Key Points
-
Integrin antagonists are highly successful drugs for targeting the ligand binding site of αIIbβ3, α4-containing or α4β7 integrins.
-
Antagonists to αIIbβ3 integrin are still being used in patients receiving percutaneous angioplasty but are being replaced in many instances by new classes of anticoagulants and platelet inhibitors.
-
Natalizumab, a monoclonal antibody against α4-containing integrins, is highly successful at treating multiple sclerosis, but can reactivate John Cunningham virus and cause lethal progressive multifocal leukoencephalopathy (PML).
-
Vedolizumab, a monoclonal antibody against α4β7 integrin, and new antibodies against the β7 integrin subunit have not shown any signs of inducing PML.
-
Vedolizumab is safe and effective in the treatment of inflammatory bowel disease and has effectively replaced natalizumab for the treatment of Crohn disease.
Abstract
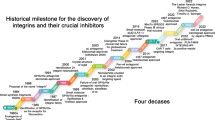
Integrins are activatable molecules that are involved in adhesion and signalling. Of the 24 known human integrins, 3 are currently targeted therapeutically by monoclonal antibodies, peptides or small molecules: drugs targeting the platelet αIIbβ3 integrin are used to prevent thrombotic complications after percutaneous coronary interventions, and compounds targeting the lymphocyte α4β1 and α4β7 integrins have indications in multiple sclerosis and inflammatory bowel disease. New antibodies and small molecules targeting β7 integrins (α4β7 and αEβ7 integrins) and their ligands are in clinical development for the treatment of inflammatory bowel diseases. Integrin-based therapeutics have shown clinically significant benefits in many patients, leading to continued medical interest in the further development of novel integrin inhibitors. Of note, almost all integrin antagonists in use or in late-stage clinical trials target either the ligand-binding site or the ligand itself.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Tadokoro, S. et al. Talin binding to integrin β tails: a final common step in integrin activation. Science 302, 103–106 (2003).
Moser, M., Legate, K. R., Zent, R. & Fassler, R. The tail of integrins, talin, and kindlins. Science 324, 895–899 (2009).
Mocsai, A. et al. Integrin signaling in neutrophils andmacrophages uses adaptors containing immunoreceptor tyrosine-based activation motifs. Nat. Immunol. 7, 1326–1333 (2006).
Mocsai, A., Zhou, M., Meng, F., Tybulewicz, V. L. & Lowell, C. A. Syk is required for integrin signaling in neutrophils. Immunity 16, 547–558 (2002).
Arias-Salgado, E. G. et al. Src kinase activation by direct interaction with the integrin β cytoplasmic domain. Proc. Natl Acad. Sci. USA 100, 13298–13302 (2003).
Scharffetter-Kochanek, K. et al. Spontaneous skin ulceration and defective T cell function in CD18 null mice. J. Exp. Med. 188, 119–131 (1998).
Shimaoka, M. & Springer, T. A. Therapeutic antagonists and conformational regulation of integrin function. Nat. Rev. Drug Discov. 2, 703–716 (2003).
Mitroulis, I. et al. Leukocyte integrins: role in leukocyte recruitment and as therapeutic targets in inflammatory disease. Pharmacol. Ther. 147, 123–135 (2015).
Wright, D. B., Meurs, H. & Dekkers, B. G. Integrins: therapeutic targets in airway hyperresponsiveness and remodelling? Trends Pharmacol. Sci. 35, 567–574 (2014).
Goodman, S. L. & Picard, M. Integrins as therapeutic targets. Trends Pharmacol. Sci. 33, 405–412 (2012).
Shimaoka, M. et al. Structures of the αL I domain and its complex with ICAM-1 reveal a shape-shifting pathway for integrin regulation. Cell 112, 99–111 (2003).
Hynes, R. O. Integrins: bidirectional, allosteric signaling machines. Cell 110, 673–687 (2002).
