Key Points
-
The first evidence of the existence of renin was presented by Tigerstedt over 100 years ago. However, the importance of renin and the renin–angiotensin system (RAS) in the pathogenesis of cardiovascular disease was only fully realized in the 1970s.
-
Although the preferred target in the RAS was renin, at the top of the cascade, it was another 20 years before the first inhibitors of renin were available for clinical research.
-
The discovery and development of aliskiren (Tekturna) led to it becoming the first orally active renin inhibitor to be approved for clinical use. It was granted approval for the treatment of hypertension by the US Food and Drug Administration and the European Medicines Agency in 2007.
-
Aliskiren has shown efficacy as a monotherapy. Owing to its long duration of action, aliskiren has been shown to reduce daytime and night-time blood pressure (BP), and its effects last up to 4 weeks after therapy is stopped.
-
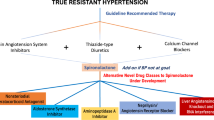
Combining aliskiren with other antihypertensive drugs, such as low-and high-dose angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), calcium-channel blockers and diuretics, results in a greater therapeutic efficacy, without adverse drug interactions being observed.
-
Aliskiren has been shown to be safe and efficacious in various patient populations including the elderly, different racial groups, diabetic patients, obese patients and patients with reduced renal and hepatic function.
-
Aliskiren shows potential for end-organ protection on top of standard therapy with ACE inhibitors and ARBs in patients with diabetic kidney disease and in patients with heart failure. When aliskiren is added to standard therapy there is a further positive therapeutic effect on surrogate markers of kidney and heart disease.
-
Renin inhibition opens up new therapeutic potential for more complete blockade of the RAS and further decreases in cardiovascular morbidity and mortality.
Abstract
The first evidence of the existence of renin was presented over 100 years ago. However, the importance of renin and the renin–angiotensin system in the pathogenesis of cardiovascular disease was only fully realized in the 1970s. It was another 20 years before the first inhibitors of renin were available for clinical research. Here, we describe the discovery and development of aliskiren, an orally active renin inhibitor, which became the first drug in its class to receive regulatory approval. In 2007, it was approved for the treatment of hypertension by the US Food and Drug Administration and the European Medicines Agency.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Tigerstedt, R. & Bergman, P. Niere und Kreislauf. Scand. Arch. Physiol. 8, 223–271 (1898). The original paper reporting the discovery or renin offers an interesting view of scientific experimentation in the late nineteenth century.
Silverman, B. D. Robert Tigerstedt — scientist, educator, social activist, humanitarian. Clin. Cardiol. 25, 399–400 (2002).
Goldblatt, H., Lynch, J., Hanzal, R. H. & Summerville, W. W. Studies on experimental hypertension: the production of persistent elevation of systolic blood pressure by means of renal ischemia. J. Exp. Med. 59, 347–349 (1934). Goldblatt's ground-breaking work on renal ischaemia and hypertension.
Skeggs, L. T., Marsh, W. H., Kahn, J. R. & Shumway, N. P. The existence of two forms of hypertensin. J. Exp. Med. 99, 275–282 (1954).
Skeggs, L. T., Lentz, K. E., Kahn, J. R., Shumway, N. P. & Woods, K. R. The amino acid sequence of hypertensin. II. J. Exp. Med. 104, 193–197 (1956).
Brunner, H. R. et al. Long-term treatment of hypertension in man by an orally active angiotensin-converting enzyme inhibitor. Clin. Sci. Mol. Med. Suppl. 4, 293S–295S (1978).
Brunner, H. R. et al. Orally active angiotensin-converting enzyme inhibitor (SQ 14,225) as a treatment for essential hypertension. Br. J. Clin. Pharmacol. 7 (Suppl. 2), 205–210 (1979).
Gavras, H., Charocopos, F., Brunner, H. & Gavras, I. Angiotensin converting enzyme inhibition: a new therapeutic modality. Bull. NY Acad. Med. 57, 304–310 (1981).
