Abstract
In the 1990s, the breast cancer drug trastuzumab (Herceptin; Genentech/Roche) — an antibody specific for human epidermal growth factor receptor 2 (HER2; also known as ERBB2) — was approved based on trials in which HER2 expression levels were used to select patients in clinical trials. This provided support for analogous efforts for drugs that target the epidermal growth factor receptor (EGFR). However, the development of these drugs, such as cetuximab (Erbitux; Bristol–Myers Squibb/Lilly) and gefitinib (Iressa; AstraZeneca), has revealed that EGFR expression is an insufficient and unreliable biomarker to select patients for EGFR-targeted therapies in both lung and colon cancer. Indeed, evidence on patient populations that are likely to respond to such therapies, on the basis of specific mutations in proteins of the targeted pathway, has only recently been clinically validated and incorporated into some of the drug labels. This article highlights lessons learned from the development of the first drugs targeting the EGFR family and discusses strategies to decrease the risk of failure in clinical development by more effectively integrating molecular diagnostics into anticancer drug discovery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Morgillo, F. & Lee, H. Y. Lonafarnib in cancer therapy. Expert Opin. Investig. Drugs 6, 709–719 (2006).
Giaccone, G. et al. Gefitinib in combination with gemcitabin and cisplatin in advanced non-small cell lung cancer: a phase III trial — INTACT1. J. Clin. Oncol. 22, 777 (2004).
Herbst, R. S. et al. Gefitinib in combination with paclitaxel and carboplatin in advanced non-small cell lung cancer: a phase III trial — INTACT2. J. Clin. Oncol. 22, 785–794 (2004).
Twombly, R. Failing survival advantage in crucial trial, future of Iressa is in jeopardy. J. Natl Cancer Inst. 97, 249–250 (2005).
Kosaka, T. et al. Mutations of the epidermal growth factor receptor gene in lung cancer: biological and clinical implications. Cancer Res. 64, 8919–8923 (2004).
Shigematsu, H. et al. Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. J. Natl Cancer Inst. 97, 339–346 (2005).
Marchetti, A. et al. EGFR mutations in non-small-cell lung cancer: analysis of a large series of cases and development of a rapid and sensitive method for diagnostic screening with potential implications on pharmacologic treatment. J. Clin. Oncol. 23, 857–865 (2005).
Bell, D. W. et al. Epidermal growth factor receptor mutations and gene amplification in non-small-cell lung cancer: molecular analysis of the IDEAL/INTACT gefitinib trials. J. Clin. Oncol. 31, 8081–8092 (2005).
Lynch, T. J. et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N. Engl. J. Med. 350, 2129–2139 (2004).
Paez, J. G. et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 304, 1497–1500 (2004).
Pao, W. et al. EGF receptor gene mutations are common in lung cancers from “never smokers” and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc. Natl Acad. Sci. USA 101, 13306–13311 (2004).
Tsao, M. S. et al. Erlotinib in lung cancer — molecular and clinical predictors of outcome. N. Engl. J. Med. 353, 133–144 (2005).
Cunningham, D. et al. Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N. Engl. J. Med. 351, 337–345 (2004).
Saltz, L. B. et al. Phase II trial of cetuximab in patients with refractory colorectal cancer that expresses the epidermal growth factor receptor. J. Clin. Oncol. 22, 1201–1208 (2004).
Normanno, N. et al. The ErbB receptors and their ligands in cancer: an overview. Curr. Drug Targets 3, 243–257 (2005).
Press, M. F. et al. Sensitivity of HER-2/neu antibodies in archival tissue samples: potential source of error in immunohistochemical studies of oncogene expression. Cancer Res. 54, 2771–2777 (1994).
Slamon, D. J. et al. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 235, 177–182 (1987).
Navolanic, P. M., Steelman, L. S. & McCurey, J. A. EGFR family signaling and its association with breast cancer development and resistance to chemotherapy. Int. J. Oncol. 22, 237–252 (2003).
Ross, J. S. et al. Targeted therapy in breast cancer: the HER-2/neu gene and protein. Mol. Cell. Proteomics 4, 379–398 (2004).
Hayes, D. F. & Thor, A. D. C-erbB-2 in breast cancer: development of a clinically useful marker. Semin. Oncol. 29, 231–145 (2002).
