Key Points
-
While TKIs have revolutionised the treatment of CML, allogeneic HSCT remains the only treatment capable of curing CML
-
For the 10–15% of patients with chronic phase CML unable to achieve an adequate response with a tolerable dose of TKI, allogeneic HSCT offers a feasible alternative strategy
-
Early assessment strategies should be used to identify those destined to fail to respond to TKIs, allowing rapid transition through multiple TKIs and on to, if necessary, HSCT before disease progression occurs
-
The mechanisms of disease control from TKI and HSCT are independent, therefore, poor response to TKI does not per se predict poor response to HSCT
-
Allogeneic HSCT remains the standard of care for patients with accelerated phase or blast crisis CML
Abstract
The management of chronic myeloid leukaemia (CML) has changed extensively over the past 15 years. Prior to the development of targeted therapies and in the absence of allogeneic haematopoetic stem-cell transplantation (HSCT), the median survival was 5–7 years. HSCT was quickly established as the standard of care for eligible patients through the 1980s and 1990s, when considerable advances were made in the optimization of conditioning regimens and supportive care. Exploiting a deeper understanding of the molecular basis of CML, the development of tyrosine kinase inhibitors (TKIs) in the late 1990s revolutionized the management of the disease. TKIs offer the prospect of long-term disease control with a simple oral therapy, and are the first-line treatment in the 21st century. The majority of patients treated with TKIs achieve excellent responses with sustained treatment, and some even continue to have undetectable or exceptionally low level disease upon TKI withdrawal; however, for an almost equal number of patients, an adequate response cannot be achieved with any of the currently available TKIs. For those patients who fail to respond adequately to TKIs, HSCT offers the best prospect of long-term survival.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Rowley, J. D. A new consistent chromosomal abnormality in chronic myelogenous leukaemia identified by quinacrine fluorescence and Giemsa staining. Nature 243, 290–293 (1973).
Shtivelman, E., Lifshitz, B., Gale, R. P. & Canaani, E. Fused transcript of abl and bcr genes in chronic myelogenous leukaemia. Nature 315, 550–554 (1985).
Voncken, J. W. et al. BCR/ABL P210 and P190 cause distinct leukemia in transgenic mice. Blood 86, 4603–4611 (1995).
Swerdlow, S. H. et al. in WHO Classification of Tumours 4th edn Vol. 2 No. 2 (World Health Organization, 2008).
Baccarani, M. et al. Evolving concepts in the management of chronic myeloid leukemia: recommendations from an expert panel on behalf of the European LeukemiaNet. Blood 108, 1809–1820 (2006).
Hermans, A. et al. Unique fusion of bcr and c-abl genes in Philadelphia chromosome positive acute lymphoblastic leukemia. Cell 51, 33–40 (1987).
Guilhot, F. et al. Interferon alfa-2b combined with cytarabine versus interferon alone in chronic myelogenous leukemia. French Chronic Myeloid Leukemia Study Group. N. Engl. J. Med. 337, 223–229 (1997).
Gratwohl, A. et al. Allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia in Europe 2006: transplant activity, long-term data and current results. An analysis by the Chronic Leukemia Working Party of the European Group for Blood and Marrow Transplantation (EBMT). Haematologica 91, 513–521 (2006).
Gratwohl, A. & Heim, D. Current role of stem cell transplantation in chronic myeloid leukaemia. Best Pract. Res. Clin. Haematol. 22, 431–443 (2009).
Saussele, S. et al. Allogeneic hematopoietic stem cell transplantation (allo SCT) for chronic myeloid leukemia in the imatinib era: evaluation of its impact within a subgroup of the randomized German CML Study IV. Blood 115, 1880–1885 (2010).
Pavlu, J., Szydlo, R. M., Goldman, J. M. & Apperley, J. F. Three decades of transplantation for chronic myeloid leukemia: what have we learned? Blood 117, 755–763 (2011).
Deininger M. et al. International randomized study of interferon vs STI571 (IRIS) 8-year follow up: sustained survival and low risk for progression or events in patients with newly diagnosed chronic myeloid leukemia in chronic phase treated with imatinib [abstract 1126]. Blood 114, a1126 (2009).
Sasaki, K., Strom, S. & O'Brien, S. Relative survival in patients with chronic-phase chronic myeloid leukaemia in the tyrosine-kinase inhibitor era: analysis of patient data from six prospective clinical trials. Lancet Haem. 2, 186–193 (2015).
