hyaluronidase from infective Ancylostoma hookworm larvae and its possible function as a virulence factor in tissue invasion and in cutaneous larva migrans. Infect. Immun. 60, 1018–1023 (1992).
Hawdon, J. M., Jones, B. F., Hoffman, D. R. & Hotez, P. J. Cloning and characterization of Ancylostoma-secreted protein. A novel protein associated with the transition to parasitism by infective hookworm larvae. J. Biol. Chem. 271, 6672–6678 (1996).
Mulvenna, J. et al. Proteomics analysis of the excretory/secretory component of the blood-feeding stage of the hookworm, Ancylostoma caninum. Mol. Cell Proteomics 8, 109–121 (2009).
Tang, Y. T. et al. Genome of the human hookworm Necator americanus. Nat. Genet. 46, 261–269 (2014). This study describes the genome, proteome and immunome of N. americanus, providing a valuable resource to bolster the discovery and development of new methods to control hookworm infection and human immunological diseases.
Diemert, D. J. et al. Generalized urticaria induced by the Na-ASP-2 hookworm vaccine: implications for the development of vaccines against helminths. J. Allergy Clin. Immunol. 130, 169–176.e6 (2012). This is the first clinical trial of a vaccine for human hookworm disease, highlighting the safety implications of vaccinating with antigens that are natural targets of IgE in endemic populations.
Ranjit, N. et al. Proteolytic degradation of hemoglobin in the intestine of the human hookworm Necator americanus. J. Infect. Dis. 199, 904–912 (2009).
Zhan, B. et al. Biochemical characterization and vaccine potential of a heme-binding glutathione transferase from the adult hookworm Ancylostoma caninum. Infect. Immun. 73, 6903–6911 (2005).
Stassens, P. et al. Anticoagulant repertoire of the hookworm Ancylostoma caninum. Proc. Natl Acad. Sci. USA 93, 2149–2154 (1996).
Layrisse, M., Linares, J. & Roche, M. Excess hemolysis in subjects with severe iron deficiency anemia associated and nonassociated with hookworm infection. Blood 25, 73–91 (1965).
Hoeppli, R. Parasites and Parasitic Infections in Early Science and Medicine (Univ. of Malaya Press, 1959).
Basta, S. S., Soekirman, Karyadi D. & Scrimshaw, N. S. Iron deficiency anemia and the productivity of adult males in Indonesia. Am. J. Clin. Nutr. 32, 916–925 (1979).
Mugisha, J. O., Baisley, K., Asiki, G., Seeley, J. & Kuper, H. Prevalence, types, risk factors and clinical correlates of anaemia in older people in a rural Ugandan population. PLoS ONE 8, e78394 (2013).
Olsen, A., Magnussen, P., Ouma, J. H., Andreassen, J. & Friis, H. The contribution of hookworm and other parasitic infections to haemoglobin and iron status among children and adults in western Kenya. Trans. R. Soc. Trop. Med. Hyg. 92, 643–649 (1998).
Stoltzfus, R. J., Dreyfuss, M. L., Chwaya, H. M. & Albonico, M. Hookworm control as a strategy to prevent iron deficiency. Nutr. Rev. 55, 223–232 (1997).
Hotez, P. J. China's hookworms. China Q. 172, 1029–1041 (2002).
Blount, D. et al. Immunologic profiles of persons recruited for a randomized, placebo-controlled clinical trial of hookworm infection. Am. J. Trop. Med. Hyg. 81, 911–916 (2009).
Maxwell, C. et al. The clinical and immunologic responses of normal human volunteers to low dose hookworm (Necator americanus) infection. Am. J. Trop. Med. Hyg. 37, 126–134 (1987).
Gaze, S. et al. Characterising the mucosal and systemic immune responses to experimental human hookworm infection. PLoS Pathog. 8, e1002520 (2012).
Daveson, A. J. et al. Effect of hookworm infection on wheat challenge in celiac disease — a randomised double-blinded placebo controlled trial. PLoS ONE 6, e17366 (2011).
Bowman, D. D., Montgomery, S. P., Zajac, A. M., Eberhard, M. L. & Kazacos, K. R. Hookworms of dogs and cats as agents of cutaneous larva migrans. Trends Parasitol. 26, 162–167 (2010).
Guill, M. A. & Odom, R. B. Larva migrans complicated by Loeffler's syndrome. Arch. Dermatol. 114, 1525–1526 (1978).
Prociv, P. & Croese, J. Human eosinophilic enteritis caused by dog hookworm Ancylostoma caninum. Lancet 335, 1299–1302 (1990). This study shows for the first time that A. caninum reached the human gut and was responsible for an outbreak of eosinophilic gastroenteritis in northern Australia, and was subsequently identified as a human pathogen in other endemic countries.