Rubin, B., Antonaccio, M. J. & Horovitz, Z. P. Captopril (SQ 14,225) (D-3-mercapto-2-methylpropranoylL-proline): a novel orally active inhibitor of angiotensin-converting enzyme and antihypertensive agent. Prog. Cardiovasc. Dis. 21, 183–194 (1978).
Brunner, H. R. et al. Clinical experience with angiotensin II receptor antagonists. Am. J. Hypertens. 5, 243S–246S (1992).
Christen, Y. et al. Oral administration of DuP 753, a specific angiotensin II receptor antagonist, to normal male volunteers. Inhibition of pressor response to exogenous angiotensin I and II. Circulation 83, 1333–1342 (1991).
Nussberger, J., Wuerzner, G., Jensen, C. & Brunner, H. R. Angiotensin II suppression in humans by the orally active renin inhibitor aliskiren (SPP100): comparison with enalapril. Hypertension 39, E1–E8 (2002). The first study on aliskiren to describe its effects on the RAS in humans.
Nussberger, J. et al. Dose-related effects of ACE inhibition in man: quinapril in patients with moderate congestive heart failure. The Study Group on Neurohormonal Regulation in Congestive Heart Failure: Lausanne, Switzerland; Berlin, Dusseldorf, Munich, Germany. Eur. Heart J. 15 (Suppl. D), 113–122 (1994).
Belova, L. A. Angiotensin II-generating enzymes. Biochemistry (Mosc.) 65, 1337–1345 (2000).
Wolny, A. et al. Functional and biochemical analysis of angiotensin II-forming pathways in the human heart. Circ. Res. 80, 219–227 (1997).
Yamada, M. et al. Mast cell chymase expression and mast cell phenotypes in human rejected kidneys. Kidney Int. 59, 1374–1381 (2001).
van den Meiracker, A. H. et al. Partial escape of angiotensin converting enzyme (ACE) inhibition during prolonged ACE inhibitor treatment: does it exist and does it affect the antihypertensive response? J. Hypertens. 10, 803–812 (1992).
Hanon, S., Vijayaraman, P., Sonnenblick, E. H. & Le Jemtel, T. H. Persistent formation of angiotensin II despite treatment with maximally recommended doses of angiotensin converting enzyme inhibitors in patients with chronic heart failure. J. Renin Angiotensin Aldosterone Syst. 1, 147–150 (2000).
Reinhardt, L. A., Wilkin, J. K. & Kirkendall, W. M. Lichenoid eruption produced by captopril. Cutis 31, 98–99 (1983).
Suarez, M., Ho, P. W., Johnson, E. S. & Perez, G. Angioneurotic edema, agranulocytosis, and fatal septicemia following captopril therapy. Am. J. Med. 81, 336–338 (1986).
Oparil, S. et al. Efficacy and safety of combined use of aliskiren and valsartan in patients with hypertension: a randomised, double-blind trial. Lancet 370, 221–229 (2007). This study showed that even at the highest recommended doses of both aliskiren and valsartan there is an additive effect on BP control.
Di, P. P. et al. Does the addition of losartan improve the beneficial effects of ACE inhibitors in patients with anterior myocardial infarction? A pilot study. Heart 81, 606–611 (1999).
Villamil, A. et al. Renin inhibition with aliskiren provides additive antihypertensive efficacy when used in combination with hydrochlorothiazide. J. Hypertens. 25, 217–226 (2007).
Alderman, M. H. et al. Association of the renin–sodium profile with the risk of myocardial infarction in patients with hypertension. N. Engl. J. Med. 324, 1098–1104 (1991).
Alderman, M. H. et al. Plasma renin activity: a risk factor for myocardial infarction in hypertensive patients. Am. J. Hypertens. 10, 1–8 (1997).