Masood, S. & Bui, M. M. Prognostic and predictive value of HER2/neu oncogene in breast cancer. Microsc. Res. Tech. 59, 102–108 (2002).
Schnitt, S. J. & Jacobs, T. W. Current status of HER2 testing: caught between a rock and a hard place. Am. J. Clin. Pathol. 116, 806–810 (2001).
Slamon, D. J. et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N. Engl. J. Med. 344, 783–792 (2001).
Vogel, C. L. et al. Efficacy and safety of trastuzumab as a single agent in first-line treatment of HER2-overexpressing metastatic breast cancer. J. Clin. Oncol. 20, 719–726 (2002).
Cobleigh, M. A. et al. Multinational study of the efficacy and safety of humanized anti-HER2 monoclonal antibody in women who have HER2-overexpressing metastatic breast cancer that has progressed after chemotherapy for metastatic disease. J. Clin. Oncol. 17, 2639–2648 (1999).
Mass, R. D., Press, M. F., Anderson, S., Murphy, M. & Slamon, D. Improved survival benefit from Herceptin (Trastuzumab) in patients selected by fluorescence in situ hybridization (FISH). Proc. ASCO. 20, 22a Abstract 85 (2001).
Ogura, H., Akiyama, F., Kasumi, F., Kazui, T. & Sakamoto, G. Evaluation of HER-2 status in breast carcinoma by fluorescence in situ hybridization and immunohistochemistry. Breast Cancer 10, 234–240 (2003).
Wolff, A. C. et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J. Clin. Oncol. 25, 118–145 (2007).
Mass, R. D. et al. The concordance between the clinical trials assay (CTA) and fluorescence in situ hybridization (FISH) in the Herceptin pivotal trials. Proc. Am. Soc. Clin. Oncol. 19, 75A (2000).
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology. v.2.2008: Breast Cancer (2008).
Fornier, M., Risio, M., Van Poznak, C. & Seidman, A. HER-2 testing and correlation with efficacy in Trastuzumab therapy. Oncology 16, 1340–1358 (2003).
Izumi, Y., Xu, L., di Tomaso, E., Fukumura, D. & Jain, R. K. Tumour biology: herceptin acts as an anti-angiogenic cocktail. Nature 416, 279–280 (2002).
Geyer, C. E. et al. Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N. Engl. J. Med. 355, 2733–2743 (2006).
Scaltriti, M. et al. Expression of p95HER2, a truncated form of the HER2 receptor, and response to anti-HER2 therapies in breast cancer. J. Natl Cancer Inst. 99, 628–638 (2007).
Kawamoto, T. et al. Growth stimulation of A431 cells by epidermal growth factor: identification of high-affinity receptors for epidermal growth factor by an anti-receptor monoclonal antibody. Proc. Natl Acad. Sci. USA 80, 1337–1341 (1983).
El-Rayes, B. F. & LoRusso, P. M. Targeting the epidermal growth factor receptor. Br. J. Cancer 91, 418–424 (2004).
Mendelsohn, J. & Baselga, J. Epidermal growth factor receptor targeting in cancer. Semin. Oncol. 33, 369–385 (2006).
Chung, K. Y., Shia, J., Kemeny, N. E. & Saltz, L. B. Cetuximab shows activity in colorectal cancer patients with tumors that do not express the epidermal growth factor receptor by immunohistochemistry. J. Clin. Oncol. 23, 1803–1810 (2005).
Moroni, M. et al. Gene copy number for epidermal growth factor receptor (EGFR) and clinical response to antiEGFR treatment in colorectal cancer: a cohort study. Lancet Oncol. 6, 279–286 (2005).
Lievre, A. KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res. 66, 3992–3995 (2006).
Shia, J. et al. Epidermal growth factor receptor expression and gene amplification in colorectal carcinoma: an immunohistochemical and chromogenic in situ hybridization study. Mod. Pathol. 18, 1350–1356 (2005).
Andreyev, H. J., Norman, A. R., Cunningham, D., Oates, J. R. & Clarke, P. A. Kirsten ras mutations in patients with colorectal cancer: the multicenter ''RASCAL'' study. J. Natl Cancer Inst. 90, 675–684 (1998).
Bokemeyer, C. et al. Fluorouracil, leucovorin, and oxaliplatin with and without cetuximab in the first-line treatment of metastatic colorectal cancer. J. Clin. Oncol. 27, 663–671 (2009).