Croese, J., Loukas, A., Opdebeeck, J. & Prociv, P. Occult enteric infection by Ancylostoma caninum: a previously unrecognized zoonosis. Gastroenterology 106, 3–12 (1994).
Khoshoo, V. et al. Dog hookworm: a cause of eosinophilic enterocolitis in humans. J. Pediatr. Gastroenterol. Nutr. 19, 448–452 (1994).
Bahgat, M. A., El Gindy, A. E., Mahmoud, L. A., Hegab, M. H. & Shahin, A. M. Evaluation of the role of Ancylostoma caninum in humans as a cause of acute and recurrent abdominal pain. J. Egypt Soc. Parasitol. 29, 873–882 (1999).
Prociv, P. & Croese, J. Human enteric infection with Ancylostoma caninum: hookworms reappraised in the light of a “new” zoonosis. Acta Trop. 62, 23–44 (1996).
Behnke, J. M., Paul, V. & Rajasekariah, G. R. The growth and migration of Necator americanus following infection of neonatal hamsters. Trans. R. Soc. Trop. Med. Hyg. 80, 146–149 (1986).
Jian, X. et al. Necator americanus: maintenance through one hundred generations in golden hamsters (Mesocricetus auratus). I. Host sex-associated differences in hookworm burden and fecundity. Exp. Parasitol. 104, 62–66 (2003).
Camberis, M., Le Gros, G. & Urban, J. Jr. Animal model of Nippostrongylus brasiliensis and Heligmosomoides polygyrus. Curr. Protoc. Immunol. 55, 19.12.1–19.12.27 (2003).
Nair, M. G. & Herbert, D. R. Immune polarization by hookworms: taking cues from T helper type 2, type 2 innate lymphoid cells and alternatively activated macrophages. Immunology 148, 115–124 (2016).
Bungiro, R. D. et al. Mucosal antibody responses in experimental hookworm infection. Parasite Immunol. 30, 293–303 (2008).
Wells, C. & Behnke, J. M. Acquired resistance to the human hookworm Necator americanus in mice. Parasite Immunol. 10, 493–505 (1988).
Reynolds, L. A., Filbey, K. J. & Maizels, R. M. Immunity to the model intestinal helminth parasite Heligmosomoides polygyrus. Semin. Immunopathol. 34, 829–846 (2012).
Held, M. R., Bungiro, R. D., Harrison, L. M., Hamza, I. & Cappello, M. Dietary iron content mediates hookworm pathogenesis in vivo. Infect. Immun. 74, 289–295 (2006).
Alkazmi, L. M. & Behnke, J. M. The mucosal response of hamsters to a low-intensity superimposed secondary infection with the hookworm Ancylostoma ceylanicum. J. Helminthol. 85, 56–65 (2011).
Xiao, S. et al. The evaluation of recombinant hookworm antigens as vaccines in hamsters (Mesocricetus auratus) challenged with human hookworm. Necator americanus. Exp. Parasitol. 118, 32–40 (2008).
Miller, T. A. Transfer of immunity to Ancylostoma caninum infection in pups by serum and lymphoid cells. Immunology 12, 231–241 (1967).
Geiger, S. M., Fujiwara, R. T., Santiago, H., Correa-Oliveira, R. & Bethony, J. M. Early stage-specific immune responses in primary experimental human hookworm infection. Microbes Infect. 10, 1524–1535 (2008).
Fujiwara, R. T., Geiger, S. M., Bethony, J. & Mendez, S. Comparative immunology of human and animal models of hookworm infection. Parasite Immunol. 28, 285–293 (2006).
Griffiths, G. D. et al. Development of a model of hookworm infection exhibiting salient characteristics of human infection. Am. J. Trop. Med. Hyg. 78, 936–945 (2008).
Navarro, S., Ferreira, I. & Loukas, A. The hookworm pharmacopoeia for inflammatory diseases. Int. J. Parasitol. 43, 225–231 (2013).
Girod, N., Brown, A., Pritchard, D. I. & Billett, E. E. Successful vaccination of BALB/c mice against human hookworm (Necator americanus): the immunological phenotype of the protective response. Int. J. Parasitol. 33, 71–80 (2003).
Obata-Ninomiya, K. et al. The skin is an important bulwark of acquired immunity against intestinal helminths. J. Exp. Med. 210, 2583–2595 (2013).