Sielecki, A. R. et al. Structure of recombinant human renin, a target for cardiovascular-active drugs, at 2.5 Å resolution. Science 243, 1346–1351 (1989).
Hobart, P. M., Fogliano, M., O'Conner, B. A., Schaefer, I. M. & Chirgwin, J. M. Human renin gene: structure and sequence analysis. Proc. Natl Acad. Sci. USA 81, 5026–5030 (1984).
Nguyen, G. et al. Pivotal role of the renin/prorenin receptor in angiotensin II production and cellular responses to renin. J. Clin. Invest. 109, 1417–1427 (2002).
Danser, A. H., Batenberg, W. W. & van Esch, J. H. Prorenin and the (pro)renin receptor — an update. Nephrol. Dial. Transplant. 22, 1288–1292 (2007).
Ichihara, A. et al. Inhibition of diabetic nephropathy by a decoy peptide corresponding to the “handle” region for nonproteolytic activation of prorenin. J. Clin. Invest. 114, 1128–1135 (2004).
Luft, F. C. Renin and its putative receptor remain enigmas. J. Am. Soc. Nephrol. 18, 1989–1992 (2007).
Goschke, R. et al. Novel 2,7-dialkyl-substituted 5(S)-amino-4(S)-hydroxy-8-phenyl-octanecarboxamide transition state peptidomimetics are potent and orally active inhibitors of human renin. J. Med. Chem. 50, 4818–4831 (2007).
Maibaum, J. et al. Structural modification of the P2′ position of 2,7-dialkyl-substituted 5(S)-amino-4(S)-hydroxy-8-phenyl-octanecarboxamides: the discovery of aliskiren, a potent non-peptide human renin inhibitor active after once daily dosing in marmosets. J. Med. Chem. 50, 4832–4844 (2007). Description of extended structure–activity relationship exploration of topologically P3-P1-tethered transition-state mimetic renin inhibitors resulting in increased in vivo potency and improved oral bioavailability.
Szelke, M. et al. Potent new inhibitors of human renin. Nature 299, 555–557 (1982).
Delabays, A. et al. Hemodynamic and humoral effects of the new renin inhibitor enalkiren in normal humans. Hypertension 13, 941–947 (1989).
Boger, R. S. et al. Prolonged duration of blood pressure response to enalkiren, the novel dipeptide renin inhibitor, in essential hypertension. Hypertension 15, 835–840 (1990).
Clozel, J. P. & Fischli, W. Discovery of remikiren as the first orally active renin inhibitor. Arzneimittelforschung 43, 260–262 (1993).
Himmelmann, A., Bergbrant, A., Svensson, A., Hansson, L. & Aurell, M. Remikiren (Ro 42-5892) — an orally active renin inhibitor in essential hypertension. Effects on blood pressure and the renin–angiotensin–aldosterone system. Am. J. Hypertens. 9, 517–522 (1996).
Rahuel, J. et al. Structure-based drug design: the discovery of novel nonpeptide orally active inhibitors of human renin. Chem. Biol. 7, 493–504 (2000). Description of crystal structure analysis of renin–inhibitor complexes and the interaction with the hitherto unrecognized large, distinct, sub-pocket S3sp of the enzyme, which is essential for high binding affinity.
Wood, J. M. et al. Structure-based design of aliskiren, a novel orally effective renin inhibitor. Biochem. Biophys. Res. Commun. 308, 698–705 (2003). Description of the discovery of aliskiren using a combination of molecular modelling and crystallographic structure analysis.
Weber, C. et al. Multiple dose pharmacokinetics and concentration effect relationship of the orally active renin inhibitor remikiren (Ro 42-5892) in hypertensive patients. Br. J. Clin. Pharmacol. 36, 547–554 (1993).
Davio, S. R., McShane, M. M., Kakuk, T. J., Zaya, R. M. & Cole, S. L. Precipitation of the renin inhibitor ditekiren upon i.v. infusion; in vitro studies and their relationship to in vivo precipitation in the cynomolgus monkey. Pharm. Res. 8, 80–83 (1991).
