Key Points
-
In 2008, rivaroxaban (Xarelto; Bayer HealthCare) became the first orally administered direct factor Xa inhibitor to be approved for clinical use in the prevention of venous thromboembolism (VTE) after elective hip- or knee-replacement surgery. This article reviews the rationale for its development, the chemical optimization programme that led to its synthesis, its pharmacological characterization and the completed and ongoing clinical studies that underlie its clinical promise.
-
The scientific premise on which a direct factor Xa inhibitor might help to reduce the burden associated with thromboembolic disorders across a range of medical conditions is also presented.
-
Successful early validation studies, conducted with naturally occurring inhibitors of factor Xa, led to the initiation in 1998 of a medicinal chemistry programme to develop oral selective synthetic factor Xa inhibitors. The article details the medicinal chemistry that culminated in the synthesis of rivaroxaban — a molecule that combines both potent, specific inhibition of factor Xa and good oral bioavailability.
-
Rivaroxaban's preclinical profile and subsequent Phase I studies showed that it has many of the characteristics required to address unmet clinical needs: high oral bioavailability, a fast onset/offset of action, dose-dependent pharmacokinetics and pharmacodynamics, few drug–drug or drug–food interactions and, as a result of these, no requirement for routine coagulation monitoring.
-
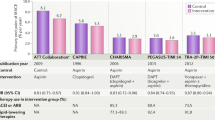
The extensive clinical-development programme, which will enrol over 65,000 patients, is reviewed and covers the four completed studies for VTE prevention after elective hip or knee replacement; the completed and ongoing VTE treatment studies; and the three ongoing studies for stroke prevention in patients with atrial fibrillation, prevention of recurrent events in acute coronary syndromes and VTE prevention in patients with an acute medical illness.
-
In closing, the article provides an overview of other oral anticoagulants in development and discusses their clinical potential with a view to the impact they may have in improving outcomes for patients affected by thromboembolic disorders.
Abstract
The activated serine protease factor Xa is a promising target for new anticoagulants. After studies on naturally occurring factor Xa inhibitors indicated that such agents could be effective and safe, research focused on small-molecule direct inhibitors of factor Xa that might address the major clinical need for improved oral anticoagulants. In 2008, rivaroxaban (Xarelto; Bayer HealthCare) became the first such compound to be approved for clinical use. This article presents the history of rivaroxaban's development, from the structure–activity relationship studies that led to its discovery to the preclinical and clinical studies, and also provides a brief overview of other oral anticoagulants in advanced clinical development.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
McLean, J. The thromboplastic action of cephalin. Am. J. Physiol. 41, 250–257 (1916).
Hirsh, J. et al. Parenteral anticoagulants: American College of Chest Physicians evidence-based clinical practice guidelines (8th Edition). Chest 133, 141S–159S (2008).
Warkentin, T. E., Greinacher, A., Koster, A., Lincoff, A. M. & American College of Chest Physicians. Treatment and prevention of heparin-induced thrombocytopenia: American College of Chest Physicians evidence-based clinical practice guidelines (8th Edition). Chest 133, 340S–380S (2008).
Warwick, D., Dahl, O. E. & Fisher, W. D. Orthopaedic thromboprophylaxis: limitations of current guidelines. J. Bone Joint Surg. Br. 90, 127–132 (2008).
Campbell, H. A. & Link, K. P. Studies on the hemorrhagic sweet clover disease. IV. The isolation and crystallization of the hemorrhagic agent. J. Biol. Chem. 138, 21–33 (1941).
Ansell, J. et al. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians evidence-based clinical practice guidelines (8th Edition). Chest 133, 160S–198S (2008).
Schwarz, U. I. et al. Genetic determinants of response to warfarin during initial anticoagulation. N. Engl. J. Med. 358, 999–1008 (2008).
Klein, T. E. et al. Estimation of the warfarin dose with clinical and pharmacogenetic data. N. Engl. J. Med. 360, 753–764 (2009).
Hirsh, J., O'Donnell, M. & Weitz, J. I. New anticoagulants. Blood 105, 453–463 (2005).
Weitz, J. I. Emerging anticoagulants for the treatment of venous thromboembolism. Thromb. Haemost. 96, 274–284 (2006).
Dyke, C. K. et al. First-in-human experience of an antidote-controlled anticoagulant using RNA aptamer technology: a phase 1a pharmacodynamic evaluation of a drug-antidote pair for the controlled regulation of factor IXa activity. Circulation 114, 2490–2497 (2006).
Eriksson, B. I. et al. Partial factor IXa inhibition with TTP889 for prevention of venous thromboembolism: an exploratory study. J. Thromb. Haemost. 6, 457–463 (2008).
Goto, S. Factor XIa as a possible new target of antithrombotic therapy. J. Thromb. Haemost. 4, 1494–1495 (2006).
Schumacher, W. A. et al. Antithrombotic and hemostatic effects of a small molecule factor XIa inhibitor in rats. Eur. J. Pharmacol. 570, 167–174 (2007).
Ho, S. J. & Brighton, T. A. Ximelagatran: direct thrombin inhibitor. Vasc. Health Risk Manag. 2, 49–58 (2006).
Nishio, H., Ieko, M. & Nakabayashi, T. New therapeutic option for thromboembolism — dabigatran etexilate. Expert Opin. Pharmacother. 9, 2509–2517 (2008).
Turpie, A. G. G., Eriksson, B. I., Lassen, M. R. & Bauer, K. A. Fondaparinux, the first selective factor Xa inhibitor. Curr. Opin. Hematol. 10, 327–332 (2003).
Carreiro, J. & Ansell, J. Apixaban, an oral direct factor Xa inhibitor: awaiting the verdict. Expert Opin. Investig. Drugs 17, 1937–1945 (2008).