Mahon, F. X. et al. Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre Stop Imatinib (STIM) trial. Lancet Oncol. 11, 1029–1035 (2010).
Ross, D. M. et al. Safety and efficacy of imatinib cessation for CML patients with stable undetectable minimal residual disease: results from the TWISTER study. Blood 122, 515–522 (2013).
Socié, G. et al. Nonmalignant late effects after allogeneic stem cell transplantation Blood. 101, 3373–3385 (2003).
Duell, T. et al. Health and functional status of long-term survivors of bone marrow transplantation. Ann. Intern. Med. 126, 184–192 (1997).
Simon, W., Segel, G. B. & Lichtman, M. A. Early allogeneic stem cell transplantation for chronic myelogenous leukemia in the imatinib era: a preliminary assessment. Blood Cells Mol. Dis. 37, 116–124 (2006).
Baccarani, M. et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood 122, 872–884 (2013).
Hanfstein, B. et al. Early molecular and cytogenetic response is predictive for long-term progression-free and overall survival in chronic myeloid leukemia (CML). Leukemia 26, 2096–2102 (2012).
Marin, D. et al. Assessment of BCR-ABL1 transcript levels at 3 months is the only requirement for predicting outcome for patients with chronic myeloid leukemia treated with tyrosine kinase inhibitors. J. Clin. Oncol. 30, 232–238 (2012).
Fefer, A. et al. Disappearance of Ph1-positive cells in four patients with chronic granulocytic leukemia after chemotherapy, irradiation and marrow transplantation from an identical twin. N. Engl. J. Med. 300, 333–337 (1979).
Goldman, J. M. et al. Marrow transplantation for patients in the chronic phase of chronic granulocytic leukaemia. Lancet 320, 623–625 (1982).
Beatty, P. G., Ash, R., Hows, J. M. & McGlave, P. B. The use of unrelated bone marrow donors in the treatment of patients with chronic myelogenous leukemia: experience of four marrow transplant centers. Bone Marrow Transplant. 4, 287–290 (1989).
Goldman, J. M. & Mackinnon, S. Bone marrow transplantation for chronic myeloid leukaemia using matched unrelated donors. Bone Marrow Transplant. 4 (Suppl.), 38–39 (1989).
Apperley, J. F. et al. Bone marrow transplantation for patients with chronic myeloid leukaemia: T-cell depletion with Campath-1 reduces the incidence of graft-versus-host disease but may increase the risk of leukaemic relapse. Bone Marrow Transplant. 1, 53–66 (1986).
Kolb, H. J. et al. Donor leukocyte transfusions for treatment of recurrent chronic myelogenous leukemia in marrow transplant patients. Blood 76, 2462–2465 (1990).
Mackinnon, S. et al. Adoptive immunotherapy evaluating escalating doses of donor leukocytes for relapse of chronic myeloid leukemia after bone marrow transplantation: separation of graft-versus-leukemia responses from graft-versus-host disease. Blood 86, 1261–1268 (1995).
Dazzi, F. et al. Comparison of single-dose and escalating-dose regimens of donor lymphocyte infusion for relapse after allografting for chronic myeloid leukemia. Blood 95, 67–71 (2000).
Innes, A. J. et al. Escalating-dose HLA-mismatched DLI is safe for the treatment of leukaemia relapse following alemtuzumab-based myeloablative allo-SCT. Bone Marrow Transplant. 48, 1324–1328 (2013).
Or, R. et al. Nonmyeloablative allogeneic stem cell transplantation for the treatment of chronic myeloid leukemia in first chronic phase. Blood 101, 441–445 (2003).
Crawley, C. et al. Outcomes of reduced-intensity transplantation for chronic myeloid leukemia: an analysis of prognostic factors from the Chronic Leukemia Working Party of the EBMT. Blood 106, 2969–29676 (2005).
Kebriaei, P. et al. Long-term follow-up of allogeneic hematopoietic stem-cell transplantation with reduced-intensity conditioning for patients with chronic myeloid leukemia. Blood 110, 3456–3462 (2007).
Gratwohl, A. et al. Risk assessment for patients with chronic myeloid leukaemia before allogeneic blood or marrow transplantation. Chronic Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Lancet 352, 1087–1092 (1998).
Gratwohl, A. et al. Risk score for outcome after allogeneic hematopoietic stem cell transplantation: a retrospective analysis. Cancer 115, 4715–4726 (2009).
Gratwohl, A., Goldman, J., Gluckman, E. & Zwaan, F. Effect of splenectomy before bone-marrow transplantation on survival in chronic granulocytic leukaemia. Lancet 326, 1290–1291 (1985).