Shibasaki, M., Usui, T., Inagaki, O., Asano, M. & Takenaka, T. Pharmacokinetics and cardiovascular effects of YM-21095, a novel renin inhibitor, in dogs and monkeys. J. Pharm. Pharmacol. 46, 68–72 (1994).
Wood, J. M., Schnell, C. R., Cumin, F., Menard, J. & Webb, R. L. Aliskiren, a novel, orally effective renin inhibitor, lowers blood pressure in marmosets and spontaneously hypertensive rats. J. Hypertens. 23, 417–426 (2005). A thorough review of the preclinical research on aliskiren.
Wood, J. M. et al. Evaluation of a potent inhibitor of subprimate and primate renins. J. Pharmacol. Exp. Ther. 253, 513–517 (1990).
Ganten, D. et al. Species specificity of renin kinetics in transgenic rats harboring the human renin and angiotensinogen genes. Proc. Natl Acad. Sci. USA 89, 7806–7810 (1992).
Pilz, B. et al. Aliskiren, a human renin inhibitor, ameliorates cardiac and renal damage in double-transgenic rats. Hypertension 46, 569–576 (2005).
Azizi, M. et al. Pharmacologic demonstration of the synergistic effects of a combination of the renin inhibitor aliskiren and the AT1 receptor antagonist valsartan on the angiotensin II-renin feedback interruption. J. Am. Soc. Nephrol. 15, 3126–3133 (2004).
Stanton, A., Jensen, C., Mann, J., and O'Brien, E. Blood pressure lowering with SPP100, a novel orally active renin inhibitor. A pilot study. Hypertension 38, 526 (2001).
Stanton, A., Jensen, C., Nussberger, J., and O'Brien, E. Blood pressure lowering in essential hypertension with an oral renin inhibitor, aliskiren. Hypertension 42, 1137–1143 (2003). The first dose-finding study with aliskiren in patients using 24-hour ambulatory BP measurements.
Gradman, A. H. et al. Aliskiren, a novel orally effective renin inhibitor, provides dose-dependent antihypertensive efficacy and placebo-like tolerability in hypertensive patients. Circulation 111, 1012–1018 (2005).
Chobanian, A. V. et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 289, 2560–2572 (2003).
Williams, B. et al. British Hypertension Society guidelines for hypertension management 2004 (BHS-IV): summary. BMJ 328, 634–640 (2004).
Erdine, S. et al. ESH–ESC guidelines for the management of hypertension. Herz 31, 331–338 (2006).
O'Brien, E. et al. Aliskiren reduces blood pressure and suppresses plasma renin activity in combination with a thiazide diuretic, an angiotensin-converting enzyme inhibitor, or an angiotensin receptor blocker. Hypertension 49, 276–284 (2007).
Uresin, Y. et al. Efficacy and safety of the direct renin inhibitor aliskiren and ramipril alone or in combination in patients with diabetes and hypertension. J. Renin Angiotensin Aldosterone Syst. 8, 190–198 (2007).
Drummond, W. et al. Antihypertensive efficacy of the oral direct renin inhibitor aliskiren as add-on therapy in patients not responding to amlodipine monotherapy. J. Clin. Hypertens. 9, 742–750 (2007).
Bramlage, P. et al. Hypertension in overweight and obese primary care patients is highly prevalent and poorly controlled. Am. J. Hypertens. 17, 904–910 (2004).
Jordan, J., Engeli, S., Boye, S. W., Le, B. S. & Keefe, D. L. Direct renin inhibition with aliskiren in obese patients with arterial hypertension. Hypertension 49, 1047–1055 (2007).
Sekikawa, A. & Hayakawa, T. Prevalence of hypertension, its awareness and control in adult population in Japan. J. Hum. Hypertens. 18, 911–912 (2004).