Piccini, J. P., Patel, M. R., Mahaffey, K. W., Fox, K. A. & Califf, R. M. Rivaroxaban, an oral direct factor Xa inhibitor. Expert Opin. Investig. Drugs 17, 925–937 (2008).
Leadley, R. J. Coagulation factor Xa inhibition: biological background and rationale. Curr. Top. Med. Chem. 1, 151–159 (2001). This comprehensive review describes some of the key studies that generated interest in factor Xa as a therapeutic target and highlights the significant findings that provided the rationale for the development of direct factor Xa inhibitors.
Kearon, C. et al. Dose-response study of recombinant human soluble thrombomodulin (ART-123) in the prevention of venous thromboembolism after total hip replacement. J. Thromb. Haemost. 3, 962–968 (2005).
Saito, H. et al. Efficacy and safety of recombinant human soluble thrombomodulin (ART-123) in disseminated intravascular coagulation: results of a phase III, randomized, double-blind clinical trial. J. Thromb. Haemost. 5, 31–41 (2007).
Bernard, G. R. et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N. Engl. J. Med. 344, 699–709 (2001).
Levi, M. & van der Poll, T. Recombinant human activated protein C: current insights into its mechanism of action. Crit. Care 11 (Suppl. 5), S3 (2007).
Ansell, J. Factor Xa or thrombin: is factor Xa a better target? J. Thromb. Haemost. 5 (Suppl. 1), 60–64 (2007).
Gerotziafas, G. T. & Samama, M. M. Heterogeneity of synthetic factor Xa inhibitors. Curr. Pharm. Des. 11, 3855–3876 (2005).
Turpie, A. G. G. Oral, direct factor Xa inhibitors in development for the prevention and treatment of thromboembolic diseases. Arterioscler. Thromb. Vasc. Biol. 27, 1238–1247 (2007).
Koller, F. History of factor X. Thromb. Diath. Haemorrh. 4, 58–65 (1960).
Brown, D. L. & Kouides, P. A. Diagnosis and treatment of inherited factor X deficiency. Haemophilia 14, 1176–1182 (2008).
Hougie, C., Barrow, H. M. & Graham, J. B. Stuart clotting defect. I. Segregation of a hereditary hemorrhagic state from the heterozygous heretofore called 'stable factor' (SPCA, proconvertin factor VII deficiency). J. Clin. Invest. 36, 485–493 (1957).
Telfer, T. P., Denson, K. W. & Wright, D. R. A 'new' coagulation defect. Br. J. Haematol. 2, 308–316 (1956).
Butenas, S., van' t Veer, C. & Mann, K. G. “Normal” thrombin generation. Blood 94, 2169–2178 (1999).
Nutt, E. et al. The amino acid sequence of antistasin. A potent inhibitor of factor Xa reveals a repeated internal structure. J. Biol. Chem. 263, 10162–10167 (1988).
Tuszynski, G. P., Gasic, T. B. & Gasic, G. J. Isolation and characterization of antistasin. An inhibitor of metastasis and coagulation. J. Biol. Chem. 262, 9718–9723 (1987).
Dunwiddie, C. et al. Antistasin, a leech-derived inhibitor of factor Xa. Kinetic analysis of enzyme inhibition and identification of the reactive site. J. Biol. Chem. 264, 16694–16699 (1989).
Waxman, L., Smith, D. E., Arcuri, K. E. & Vlasuk, G. P. Tick anticoagulant peptide (TAP) is a novel inhibitor of blood coagulation factor Xa. Science 248, 593–596 (1990).
Nicolini, F. A. et al. Selective inhibition of factor Xa during thrombolytic therapy markedly improves coronary artery patency in a canine model of coronary thrombosis. Blood Coagul. Fibrinolysis 7, 39–48 (1996).
Vlasuk, G. P. et al. Comparison of the in vivo anticoagulant properties of standard heparin and the highly selective factor Xa inhibitors antistasin and tick anticoagulant peptide (TAP) in a rabbit model of venous thrombosis. Thromb. Haemost. 65, 257–262 (1991).
Lynch, J. J. et al. Maintenance of canine coronary artery patency following thrombolysis with front loaded plus low dose maintenance conjunctive therapy. A comparison of factor Xa versus thrombin inhibition. Cardiovasc. Res. 28, 78–85 (1994).
Sitko, G. R. et al. Conjunctive enhancement of enzymatic thrombolysis and prevention of thrombotic reocclusion with the selective factor Xa inhibitor, tick anticoagulant peptide. Comparison to hirudin and heparin in a canine model of acute coronary artery thrombosis. Circulation 85, 805–815 (1992).
Lefkovits, J. et al. Selective inhibition of factor Xa is more efficient than factor VIIa-tissue factor complex blockade at facilitating coronary thrombolysis in the canine model. J. Am. Coll. Cardiol. 28, 1858–1865 (1996).
Eisenberg, P. R., Siegel, J. E., Abendschein, D. R. & Miletich, J. P. Importance of factor Xa in determining the procoagulant activity of whole-blood clots. J. Clin. Invest. 91, 1877–1883 (1993).
Prager, N. A., Abendschein, D. R., McKenzie, C. R. & Eisenberg, P. R. Role of thrombin compared with factor Xa in the procoagulant activity of whole blood clots. Circulation 92, 962–967 (1995).
McKenzie, C. R., Abendschein, D. R. & Eisenberg, P. R. Sustained inhibition of whole-blood clot procoagulant activity by inhibition of thrombus-associated factor Xa. Arterioscler. Thromb. Vasc. Biol. 16, 1285–1291 (1996).
Kotze, H. F., Lamprecht, S., Badenhorst, P. N., Roodt, J. P. & van Wyk, V. Transient interruption of arterial thrombosis by inhibition of factor Xa results in long-term antithrombotic effects in baboons. Thromb. Haemost. 77, 1137–1142 (1997).