Kim, M., Carman, C. V. & Springer, T. A. Bidirectional transmembrane signaling by cytoplasmic domain separation in integrins. Science 301, 1720–1725 (2003).
Shattil, S. J., Kim, C. & Ginsberg, M. H. The final steps of integrin activation: the end game. Nat. Rev. Mol. Cell. Biol. 11, 288–300 (2010).
Luo, B. H., Carman, C. V. & Springer, T. A. Structural basis of integrin regulation and signaling. Annu. Rev. Immunol. 25, 619–647 (2007).
Ye, F., Kim, C. & Ginsberg, M. H. Reconstruction of integrin activation. Blood 119, 26–33 (2012).
Pierschbacher, M. D. & Ruoslahti, E. Cell attachment activity of fibronectin can be duplicated by small synthetic fragments of the molecule. Nature 309, 30–33 (1984).
Wayner, E. A., Garcia-Pardo, A., Humphries, M. J., McDonald, J. A. & Carter, W. G. Identification and characterization of the T lymphocyte adhesion receptor for an alternative cell attachment domain (CS-1) in plasma fibronectin. J. Cell Biol. 109, 1321–1330 (1989).
Shimaoka, M., Salas, A., Yang, W., Weitz-Schmidt, G. & Springer, T. A. Small molecule integrin antagonists that bind to the β2 subunit I-like domain and activate signals in one direction and block them in the other. Immunity 19, 391–402 (2003).
Xiao, T., Takagi, J., Coller, B. S., Wang, J. H. & Springer, T. A. Structural basis for allostery in integrins and binding to fibrinogen-mimetic therapeutics. Nature 432, 59–67 (2004).
Salas, A. et al. Rolling adhesion through an extended conformation of integrin αLβ2 and relation to α I and β I-like domain interaction. Immunity 20, 393–406 (2004).
Kuwano, Y., Spelten, O., Zhang, H., Ley, K. & Zarbock, A. Rolling on E- or P-selectin induces the extended but not high-affinity conformation of LFA-1 in neutrophils. Blood 116, 617–624 (2010).
Zarbock, A., Lowell, C. A. & Ley, K. Spleen tyrosine kinase Syk is necessary for E-selectin-induced αLβ2 integrin mediated rolling on Intercellular Adhesion Molecule-1. Immunity 26, 773–783 (2007).
Lefort, C. T. et al. Distinct roles for talin-1 and kindlin-3 in LFA-1 extension and affinity regulation. Blood 119, 4275–4283 (2012).
Weitz-Schmidt, G. et al. Statins selectively inhibit leukocyte function antigen-1 by binding to a novel regulatory integrin site. Nat. Med. 7, 687–692 (2001).
Chigaev, A. et al. Real-time analysis of the inside-out regulation of lymphocyte function-associated antigen-1 revealed similarities and differences with very late antigen-4. J. Biol. Chem. 286, 20375–20386 (2011).
Chigaev, A., Wu, Y., Williams, D. B., Smagley, Y. & Sklar, L. A. Discovery of very late antigen-4 (VLA-4, α4β1 integrin) allosteric antagonists. J. Biol. Chem. 286, 5455–5463 (2011).
Coller, B. S. & Shattil, S. J. The GPIIb/IIIa (integrin αIIbβ3) odyssey: a technology driven saga of a receptor with twists, turns and even a bend. Blood 112, 3011–3025 (2008).
Nieswandt, B. & Watson, S. P. Platelet-collagen interaction: is GPVI the central receptor? Blood 102, 449–461 (2003).
Bledzka, K., Smyth, S. S. & Plow, E. F. Integrin αIIbβ3: from discovery to efficacious therapeutic target. Circ. Res. 112, 1189–1200 (2013).
Hawiger, J., Timmons, S., Kloczewiak, M., Strong, D. D. & Doolittle, R. F. γ and α chains of human fibrinogen possess sites reactive with human platelet receptors. Proc. Natl Acad. Sci. USA 79, 2068–2071 (1982).