Hasegawa, T., Hori, Y., Sakamaki, H. & Suzuki, K. Meta-analysis on the therapeutic state of hypertensive population in Japan: focusing on the impact of new diagnostic criteria of Japanese Guideline for the Management of Hypertension 2000. J. Epidemiol. 12, 112–119 (2002).
Hozawa, A. et al. Blood pressure control assessed by home, ambulatory and conventional blood pressure measurements in the Japanese general population: the Ohasama study. Hypertens. Res. 25, 57–63 (2002).
Kushiro, T. et al. Aliskiren, a novel oral renin inhibitor, provides dose-dependent efficacy and placebo-like tolerability in Japanese patients with hypertension. Hypertens. Res. 29, 997–1005 (2006).
Vaidyanathan, S., Jermany, J., Yeh, C., Bizot, M. N. & Camisasca, R. Aliskiren, a novel orally effective renin inhibitor, exhibits similar pharmacokinetics and pharmacodynamics in Japanese and Caucasian subjects. Br. J. Clin. Pharmacol. 62, 690–698 (2006).
Vaidyanathan, S. et al. Pharmacokinetics, safety, and tolerability of the novel oral direct renin inhibitor aliskiren in elderly healthy subjects. J. Clin. Pharmacol. 47, 453–460 (2007).
Weir, M., Bush, C. & Zhang, J. Antihypertensive efficacy and safety of the oral renin inhibitor aliskiren in patients with hypertension: a pooled analysis. Eur. Heart J. 27 (Suppl. 1), 299 (2006).
Waldmeier, F. et al. Absorption, distribution, metabolism, and elimination of the direct renin inhibitor aliskiren in healthy volunteers. Drug Metab. Dispos. 35, 1418–1428 (2007).
Vaidyanathan, S. et al. Pharmacokinetics of the oral direct renin inhibitor aliskiren alone and in combination with irbesartan in renal impairment. Clin. Pharmacokinet. 46, 661–675 (2007).
Vaidyanathan, S. et al. Pharmacokinetics, safety, and tolerability of the oral renin inhibitor aliskiren in patients with hepatic impairment. J. Clin. Pharmacol. 47, 192–200 (2007).
Zhao, C., Vaidyanathan, S., Yeh, C. M., Maboudian, M. & Armin, D. H. Aliskiren exhibits similar pharmacokinetics in healthy volunteers and patients with type 2 diabetes mellitus. Clin. Pharmacokinet. 45, 1125–1134 (2006).
European Medicines Agency (EMEA). Rasilez: European Public Assessment Report. EMEA web site [online], (2007).
Textor, S. C., Bravo, E. L., Fouad, F. M. & Tarazi, R. C. Hyperkalemia in azotemic patients during angiotensin-converting enzyme inhibition and aldosterone reduction with captopril. Am. J. Med. 73, 719–725 (1982).
Kostis, J. B. et al. Adverse effects of enalapril in the Studies of Left Ventricular Dysfunction (SOLVD). SOLVD Investigators. Am. Heart J. 131, 350–355 (1996).
Sealey, J. E. & Laragh, J. H. Aliskiren, the first renin inhibitor for treating hypertension: reactive renin secretion may limit its effectiveness. Am. J. Hypertens. 20, 587–597 (2007).
Pool, J. L. et al. Aliskiren, a novel renin inhibitor, provides long-term suppression of the renin system, when used alone or in combination with hydrochlorothiazide in the treatment of hypertension. Eur. Heart J. 27 (Suppl. 1), 119 (2006).
Weinberger, M. H. et al. Aliskiren-based therapy provides long-term suppression of plasma renin activity that persists after treatment withdrawal in patients with hypertension. J. Am. Coll. Cardiol. 49, 390A (2007).