Gold, H. K. et al. Evidence for a rebound coagulation phenomenon after cessation of a 4-hour infusion of a specific thrombin inhibitor in patients with unstable angina pectoris. J. Am. Coll. Cardiol. 21, 1039–1047 (1993).
Theroux, P., Waters, D., Lam, J., Juneau, M. & McCans, J. Reactivation of unstable angina after the discontinuation of heparin. N. Engl. J. Med. 327, 141–145 (1992).
Hermans, C. & Claeys, D. Review of the rebound phenomenon in new anticoagulant treatments. Curr. Med. Res. Opin. 22, 471–481 (2006).
Furugohri, T. et al. Different antithrombotic properties of factor Xa inhibitor and thrombin inhibitor in rat thrombosis models. Eur. J. Pharmacol. 514, 35–42 (2005).
Becker, R. C., Alexander, J., Dyke, C. K. & Harrington, R. A. Development of DX-9065a, a novel direct factor Xa antagonist, in cardiovascular disease. Thromb. Haemost. 92, 1182–1193 (2004).
Sato, K. et al. YM-60828, a novel factor Xa inhibitor: separation of its antithrombotic effects from its prolongation of bleeding time. Eur. J. Pharmacol. 339, 141–146 (1997).
Taniuchi, Y. et al. Biochemical and pharmacological characterization of YM-60828, a newly synthesized and orally active inhibitor of human factor Xa. Thromb. Haemost. 79, 543–548 (1998).
Hara, T. et al. DX-9065a, a new synthetic, potent anticoagulant and selective inhibitor for factor Xa. Thromb. Haemost. 71, 314–319 (1994).
Fujii, Y. et al. Characteristics of gastrointestinal absorption of DX-9065a, a new synthetic anticoagulant. Drug Metab. Pharmacokinet. 22, 26–32 (2007).
Alexander, J. H. et al. First experience with direct, selective factor Xa inhibition in patients with non-ST-elevation acute coronary syndromes: results of the XaNADU-ACS Trial. J. Thromb. Haemost. 3, 439–447 (2005).
Bauer, K. A. et al. Fondaparinux, a synthetic pentasaccharide: the first in a new class of antithrombotic agents — the selective factor Xa inhibitors. Cardiovasc. Drug Rev. 20, 37–52 (2002).
Bergqvist, D. Review of fondaparinux sodium injection for the prevention of venous thromboembolism in patients undergoing surgery. Vasc. Health Risk Manag. 2, 365–370 (2006).
Eriksson, B. I., Bauer, K. A., Lassen, M. R., Turpie, A. G. G. Steering Committee of the Pentasaccharide in Hip-Fracture Surgery Study. Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after hip-fracture surgery. N. Engl. J. Med. 345, 1298–1304 (2001).
Lassen, M. R., Bauer, K. A., Eriksson, B. I. & Turpie, A. G. G. Postoperative fondaparinux versus preoperative enoxaparin for prevention of venous thromboembolism in elective hip-replacement surgery: a randomised double-blind comparison. Lancet 359, 1715–1720 (2002).
Turpie, A. G. G., Bauer, K. A., Eriksson, B. I., Lassen, M. R. PENTATHLON 2000 Study Steering Committee. Postoperative fondaparinux versus postoperative enoxaparin for prevention of venous thromboembolism after elective hip-replacement surgery: a randomised double-blind trial. Lancet 359, 1721–1726 (2002).
Bauer, K. A., Eriksson, B. I., Lassen, M. R. & Turpie, A. G. G. Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after elective major knee surgery. N. Engl. J. Med. 345, 1305–1310 (2001).
Turpie, A. G. G., Bauer, K. A., Eriksson, B. I., Lassen, M. R. Steering Committees of the Pentasaccharide Orthopedic Prophylaxis Studies. Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major orthopedic surgery: a meta-analysis of 4 randomized double-blind studies. Arch. Intern. Med. 162, 1833–1840 (2002).
Roehrig, S. et al. Discovery of the novel antithrombotic agent 5-chloro-N-([(5S)-2-oxo-3-[4-(3-oxomorpholin-4-yl)phenyl]-1,3-oxazolidin-5-yl]methyl)thiophene-2-carboxamide (BAY 59-7939): an oral, direct factor Xa inhibitor. J. Med. Chem. 48, 5900–5908 (2005). Describes the chemical development of rivaroxaban, including the important structure–activity relationship that led to the combination of high binding affinity with high oral bioavailability.
Lam, P. Y. et al. Structure-based design of novel guanidine/benzamidine mimics: potent and orally bioavailable factor Xa inhibitors as novel anticoagulants. J. Med. Chem. 46, 4405–4418 (2003).
Pinto, D. J. et al. Discovery of 1-[3-(aminomethyl)phenyl]-N-3-fluoro-2-(methylsulfonyl)-[1,1-biphenyl]-4-yl]-3-(trifluoromethyl)-1H-pyrazole-5-carboxamide (DPC423), a highly potent, selective, and orally bioavailable inhibitor of blood coagulation factor Xa. J. Med. Chem. 44, 566–578 (2001).
Adler, M. et al. Crystal structures of two potent nonamidine inhibitors bound to factor Xa. Biochem. Mosc. 41, 15514–15523 (2002).
Choi-Sledeski, Y. M. et al. Discovery of an orally efficacious inhibitor of coagulation factor Xa which incorporates a neutral P1 ligand. J. Med. Chem. 46, 681–684 (2003).
Maignan, S. et al. Molecular structures of human factor Xa complexed with ketopiperazine inhibitors: preference for a neutral group in the S1 pocket. J. Med. Chem. 46, 685–690 (2003).
Mederski, W. W. et al. Chlorothiophenecarboxamides as P1 surrogates of inhibitors of blood coagulation factor Xa. Bioorg. Med. Chem. Lett. 14, 5817–5822 (2004).