Scrivener, S. et al. Independent effects of intestinal parasite infection and domestic allergen exposure on risk of wheeze in Ethiopia: a nested case–control study. Lancet 358, 1493–1499 (2001). This study shows that the risk of asthma was independently reduced by hookworm but not viral infection, indicating that parasitic infection might prevent asthma in atopic individuals.
Chen, F. et al. Neutrophils prime a long-lived effector macrophage phenotype that mediates accelerated helminth expulsion. Nat. Immunol. 15, 938–946 (2014).
Gerbe, F. et al. Intestinal epithelial tuft cells initiate type 2 mucosal immunity to helminth parasites. Nature 529, 226–230 (2016).
Ball, P. A. & Bartlett, A. Serological reactions to infection with Necator americanus. Trans. R. Soc. Trop. Med. Hyg. 63, 362–369 (1969).
Quinnell, R. J., Bethony, J. & Pritchard, D. I. The immunoepidemiology of human hookworm infection. Parasite Immunol. 26, 443–454 (2004).
Quinnell, R. J., Pritchard, D. I., Raiko, A., Brown, A. P. & Shaw, M. A. Immune responses in human necatoriasis: association between interleukin-5 responses and resistance to reinfection. J. Infect. Dis. 190, 430–438 (2004).
Cooper, P. J. et al. Geohelminth infections: a review of the role of IgE and assessment of potential risks of anti-IgE treatment. Allergy 63, 409–417 (2008).
Grove, D. I., Burston, T. O. & Forbes, I. J. Fall in IgE levels after treatment for hookworm. Clin. Exp. Immunol. 18, 565–569 (1974).
Grove, D. I. & Forbes, I. J. Increased resistance to helminth infestation in an atopic population. Med. J. Aust. 1, 336–338 (1975).
Falcone, F. H. et al. Antigen-driven basophil activation is indicative of early Necator americanus infection in IgE-seronegative patients. J. Allergy Clin. Immunol. 124, 1343–1350.e7 (2009).
Maizels, R. M. & Yazdanbakhsh, M. Immune regulation by helminth parasites: cellular and molecular mechanisms. Nat. Rev. Immunol. 3, 733–744 (2003).
Loukas, A., Opdebeeck, J., Croese, J. & Prociv, P. Immunoglobulin G subclass antibodies against excretory/secretory antigens of Ancylostoma caninum in human enteric infections. Am. J. Trop. Med. Hyg. 54, 672–676 (1996).
Palmer, D. R., Bradley, M. & Bundy, D. A. IgG4 responses to antigens of adult Necator americanus: potential for use in large-scale epidemiological studies. Bull. World Health Organ. 74, 381–386 (1996).
McSorley, H. J. & Loukas, A. The immunology of human hookworm infections. Parasite Immunol. 32, 549–559 (2010).
Allen, J. E. & Sutherland, T. E. Host protective roles of type 2 immunity: parasite killing and tissue repair, flip sides of the same coin. Semin. Immunol. 26, 329–340 (2014).
Wammes, L. J., Mpairwe, H., Elliott, A. M. & Yazdanbakhsh, M. Helminth therapy or elimination: epidemiological, immunological, and clinical considerations. Lancet Infect. Dis. 14, 1150–1162 (2014). This important review discusses the implication of mass deworming programmes on the potential emergence of inflammatory and metabolic conditions in developing countries that are ill-equipped for these new epidemics.
Ricci, N. D. et al. Induction of CD4+CD25+FOXP3+ regulatory T cells during human hookworm infection modulates antigen-mediated lymphocyte proliferation. PLoS Negl. Trop. Dis. 5, e1383 (2011).
Brenchley, J. M. & Douek, D. C. Microbial translocation across the GI tract. Annu. Rev. Immunol. 30, 149–173 (2012).
George, P. J. et al. Evidence of microbial translocation associated with perturbations in T cell and antigen-presenting cell homeostasis in hookworm infections. PLoS Negl. Trop. Dis. 6, e1830 (2012).
Verweij, J. J. Application of PCR-based methods for diagnosis of intestinal parasitic infections in the clinical laboratory. Parasitology 141, 1863–1872 (2014).
Easton, A. V. et al. Multi-parallel qPCR provides increased sensitivity and diagnostic breadth for gastrointestinal parasites of humans: field-based inferences on the impact of mass deworming. Parasit. Vectors 9, 38 (2016).
Cimino, R. O. et al. Identification of human intestinal parasites affecting an asymptomatic peri-urban Argentinian population using multi-parallel quantitative real-time polymerase chain reaction. Parasit. Vectors 8, 380 (2015).