Van Cutsem, E. et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N. Engl. J. Med. 360, 1408–1417 (2009).
Pirker, R. et al. Cetuximab plus chemotherapy in patients with advanced non-small-cell lung cancer (FLEX): an open-label randomised phase III trial. Lancet 373, 1525–1531 (2009).
Hirsch, F. R. et al. Increased EGFR gene copy number detected by fluorescent in situ hybridization predicts outcome in non-small-cell lung cancer patients treated with cetuximab and chemotherapy. J. Clin. Oncol. 26, 3351–3357 (2008).
Khambata-Ford, S. et al. K-Ras mutations (MT) and EGFR-related markers as potential predictors of cetuximab benefit in 1st line advanced NSCLC: results from the BMS099 study. J. Thorac Oncol. 3, S304 (2008).
O'Byrne, K. J. et al. Molecular and clinical predictors of outcome for cetuximab in non-small cell lung cancer (NSCLC): data from the FLEX study. J. Clin. Oncol. 27, 15S Abstract 8007 (2009).
Gibson, T. B., Ranganathan, A. & Grothey, A. Randomized phase III trial results of panitumumab, a fully human anti-epidermal growth factor receptor monoclonal antibody, in metastatic colorectal cancer. Clin. Colorectal Cancer 1, 29–31 (2006).
Fry, D. W. Mechanism of action of erbB tyrosine kinase inhibitors. Exp. Cell Res. 10, 131–139 (2003).
Fukuoka, M. et al. Multi-institutional randomized phase II trial of gefitinib for previously treated patients with advanced non-small-cell lung cancer (The IDEAL 1 Trial). J. Clin. Oncol. 15, 2237–2246 (2003).
Kris, M. G. et al. Efficacy of gefitinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in symptomatic patients with non-small cell lung cancer: a randomized trial. JAMA 22, 2149–2158 (2003).
Thatcher, N. et al. Gefitinib plus best supportive care in previously treated patients with refractory advanced non-small-cell lung cancer: results from a randomised, placebo-controlled, multicentre study (Iressa Survival Evaluation in Lung Cancer). Lancet 366, 1527–1537 (2005).
US Food and Drug Administration. FDA public health advisory: new labeling and distribution program for gefitinib (Iressa). Washington, DC. 17 June 2005.
Gatzemeier, U. et al. Phase III study of erlotinib in combination with cisplatin and gemcitabine in advanced non-small-cell lung cancer: the Tarceva Lung Cancer Investigation Trial. J. Clin. Oncol. 25, 1545–1552 (2007).
Herbst, R. S. et al. TRIBUTE: a phase III trial of erlotinib hydrochloride (OSI-774) combined with carboplatin and paclitaxel chemotherapy in advanced non-small-cell lung cancer. J. Clin. Oncol. 23, 5892–5899 (2005).
Shepherd, F. A. et al. National Cancer Institute of Canada Clinical Trials Group. Erlotinib in previously treated non-small-cell lung cancer. N. Engl. J. Med. 353, 123–132 (2005).
Uramoto, H. & Mitsudomi, T. Which biomarker predicts benefit from EGFR-TKI treatment for patients with lung cancer? Br. J. Cancer 96, 857–863 (2007).
Tokumo, M. et al. The relationship between epidermal growth factor receptor mutations and clinicopathologic features in non-small cell lung cancers. Clin. Cancer Res. 11, 1167–1173 (2005).
Cortes-Funes, H. et al. Epidermal growth factor receptor activating mutations in Spanish gefitinib-treated non-small-cell lung cancer patients. Ann. Oncol. 16, 1081–1086 (2005).
Eberhard, D. A. et al. Mutations in the epidermal growth factor receptor and in KRAS are predictive and prognostic indicators in patients with non-small-cell lung cancer treated with chemotherapy alone and in combination with erlotinib. J. Clin. Oncol. 23, 5900–5909 (2005).
Sequist, L. V. et al. Epidermal growth factor receptor mutation testing in the care of lung cancer patients. Clin. Cancer Res. 12, 4403–4408 (2006).
Zhu, C. Q. et al. Role of KRAS and EGFR as biomarkers of response to erlotinib in National Cancer Institute of Canada clinical trials group study BR.21. J. Clin. Oncol. 26, 4268–4275 (2008).