Keefe, D. L. et al. Blood pressure lowering effects persist following the last dose of long-term therapy with aliskiren: an oral direct renin inhibitor. J. Am. Coll. Cardiol. 49, 372A (2007).
Vaidyanathan, S. Aliskiren, a novel oral renin inhibitor, has no interaction with cytochrome P450 isoenzymes in vitro. Basic Res. Pharmacol. Toxicol. 97, 239–239 (2005).
Zhao, C. et al. Assessment of the pharmacokinetic interaction between the oral direct inhibitor aliskiren and furosemide: a study in healthy volunteers. Clin. Pharmacol. Ther. 81 (Suppl. 1) S110 (2007).
Vaidyanathan, S. et al. Lack of pharmacokinetic interactions of aliskiren, a novel direct renin inhibitor for the treatment of hypertension, with the antihypertensives amlodipine, valsartan, hydrochlorothiazide (HCTZ) and ramipril in healthy volunteers. Int. J. Clin. Pract. 60, 1343–1356 (2006).
Azizi, M. & Menard, J. Combined blockade of the renin–angiotensin system with angiotensin-converting enzyme inhibitors and angiotensin II type 1 receptor antagonists. Circulation 109, 2492–2499 (2004).
Muller, D. N. & Luft, F. C. Direct renin inhibition with aliskiren in hypertension and target organ damage. Clin. J. Am. Soc. Nephrol. 1, 221–228 (2006).
Mervaala, E. et al. Angiotensin-converting enzyme inhibition and AT1 receptor blockade modify the pressure–natriuresis relationship by additive mechanisms in rats with human renin and angiotensinogen genes. J. Am. Soc. Nephrol. 10, 1669–1680 (1999).
Mervaala, E. et al. Blood pressure-independent effects in rats with human renin and angiotensinogen genes. Hypertension 35, 587–594 (2000).
Shagdarsuren, E. et al. Complement activation in angiotensin II-induced organ damage. Circ. Res. 97, 716–724 (2005).
Fisher, N. D. & Hollenberg, N. K. Unprecedented renal response to direct bloackade of the renin–angiotensin system with aliskiren, a novel renin inhibitor. Circulation 116 (Suppl. 2) 556 (2007).
Kjeldsen, S. E. Direct renin inhibition with focus on aliskiren and cardiovascular outcome studies. Eur. Cardiovasc. Dis. 2, 17–19 (2006).
Recio-Mayoral, A. et al. Clinical trials update from the European Society of Cardiology Congress in Vienna, 2007: PROSPECT, EVEREST, ARISE, ALOFT, FINESSE, Prague-8, CARESS in MI and ACUITY. Cardiovasc. Drugs Ther. 21, 1573–7241 (2007).
Recion-Mayoral, A. et al. Clinical trials update from the European Society of Cardiology Congress in Vienna, 2007: PROSPECT, EVEREST, ARISE, ALOFT, FINESSE, Prague-8, CARESS in MI and ACUITY. Cardiovasc. Drugs Ther. 21, 459–465 (2007).
Pitt, B. et al. Neurohormonal effects of a new oral direct renin inhibitor in stable heart failure: the alisikiren observation of heart failure treatment study (ALOFT). Circulation 116 (Suppl. 2), 549 (2007).
Parving, H. H., Lewis, J. B., Lewis, E. J. & Hollenberg, N. K. Aliskiren in the evaluation of proteinuria in diabetes (AVOID). Renal Week October 31–November 5; Abstract SA-PO1051. American Society of Nephrology web site [online], (2007).
Persson, F., Rossing, P., Schjoedt, K. J., Stehouwer, C. D. & Parving, H. H. Time course of the antiproteinuric and antihypertensive effect of direct renin inhibition with aliskiren in patients with type 2 diabetes and albuminuria. Circulation 116 (Suppl.), PS112 (2007).
Brenner, B. M. et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N. Engl. J. Med. 345, 861–869 (2001).
Lewis, E. J. et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N. Engl. J. Med. 345, 851–860 (2001).