Coffeng, L. E., Bakker, R., Montresor, A. & de Vlas, S. J. Feasibility of controlling hookworm infection through preventive chemotherapy: a simulation study using the individual-based WORMSIM modelling framework. Parasit. Vectors 8, 541 (2015).
Strunz, E. C. et al. Water, sanitation, hygiene, and soil-transmitted helminth infection: a systematic review and meta-analysis. PLoS Med. 11, e1001620 (2014). This systematic review and meta-analysis examines the associations of improved WASH on STH infections and found that WASH was generally associated with reduced odds of infection.
Cairncross, S. et al. Water, sanitation and hygiene for the prevention of diarrhoea. Int. J. Epidemiol. 39 (Suppl. 1), i193–i205 (2010).
Clasen, T. F. et al. Interventions to improve disposal of human excreta for preventing diarrhoea. Cochrane Database Syst. Rev. 6, CD007180 (2010).
Hunter, P. R., Ramirez Toro, G. I. & Minnigh, H. A. Impact on diarrhoeal illness of a community educational intervention to improve drinking water quality in rural communities in Puerto Rico. BMC Public Health 10, 219 (2010).
Bieri, F. A. et al. Health-education package to prevent worm infections in Chinese schoolchildren. N. Engl. J. Med. 368, 1603–1612 (2013).
Bird, C., Ame, S., Albonico, M. & Bickle, Q. Do shoes reduce hookworm infection in school-aged children on Pemba Island, Zanzibar? A pragmatic trial. Trans. R. Soc. Trop. Med. Hyg. 108, 297–304 (2014).
Ziegelbauer, K. et al. Effect of sanitation on soil-transmitted helminth infection: systematic review and meta-analysis. PLoS Med. 9, e1001162 (2012).
Freeman, M. C. & Clasen, T. Assessing the impact of a school-based safe water intervention on household adoption of point-of-use water treatment practices in southern India. Am. J. Trop. Med. Hyg. 84, 370–378 (2011).
Hong, S. T. et al. A successful experience of soil-transmitted helminth control in the Republic of Korea. Korean J. Parasitol. 44, 177–185 (2006).
Kobayashi, A., Hara, T. & Kajima, J. Historical aspects for the control of soil-transmitted helminthiases. Parasitol. Int. 55, S289–S291 (2006).
Hawdon, J. M. Controlling soil-transmitted helminths: time to think inside the box? J. Parasitol. 100, 166–188 (2014).
Keiser, J. & Utzinger, J. Efficacy of current drugs against soil-transmitted helminth infections: systematic review and meta-analysis. JAMA 299, 1937–1948 (2008). This analysis concludes that albendazole was more efficacious than mebendazole and pyrantel pamoate for treating hookworm infection, and that new anthelmintics for STH infections are urgently needed.
Vercruysse, J. et al. Assessment of the anthelmintic efficacy of albendazole in school children in seven countries where soil-transmitted helminths are endemic. PLoS Negl. Trop. Dis. 5, e948 (2011).
Steinmann, P. et al. Efficacy of single-dose and triple-dose albendazole and mebendazole against soil-transmitted helminths and Taenia spp.: a randomized controlled trial. PLoS ONE 6, e25003 (2011).
Belew, S. et al. Assessment of efficacy and quality of two albendazole brands commonly used against soil-transmitted helminth infections in school children in Jimma Town, Ethiopia. PLoS Negl. Trop. Dis. 9, e0004057 (2015).
Albonico, M. et al. Efficacy of mebendazole and levamisole alone or in combination against intestinal nematode infections after repeated targeted mebendazole treatment in Zanzibar. Bull. World Health Organ. 81, 343–352 (2003).
Demeler, J. et al. Phylogenetic characterization of beta-tubulins and development of pyrosequencing assays for benzimidazole resistance in cattle nematodes. PLoS ONE 8, e70212 (2013).
Diawara, A. et al. Association between response to albendazole treatment and β-tubulin genotype frequencies in soil-transmitted helminths. PLoS Negl. Trop. Dis. 7, e2247 (2013).
Dayan, A. D. Albendazole, mebendazole and praziquantel. Review of non-clinical toxicity and pharmacokinetics. Acta Trop. 86, 141–159 (2003).
Ndyomugyenyi, R., Kabatereine, N., Olsen, A. & Magnussen, P. Efficacy of ivermectin and albendazole alone and in combination for treatment of soil-transmitted helminths in pregnancy and adverse events: a randomized open label controlled intervention trial in Masindi district, western Uganda. Am. J. Trop. Med. Hyg. 79, 856–863 (2008).
Montresor, A., Awasthi, S. & Crompton, D. W. Use of benzimidazoles in children younger than 24 months for the treatment of soil-transmitted helminthiasis. Acta Trop. 86, 223–232 (2003).