Pinter, F. et al. Epidermal growth factor receptor (EGFR) high gene copy number and activating mutations in lung adenocarcinomas are not consistently accompanied by positivity for EGFR protein by standard immunohistochemistry. J. Mol. Diagn. 10, 160–168 (2008).
Helfrich, B. A. et al. Antitumor activity of the epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor gefitinib (ZD1839, Iressa) in non-small cell lung cancer cell lines correlates with gene copy number and EGFR mutations but not EGFR protein levels. Clin. Cancer Res. 12, 7117–7125 (2006).
Mok, T. S. et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N. Engl. J. Med. 361, 947–957 (2009).
Kim, E. S. et al. Gefitinib versus docetaxel in previously treated non-small-cell lung cancer (INTEREST): a randomised phase III trial. Lancet 372, 1809–1818 (2008).
Douillard, J. Y. et al. Molecular predictors of outcome with gefitinib and docetaxel in previously treated non-small-cell lung cancer: data from the randomized phase III INTEREST trial. J. Clin. Oncol. 28 Dec 2009 (doi: 10.1200/JCO.2009.24.3030).
Li, J. et al. CYP3A phenotyping approach to predict systemic exposure to EGFR tyrosine kinase inhibitors. J. Natl Cancer Inst. 98, 1714–1723 (2006).
Hidalgo, M. et al. Phase I and pharmacologic study of OSI-774, an epidermal growth factor receptor tyrosine kinase inhibitor, in patients with advanced solid malignancies J. Clin. Oncol. 19, 3267–3279 (2001).
Varkondi, E. et al. Biochemical assay-based selectivity profiling of clinically relevant kinase inhibitors on mutant forms of EGF receptor. J. Recept. Signal. Transduct. Res. 28, 295–306 (2008).
Riely, G. J., Marks, J. & Pao, W. KRAS mutations in non-small cell lung cancer. Proc. Am. Thorac. Soc. 6, 201–205 (2009).
Jackman, D. M. et al. Impact of epidermal growth factor receptor and KRAS mutations on clinical outcomes in previously untreated non-small cell lung cancer patients: results of an online tumor registry of clinical trials. Clin. Cancer Res. 15, 5267–5273 (2009).
Bonomi, P. D., Buckingham, L. & Coon, J. Selecting patients for treatment with epidermal growth factor tyrosine kinase inhibitors. Clin. Cancer Res. 13, 4606–4612 (2007).
Lim, K. H. et al. Lack of prognostic value of EGFR mutations in primary resected non-small cell lung cancer. Med. Oncol. 24, 388–393 (2007).
Kim, Y. T. et al. Molecular changes of epidermal growth factor receptor (EGFR) and KRAS and their impact on the clinical outcomes in surgically resected adenocarcinoma of the lung. Lung Cancer 59, 111–118 (2008).
van Krieken, J. H. et al. KRAS mutation testing for predicting response to anti-EGFR therapy for colorectal carcinoma: proposal for an European quality assurance program. Virchows Arch. 453, 417–431 (2008).
Viani, G. A., Afonso, S. L., Stefano, E. J., De Fendi, L. I. & Soares, F. V. Adjuvant trastuzumab in the treatment of her-2-positive early breast cancer: a meta-analysis of published randomized trials. BMC Cancer 7, 153 (2007).
Keri, G. et al. Drug discovery in the kinase inhibitory field using the nested chemical library™ technology. ASSAY Drug Dev. Techn. 3, 543–551 (2005).
Vulpetti, A. & Bosotti, R. Sequence and structural analysis of kinase ATP pocket residues. Farmaco. 59, 759–765 (2004).
Szántai-Kis, C. et al. Prediction oriented QSAR modelling of EGFR inhibition. Curr. Med. Chem. 13, 277–287 (2006).
Ding, L. et al. Somatic mutations affect key pathways in lung adenocarcinoma. Nature 455, 1069–1075 (2008).
Wood, L. D. et al. The genomic landscapes of human breast and colorectal cancers. Science 16, 1108–1113 (2007).
Keri, G. et al. Signal transduction therapy with rationally designed kinase inhibitors. Curr. Signal Transd. 1, 67–95 (2006).
Jain, K. K. Personalised medicine. Curr. Opin. Mol. Ther. 4, 548–558 (2002).