Nazare, M. et al. Probing the subpockets of factor Xa reveals two binding modes for inhibitors based on a 2-carboxyindole scaffold: a study combining structure–activity relationship and X-ray crystallography. J. Med. Chem. 48, 4511–4525 (2005).
Perzborn, E. et al. In vitro and in vivo studies of the novel antithrombotic agent BAY 59-7939 — an oral, direct factor Xa inhibitor. J. Thromb. Haemost. 3, 514–521 (2005). This paper reports the in vitro properties of rivaroxaban, its antithrombotic efficacy in animal models of arterial and venous thrombosis and its effect on haemostasis — the key findings that established the rationale for its clinical development.
Depasse, F. et al. Effect of BAY 59-7939 — a novel, oral, direct factor Xa inhibitor — on clot-bound factor Xa activity in vitro. J. Thromb. Haemost. Abstr. 3 (Suppl. 1), P1104 (2005).
Gerotziafas, G. T., Elalamy, I., Depasse, F., Perzborn, E. & Samama, M. M. In vitro inhibition of thrombin generation, after tissue factor pathway activation, by the oral, direct factor Xa inhibitor rivaroxaban. J. Thromb. Haemost. 5, 886–888 (2007).
Graff, J. et al. Effects of the oral, direct factor Xa inhibitor rivaroxaban on platelet-induced thrombin generation and prothrombinase activity. J. Clin. Pharmacol. 47, 1398–1407 (2007).
Perzborn, E. & Harwardt, M. Direct thrombin inhibitors, but not factor Xa inhibitors, enhance thrombin formation in human plasma by interfering with the thrombin-thrombomodulin-protein C system. Blood (ASH Annual Meeting Abstracts) 112, 198–199 (2008).
Perzborn, E. et al. Biochemical and pharmacologic properties of BAY 59–7939, an oral, direct factor Xa inhibitor. Pathophysiol. Haemost. Thromb. 33 (Suppl. 2), PO079 (2004).
Perzborn, E. & Lange, U. Rivaroxaban — an oral, direct factor Xa inhibitor — inhibits tissue factor-mediated platelet aggregation. J. Thromb. Haemost. 5 (Suppl. 2), P-W-642 (2007).
Furugohri, T. et al. DU-176b, a potent and orally active factor Xa inhibitor: in vitro and in vivo pharmacological profiles. J. Thromb. Haemost. 6, 1542–1549 (2008).
Shantsila, E. & Lip, G. Y. Apixaban, an oral, direct inhibitor of activated factor Xa. Curr. Opin. Investig. Drugs 9, 1020–1033 (2008).
Biemond, B. J. et al. Prevention and treatment of experimental thrombosis in rabbits with rivaroxaban (BAY 59-7939) — an oral, direct factor Xa inhibitor. Thromb. Haemost. 97, 471–477 (2007).
Kubitza, D., Becka, M., Roth, A. & Mueck, W. Dose-escalation study of the pharmacokinetics and pharmacodynamics of rivaroxaban in healthy elderly subjects. Curr. Med. Res. Opin. 24, 2757–2765 (2008).
Kubitza, D., Becka, M., Wensing, G., Voith, B. & Zuehlsdorf, M. Safety, pharmacodynamics, and pharmacokinetics of BAY 59-7939 — an oral, direct factor Xa inhibitor — after multiple dosing in healthy male subjects. Eur. J. Clin. Pharmacol. 61, 873–880 (2005). This Phase I study reported the safety, tolerability, pharmacodynamics and pharmacokinetics of rivaroxaban when administered as multiple doses to healthy male subjects. The favourable results of this study, and others, supported the progression to Phase II clinical trials.
Gruber, A., Marzec, U. M., Buetehorn, U., Hanson, S. & Perzborn, E. Potential of activated prothrombin complex concentrate and activated factor VII to reverse the anticoagulant effects of rivaroxaban in primates. Blood (ASH Annual Meeting Abstracts) 112, 1307 (2008).
Perzborn, E., Trabandt, A., Selbach, K. & Tinel, H. Prothrombin complex concentrate reverses the effects of high-dose rivaroxaban in rats. J. Thromb. Haemost. 7 (Suppl. 2), 379 (2009).
Kubitza, D., Becka, M., Voith, B., Zuehlsdorf, M. & Wensing, G. Safety, pharmacodynamics, and pharmacokinetics of single doses of BAY 59-7939, an oral, direct factor Xa inhibitor. Clin. Pharmacol. Ther. 78, 412–421 (2005).
Zhang, L., Reynolds, K. S., Zhao, P. & Huang, S. M. Drug interactions evaluation: an integrated part of risk assessment of therapeutics. Toxicol. Appl. Pharmacol. 243, 134–145 (2010).
Zhang, L., Zhang, Y. D., Strong, J. M., Reynolds, K. S. & Huang, S. M. A regulatory viewpoint on transporter-based drug interactions. Xenobiotica 38, 709–724 (2008).
Kubitza, D., Becka, M., Mueck, W. & Zuehlsdorf, M. Rivaroxaban (BAY 59-7939) — an oral, direct factor Xa inhibitor — has no clinically relevant interaction with naproxen. Br. J. Clin. Pharmacol. 63, 469–476 (2007).
Kubitza, D., Becka, M., Mueck, W. & Zuehlsdorf, M. Safety, tolerability, pharmacodynamics, and pharmacokinetics of rivaroxaban — an oral, direct factor Xa inhibitor — are not affected by aspirin. J. Clin. Pharmacol. 46, 981–990 (2006).
Eriksson, B. I. et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N. Engl. J. Med. 358, 2765–2775 (2008).
Kakkar, A. K. et al. Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: a double-blind, randomised controlled trial. Lancet 372, 31–39 (2008).