Plow, E. F., Pierschbacher, M. D., Ruoslahti, E., Marguerie, G. A. & Ginsberg, M. H. The effect of Arg-Gly-Asp-containing peptides on fibrinogen and von Willebrand factor binding to platelets. Proc. Natl Acad. Sci. USA 82, 8057–8061 (1985).
Moser, M., Nieswandt, B., Ussar, S., Pozgajova, M. & Fassler, R. Kindlin-3 is essential for integrin activation and platelet aggregation. Nat. Med. 14, 325–330 (2008).
Kuijpers, T. W. et al. LAD-1/variant syndrome is caused by mutations in FERMT3. Blood 113, 4740–4746 (2009).
Ye, F. et al. The mechanism of kindlin-mediated activation of integrin αIIbβ3. Curr. Biol. 23, 2288–2295 (2013).
Coller, B. S. Platelet GPIIb/IIIa antagonists: The first anti-integrin receptor therapeutics. J. Clin. Invest. 99, 1467–1471 (1997).
Phillips, D. R. & Scarborough, R. M. Clinical pharmacology of eptifibatide. Am J. Cardiol. 80, 11B–20B (1997).
Cook, J. J. et al. Tirofiban (Aggrastat(R)). Cardiovasc. Drug Rev. 17, 199–224 (1999).
Estevez, B., Shen, B. & Du, X. Targeting integrin and integrin signaling in treating thrombosis. Arterioscler. Thromb. Vasc. Biol. 35, 24–29 (2014).
Felding-Habermann, B. & Cheresh, D. A. Vitronectin and its receptors. Curr. Opin. Cell Biol. 5, 864–868 (1993).
Chinot, O. L. Cilengitide in glioblastoma: when did it fail? Lancet Oncol. 15, 1044–1045 (2014).
Reynolds, A. R. et al. Stimulation of tumor growth and angiogenesis by low concentrations of RGD-mimetic integrin inhibitors. Nat. Med. 15, 392–400 (2009).
Wong, P. P. et al. Dual-action combination therapy enhances angiogenesis while reducing tumor growth and spread. Cancer Cell 27, 123–137 (2015).
Coller, B. S. Anti-GPIIb/IIIa drugs: current strategies and future directions. Thromb. Haemost. 86, 427–443 (2001).
Artoni, A. et al. Integrin β3 regions controlling binding of murine mAb 7E3: implications for the mechanism of integrin αIIbβ3 activation. Proc. Natl Acad. Sci. USA 101, 13114–13120 (2004).
Tam, S. H., Sassoli, P. M., Jordan, R. E. & Nakada, M. T. Abciximab (ReoPro, chimeric 7E3 Fab) demonstrates equivalent affinity and functional blockade of glycoprotein IIb/IIIa and avb3 integrins. Circulation 98, 1085–1091 (1998).
Kintscher, U. et al. Effects of abciximab and tirofiban on vitronectin receptors in human endothelial and smooth muscle cells. Eur. J. Pharmacol. 390, 75–87 (2000).
Scarborough, R. M. Structure-activity relationships of b-amino acid-containing integrin antagonists. Curr. Med. Chem. 6, 971–981 (1999).
Aster, R. H. Immune thrombocytopenia caused by glycoprotein IIb/IIIa inhibitors. Chest 127, 53S–59S (2005).
Bougie, D. W. et al. Acute thrombocytopenia after treatment with tirofiban or eptifibatide is associated with antibodies specific for ligand-occupied GPIIb/IIIa. Blood 100, 2071–2076 (2002).
Kastrati, A. et al. Abciximab in patients with acute coronary syndromes undergoing percutaneous coronary intervention after clopidogrel pretreatment: the ISAR-REACT 2 randomized trial. JAMA 295, 1531–1538 (2006).
Franchi, F. & Angiolillo, D. J. Novel antiplatelet agents in acute coronary syndrome. Nat. Rev. Cardiol. 12, 30–47 (2015).