Lin, F., van Rhee, F., Goldman, J. M. & Cross, N. C. Kinetics of increasing BCR-ABL transcript numbers in chronic myeloid leukemia patients who relapse after bone marrow transplantation. Blood 87, 4473–4478 (1996).
Olavarria, E. et al. Early detection of BCR-ABL transcripts by quantitative reverse transcriptase-polymerase chain reaction predicts outcome after allogeneic stem cell transplantation for chronic myeloid leukemia. Blood 97, 1560–1565 (2001).
Hehlmann, R. How I treat CML blast crisis. Blood 120, 737–747 (2012).
Silver, R. T. The blast phase of chronic myeloid leukaemia. Best Pract. Res. Clin. Haematol. 22, 387–394 (2009).
Kantarjian, H. M. et al. Imatinib mesylate (STI571) therapy for Philadelphia chromosome-positive chronic myelogenous leukemia in blast phase. Blood 99, 3547–53 (2002).
Wadhwa, J. et al. Factors affecting duration of survival after onset of blastic transformation of chronic myeloid leukemia. Blood 99, 2304–2309 (2002).
Fruehauf, S. et al. Imatinib combined with mitoxantrone/etoposide and cytarabine is an effective induction therapy for patients with chronic myeloid leukemia in myeloid blast crisis. Cancer 109, 1543–1549 (2007).
Oki, Y. et al. Phase II study of low-dose decitabine in combination with imatinib mesylate in patients with accelerated or myeloid blastic phase of chronic myelogenous leukemia. Cancer 109, 899–906 (2007).
Milojkovic, D. et al. Efficacy of combining dasatinib and FLAG-IDA for patients with chronic myeloid leukemia in blastic transformation. Haematologica 97, 473–474 (2012).
Khoury, H. J. et al. Prognostic factors for outcomes in allogeneic transplantation for CML in the imatinib era: a CIBMTR analysis. Bone Marrow Transplant. 47, 810–816 (2012).
Koreth, J. et al. Allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission: systematic review and meta-analysis of prospective clinical trials. JAMA 301, 2349–2361 (2009).
Gupta, V. et al. Comparable survival after HLA-well-matched unrelated or matched sibling donor transplantation for acute myeloid leukemia in first remission with unfavorable cytogenetics at diagnosis. Blood 116, 1839–1848 (2010).
Jiang, Q. et al. Imatinib mesylate versus allogeneic hematopoietic stem cell transplantation for patients with chronic myelogenous leukemia in the accelerated phase. Blood 117, 3032–3040 (2011).
Ohanian, M. et al. Tyrosine kinase inhibitors as initial therapy for patients with chronic myeloid leukemia in accelerated phase. Clin. Lymphoma Myeloma Leuk. 14, 155–162 (2014).
Cortes, J. E. et al. Four-year (yr) follow-up of patients (pts) with newly diagnosed chronic myeloid leukemia in chronic phase (CML-CP) receiving dasatinib or imatinib: efficacy based on early response [abstract 653]. Blood 122, a653 (2013).
Saglio, G. et al. ENESTnd Update: nilotinib (NIL) vs imatinib (IM) in patients (pts) with newly diagnosed chronic myeloid leukemia in chronic phase (CML-CP) and the impact of early molecular response (EMR) and Sokal risk at diagnosis on long-term outcomes [abstract 632]. Blood 122, a632 (2013).
Shah, N. P. et al. Long-term outcome with dasatinib after imatinib failure in chronic-phase chronic myeloid leukemia: follow-up of a phase 3 study. Blood 123, 2317–2324 (2014).
Giles, F. J. et al. Nilotinib in imatinib-resistant or imatinib-intolerant patients with chronic myeloid leukemia in chronic phase: 48-month follow-up results of a phase II study. Leukemia 27, 107–112 (2013).
Ibrahim, A. R. et al. Efficacy of tyrosine kinase inhibitors (TKIs) as third-line therapy in patients with chronic myeloid leukemia in chronic phase who have failed 2 prior lines of TKI therapy. Blood 116, 5497–5500 (2010).
Russo Rossi, A. et al. Outcome of 82 chronic myeloid leukemia patients treated with nilotinib or dasatinib after failure of two prior tyrosine kinase inhibitors. Haematologica 98, 399–403 (2013).