World Health Organization. Report of the WHO Informal Consultation on the Use of Praziquantel During Pregnancy/Lactation and Albendazole/Mebendazole in Children Under 24 Months (WHO, 2002).
Kohler, P. The biochemical basis of anthelmintic action and resistance. Int. J. Parasitol. 31, 336–345 (2001).
Steinmann, P. et al. Tribendimidine and albendazole for treating soil-transmitted helminths. Strongyloides stercoralis and Taenia spp.: open-label randomized trial. PLoS Negl. Trop. Dis. 2, e322 (2008).
Xiao, S. H., Utzinger, J., Tanner, M., Keiser, J. & Xue, J. Advances with the Chinese anthelminthic drug tribendimidine in clinical trials and laboratory investigations. Acta Trop. 126, 115–126 (2013).
Hu, Y., Platzer, E. G., Bellier, A. & Aroian, R. V. Discovery of a highly synergistic anthelmintic combination that shows mutual hypersusceptibility. Proc. Natl Acad. Sci. USA 107, 5955–5960 (2010).
Hu, Y. et al. Mechanistic and single-dose in vivo therapeutic studies of Cry5B anthelmintic action against hookworms. PLoS Negl. Trop. Dis. 6, e1900 (2012).
Keiser, J. et al. Activity of oxantel pamoate monotherapy and combination chemotherapy against Trichuris muris and hookworms: revival of an old drug. PLoS Negl. Trop. Dis. 7, e2119 (2013).
Speich, B. et al. Efficacy and reinfection with soil-transmitted helminths 18-weeks post-treatment with albendazole–ivermectin, albendazole–mebendazole, albendazole–oxantel pamoate and mebendazole. Parasit. Vectors 9, 123 (2016).
Rajagopal, S., Hotez, P. J. & Bundy, D. A. Micronutrient supplementation and deworming in children with geohelminth infections. PLoS Negl. Trop. Dis. 8, e2920 (2014).
Torlesse, H. & Hodges, M. Albendazole therapy and reduced decline in haemoglobin concentration during pregnancy (Sierra Leone). Trans. R. Soc. Trop. Med. Hyg. 95, 195–201 (2001).
Montresor, A. et al. Is the exclusion of children under 24 months from anthelmintic treatment justifiable? Trans. R. Soc. Trop. Med. Hyg. 96, 197–199 (2002).
Truscott, J. E., Turner, H. C. & Anderson, R. M. What impact will the achievement of the current World Health Organisation targets for anthelmintic treatment coverage in children have on the intensity of soil transmitted helminth infections? Parasit. Vectors 8, 551 (2015).
Bundy, D. A., Michael, E. & Guyatt, H. in The Biology of Nematodes (ed. Lee, D. L. ) 599–617 (Taylor and Francis, 2002).
Savioli, L. et al. Schistosomiasis and soil-transmitted helminth infections: forging control efforts. Trans. R. Soc. Trop. Med. Hyg. 96, 577–579 (2002).
Awasthi, S., Pande, V. K. & Fletcher, R. H. Effectiveness and cost-effectiveness of albendazole in improving nutritional status of pre-school children in urban slums. Indian Pediatr. 37, 19–29 (2000).
Taylor-Robinson, D., Jones, A. & Garner, P. Does deworming improve growth and school performance in children? PLoS Negl. Trop. Dis. 3, e358 (2009).
Yap, P. et al. Rapid re-infection with soil-transmitted helminths after triple-dose albendazole treatment of school-aged children in Yunnan, People's Republic of China. Am. J. Trop. Med. Hyg. 89, 23–31 (2013).
Supali, T. et al. Impact of six rounds of mass drug administration on Brugian filariasis and soil-transmitted helminth infections in eastern Indonesia. PLoS Negl. Trop. Dis. 7, e2586 (2013).
Geerts, S., Coles, G. C. & Gryseels, B. Anthelmintic resistance in human helminths: learning from the problems with worm control in livestock. Parasitol. Today 13, 149–151; discussion 156 (1997).
Humphries, D. et al. Epidemiology of hookworm infection in Kintampo North Municipality, Ghana: patterns of malaria coinfection, anemia, and albendazole treatment failure. Am. J. Trop. Med. Hyg. 84, 792–800 (2011).
Stothard, J. R., Rollinson, D., Imison, E. & Khamis, I. S. A spot-check of the efficacies of albendazole or levamisole, against soil-transmitted helminthiases in young Ungujan children, reveals low frequencies of cure. Ann. Trop. Med. Parasitol. 103, 357–360 (2009).