Herold, P., Stutz, S. & Indoloese, A. Production of N-substituted 2,7-dialkyl-4-hydroxy-5-amino-8-aryl octanoylamides. WO0109083 (2001).
Herold, P. & Stutz, S. 2-Alkyl-5-halogen-pent-4-ene carboxylic acids and their production. WO0109079 (2001).
Herold, P. & Stutz, S. Preparation of (R)-2-alkyl-3-phenylpropionic acids. Patent WO0202500 (2002).
Herold, P., Stutz, S. & Spindler, F. Process for the preparation of (R)-2-Alkyl-3-phenyl-1-propanols. WO0202487 (2002).
Herold, P., Stutz, S. & Spindler, F. Process for the preparation of substituted octanoyl amides. WO0202508 (2002).
Stutz, S. & Herold, P. Process for the preparation of substituted carboxylic acid esters by enzymatic hydrolysis. WO02092828 (2002).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Chris Jensen is a consultant to Speedel Holding Ltd and a shareholder. He is also a former employee of Speedel Experimenta Ltd, Basel, Switzerland.
Peter Herold is employed by Speedel Experimenta Ltd.
Hans Rudolf Brunner is a consultant to Speedel Holding ltd and a shareholder.
Supplementary information
Supplementary information S1 (table)
Change from baseline to endpoint in mean sitting diastolic (DBP) and systolic blood (SBP) pressure in five placebo-controlled studies, ITT population1–5. (PDF 161 kb)
Glossary
- Hypertrophy
-
An increase in ventricular mass, which is typically characterized by an increased cardiac myocyte size in conjunction with cardiac fibrosis.
- Fibrosis
-
The formation of excess connective tissue.
- Angioedema
-
A rapid swelling of the skin, mucosa or submucosal tissues.
- Diuretics
-
Drugs that increase the net renal excretion of solute and water.
- Peptidomimetic
-
Small-molecule chemicals that mimic the effects of short peptides.
- Chiral centre
-
Any atom in a molecule bearing at least four different substituents.
- Synthon
-
A synthon is defined as a structural unit within a molecule that is related to a possible synthetic operation.
- Proteinuria
-
The presence of excess serum proteins in the urine.
- Aldosterone
-
A steroid hormone that acts to reabsorb sodium and increases blood pressure.
- Retrosynthetic analysis
-
A synthesis that is planned in reverse, beginning with the final product.
- Cytochrome P450 system
-
A family of haem proteins responsible for oxidative drug metabolism.
- BNP
-
Brain natiuretic protein is secreted by the heart in response to stretching of the heart muscle cells. It is used as a biochemical measure of heart failure.
- Macro-albuminuria
-
The urinary excretion of >300 mg per day of serum albumin.
- Urinary albumin creatinine ratio
-
A biochemical measure of chronic kidney disease.
Rights and permissions
About this article
Cite this article
Jensen, C., Herold, P. & Brunner, H. Aliskiren: the first renin inhibitor for clinical treatment. Nat Rev Drug Discov 7, 399–410 (2008). https://doi.org/10.1038/nrd2550
Issue Date:
DOI: https://doi.org/10.1038/nrd2550
This article is cited by
-
Sex differences in preclinical models of hypertension
Journal of Human Hypertension (2022)
-
Current and Emerging Classes of Pharmacological Agents for the Management of Hypertension
American Journal of Cardiovascular Drugs (2022)
-
Importance of the renal ion channel TRPM6 in the circadian secretion of renin to raise blood pressure
Nature Communications (2021)
-
Drug discovery effectiveness from the standpoint of therapeutic mechanisms and indications
Nature Reviews Drug Discovery (2018)
-
Anti-diabetic and renoprotective effects of aliskiren in streptozotocin-induced diabetic nephropathy in female rats
Naunyn-Schmiedeberg's Archives of Pharmacology (2016)