Lipton, J. H. et al. Comparative efficacy of tyrosine kinase inhibitor treatments in the third-line setting, for chronic-phase chronic myelogenous leukemia after failure of second-generation tyrosine kinase inhibitors. Leuk. Res. 39, 58–64 (2015).
Milojkovic, D. et al. Early prediction of success or failure of treatment with second-generation tyrosine kinase inhibitors in patients with chronic myeloid leukemia. Haematologica 95, 224–231 (2010).
Cortes, J. E. et al. A phase 2 trial of ponatinib in Philadelphia chromosome-positive leukemias. N. Engl. J. Med. 369, 1783–1796 (2013).
Zaucha, J. M. et al. Imatinib therapy prior to myeloablative allogeneic stem cell transplantation. Bone Marrow Transplant. 36, 417–424 (2005).
Deininger, M. et al. The effect of prior exposure to imatinib on transplant-related mortality. Haematologica 91, 452–459 (2006).
Lee, S. J. et al. Impact of prior imatinib mesylate on the outcome of hematopoietic cell transplantation for chronic myeloid leukemia. Blood 112, 3500–3507 (2008).
Milojkovic, D. et al. Prognostic significance of EBMT score for chronic myeloid leukaemia patients in the era of tyrosine kinase inhibitor therapy: a retrospective study from the chronic malignancy working party of the European Group for Blood and Marrow Transplantation (EBMT) [abstract PH0064]. Bone Marrow Transplant. 49, S6–S88 (2014)
Krejci, M. et al. Clinical outcomes and direct hospital costs of reduced-intensity allogeneic transplantation in chronic myeloid leukemia. Bone Marrow Transplant. 38, 483–491 (2006).
Jabbour, E. et al. Early response with dasatinib or imatinib in chronic myeloid leukemia: 3-year follow-up from a randomized phase 3 trial (DASISION). Blood 123, 494–500 (2014).
Saglio, G. et al. Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N. Engl. J. Med. 362, 2251–2259 (2010).
Marin, D. et al. Adherence is the critical factor for achieving molecular responses in patients with chronic myeloid leukemia who achieve complete cytogenetic responses on imatinib. J. Clin. Oncol. 28, 2381–2318 (2010).
Eliasson, L., Clifford, S., Barber, N. & Marin, D. Exploring chronic myeloid leukemia patients' reasons for not adhering to the oral anticancer drug imatinib as prescribed. Leuk. Res. 35, 626–630 (2011).
Socié, G. et al. Chronic graft-versus-host disease: long-term results from a randomized trial on graft-versus-host disease prophylaxis with or without anti-T-cell globulin ATG-Fresenius. Blood 117, 6375–6382 (2011).
Eapen, M. et al. Long-term survival after transplantation of unrelated donor peripheral blood or bone marrow hematopoietic cells for hematologic malignancy. Biol. Blood Marrow Transplant. 21, 55–59 (2015).
Anasetti, C. et al. Peripheral-blood stem cells versus bone marrow from unrelated donors. N. Engl. J. Med. 367, 1487–1496 (2012).
Kaeda, J. et al. Serial measurement of BCR-ABL transcripts in the peripheral blood after allogeneic stem cell transplantation for chronic myeloid leukemia: an attempt to define patients who may not require further therapy. Blood 107, 4171–4176 (2006).
Innes, A. J. et al. The majority of patients receiving donor lymphocyte infusions for relapsed chronic myeloid leukemia remain PCR positive despite maintaining long-term remission [abstract 4103]. Blood 118, a4103 (2011).
Luo, Y. et al. Reduced-intensity allogeneic transplantation combined with imatinib mesylate for chronic myeloid leukemia in first chronic phase. Leukemia 23, 1171–1174 (2009).
Liu, Q. F. et al. Long-term outcomes of HLA-matched sibling compared with mismatched related and unrelated donor hematopoietic stem cell transplantation for chronic phase chronic myelogenous leukemia: a single institution experience in China. Ann. Hematol. 90, 331–341 (2011).
Zheng, C. et al. Comparison of unrelated cord blood transplantation and HLA-matched sibling hematopoietic stem cell transplantation for patients with chronic myeloid leukemia in advanced stage. Biol. Blood Marrow Transplant. 19, 1708–1712 (2013).
Shimoni, A. et al. Prior treatment with the tyrosine kinase inhibitors dasatinib and nilotinib allows stem cell transplantation (SCT) in a less advanced disease phase and does not increase SCT Toxicity in patients with chronic myelogenous leukemia and philadelphia positive acute lymphoblastic leukemia. Leukemia 23, 190–194 (2009).