Taylor-Robinson, D. C., Maayan, N., Soares-Weiser, K., Donegan, S. & Garner, P. Deworming drugs for soil-transmitted intestinal worms in children: effects on nutritional indicators, haemoglobin, and school performance. Cochrane Database Syst. Rev. 7, CD000371 (2015).
Adegnika, A. A. et al. Randomized, controlled, assessor-blind clinical trial to assess the efficacy of single- versus repeated-dose albendazole to treat Ascaris lumbricoides. Trichuris trichiura, and hookworm infection. Antimicrob. Agents Chemother. 58, 2535–2540 (2014).
Lenk, E. J., Redekop, W. K., Luyendijk, M., Rijnsburger, A. J. & Severens, J. L. Productivity loss related to neglected tropical diseases eligible for preventive chemotherapy: a systematic literature review. PLoS Negl. Trop. Dis. 10, e0004397 (2016).
Hotez, P. & Whitham, M. Helminth infections: a new global women's health agenda. Obstet. Gynecol. 123, 155–160 (2014).
Stephenson, L. S., Latham, M. C., Adams, E. J., Kinoti, S. N. & Pertet, A. Physical fitness, growth and appetite of Kenyan school boys with hookworm. Trichuris trichiura and Ascaris lumbricoides infections are improved four months after a single dose of albendazole. J. Nutr. 123, 1036–1046 (1993). This study shows that single-dose treatment with albendazole resulted in improved physical fitness, growth and appetite in school-aged children in STH-endemic areas with high hookworm prevalence.
Smillie, W. G. & Augustine, D. L. Hookworm infestation: the effects of varying intensities on the physical condition of school children. Am. J. Dis. Child 31, 151–168 (1926).
Smillie, W. G. & Spencer, C. R. Mental retardation in school children infested with hookworms. J. Educ. Pyschol. 17, 314–321 (1926).
Hurlimann, E. et al. Health-related quality of life among school children with parasitic infections: findings from a national cross-sectional survey in Cote d'Ivoire. PLoS Negl. Trop. Dis. 8, e3287 (2014).
Ziegelbauer, K. et al. Self-rated quality of life and school performance in relation to helminth infections: case study from Yunnan, People's Republic of China. Parasit. Vectors 3, 61 (2010).
Bleakley, H. Disease and development: evidence from hookworm eradication in the American South. Q. J. Econ. 122, 73–117 (2007).
Hotez, P. J. & Ferris, M. T. The antipoverty vaccines. Vaccine 24, 5787–5799 (2006).
Gilgen, D. D., Mascie-Taylor, C. G. & Rosetta, L. L. Intestinal helminth infections, anaemia and labour productivity of female tea pluckers in Bangladesh. Trop. Med. Int. Health 6, 449–457 (2001).
Selvaratnam, R. R., de Silva, L. D., Pathmeswaran, A. & de Silva, N. R. Nutritional status and productivity of Sri Lankan tea pluckers. Ceylon Med. J. 48, 114–118 (2003).
Schuster, A. et al. Life quality impairment caused by hookworm-related cutaneous larva migrans in resource-poor communities in Manaus, Brazil. PLoS Negl. Trop. Dis. 5, e1355 (2011).
Brooker, S. et al. The co-distribution of Plasmodium falciparum and hookworm among African schoolchildren. Malar. J. 5, 99 (2006).
Raso, G. et al. An integrated approach for risk profiling and spatial prediction of Schistosoma mansoni-hookworm coinfection. Proc. Natl Acad. Sci. USA 103, 6934–6939 (2006).
Hotez, P. J. & Molyneux, D. H. Tropical anemia: one of Africa's great killers and a rationale for linking malaria and neglected tropical disease control to achieve a common goal. PLoS Negl. Trop. Dis. 2, e270 (2008).
Hotez, P. J., Bethony, J. M., Oliveira, S. C., Brindley, P. J. & Loukas, A. Multivalent anthelminthic vaccine to prevent hookworm and schistosomiasis. Expert Rev. Vaccines 7, 745–752 (2008).
World Health Organization. Soil-transmitted helminthiasis. Progress report on number of children treated with anthelminthic drugs: an update towards the 2010 global target. Wkly Epidemiol. Rec. 82, 237–252 (2008).
Turner, H. C. et al. An economic evaluation of expanding hookworm control strategies to target the whole community. Parasit. Vectors 8, 570 (2015).
Hotez, P. J., Strych, U., Lustigman, S. & Bottazzi, M. E. Human anthelminthic vaccines: rationale and challenges. Vaccine 34, 3549–3555 (2016).