Cappuzzo, F. et al. Primary resistance to cetuximab therapy in EGFR FISH-positive colorectal cancer patients. Br. J. Cancer 99, 83–89 (2008).
Ikehara, N. et al. BRAF mutation associated with dysregulation of apoptosis in human colorectal neoplasms. Int. J. Cancer 115, 943–950 (2005).
Endoh, H., Yatabe, Y., Kosaka, T., Kuwano, H. & Mitsudomi, T. PTEN and PIK3CA expression is associated with prolonged survival after gefitinib treatment in EGFR-mutated lung cancer patients. J. Thorac. Oncol. 1, 629–634 (2006).
Noro, R. et al. PTEN inactivation in lung cancer cells and the effect of its recovery on treatment with epidermal growth factor receptor tyrosine kinase inhibitors. Int. J. Oncol. 31, 1157–1163 (2007).
Frattini, M. et al. PTEN loss of expression predicts cetuximab efficacy in metastatic colorectal cancer patients. Br. J. Cancer 97, 1139–1145 (2007).
Jhawer, M. et al. PIK3CA mutation/PTEN expression status predicts response of colon cancer cells to the epidermal growth factor receptor inhibitor cetuximab. Cancer Res. 68, 1953–1961 (2008).
Mellinghoff, I. K. et al. Molecular determinants of the response of glioblastomas to EGFR kinase inhibitors. N. Engl. J. Med. 353, 2012–2024 (2006).
Berns, K. et al. A functional genetic approach identifies the PI3K pathway as a major determinant of trastuzumab resistance in breast cancer. Cancer Cell 4, 395–402 (2007).
Petak, I., Tillman, D. M. & Houghton, J. A. p53 dependence of Fas induction and acute apoptosis in response to 5-fluorouracil-leucovorin in human colon carcinoma cell lines. Clin. Cancer Res. 6, 4432–4441 (2000).
Petak, I. & Houghton, J. A. Shared pathways: death receptors and cytotoxic drugs in cancer therapy. Pathol. Oncol. Res. 7, 95–106 (2001).
Rho, J. K. et al. p53 enhances gefitinib-induced growth inhibition and apoptosis by regulation of Fas in non-small cell lung cancer. Cancer Res. 67, 1163–1169 (2007).
Cohen, S. J., Cohen, R. B. & Meropol, N. J. Targeting signal transduction pathways in colorectal cancer — more than skin deep. J. Clin. Oncol. 23, 5374–5385 (2005).
Wang, S. E. et al. HER2 kinase domain mutation results in constitutive phosphorylation and activation of HER2 and EGFR and resistance to EGFR tyrosine kinase inhibitors. Cancer Cell 10, 25–38 (2006).
Engelman, J. A. et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science 316, 1039–1043 (2007).
Gandhi, J. et al. Alterations in genes of the EGFR signaling pathway and their relationship to EGFR tyrosine kinase inhibitor sensitivity in lung cancer cell lines. PLoS One 4, 4576 (2009).
Wakeling, A. E. et al. Specific inhibition of epidermal growth factor receptor tyrosine kinase by 4-anilinoquinazolines. Breast Cancer Res. Treat. 38, 67–73 (1996).
Pratilas, C. A. et al. Genetic predictors of MEK dependence in non-small cell lung cancer. Cancer Res. 68, 9375–9383 (2008).
Kaelin, W. G. Jr. The concept of synthetic lethality in the context of anticancer therapy. Nature Rev. Cancer 9, 689–698 (2005).
Pao, W. et al. Integration of molecular profiling into the lung cancer clinic. Cancer Res. 15, 5317–5322 (2009).
Saif, M. W. Secondary hepatic resection as a therapeutic goal in advanced colorectal cancer. World J. Gastroenterol. 15, 3855–3864 (2009).
Morelli, M. P. et al. Sequence-dependent antiproliferative effects of cytotoxic drugs and epidermal growth factor receptor inhibitors. Ann. Oncol. 4, 61–66 (2005).
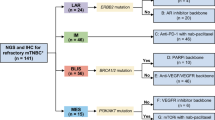
Kim, E. S. et al. Phase II randomized study of biomarker-directed treatment for non-small cell lung cancer (NSCLC): the BATTLE (Biomarker-Integrated Approaches of Targeted Therapy for Lung Cancer Elimination) clinical trial program. J. Clin. Oncol. 27, 15S Abstract 8024 (2009).