Kristensen, S. D. et al. Contemporary use of glycoprotein IIb/IIIa inhibitors. Thromb. Haemost. 107, 215–224 (2012).
Cox, D. Oral GPIIb/IIIa antagonists: what went wrong? Curr. Pharm. Des. 10, 1587–1596 (2004).
Bassler, N. et al. A mechanistic model for paradoxical platelet activation by ligand-mimetic αIIbβ3 (GPIIb/IIIa) antagonists. Arterioscler. Thromb. Vasc. Biol. 27, e9–e15 (2007).
Li, J. et al. RUC-4: a novel αIIbβ3 antagonist for prehospital therapy of myocardial infarction. Arterioscler. Thromb. Vasc. Biol. 34, 2321–2329 (2014).
Takagi, J., Petre, B., Walz, T. & Springer, T. Global conformational rearrangements in integrin extracellular domains in outside-in and inside-out signaling. Cell 110, 599–611 (2002).
Xie, C. et al. Structure of an integrin with an alphaI domain, complement receptor type 4. EMBO J. 29, 666–679 (2010).
Springer, T. A., Thompson, W. S., Miller, L. J., Schmalstieg, F. C. & Anderson, D. C. Inherited deficiency of the Mac-1, LFA-1, 150,95 glycoprotein family and its molecular basis. J. Exp. Med. 160, 1901–1918 (1984).
Grakoui, A. et al. The immunological synapse: a molecular machine controlling T cell activation. Science 285, 221–227 (1999).
Henderson, R. B. et al. The use of lymphocyte function-associated antigen (LFA)-1-deficient mice to determine the role of LFA-1, Mac-1, and α4 integrin in the inflammatory response of neutrophils. J. Exp. Med. 194, 219–226 (2001).
Coxon, A. et al. A novel role for the β-2 integrin CD11b/CD18 in neutrophil apoptosis — a homeostatic mechanism in inflammation. Immunity 5, 653–666 (1996).
Tang, T. et al. A role for Mac-1 (CD11b/CD18) in immune complex-stimulated neutrophil function in vivo — Mac-1 deficiency abrogates sustained Fc-γ receptor-dependent neutrophil adhesion and complement-dependent proteinuria in acute glomerulonephritis. J. Exp. Med. 186, 1853–1863 (1997).
Hom, G. et al. Association of systemic lupus erythematosus with C8orf13-BLK and ITGAM-ITGAX. N. Engl. J. Med. 358, 900–909 (2008).
Nath, S. K. et al. A nonsynonymous functional variant in integrin-αM (encoded by ITGAM) is associated with systemic lupus erythematosus. Nat. Genet. 40, 152–154 (2008).
Wu, H. et al. Functional role of CD11c+ monocytes in atherogenesis associated with hypercholesterolemia. Circulation 119, 2708–2717 (2009).
Berlin, C. et al. α4β7 integrin mediates lymphocyte binding to the mucosal vascular addressin MAdCAM-1. Cell 74, 185–195 (1993).
Iwata, M. et al. Retinoic acid imprints gut-homing specificity on T cells. Immunity 21, 527–538 (2004).
Hemler, M. E., Huang, C. & Schwarz, L. The VLA protein family: characterization of five distinct cell surface heterodimers each with a common 130,000 Mr subunit. J. Biol. Chem. 262, 3300–3309 (1987).
Cybulsky, M. I. & Gimbrone, M. A. Jr. Endothelial expression of a mononuclear leukocyte adhesion molecule during atherogenesis. Science 251, 788–791 (1991).
Vedder, N. B. et al. A monoclonal antibody to the adherence-promoting leukocyte glycoprotein, CD18, reduces organ injury and improves survival from hemorrhagic shock and resuscitation in rabbits. J. Clin. Invest. 81, 939–944 (1988).
Yonekawa, K. & Harlan, J. M. Targeting leukocyte integrins in human diseases. J. Leukoc. Biol. 77, 129–140 (2005).