Lassen, M. R. et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty. N. Engl. J. Med. 358, 2776–2786 (2008).
Turpie, A. G. G. et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty (RECORD4): a randomised trial. Lancet 373, 1673–1680 (2009).
Weinz, C. et al. Pharmacokinetics of BAY 59-7939 — an oral, direct factor Xa inhibitor — in rats and dogs. Xenobiotica 35, 891–910 (2005). This preclinical study established some of the key pharmacokinetic characteristics of rivaroxaban, including a fully reversible, high level of plasma protein binding, a dual mode of excretion and moderate tissue affinity.
Lang, D., Freudenberger, C. & Weinz, C. In vitro metabolism of rivaroxaban — an oral, direct factor Xa inhibitor — in liver microsomes and hepatocytes of rat, dog and man. Drug Metab. Dispos. 37, 1046–1055 (2009).
Weinz, C., Schwarz, T., Kubitza, D., Mueck, W. & Lang, D. Metabolism and excretion of rivaroxaban, an oral, direct factor Xa inhibitor, in rats, dogs and humans. Drug Metab. Dispos. 37, 1056–1064 (2009).
Mueck, W. et al. Population pharmacokinetics and pharmacodynamics of rivaroxaban — an oral, direct factor Xa inhibitor — in patients undergoing major orthopaedic surgery. Clin. Pharmacokinet. 47, 203–216 (2008). The results showed that rivaroxaban has predictable, dose-dependent pharmacokinetics and pharmacodynamics and indicated that rivaroxaban could be administered in fixed doses without routine coagulation monitoring.
Mueck, W., Becka, M., Kubitza, D., Voith, B. & Zuehlsdorf, M. Population model of the pharmacokinetics and pharmacodynamics of rivaroxaban — an oral, direct factor Xa inhibitor — in healthy subjects. Int. J. Clin. Pharmacol. Ther. 45, 335–344 (2007).
Kubitza, D., Becka, M., Zuehlsdorf, M. & Mueck, W. Body weight has limited influence on the safety, tolerability, pharmacokinetics, or pharmacodynamics of rivaroxaban (BAY 59-7939) in healthy subjects. J. Clin. Pharmacol. 47, 218–226 (2007).
Kubitza, D. et al. Effects of renal impairment on the pharmacokinetics, pharmacodynamics and safety of rivaroxaban — an oral, direct factor Xa inhibitor. Br. J. Clin. Pharmacol. 70, 703–712 (2010).
Halabi, A. et al. Effect of hepatic impairment on the pharmacokinetics, pharmacodynamics and tolerability of rivaroxaban — an oral, direct factor Xa inhibitor. J. Thromb. Haemost. 5 (Suppl. 2), P-M-635 (2007).
Eriksson, B. I. et al. Dose-escalation study of rivaroxaban (BAY 59-7939) — an oral, direct factor Xa inhibitor — for the prevention of venous thromboembolism in patients undergoing total hip replacement. Thromb. Res. 120, 685–693 (2007).
Eriksson, B. I. et al. A once-daily, oral, direct factor Xa inhibitor, rivaroxaban (BAY 59-7939), for thromboprophylaxis after total hip replacement. Circulation 114, 2374–2381 (2006). The results from this study, and others, led to the selection of 10 mg rivaroxaban once daily for use in Phase III studies for the prevention of venous thromboembolism after hip or knee replacement.
Eriksson, B. I. et al. Oral, direct factor Xa inhibition with BAY 59-7939 for the prevention of venous thromboembolism after total hip replacement. J. Thromb. Haemost. 4, 121–128 (2006).
Turpie, A. G. G. et al. BAY 59-7939: an oral, direct factor Xa inhibitor for the prevention of venous thromboembolism in patients after total knee replacement. A phase II dose-ranging study. J. Thromb. Haemost. 3, 2479–2486 (2005).
Kubitza, D., Mueck, W. & Becka, M. Randomized, double-blind, crossover study to investigate the effect of rivaroxaban on QT-interval prolongation. Drug Saf. 31, 67–77 (2008).
Samama, M. M. et al. Suitability of chromogenic anti-FXa methods to measure rivaroxaban in human plasma. J. Thromb. Haemost. 7 (Suppl. 2), 693 (2009).
Karst, A., Bakowski-Enzian, B. & Perzborn, E. Monitoring of rivaroxaban: suitability of a well-established chromogenic anti-factor Xa assay. J. Thromb. Haemost. 7 (Suppl. 2), 372 (2009).
Fisher, W. D. et al. Rivaroxaban for thromboprophylaxis after orthopaedic surgery: pooled analysis of two studies. Thromb. Haemost. 97, 931–937 (2007).
Geerts, W. H. et al. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th Edition). Chest 133, 381S–453S (2008).
Lassen, M. R. et al. Apixaban or enoxaparin for thromboprophylaxis after knee replacement. N. Engl. J. Med. 361, 594–604 (2009).
The RE-MOBILIZE Writing Committee. Oral thrombin inhibitor dabigatran etexilate vs North American enoxaparin regimen for prevention of venous thromboembolism after knee arthroplasty surgery. J. Arthroplasty 24, 1–9 (2009).
Eriksson, B. I. et al. Oral rivaroxaban for the prevention of symptomatic venous thromboembolism after elective hip and knee replacement. J. Bone Joint Surg. Br. 91, 636–644 (2009). A pooled analysis of data from the pivotal Phase III clinical trials that, together with other publications, demonstrated the clinical efficacy and safety of rivaroxaban for thromboprophylaxis after total knee- or hip-replacement surgery.
Mega, J. L. et al. Rivaroxaban versus placebo in patients with acute coronary syndromes (ATLAS ACS-TIMI 46): a randomised, double-blind, phase II trial. Lancet 374, 29–38 (2009). A Phase II dose-ranging study investigating the use of rivaroxaban for the secondary prevention of ischaemic events in patients with ACS receiving aspirin with or without a thienopyridine.