Hotez, P. J. et al. Advancing a vaccine to prevent hookworm disease and anemia. Vaccine 34, 3001–3005 (2016).
Hotez, P. J., Bethony, J. M., Diemert, D. J., Pearson, M. & Loukas, A. Developing vaccines to combat hookworm infection and intestinal schistosomiasis. Nat. Rev. Microbiol. 8, 814–826 (2010). This article discusses the rationale for the development of vaccines against the two main blood-feeding helminths of humans and proposes antigen ranking criteria for progression to clinical trials.
Loukas, A., Bethony, J., Brooker, S. & Hotez, P. Hookworm vaccines: past, present, and future. Lancet Infect. Dis. 6, 733–741 (2006).
Yazdanbakhsh, M., Kremsner, P. G. & van Ree, R. Allergy, parasites, and the hygiene hypothesis. Science 296, 490–494 (2002).
Rook, G. A. & Brunet, L. R. Old friends for breakfast. Clin. Exp. Allergy 35, 841–842 (2005).
Hamid, F. et al. Risk factors associated with the development of atopic sensitization in Indonesia. PLoS ONE 8, e67064 (2013).
Wiria, A. E. et al. Infection with soil-transmitted helminths is associated with increased insulin sensitivity. PLoS ONE 10, e0127746 (2015).
Prideaux, L., Kamm, M. A., De Cruz, P. P., Chan, F. K. & Ng, S. C. Inflammatory bowel disease in Asia: a systematic review. J. Gastroenterol. Hepatol. 27, 1266–1280 (2012).
Jackson, J. A., Friberg, I. M., Little, S. & Bradley, J. E. Review series on helminths, immune modulation and the hygiene hypothesis: immunity against helminths and immunological phenomena in modern human populations: coevolutionary legacies? Immunology 126, 18–27 (2009).
Briggs, N., Weatherhead, J., Sastry, K. J. & Hotez, P. J. The hygiene hypothesis and its inconvenient truths about helminth infections. PLoS Negl. Trop. Dis. 10, e0004944 (2016).
Helmby, H. Human helminth therapy to treat inflammatory disorders — where do we stand? BMC Immunol. 16, 12 (2015). This comprehensive review considers animal data and clinical trials on the use of human helminths to treat autoimmune and allergic diseases.
Feary, J. R. et al. Experimental hookworm infection: a randomized placebo-controlled trial in asthma. Clin. Exp. Allergy 40, 299–306 (2010).
Giacomin, P. et al. Experimental hookworm infection and escalating gluten challenges are associated with increased microbial richness in celiac subjects. Sci. Rep. 5, 13797 (2015).
Zaiss, M. M. et al. The intestinal microbiota contributes to the ability of helminths to modulate allergic inflammation. Immunity 43, 998–1010 (2015).
Cancado, G. G. et al. Hookworm products ameliorate dextran sodium sulfate-induced colitis in BALB/c mice. Inflamm. Bowel Dis. 17, 2275–2286 (2011).
Ferreira, I. et al. Hookworm excretory/secretory products induce interleukin-4 (IL-4)+ IL-10+ CD4+ T cell responses and suppress pathology in a mouse model of colitis. Infect. Immun. 81, 2104–2111 (2013).
Ruyssers, N. E. et al. Therapeutic potential of helminth soluble proteins in TNBS-induced colitis in mice. Inflamm. Bowel Dis. 15, 491–500 (2009).
Chhabra, S. et al. Kv1.3 channel-blocking immunomodulatory peptides from parasitic worms: implications for autoimmune diseases. FASEB J. 28, 3952–3964 (2014).
Navarro, S. et al. Hookworm recombinant protein promotes regulatory T cell responses that suppress experimental asthma. Sci. Transl Med. 8, 362ra143 (2016). This study shows that recombinant hookworm protein resolved allergic inflammation in mouse models by driving tolerogenic dendritic cells and Treg cell homing to mucosal sites; the protein was bioactive on human cells.
Jiang, N., Moyle, M., Soule, H. R., Rote, W. E. & Chopp, M. Neutrophil inhibitory factor is neuroprotective after focal ischemia in rats. Ann. Neurol. 38, 935–942 (1995).
Lees, K. R., Diener, H. C., Asplund, K., Krams, M. & UK-279,276-301 Study Investigators. UK-279,276, a neutrophil inhibitory glycoprotein, in acute stroke: tolerability and pharmacokinetics. Stroke 34, 1704–1709 (2003).
Ledizet, M., Harrison, L. M., Koskia, R. A. & Cappello, M. Discovery and pre-clinical development of antithrombotics from hematophagous invertebrates. Curr. Med. Chem. Cardiovasc. Hematol. Agents 3, 1–10 (2005).