Briskin, M. J., McEvoy, L. M. & Butcher, E. C. MAdCAM-1 has homology to immunoglobulin and mucin-like adhesion receptors and to IgA1. Nature 363, 461–464 (1993).
Yednock, T. A. et al. Prevention of experimental autoimmune encephalomyelitis by antibodies against α4β1 integrin. Nature 356, 63–66 (1992).
Calabresi, P. A. et al. The incidence and significance of anti-natalizumab antibodies: results from AFFIRM and SENTINEL. Neurology 69, 1391–1403 (2007).
Hesterberg, P. E. et al. Rapid resolution of chronic colitis in the cotton-top tamarin with an antibody to a gut-homing integrin α4β7 . Gastroenterology 111, 1373–1380 (1996).
Picarella, D. et al. Monoclonal antibodies specific for β7 integrin and mucosal addressin cell adhesion molecule-1 (MAdCAM-1) reduce inflammation in the colon of scid mice reconstituted with CD45RBhigh CD4+ T cells. J. Immunol. 158, 2099–2106 (1997).
Grant, A. J., Lalor, P. F., Hubscher, S. G., Briskin, M. & Adams, D. H. MAdCAM-1 expressed in chronic inflammatory liver disease supports mucosal lymphocyte adhesion to hepatic endothelium (MAdCAM-1 in chronic inflammatory liver disease). Hepatology 33, 1065–1072 (2001).
Pan, W. J. et al. Pharmacology of AMG 181, a human anti-α4β7 antibody that specifically alters trafficking of gut-homing T cells. Br. J. Pharmacol. 169, 51–68 (2013).
Pan, W. J. et al. Clinical pharmacology of AMG 181, a gut-specific human anti-α4β7 monoclonal antibody, for treating inflammatory bowel diseases. Br. J. Clin. Pharmacol. 78, 1315–1333 (2014).
Mucida, D. et al. Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science 317, 256–260 (2007).
Stefanich, E. G. et al. A humanized monoclonal antibody targeting the β7 integrin selectively blocks intestinal homing of T lymphocytes. Br. J. Pharmacol. 162, 1855–1870 (2011).
Rutgeerts, P. J. et al. A randomised phase I study of etrolizumab (rhuMAb β7) in moderate to severe ulcerative colitis. Gut 62, 1122–1130 (2012).
Vermeire, S. et al. Etrolizumab as induction therapy for ulcerative colitis: a randomised, controlled, Phase 2 trial. Lancet 384, 309–318 (2014).
Masopust, D. et al. Dynamic T cell migration program provides resident memory within intestinal epithelium. J. Exp. Med. 207, 553–564 (2010).
Sugiura, T. et al. A novel, orally active α4 integrin antagonist, AJM300 prevents the development of experimental colitis induced by adoptive transfer of IL-10 deficient CD4+ T cells in mice. J. Pharmacol. Exp. Ther. (2012).
Takazoe, M. Oral α-4 integrin inhibitor (AJM300) in patients with active Crohn's disease — a randomized, double-blind, placebo-controlled trial. Gastroenterology 136 (Suppl. 1), A-181 (2009).
Connor, E. M., Eppihimer, M. J., Morise, Z., Granger, D. N. & Grisham, M. B. Expression of mucosal addressin cell adhesion molecule-1 (MAdCAM- 1) in acute and chronic inflammation. J. Leukocyte Biol. 65, 349–355 (1999).
Briskin, M. et al. Human mucosal addressin cell adhesion molecule-1 is preferentially expressed in intestinal tract and associated lymphoid tissue. Am. J. Pathol. 151, 97–110 (1997).
Sikorski, E. E., Hallmann, R., Berg, E. L. & Butcher, E. C. The Peyer's patch high endothelial receptor for lymphocytes, the mucosal vascular addressin, is induced on a murine endothelial cell line by tumor necrosis factor-α and IL- 1. J. Immunol. 151, 5239–5250 (1993).