Sanz, J. et al. Single-unit umbilical cord blood transplantation from unrelated donors in adult patients with chronic myelogenous leukemia. Biol. Blood Marrow Transplant. 16, 1589–1595 (2010).
Jabbour, E. et al. Results of allogeneic hematopoietic stem cell transplantation for chronic myelogenous leukemia patients who failed tyrosine kinase inhibitors after developing BCR-ABL1 kinase domain mutations. Blood 117, 3641–3647 (2011).
Warlick, E. et al. Reduced intensity conditioning is superior to nonmyeloablative conditioning for older chronic myelogenous leukemia patients undergoing hematopoietic cell transplant during the tyrosine kinase inhibitor era. Blood 119, 4083–4090 (2012).
Topcuoglu, P. et al. Case-matched comparison with standard versus reduced intensity conditioning regimen in chronic myeloid leukemia patients. Ann. Hematol. 91, 577–586 (2012).
Zuckerman, T. et al. Allogeneic stem cell transplantation for patients with chronic myeloid leukemia: risk stratified approach with a long-term follow-up. Am. J. Hematol. 87, 875–879 (2012).
Oyekunle, A. et al. Outcome of allogeneic SCT in patients with chronic myeloid leukemia in the era of tyrosine kinase inhibitor therapy. Ann. Hematol. 92, 487–496 (2013).
Kelemen, E., Masszi, T., Reményi, P., Barta, A. & Pálóczi, K. Reduction in the frequency of transplant-related complications in patients with chronic myeloid leukemia undergoing BMT preconditioned with a new, non-myeloablative drug combination. Bone Marrow Transplant. 21, 747–749 (1998).
Barta, A. et al. Remarkably reduced transplant-related complications by dibromomannitol non-myeloablative conditioning before allogeneic bone marrow transplantation in chronic myeloid leukemia. Acta Haematol. 105, 64–70 (2001).
Weisser, M. et al. Reduced-intensity conditioning using TBI (8 Gy), fludarabine, cyclophosphamide and ATG in elderly CML patients provides excellent results especially when performed in the early course of the disease. Bone Marrow Transplant. 34, 1083–1088 (2004).
Kerbauy, F. R. et al. Hematopoietic cell transplantation from HLA-identical sibling donors after low-dose radiation-based conditioning for treatment of CML. Leukemia 19, 990–997 (2005).
Ruiz-Argüelles, G. J. et al. The early referral for reduced-intensity stem cell transplantation in patients with Ph1 (+) chronic myelogenous leukemia in chronic phase in the imatinib era: results of the Latin American Cooperative Oncohematology Group (LACOHG) prospective, multicenter study. Bone Marrow Transplant. 36, 1043–1047 (2005).
Faber, E. et al. Reduced-intensity conditioning for allogeneic stem cell transplantation in patients with chronic myeloid leukemia is associated with better overall survival but inferior disease-free survival when compared with myeloablative conditioning–a retrospective study of the Czech National Hematopoietic Stem Cell Transplantation Registry. Neoplasma 54, 443–446 (2007).
Olavarria, E. et al. Posttransplantation imatinib as a strategy to postpone the requirement for immunotherapy in patients undergoing reduced-intensity allografts for chronic myeloid leukemia. Blood 110, 4614–4617 (2007).
Acknowledgements
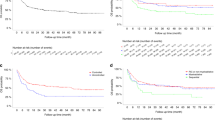
J.F.A. and D.M. acknowledge the support of the NIHR Biomedical Research Centre. A.J.I. acknowledges the support of an MRC and NIHR Chain-Florey Clinical Research Fellowship. We are extremely grateful to the EBMT Transplant activity survey office, and in particular to Helen Baldomero and Alois Gratwohl, for the data in Fig. 2.
Author information
Authors and Affiliations
Contributions
A.J.I., D.M. and J.F.A. contributed equally to researching data for article, discussing its content, writing the article, and reviewing and/or editing the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
J.F.A. and D.M have received honouraria from, and serve on advisory boards for, Ariad, Bristol–Myers Squibb, Novartis and Pfizer. A.J.I. declares no competing interests.
Rights and permissions
About this article
Cite this article
Innes, A., Milojkovic, D. & Apperley, J. Allogeneic transplantation for CML in the TKI era: striking the right balance. Nat Rev Clin Oncol 13, 79–91 (2016). https://doi.org/10.1038/nrclinonc.2015.193
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrclinonc.2015.193