Cox, F. E. History of human parasitology. Clin. Microbiol. Rev. 15, 595–612 (2002).
Maloy, K. J. & Powrie, F. Intestinal homeostasis and its breakdown in inflammatory bowel disease. Nature 474, 298–306 (2011).
Lee, S. C. et al. Helminth colonization is associated with increased diversity of the gut microbiota. PLoS Negl. Trop. Dis. 8, e2880 (2014).
Cantacessi, C. et al. Impact of experimental hookworm infection on the human gut microbiota. J. Infect. Dis. 210, 1431–1434 (2014).
Cringoli, G. et al. Ancylostoma caninum: calibration and comparison of diagnostic accuracy of flotation in tube, McMaster and FLOTAC in faecal samples of dogs. Exp. Parasitol. 128, 32–37 (2011).
Barda, B. D. et al. Mini-FLOTAC, an innovative direct diagnostic technique for intestinal parasitic infections: experience from the field. PLoS Negl. Trop. Dis. 7, e2344 (2013).
Cringoli, G. FLOTAC, a novel apparatus for a multivalent faecal egg count technique. Parassitologia 48, 381–384 (2006).
Robertson, L. J. et al. Soil-transmitted helminth infections in school children from Cocle Province, Republic of Panama. Parasitology 99, 287–292 (1989).
Levecke, B. et al. A comparison of the sensitivity and fecal egg counts of the McMaster egg counting and Kato–Katz thick smear methods for soil-transmitted helminths. PLoS Negl. Trop. Dis. 5, e1201 (2011).
Pearson, M. S., Ranjit, N. & Loukas, A. Blunting the knife: development of vaccines targeting digestive proteases of blood-feeding helminth parasites. Biol. Chem. 391, 901–911 (2010).
Karmakar, S. et al. Use of an Sm-p80-based therapeutic vaccine to kill established adult schistosome parasites in chronically infected baboons. J. Infect. Dis. 209, 1929–1940 (2014).
Loukas, A. et al. Vaccination with recombinant aspartic hemoglobinase reduces parasite load and blood loss after hookworm infection in dogs. PLoS Med. 2, e295 (2005).
Seid, C. A. et al. Expression, purification, and characterization of the Necator americanus aspartic protease-1 (Na-APR-1 (M74)) antigen, a component of the bivalent human hookworm vaccine. Hum. Vaccin. Immunother. 11, 1474–1488 (2015).
Zhan, B. et al. Molecular cloning, biochemical characterization, and partial protective immunity of the heme-binding glutathione S-transferases from the human hookworm Necator americanus. Infect. Immun. 78, 1552–1563 (2010).
Loukas, A. et al. Vaccinomics for the major blood feeding helminths of humans. OMICS 15, 567–577 (2011).
Author information
Authors and Affiliations
Contributions
Introduction (A.L.); Epidemiology (J.M.B. and P.J.H.); Mechanisms/pathophysiology (A.L., M.Y. and J.C.); Diagnosis, screening and prevention (J.M.B., R.C.-O., P.J.H., J.C., D.D. and J.S.M.); Management (D.D., P.J.H. and J.S.M.); Quality of life (P.J.H.); Outlook (A.L.); Overview of Primer (A.L.).
Corresponding author
Ethics declarations
Competing interests
A.L., P.J.H. and J.M.B. are co-inventors on patents for the use of hookworm proteins as subunit vaccines against human hookworm disease. A.L. is an inventor on patents for the use of hookworm proteins as therapeutics for the treatment of inflammatory diseases and has received funding for such projects from Janssen R&D, USA. All other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Loukas, A., Hotez, P., Diemert, D. et al. Hookworm infection. Nat Rev Dis Primers 2, 16088 (2016). https://doi.org/10.1038/nrdp.2016.88
Published:
DOI: https://doi.org/10.1038/nrdp.2016.88
This article is cited by
-
Development of a hookworm egg hatching assay to determine the ovicidal effects of anthelminthics
Parasites & Vectors (2023)
-
Soil microbiomes and one health
Nature Reviews Microbiology (2023)
-
Chronic Hemorrhagic Anemia Caused by Hookworm Infection: A Case Report
Acta Parasitologica (2023)
-
Metabolomics and lipidomics studies of parasitic helminths: molecular diversity and identification levels achieved by using different characterisation tools
Metabolomics (2023)
-
Application of multiplex amplicon deep-sequencing (MAD-seq) to screen for putative drug resistance markers in the Necator americanus isotype-1 β-tubulin gene
Scientific Reports (2022)