Adams, D. H. & Eksteen, B. Aberrant homing of mucosal T cells and extra-intestinal manifestations of inflammatory bowel disease. Nat. Rev. Immunol. 6, 244–251 (2006).
Salmi, M., Andrew, D. P., Butcher, E. C. & Jalkanen, S. Dual binding capacity of mucosal immunoblasts to mucosal and synovial endothelium in humans: dissection of the molecular mechanisms. J. Exp. Med. 181, 137–149 (1995).
Pullen, N. et al. Pharmacological characterization of PF-00547659, an anti-human MAdCAM monoclonal antibody. Br. J. Pharmacol. 157, 281–293 (2009).
Reinisch, W. A. Randomized, multicenter double-blind, placebo-controlled study of the safety and efficacy of anti-MAdCAM antibody PF-00547659 (PF) in patients with moderate to severe ulcerative colitis: results of the TURANDOT study. Gastroenterology 148 (Suppl. 1), S-1193 (2015).
Sandborn, W. J. Anti-MAdCAM-1 antibody (PF-00547659) for active refractory crohn's disease: results of the OPERA study. J. Crohns Colitis 9 (Suppl.), S14 (2015).
Lazaar, A. L. et al. T lymphocytes adhere to airway smooth muscle cells via integrins and CD44 and induce smooth muscle cell DNA synthesis. J. Exp. Med. 180, 807–816 (1994).
Enlimomab Acute Stroke Trial Investigators Use of anti-ICAM-1 therapy in ischemic stroke: results of the Enlimomab Acute Stroke Trial. Neurology 57, 1428–1434 (2001).
Monkley, S. J. et al. Disruption of the talin gene arrests mouse development at the gastrulation stage. Dev. Dyn. 219, 560–574 (2000).
Moser, M. et al. Kindlin-3 is required for β2 integrin–mediated leukocyte adhesion to endothelial cells. Nat. Med. 15, 300–305 (2009).
Shattil, S. J. Integrins and Src: dynamic duo of adhesion signaling. Trends Cell Biol. 15, 399–403 (2005).
Mocsai, A., Ruland, J. & Tybulewicz, V. L. The SYK tyrosine kinase: a crucial player in diverse biological functions. Nat. Rev. Immunol. 10, 387–402 (2010).
Polman, C. H. et al. A randomized, placebo-controlled trial of natalizumab for relapsing multiple sclerosis. N. Engl. J. Med. 354, 899–910 (2006).
Natalizumab: new drug. Multiple sclerosis: risky market approval. Prescrire Int. 17, 7–10 (2008).
Balcer, L. J. et al. Natalizumab reduces visual loss in patients with relapsing multiple sclerosis. Neurology 68, 1299–1304 (2007).
Rudick, R. A. et al. Health-related quality of life in multiple sclerosis: effects of natalizumab. Ann. Neurol. 62, 335–346 (2007).
Rudick, R. A. & Miller, D. M. Health-related quality of life in multiple sclerosis: current evidence, measurement and effects of disease severity and treatment. CNS Drugs 22, 827–839 (2008).
Miller, D. H. et al. MRI outcomes in a placebo-controlled trial of natalizumab in relapsing MS. Neurology 68, 1390–1401 (2007).
Berger, J. R. & Houff, S. A. Neurological infections: the year of PML and influenza. Lancet Neurol. 9, 14–17 (2010).
Sandborn, W. J. et al. Natalizumab induction and maintenance therapy for Crohn's disease. N. Engl. J. Med. 353, 1912–1925 (2005).
Targan, S. R. et al. Natalizumab for the treatment of active Crohn's disease: results of the ENCORE Trial. Gastroenterology 132, 1672–1683 (2007).
Gordon, F. H. et al. A pilot study of treatment of active ulcerative colitis with natalizumab, a humanized monoclonal antibody to α-4 integrin. Aliment. Pharmacol. Ther. 16, 699–705 (2002).