Bauer, K. A., Homering, M. & Berkowitz, S. D. Effects of age, weight, gender and renal function in a pooled analysis of four phase III studies of rivaroxaban for prevention of venous thromboembolism after major orthopedic surgery. Blood (ASH Annual Meeting Abstracts) 112, 166–167 (2008).
Agnelli, G. et al. Treatment of proximal deep-vein thrombosis with the oral direct factor Xa inhibitor rivaroxaban (BAY 59-7939): the ODIXa-DVT (oral direct factor Xa inhibitor BAY 59–7939 in patients with acute symptomatic deep-vein thrombosis) study. Circulation 116, 180–187 (2007).
Buller, H. R. et al. A dose-ranging study evaluating once-daily oral administration of the factor Xa inhibitor rivaroxaban in the treatment of patients with acute symptomatic deep vein thrombosis. The EINSTEIN-DVT Dose-Ranging Study. Blood 112, 2242–2247 (2008). This Phase II study, with one other, provided the basis for the dosing strategy in the Phase III VTE treatment trials and the dose selection for the Phase III ROCKET AF trial.
Buller, H.R. Oral rivaroxaban for the acute and continued treatment of symptomatic venous thromboembolism. The Einstein-DVT and Einstein-Extension Study (Abstract 187). ASH Annual Meeting Abstracts [online], (2010).
The EINSTEIN Investigators. Oral rivaroxaban for symptomatic venous thromboembolism. New Engl. J. Med. 4 Dec 2010 (doi:10.1056/NEJMoa1007903).
ROCKET AF Study Investigators. Rivaroxaban — once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation: rationale and design of the ROCKET AF study. Am. Heart J. 159, 340–347 (2010).
Wong, P. C. et al. Apixaban, an oral, direct and highly selective factor Xa inhibitor: in vitro, antithrombotic and antihemostatic studies. J. Thromb. Haemost. 6, 820–829 (2008).
Luettgen, J. M. et al. Inhibition of measured thrombin generation in human plasma by apixaban: a predictive mathematical model based on experimentally determined rate constants. J. Thromb. Haemost. 5 (Suppl. 1), P-T-633 (2007).
Lassen, M. R. et al. Apixaban versus enoxaparin for thromboprophylaxis after knee replacement (ADVANCE-2): a randomised double-blind trial. Lancet 375, 807–815 (2010).
Lassen, M. R. et al. Randomized double-blind comparison of apixaban and enoxaparin for thromboprophylaxis after hip replacement: the ADVANCE-3 trial. Pathophysiol. Haemost. Thromb. 37, A20 (2010).
Alexander, J. H. et al. Apixaban, an oral, direct, selective factor Xa inhibitor, in combination with antiplatelet therapy after acute coronary syndrome: results of the Apixaban for Prevention of Acute Ischemic and Safety Events (APPRAISE) trial. Circulation 119, 2877–2885 (2009).
Eikelboom, J. W. et al. Rationale and design of AVERROES: apixaban versus acetylsalicylic acid to prevent stroke in atrial fibrillation patients who have failed or are unsuitable for vitamin K antagonist treatment. Am. Heart J. 159, 348–353 (2010).
Lopes, R. D. et al. Apixaban for Reduction In Stroke and Other ThromboemboLic Events in Atrial Fibrillation (ARISTOTLE) trial: design and rationale. Am. Heart J. 159, 331–339 (2010).
Connolly, S. J. & Arnesen, H. AVERROES: apixaban versus acetylsalicylic acid to prevent strokes. European Society of Cardiology website [online] (2010).
Zafar, M. U. et al. Antithrombotic effects of factor Xa inhibition with DU-176b: phase-I study of an oral, direct factor Xa inhibitor using an ex-vivo flow chamber. Thromb. Haemost. 98, 883–888 (2007).
Fuji, T., Fujita, S., Tachibana, S. & Kawai, Y. A dose-ranging study evaluating the oral factor Xa inhibitor edoxaban for the prevention of venous thromboembolism in patients undergoing total knee arthroplasty. J. Thromb. Haemost. 8, 2458–2468 (2010).
Raskob, G. et al. Oral direct factor Xa inhibition with edoxaban for thromboprophylaxis after elective total hip replacement. A randomised double-blind dose-response study. Thromb. Haemost. 104, 642–649 (2010).
Weitz, J. I. et al. Randomised, parallel-group, multicentre, multinational phase 2 study comparing edoxaban, an oral factor Xa inhibitor, with warfarin for stroke prevention in patients with atrial fibrillation. Thromb. Haemost. 104, 633–641 (2010).
Iwatsuki, Y. et al. Biochemical and pharmacological profiles of YM150, an oral direct factor Xa inhibitor. Blood (ASH Annual Meeting Abstracts) 108, 273a (2006).
Eriksson, B. I. et al. Prevention of venous thromboembolism with an oral factor Xa inhibitor, YM150, after total hip arthroplasty. A dose finding study (ONYX-2). J. Thromb. Haemost. 8, 714–721 (2010).
Sabatine, M. S. et al. Otamixaban for the treatment of patients with non-ST-elevation acute coronary syndromes (SEPIA-ACS1 TIMI 42): a randomised, double-blind, active-controlled, phase 2 trial. Lancet 374, 787–795 (2009).
Cohen, M. et al. Randomized, double-blind, dose-ranging study of otamixaban, a novel, parenteral, short-acting direct factor Xa inhibitor, in percutaneous coronary intervention: the SEPIA-PCI trial. Circulation 115, 2642–2651 (2007).
Harenberg, J. Development of idraparinux and idrabiotaparinux for anticoagulant therapy. Thromb. Haemost. 102, 811–815 (2009).