Ramanathan, R. K. et al. Low overexpression of HER-2/neu in advanced colorectal cancer limits the usefulness of trastuzumab (Herceptin) and irinotecan as therapy. A phase II trial. Cancer Invest. 22, 858–865 (2004).
Schilder, R. J. Phase II study of gefitinib in patients with relapsed or persistent ovarian or primary peritoneal carcinoma and evaluation of epidermal growth factor receptor mutations and immunohistochemical expression: a Gynecologic Oncology Group Study. Clin. Cancer Res. 11, 5539–5548 (2005).
Xia, W. et al. Lapatinib antitumor activity is not dependent upon phosphatase and tensin homologue deleted on chromosome 10 in ErbB2-overexpressing breast cancers. Cancer Res. 67, 1170–1175 (2007).
Guffanti, A. et al. A transcriptional sketch of a primary human breast cancer by 454 deep sequencing. BMC Genomics. 10, 163 (2009).
Abraham, J., Earl, H. M., Pharoah, P. D. & Caldas, C. Pharmacogenetics of cancer chemotherapy. Biochim. Biophys. Acta 1766, 168–183 (2006).
Jänsch, L. et al. Proteomics analysis of protein kinases by target class-selective prefractionation and tandem mass spectrometry. Mol. Cell Proteomics 6, 537–547 (2007).
Godl, K. et al. Proteomic characterization of the angiogenesis inhibitor SU6668 reveals multiple impacts on cellular kinase signalling. Cancer Res. 65, 6919–6926 (2005).
Brehmer, D. et al. Cellular targets of gefitinib. Cancer Res. 65, 379–382 (2005).
Daub, H. et al. Kinase-selective enrichment enables quantitative phosphoproteomics of the kinome across the cell cycle. Mol. Cell 31, 438–448 (2008).
Sharm, K. et al. Proteomics strategy for quantitative protein interaction profiling in cell extracts. Nature Methods 6, 741–744 (2009).
Bantscheff, M., Scholten, A. & Heck, A. J. Revealing promiscuous drug-target interactions by chemical proteomics. Drug Discov. Today 14, 1021–1029 (2009).
Bantscheff, M. et al. Quantitative chemical proteomics reveals mechanisms of action of clinical ABL kinase inhibitors. Nature Biotechnol. 25, 994–996 (2007).
Acknowledgements
This work was supported by grants (KKKII-05/2005, NKFP_07_A2-NANODRUG, TECH_08_A2-STEMKILL, NAP_BIO_06-FLU_DRUG and OTKA-T046665).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
István Peták and Richárd Schwab are co-founders of KPS, a company working in the field of molecular diagnostics. György Kéri and László Őrfi are co-founders of Vichem, a drug discovery company focusing on kinase inhibitors. István Peták and László Kopper have occasionally served on the advisory board of and have received honoraria from the Hungarian subsidies of Roche, AstraZeneca, Merck and Amgen.
Supplementary information
Supplementary information S1 (box)
Case study of an EGFR-TKI treated lung cancer patient (PDF 294 kb)
Supplementary information S2 (table)
Major clinical responses to signal transduction therapies are usually associated with the presence of cancer specific genetic changes detected by molecular diagnostic methods. (PDF 205 kb)
Related links
Rights and permissions
About this article
Cite this article
Peták, I., Schwab, R., Őrfi, L. et al. Integrating molecular diagnostics into anticancer drug discovery. Nat Rev Drug Discov 9, 523–535 (2010). https://doi.org/10.1038/nrd3135
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrd3135
This article is cited by
-
Bacteria‐derived ferrichrome inhibits tumor progression in sporadic colorectal neoplasms and colitis‐associated cancer
Cancer Cell International (2021)
-
A discrete organoplatinum(II) metallacage as a multimodality theranostic platform for cancer photochemotherapy
Nature Communications (2018)
-
Poly-ligand profiling differentiates trastuzumab-treated breast cancer patients according to their outcomes
Nature Communications (2018)
-
Systems biology driving drug development: from design to the clinical testing of the anti-ErbB3 antibody seribantumab (MM-121)
npj Systems Biology and Applications (2017)
-
Real-time single-molecule co-immunoprecipitation analyses reveal cancer-specific Ras signalling dynamics
Nature Communications (2013)