Ghosh, S. et al. Natalizumab for active Crohn's disease. New Engl. J. Med. 348, 24–32 (2003).
Best, W. R., Becktel, J. M., Singleton, J. W. & Kern, F. Jr. Development of a Crohn's disease activity index. National Cooperative Crohn's Disease Study. Gastroenterology 70, 439–444 (1976).
Du Pasquier, R. A. et al. A prospective study demonstrates an association between JC virus-specific cytotoxic T lymphocytes and the early control of progressive multifocal leukoencephalopathy. Brain 127, 1970–1978 (2004).
Krumbholz, M., Meinl, I., Kumpfel, T., Hohlfeld, R. & Meinl, E. Natalizumab disproportionately increases circulating pre-B and B cells in multiple sclerosis. Neurology 71, 1350–1354 (2008).
Carson, K. R. et al. Monoclonal antibody-associated progressive multifocal leucoencephalopathy in patients treated with rituximab, natalizumab, and efalizumab: a review from the Research on Adverse Drug Events and Reports (RADAR) Project. Lancet Oncol. 10, 816–824 (2009).
Feagan, B. G. et al. An ascending dose trial of a humanised a4b7 antibody in ulcerative colitis (UC). Gastroenterology 118 (Suppl. 2), A874 (2000).
Feagan, B. G. et al. Treatment of ulcerative colitis with a humanized antibody to the α4β7 integrin. N. Engl. J. Med. 352, 2499–2507 (2005).
Feagan, B. G. et al. Treatment of active Crohn's disease with MLN0002, a humanized antibody to the α4β7 integrin. Clin. Gastroenterol. Hepatol 6, 1370–1377 (2008).
Sands, B. E. et al. Effects of vedolizumab induction therapy for patients with Crohn's disease who failed tumor necrosis factor antagonist treatment. Gastroenterology 147, 618–627.e3 (2013).
Parikh, A. et al. Vedolizumab for the treatment of active ulcerative colitis: a randomized controlled phase 2 dose-ranging study. Inflamm. Bowel Dis. 18, 1470–1479 (2011).
Feagan, B. G. et al. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N. Engl. J. Med. 369, 699–710 (2013).
Sandborn, W. J. et al. Vedolizumab as induction and maintenance therapy for Crohn's disease. N. Engl. J. Med. 369, 711–721 (2013).
Acknowledgements
The authors are supported by a grant from the National Institutes of Health (DK108670) and a Biomedical Laboratory Research and Development Vetrans Affairs Merit Review award (1I01BX001051) to J.R.-N., grants from the National Institutes of Health (HL 56595 and HL 78784) to S.S., and grants from the National Institutes of Health (DK091222 and HL078784) to K.L.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
W.J.S. participates in clinical trials in this area. The other authors declare no competing interests.
Related links
FURTHER INFORMATION
Rights and permissions
About this article
Cite this article
Ley, K., Rivera-Nieves, J., Sandborn, W. et al. Integrin-based therapeutics: biological basis, clinical use and new drugs. Nat Rev Drug Discov 15, 173–183 (2016). https://doi.org/10.1038/nrd.2015.10
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrd.2015.10
This article is cited by
-
Integrin signaling in cancer: bidirectional mechanisms and therapeutic opportunities
Cell Communication and Signaling (2023)
-
The characteristics and the multiple functions of integrin β1 in human cancers
Journal of Translational Medicine (2023)
-
Combination of Quercetin or/and siRNA-loaded DDAB-mPEG-PCL hybrid nanoparticles reverse resistance to Regorafenib in colon cancer cells
BMC Complementary Medicine and Therapies (2022)
-
Foudroyant cerebral venous (sinus) thrombosis triggered through CLEC-2 and GPIIb/IIIa dependent platelet activation
Nature Cardiovascular Research (2022)
-
Emerging therapeutic opportunities for integrin inhibitors
Nature Reviews Drug Discovery (2022)