Veyrat-Follet, C., Vivier, N., Trellu, M., Dubruc, C. & Sanderink, G. J. The pharmacokinetics of idraparinux, a long-acting indirect factor Xa inhibitor: population pharmacokinetic analysis from Phase III clinical trials. J. Thromb. Haemost. 7, 559–565 (2009).
Amadeus Investigators et al. Comparison of idraparinux with vitamin K antagonists for prevention of thromboembolism in patients with atrial fibrillation: a randomised, open-label, non-inferiority trial. Lancet 371, 315–321 (2008).
van Gogh Investigators et al. Idraparinux versus standard therapy for venous thromboembolic disease. N. Engl. J. Med. 357, 1094–1104 (2007).
Connolly, S. J. et al. Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 361, 1139–1151 (2009).
Eriksson, B. I. et al. Dabigatran etexilate versus enoxaparin for prevention of venous thromboembolism after total hip replacement: a randomised, double-blind, non-inferiority trial. Lancet 370, 949–956 (2007).
Eriksson, B. I. et al. Oral dabigatran etexilate vs. subcutaneous enoxaparin for the prevention of venous thromboembolism after total knee replacement: the RE-MODEL randomized trial. J. Thromb. Haemost. 5, 2178–2185 (2007).
Schulman, S. et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N. Engl. J. Med. 361, 2342–2352 (2009).
Squizzato, A., Dentali, F., Steidl, L. & Ageno, W. New direct thrombin inhibitors. Intern. Emerg. Med. 4, 479–484 (2009).
Straub, A. et al. Substituted oxazolidinones and their use in the field of blood coagulation. WO0147919 (A1) (2001).
Mederski, W. W. et al. Halothiophene benzimidazoles as P1 surrogates of inhibitors of blood coagulation factor Xa. Bioorg. Med. Chem. Lett. 14, 3763–3769 (2004).
Pinto, D. J. et al. Discovery of 1-(4-methoxyphenyl)-7-oxo-6-(4-(2-oxopiperidin-1-yl)phenyl)-4,5,6,7-tetrahydro-1H-pyrazolo[3,4-c]pyridine-3-carboxamide (Apixaban, BMS-562247), a highly potent, selective, efficacious, and orally bioavailable inhibitor of blood coagulation factor Xa. J. Med. Chem. 50, 5339–5356 (2007).
Kohrt, J. T. et al. The discovery of (2R,4R)-N-(4-chlorophenyl)-N-(2-fluoro-4-(2-oxopyridin-1(2H)-yl)phenyl)-4-methoxypyrrolidine-1,2-dicarboxamide (PD 0348292), an orally efficacious factor Xa inhibitor. Chem. Biol. Drug Des. 70, 100–112 (2007).
Mann, K. G., Butenas, S. & Brummel, K. The dynamics of thrombin formation. Arterioscler. Thromb. Vasc. Biol. 23, 17–25 (2003).
Furie, B. & Furie, B. C. Mechanisms of thrombus formation. N. Engl. J. Med. 359, 938–949 (2008).
Mann, K. G., Jenny, R. J. & Krishnaswamy, S. Cofactor proteins in the assembly and expression of blood clotting enzyme complexes. Annu. Rev. Biochem. 57, 915–956 (1988).
Licari, L. G. & Kovacic, J. P. Thrombin physiology and pathophysiology. J. Vet. Emerg. Crit. Care (San Antonio) 19, 11–22 (2009).
Mann, K. G., Brummel, K. & Butenas, S. What is all that thrombin for? J. Thromb. Haemost. 1, 1504–1514 (2003).
Kaiser, B. Factor Xa-a promising target for drug development. Cell. Mol. Life Sci. 59, 189–192 (2002).
Wienen, W., Stassen, J. M., Priepke, H., Ries, U. J. & Hauel, N. In-vitro profile and ex-vivo anticoagulant activity of the direct thrombin inhibitor dabigatran and its orally active prodrug, dabigatran etexilate. Thromb. Haemost. 98, 155–162 (2007).
Kakkar, A. K. et al. Extended thromboprophylaxis with rivaroxaban compared with short-term thromboprophylaxis with enoxaparin after total hip arthroplasty: the RECORD2 trial. Blood (ASH Annual Meeting Abstracts) 110, 307 (2007).
Acknowledgements
The authors would like to acknowledge S. Salaria and S. McMillan, who provided medical writing services, with funding from Bayer HealthCare and Johnson & Johnson Pharmaceutical Research & Development. We would also like to thank Proteros Biostructures, Planegg-Martinsried, Germany, for performing the X-ray crystal structure work on rivaroxaban.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
E.P., S.R., A.S., D.K. and F.M. are employed at Bayer HealthCare. E.P., S.R., A.S. and F.M. are shareholders.
Related links
Related links
FURTHER INFORMATION
Bayer HealthCare Xarelto (rivaroxaban) Summary of Product Characteristics
GlaxoSmithKline, Arixtra (fondaparinux) prescribing information
Janssen Pharmaceutica Products, Nizoral (ketoconazole) tablets prescribing information
Abbott Laboratories, Norvir (ritonavir) prescribing information
Glossary
- Thromboembolic disorders
-
A group of conditions characterized by an increased incidence of thrombi in the vasculature, such as deep-vein thrombosis, pulmonary embolism, systemic embolism or coronary and cerebral ischaemia.
- Unfractionated heparin
-
(UFH). An anticoagulant administered intravenously or subcutaneously. It binds to antithrombin, greatly increasing its activity and resulting in the inhibition of factors Xa, IXa, XIa, XIIa and thrombin (factor IIa).
- Heparin-induced thrombocytopaenia
-
The process by which antibodies against the complex of heparin and platelet factor 4 activate platelets, resulting in a decrease in platelet numbers of more than 50%.
- Low-molecular-weight heparins
-
(LMWHs). A class of anticoagulants derived from unfractionated heparin by chemical or enzymatic degradation. They induce a conformational change in antithrombin that greatly increases its anticoagulant activity.
- Thrombin
-
Thrombin (also known as factor IIa) is the terminal enzyme of the coagulation cascade and converts fibrinogen into fibrin, which forms clot fibres. Thrombin also activates several other coagulation factors, as well as protein C.
- Antithrombin
-
An endogenous glycoprotein that binds covalently to thrombin and other coagulation factors, resulting in their inhibition. Antithrombin functions as a natural anticoagulant, and its inhibitory action is accelerated by heparin.
- Warfarin
-
A vitamin K antagonist that is currently the most commonly used oral anticoagulant.
- Vitamin K antagonist
-
A class of compounds that inhibit the vitamin K-dependent carboxylation of specific coagulation factors, resulting in decreased levels of the affected coagulation factors, leading to anticoagulation.
- Therapeutic window
-
The interval between the lowest dose of a drug that is sufficient for clinical effectiveness and a higher dose at which adverse events or toxicity become unacceptable.
- International normalized ratio
-
(INR). Because prothrombin time-test results vary according to the activity of the thromboplastin used, the INR conversion is used to normalize results for any thromboplastin preparation. It is valid only with vitamin K antagonists.
- Thromboprophylaxis
-
A measure taken to prevent the development of a thrombus. It can be pharmaceutical or mechanical.
- Tissue factor
-
A cell-membrane-bound receptor protein that is exposed to the circulating blood during vessel injury. Pre-existing factor VIIa in the blood binds to tissue factor, initiating the coagulation cascade.
- Direct thrombin inhibitors
-
A class of anticoagulants that bind directly to thrombin and block the interaction with its substrate, fibrinogen, thereby inhibiting the generation of fibrin and clot formation.
- Thrombomodulin
-
A membrane-bound thrombin receptor that, when bound to thrombin, functions as a cofactor in the thrombin-induced activation of protein C.
- Protein C
-
The inactive precursor of activated protein C (APC). APC, with its cofactor protein S, inactivates factor Va and factor VIIIa, thus providing an important anticoagulant feedback function.
- Factor Xa inhibitor
-
A class of anticoagulants that inhibit factor Xa in the coagulation cascade, either by binding directly, or indirectly through antithrombin. Inhibition of factor Xa reduces the production of thrombin.
- Venous thromboembolism
-
(VTE). A condition in which a blood clot (thrombus) that has formed in the venous system breaks free (becoming an embolus) and migrates through the circulation to lodge in and block another blood vessel.
- Deep-vein thrombosis
-
(DVT). A blood clot in a deep vein, usually in the leg. Distal DVT occurs in the calf, whereas proximal DVT occurs above the knee.
- Pulmonary embolism
-
A blood clot or thromboembolus in a pulmonary blood vessel. Such emboli generally originate from a deep-vein thrombosis and can cause permanent lung damage, chronic pulmonary hypertension and death.
- Haemostasis
-
The complex process that leads to the formation of a blood clot, causing bleeding to stop.
- Fibrinogen
-
A soluble plasma protein that, in the final phase of the coagulation process, is converted to fibrin by thrombin. Fibrin then polymerizes and forms the fibrous network base of a clot.
- Oral bioavailability
-
The total proportion of pharmacologically active drug that enters the systemic circulation after oral administration. It is affected by both absorption and local metabolic inactivation.
- Prothrombin time
-
A laboratory test that measures clotting time in the presence of tissue factor (thromboplastin). It is used to assess the activity of the extrinsic coagulation pathway.
- Activated partial thromboplastin time
-
A laboratory test that measures the clotting time of plasma after contact activation. It assesses the function of the intrinsic coagulation pathway.
- CYP450 isoforms
-
Many therapeutic drugs are metabolized by cytochrome P450 (CYP450) enzymes, a 'superfamily' of related but distinct enzymes that differ in their substrate specificity.
- Creatinine clearance
-
The rate at which the kidney clears the blood of creatinine (a waste product from muscles that is excreted at a fairly constant rate). Creatinine clearance is used as an approximation of the glomerular filtration rate.
- Chromogenic assay
-
An enzymatic assay in which a colour develops during the course of the reaction, which can then be measured spectrophotometrically. Colour development is reduced in the presence of an inhibitor.
- Venography
-
Radiography of the veins after intravenous injection of a radioactive isotope or contrast dye. This can be used to confirm the presence of deep-vein thromboses.
- Index event
-
The acute event that leads to a patient's initial presentation. The term can also refer to the initial event resulting in a patient's inclusion in a follow-up study, such as a survey of recurrent strokes.
Rights and permissions
About this article
Cite this article
Perzborn, E., Roehrig, S., Straub, A. et al. The discovery and development of rivaroxaban, an oral, direct factor Xa inhibitor. Nat Rev Drug Discov 10, 61–75 (2011). https://doi.org/10.1038/nrd3185
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrd3185
This article is cited by
-
Anticoagulant activity screening of an in-house database of natural compounds for discovering novel selective factor Xa inhibitors; a combined in silico and in vitro approach
Medicinal Chemistry Research (2020)
-
Simultaneous Determination of Rivaroxaban and Enalapril in Rat Plasma by UPLC–MS/MS and Its Application to A Pharmacokinetic Interaction Study
European Journal of Drug Metabolism and Pharmacokinetics (2019)
-
Use of rivaroxaban in patients with stroke
Neurological Sciences (2017)
-
Drug Interactions of Direct-Acting Oral Anticoagulants
Drug Safety (2016)
-
Risk–Benefit Profile of Direct-Acting Oral Anticoagulants in Established Therapeutic Indications: An Overview of Systematic Reviews and Observational Studies
Drug Safety (2016)